Volume 7, Issue 1 (1-2019)
J. Pediatr. Rev 2019, 7(1): 41-44 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shayesteh Azar M, Taheri S, Jafarpour H, Shayesteh Azar S, Ghaffari S. Diagnostic Methods and Treatments of Anterior Interosseous Nerve Syndromes in Supracondylar Humerus Fractures: Case Series and Literature Review. J. Pediatr. Rev 2019; 7 (1) :41-44
URL: http://jpr.mazums.ac.ir/article-1-174-en.html
URL: http://jpr.mazums.ac.ir/article-1-174-en.html
Masoud Shayesteh Azar *1 
 , Sadegh Taheri2
, Sadegh Taheri2 
 , Hamed Jafarpour3
, Hamed Jafarpour3 
 , Shadi Shayesteh Azar4
, Shadi Shayesteh Azar4 
 , Salman Ghaffari5
, Salman Ghaffari5 



 , Sadegh Taheri2
, Sadegh Taheri2 
 , Hamed Jafarpour3
, Hamed Jafarpour3 
 , Shadi Shayesteh Azar4
, Shadi Shayesteh Azar4 
 , Salman Ghaffari5
, Salman Ghaffari5 


1- Orthopedic Research Centre, Mazandaran University of Medical Sciences, Sari, Iran.
2- Department of Orthopedic Surgery, Mazandaran University of Medical Science, Sari, Iran
3- Student Research Committee, Mazandaran University of Medical Science, Sari, Iran.
4- Student Research Committee, Mazandaran University of Medical Sciences, Sari, Iran.
5- Student Research Committee, Mazandaran University of Medical Sciences, Sari, Iran
2- Department of Orthopedic Surgery, Mazandaran University of Medical Science, Sari, Iran
3- Student Research Committee, Mazandaran University of Medical Science, Sari, Iran.
4- Student Research Committee, Mazandaran University of Medical Sciences, Sari, Iran.
5- Student Research Committee, Mazandaran University of Medical Sciences, Sari, Iran
Full-Text [PDF 364 kb]
(2900 Downloads)
| Abstract (HTML) (7423 Views)
Full-Text: (5237 Views)
1. Introduction
Supracondylar humerus fracture is one of the most common fractures in children (1). It includes half of all fractures of the elbow and about 30% of all limb fractures in children below 7 years (2-4). According to the fracture pattern and mechanism of the injury, the supracondylar humerus fractures are classified into two types: extension or flexion type (2, 5-7). The standard surgical treatment for displaced supracondylar humeral fracture is reduction followed by percutaneous pin fixation (8). Neurovascular structures are prone to damage because of proximity to fracture location. The neurovascular complication has been reported in 5%-19% of displaced fractures. Neurological complications associated with supracondylar humerus fractures in children, such as Anterior Interosseous Nerve (AIN) syndrome, are well- known (6, 9, 10). The AIN innervates three muscles: the flexor pollicis longus, flexor digitorum profundus of the second digit and the pronator quadratus (11, 12). AIN deficit was discovered as isolated or in combination with other nerve palsies in almost 12.9% of supracondylar humerus fractures (7).
2. Cases Presentation
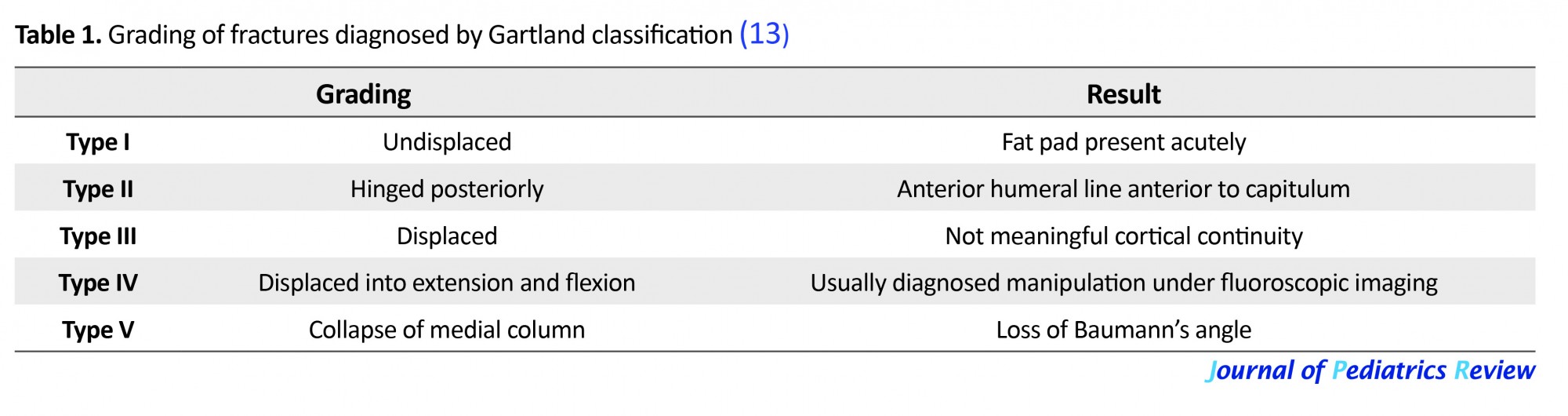
From November 2014 to November 2016, 33 children with humeral supracondylar fracture were admitted to the orthopedic surgery centers of Imam Hospital in Sari, north of Iran. Four of them had AIN syndrome. The mean age of the patients was 6 years. All patients had extension type fracture. Based on the Gartland grade classification (13), three cases were of grade 3, and 1 case was of grade 2. The average nerve recovery period took up to four weeks. Closed or open reduction and pinning were taken as treatment procedures for these patients (Tables 1 and 2).
Supracondylar humerus fracture is one of the most common fractures in children (1). It includes half of all fractures of the elbow and about 30% of all limb fractures in children below 7 years (2-4). According to the fracture pattern and mechanism of the injury, the supracondylar humerus fractures are classified into two types: extension or flexion type (2, 5-7). The standard surgical treatment for displaced supracondylar humeral fracture is reduction followed by percutaneous pin fixation (8). Neurovascular structures are prone to damage because of proximity to fracture location. The neurovascular complication has been reported in 5%-19% of displaced fractures. Neurological complications associated with supracondylar humerus fractures in children, such as Anterior Interosseous Nerve (AIN) syndrome, are well- known (6, 9, 10). The AIN innervates three muscles: the flexor pollicis longus, flexor digitorum profundus of the second digit and the pronator quadratus (11, 12). AIN deficit was discovered as isolated or in combination with other nerve palsies in almost 12.9% of supracondylar humerus fractures (7).
2. Cases Presentation
From November 2014 to November 2016, 33 children with humeral supracondylar fracture were admitted to the orthopedic surgery centers of Imam Hospital in Sari, north of Iran. Four of them had AIN syndrome. The mean age of the patients was 6 years. All patients had extension type fracture. Based on the Gartland grade classification (13), three cases were of grade 3, and 1 case was of grade 2. The average nerve recovery period took up to four weeks. Closed or open reduction and pinning were taken as treatment procedures for these patients (Tables 1 and 2).
3. Discussion
Non-displaced or minimally displaced fractures in children can be treated with a splint at 90° of flexion for 2-3 weeks (8). While the angulation is more clearly visible on lateral radiographs, varus deformities can be measured more effectively on anteroposterior radiographs using Baumann’s angle. In case of an over 10° varus, closed reduction and pinning must be performed. Gartland type II fractures need closed reduction. These fractures may be stabilized at 90° of flexion. However, fixation with pin is required for stabilizing the fracture in more than 90° of elbow flexion (13, 14).
3.1. Reduction maneuver for supracondylar humerus fractures
Wide-wake fluoroscopy-based reduction must be performed. First, for neurovascular release, traction must be performed along the humerus within the range of elbow flexion. Traction must be avoided in elbow extension, as it can entangle blood vessels and nerves. If the proximal segment has penetrated the brachialis muscle, longer traction is required to induce the sensation of release of the fractured segment. The release is achieved by the proximal-to-distal milking of the brachialis muscle. Thus, the reduction maneuver starts by the hyperflexion of elbow, while applying pressure towards the anterior of the olecranon. The control radiograph is taken at this point. If the distal segment is rotated, it can be corrected in two ways. The most prevalent type is the varus rotation of the distal segment. In this case, extra pressure is applied inwardly with simultaneous pronation of the forearm. If the appropriate Baumann’s angle is not achieved, the reduction maneuver is repeated with extra valgus pressure. If the vascular injury is not improved after the initial closed reduction and splinting, the open method must be considered as well, especially in case of open fractures, severe elbow inflammation, and vascular injury (1, 14-16). Gartland type III fractures are susceptible to neurovascular injuries. The preferred treatment for this type of fracture is the open/closed reduction and pinning method, which has fewer complications than reduction and splinting.
3.2. Indication for surgery in supracondylar humerus fractures
Surgical treatment is indicated in supracondylar humerus fractures for the following cases: 1. Closed reduction is not possible; 2. The fracture is unstable after reduction, and reduction cannot be maintained; 3. In case of neural injury during or following reduction; 4. If vascular exploration is required; 5. In open fractures; 6. In all Gartland type II or III fractures which need an over 90° of flexion to maintain reduction; 7. In all Gartland type IV fractures; 8. For polytraumatized patients with another ipsilateral fracture (17).
3.3. Classification of supracondylar humerus fractures
There are various classifications for these fractures: a) Displaced or non-displaced; b) Open or closed; c) Complicated or uncomplicated (with or without neural/vascular involvement; d) Extension type (95%) or flexion type (5%); and e) Gartland classification system which is based on lateral radiographs; it is mostly used for extension-type fractures and can serve as a guide for the treatment method (14, 18).
Patients who suffer from AIN syndrome are typically unable to form an “O” by using the index finger and thumb because of paralysis of the flexor pollicis longus and flexor digitorum profundus (impaired flexion of the interphalangeal joint of the thumb and the distal interphalangeal joint of the index finger). For example, the patients will lose the ability to button their shirts or turn on their car keys to start it. On physical examination, the Pinch Grip test shows a positive result for patients who are unable to demonstrate the “OK” sign; instead they clamp the sheet between an extended thumb and index finger (19).
For the surgeon, the most concerning issue in the humeral supracondylar fracture is a vascular state, so there may not be any specific test for flexion of the terminal phalanges of thumb and index. So it can be missed easily. Furthermore, AIN is a motor nerve without a sensory task, so the lack of sensory loss does not exist to help diagnosis. Usually, median nerve and AIN are examined by finger flexion, but children deceive examiner by using the third finger to flex the second finger (18).
In all our cases, complete nerve palsy recovery was observed within 3 to 5 weeks. In past studies, complete AIN palsy recovery was observed after 4 to 17 weeks. The neurophysiological and electromyographic examination should be performed after 4 months of conservative treatment without any recovery (8).
The clinical findings of AIN syndrome are composed of lack of flexion of the terminal interphalangeal joint of the thumb and the distal interphalangeal joint of the index finger. The pinch position can only be accomplished with the terminal phalanges of these fingers hyperextended. Pathological spontaneous activity in the affected muscles can be manifested by the electromyographic examination, positive sharp waves, and fibrillation that show denervation (20-22).
Complete AIN palsy recovery was observed after 4 to 17 weeks. Electromyographic examination should be performed after 4 months of conservative treatment without any recovery (23).
According to the just motor (no sensory) function of AIN and also deceiving children using the third finger to flex the second one, underestimation of AIN syndrome in supracondylar fracture of the humerus can be expected. So, the physician should be more careful about physical examination (OK sign) in supracondylar fracture of humerus besides the vascular state.
Ethical Considerations
Compliance with ethical guidelines
This study is just a case report for the diagnostic methods and treatments and all procedures are performed according to the standard protocols.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgements
The authors would like to express their thanks to the Department of Orthopedic Surgery of Imam Khomeini Hospital and Student Research Committee of Mazandaran University of Medical Sciences to support this research.
References
Non-displaced or minimally displaced fractures in children can be treated with a splint at 90° of flexion for 2-3 weeks (8). While the angulation is more clearly visible on lateral radiographs, varus deformities can be measured more effectively on anteroposterior radiographs using Baumann’s angle. In case of an over 10° varus, closed reduction and pinning must be performed. Gartland type II fractures need closed reduction. These fractures may be stabilized at 90° of flexion. However, fixation with pin is required for stabilizing the fracture in more than 90° of elbow flexion (13, 14).
3.1. Reduction maneuver for supracondylar humerus fractures
Wide-wake fluoroscopy-based reduction must be performed. First, for neurovascular release, traction must be performed along the humerus within the range of elbow flexion. Traction must be avoided in elbow extension, as it can entangle blood vessels and nerves. If the proximal segment has penetrated the brachialis muscle, longer traction is required to induce the sensation of release of the fractured segment. The release is achieved by the proximal-to-distal milking of the brachialis muscle. Thus, the reduction maneuver starts by the hyperflexion of elbow, while applying pressure towards the anterior of the olecranon. The control radiograph is taken at this point. If the distal segment is rotated, it can be corrected in two ways. The most prevalent type is the varus rotation of the distal segment. In this case, extra pressure is applied inwardly with simultaneous pronation of the forearm. If the appropriate Baumann’s angle is not achieved, the reduction maneuver is repeated with extra valgus pressure. If the vascular injury is not improved after the initial closed reduction and splinting, the open method must be considered as well, especially in case of open fractures, severe elbow inflammation, and vascular injury (1, 14-16). Gartland type III fractures are susceptible to neurovascular injuries. The preferred treatment for this type of fracture is the open/closed reduction and pinning method, which has fewer complications than reduction and splinting.
3.2. Indication for surgery in supracondylar humerus fractures
Surgical treatment is indicated in supracondylar humerus fractures for the following cases: 1. Closed reduction is not possible; 2. The fracture is unstable after reduction, and reduction cannot be maintained; 3. In case of neural injury during or following reduction; 4. If vascular exploration is required; 5. In open fractures; 6. In all Gartland type II or III fractures which need an over 90° of flexion to maintain reduction; 7. In all Gartland type IV fractures; 8. For polytraumatized patients with another ipsilateral fracture (17).
3.3. Classification of supracondylar humerus fractures
There are various classifications for these fractures: a) Displaced or non-displaced; b) Open or closed; c) Complicated or uncomplicated (with or without neural/vascular involvement; d) Extension type (95%) or flexion type (5%); and e) Gartland classification system which is based on lateral radiographs; it is mostly used for extension-type fractures and can serve as a guide for the treatment method (14, 18).
Patients who suffer from AIN syndrome are typically unable to form an “O” by using the index finger and thumb because of paralysis of the flexor pollicis longus and flexor digitorum profundus (impaired flexion of the interphalangeal joint of the thumb and the distal interphalangeal joint of the index finger). For example, the patients will lose the ability to button their shirts or turn on their car keys to start it. On physical examination, the Pinch Grip test shows a positive result for patients who are unable to demonstrate the “OK” sign; instead they clamp the sheet between an extended thumb and index finger (19).
For the surgeon, the most concerning issue in the humeral supracondylar fracture is a vascular state, so there may not be any specific test for flexion of the terminal phalanges of thumb and index. So it can be missed easily. Furthermore, AIN is a motor nerve without a sensory task, so the lack of sensory loss does not exist to help diagnosis. Usually, median nerve and AIN are examined by finger flexion, but children deceive examiner by using the third finger to flex the second finger (18).
In all our cases, complete nerve palsy recovery was observed within 3 to 5 weeks. In past studies, complete AIN palsy recovery was observed after 4 to 17 weeks. The neurophysiological and electromyographic examination should be performed after 4 months of conservative treatment without any recovery (8).
The clinical findings of AIN syndrome are composed of lack of flexion of the terminal interphalangeal joint of the thumb and the distal interphalangeal joint of the index finger. The pinch position can only be accomplished with the terminal phalanges of these fingers hyperextended. Pathological spontaneous activity in the affected muscles can be manifested by the electromyographic examination, positive sharp waves, and fibrillation that show denervation (20-22).
Complete AIN palsy recovery was observed after 4 to 17 weeks. Electromyographic examination should be performed after 4 months of conservative treatment without any recovery (23).
According to the just motor (no sensory) function of AIN and also deceiving children using the third finger to flex the second one, underestimation of AIN syndrome in supracondylar fracture of the humerus can be expected. So, the physician should be more careful about physical examination (OK sign) in supracondylar fracture of humerus besides the vascular state.
Ethical Considerations
Compliance with ethical guidelines
This study is just a case report for the diagnostic methods and treatments and all procedures are performed according to the standard protocols.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgements
The authors would like to express their thanks to the Department of Orthopedic Surgery of Imam Khomeini Hospital and Student Research Committee of Mazandaran University of Medical Sciences to support this research.
References
- Kwok IH, Silk ZM, Quick TJ, Sinisi M, MacQuillan A, Fox M. Nerve injuries associated with supracondylar fractures of the humerus in children: Our experience in a specialist peripheral nerve injury unit. The Bone & Joint Journal. 2016; 98(6):851-6. [DOI:10.1302/0301-620X.98B6.35686]
- Babal JC, Mehlman CT, Klein G. Nerve injuries associated with pediatric supracondylar humeral fractures: A meta-analysis. Journal of Pediatric Orthopedics. 2010; 30(3):253-63. [PMID] [DOI:10.1097/BPO.0b013e3181d213a6]
- Herring JA. Tachdjian's pediatric orthopaedics E-Book: From the Texas Scottish Rite Hospital for children. New York: Elsevier Health Sciences; 2013.
- Flynn JM, Skaggs DL, Waters PM. Rockwood and Wilkins' fractures in children. Philadelphia: Lippincott Williams & Wilkins; 2014.
- Cheng JC, Lam TP, Maffulli N. Epidemiological features of supracondylar fractures of the humerus in Chinese children. Journal of Pediatric Orthopedics; Part B. 2001; 10(1):63-7. [DOI:10.1097/00009957-200101000-00011]
- Culp RW, Osterman A, Davidson R, Skirven T, Bora F. Neural injuries associated with supracondylar fractures of the humerus in children. The Journal of Bone and Joint Surgery; American Volume. 1990; 72(8):1211-5. [DOI:10.2106/00004623-199072080-00013]
- Cramer KE, Green NE, Devito DP. Incidence of anterior interosseous nerve palsy in supracondylar humerus fractures in children. Journal of Pediatric Orthopedics. 1993; 13(4):502-5. [DOI:10.1097/01241398-199307000-00015]
- Otsuka NY, Kasser JR. Supracondylar fractures of the humerus in children. Journal of the American Academy of Orthopaedic Surgeons. 1997; 5(1):19-26. [DOI:10.5435/00124635-199701000-00003]]
- Ramachandran M, Birch R, Eastwood DM. Clinical outcome of nerve injuries associated with supracondylar fractures of the humerus in children: The experience of a specialist referral centre. The Journal of Bone and Joint Surgery; British Volume. 2006; 88(1):90-4. [PMID] [DOI:10.1302/0301-620X.88B1.16869]
- Dormans JP, Squillante R, Sharf H. Acute neurovascular complications with supracondylar humerus fractures in children. The Journal of Hand Surgery. 1995; 20(1):1-4. [DOI:10.1016/S0363-5023(05)80046-2]
- Pongowski B, Panasiuk M. Anterior interosseous nerve palsy after supracondylar fracture of humerus in adult: Case report. Ortopedia, Traumatologia, Rehabilitacja. 2013; 15(4):363-8. [PMID] [DOI:10.5604/15093492.1073836]
- Kajiwara R, Matsuno T, Ishida O, Sunagawa T, Suzuki O, Ochi M. Anterior interosseous nerve palsy after reduction and percutaneous pinning of open fractures of the radius and ulna. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery. 2004; 38(6):373-5. [PMID] [DOI:10.1080/02844310410034321]
- Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. The Journal of Bone and Joint Surgery American volume. 2008; 90(5):1121-32. [PMID] [DOI:10.2106/JBJS.G.01354]
- Kumar V, Singh A. Fracture Supracondylar Humerus: A Review. Journal of Clinical and Diagnostic Research. 2016; 10(12):RE01. [DOI:10.7860/JCDR/2016/21647.8942]
- Deslivia MF, Lee HJ, Lee SM, Zhu B, Jeon IH. Anterior interosseous nerve syndrome after shoulder arthroscopy: Report of 3 cases. Journal of Shoulder and Elbow Surgery. 2016; 25(11):e348-52. [PMID] [DOI:10.1016/j.jse.2016.07.028]
- Aljawder A, Faqi MK, Mohamed A, Alkhalifa F. Anterior interosseous nerve syndrome diagnosis and intraoperative findings: A case report. International Journal of Surgery Case Reports. 2016; 21:44-7. [PMID] [PMCID] [DOI:10.1016/j.ijscr.2016.02.021]
- Shaw BA, Kasser JR, Emans JB, Rand FF. Management of vascular injuries in displaced supracondylar humerus fractures without arteriography. Journal of Orthopaedic Trauma. 1990; 4(1):25-9. [PMID] [DOI:10.1097/00005131-199003000-00004]
- Barton KL, Kaminsky CK, Green DW, Shean CJ, Kautz SM, Skaggs DL. Reliability of a modified Gartland classification of supracondylar humerus fractures. Journal of Pediatric Orthopaedics. 2001; 21(1):27-30. [PMID] [DOI:10.1097/00004694-200101000-00007]
- Berger R.A. Hand Surgery. Philadelphia: Lippincott Williams & Wilkins, 2004.
- Farber JS, Bryan CR. The anterior interosseous nerve syndrome. Journal of Bone and Joint Surgery. 1968; 50(3):521-3. [DOI:10.2106/00004623-196850030-00011]
- Lake PA. Anterior interosseous nerve syndrome. Journal of Neurosurgery. 1974; 41(3):306-9. [PMID] [DOI:10.3171/jns.1974.41.3.0306]
- Lipscomb PR, Burleson RJ. Vascular and neural complications in supracondylar fractures of the humerus in children. The Journal of Bone and Joint Surgery; American Volume. 1955; 37(3):487-92. [DOI:10.2106/00004623-195537030-00004]
- Joist A, Joosten U, Wetterkamp D, Neuber M, Probst A, Rieger H. Anterior interosseous nerve compression after supracondylar fracture of the humerus: A metaanalysis. Journal of Neurosurgery. 1999; 90(6):1053-6. [PMID] [DOI:10.3171/jns.1999.90.6.1053]
Type of Study: Case & Review |
Received: 2017/04/19 | Accepted: 2018/03/3 | Published: 2019/01/1
Received: 2017/04/19 | Accepted: 2018/03/3 | Published: 2019/01/1
References
1. Kwok IH, Silk ZM, Quick TJ, Sinisi M, MacQuillan A, Fox M. Nerve injuries associated with supracondylar fractures of the humerus in children: Our experience in a specialist peripheral nerve injury unit. The Bone & Joint Journal. 2016; 98(6):851-6. [DOI:10.1302/0301-620X.98B6.35686] [DOI:10.1302/0301-620X.98B6.35686]
2. Babal JC, Mehlman CT, Klein G. Nerve injuries associated with pediatric supracondylar humeral fractures: A meta-analysis. Journal of Pediatric Orthopedics. 2010; 30(3):253-63. [PMID] [DOI:10.1097/BPO.0b013e3181d213a6] [DOI:10.1097/BPO.0b013e3181d213a6]
3. Herring JA. Tachdjian's pediatric orthopaedics E-Book: From the Texas Scottish Rite Hospital for children. New York: Elsevier Health Sciences; 2013.
4. Flynn JM, Skaggs DL, Waters PM. Rockwood and Wilkins' fractures in children. Philadelphia: Lippincott Williams & Wilkins; 2014.
5. Cheng JC, Lam TP, Maffulli N. Epidemiological features of supracondylar fractures of the humerus in Chinese children. Journal of Pediatric Orthopedics; Part B. 2001; 10(1):63-7. [DOI:10.1097/00009957-200101000-00011] [DOI:10.1097/00009957-200101000-00011]
6. Culp RW, Osterman A, Davidson R, Skirven T, Bora F. Neural injuries associated with supracondylar fractures of the humerus in children. The Journal of Bone and Joint Surgery; American Volume. 1990; 72(8):1211-5. [DOI:10.2106/00004623-199072080-00013] [DOI:10.2106/00004623-199072080-00013]
7. Cramer KE, Green NE, Devito DP. Incidence of anterior interosseous nerve palsy in supracondylar humerus fractures in children. Journal of Pediatric Orthopedics. 1993; 13(4):502-5. [DOI:10.1097/01241398-199307000-00015] [DOI:10.1097/01241398-199307000-00015]
8. Otsuka NY, Kasser JR. Supracondylar fractures of the humerus in children. Journal of the American Academy of Orthopaedic Surgeons. 1997; 5(1):19-26. [DOI:10.5435/00124635-199701000-00003]] [DOI:10.5435/00124635-199701000-00003]
9. Ramachandran M, Birch R, Eastwood DM. Clinical outcome of nerve injuries associated with supracondylar fractures of the humerus in children: The experience of a specialist referral centre. The Journal of Bone and Joint Surgery; British Volume. 2006; 88(1):90-4. [PMID] [DOI:10.1302/0301-620X.88B1.16869] [DOI:10.1302/0301-620X.88B1.16869]
10. Dormans JP, Squillante R, Sharf H. Acute neurovascular complications with supracondylar humerus fractures in children. The Journal of Hand Surgery. 1995; 20(1):1-4. [DOI:10.1016/S0363-5023(05)80046-2] [DOI:10.1016/S0363-5023(05)80046-2]
11. Pongowski B, Panasiuk M. Anterior interosseous nerve palsy after supracondylar fracture of humerus in adult: Case report. Ortopedia, Traumatologia, Rehabilitacja. 2013; 15(4):363-8. [PMID] [DOI:10.5604/15093492.1073836] [DOI:10.5604/15093492.1073836]
12. Kajiwara R, Matsuno T, Ishida O, Sunagawa T, Suzuki O, Ochi M. Anterior interosseous nerve palsy after reduction and percutaneous pinning of open fractures of the radius and ulna. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery. 2004; 38(6):373-5. [PMID] [DOI:10.1080/02844310410034321] [DOI:10.1080/02844310410034321]
13. Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. The Journal of Bone and Joint Surgery American volume. 2008; 90(5):1121-32. [PMID] [DOI:10.2106/JBJS.G.01354] [DOI:10.2106/JBJS.G.01354]
14. Kumar V, Singh A. Fracture Supracondylar Humerus: A Review. Journal of Clinical and Diagnostic Research. 2016; 10(12):RE01. [DOI:10.7860/JCDR/2016/21647.8942] [DOI:10.7860/JCDR/2016/21647.8942]
15. Deslivia MF, Lee HJ, Lee SM, Zhu B, Jeon IH. Anterior interosseous nerve syndrome after shoulder arthroscopy: Report of 3 cases. Journal of Shoulder and Elbow Surgery. 2016; 25(11):e348-52. [PMID] [DOI:10.1016/j.jse.2016.07.028] [DOI:10.1016/j.jse.2016.07.028]
16. Aljawder A, Faqi MK, Mohamed A, Alkhalifa F. Anterior interosseous nerve syndrome diagnosis and intraoperative findings: A case report. International Journal of Surgery Case Reports. 2016; 21:44-7. [PMID] [PMCID] [DOI:10.1016/j.ijscr.2016.02.021] [DOI:10.1016/j.ijscr.2016.02.021]
17. Shaw BA, Kasser JR, Emans JB, Rand FF. Management of vascular injuries in displaced supracondylar humerus fractures without arteriography. Journal of Orthopaedic Trauma. 1990; 4(1):25-9. [PMID] [DOI:10.1097/00005131-199003000-00004] [DOI:10.1097/00005131-199003000-00004]
18. Barton KL, Kaminsky CK, Green DW, Shean CJ, Kautz SM, Skaggs DL. Reliability of a modified Gartland classification of supracondylar humerus fractures. Journal of Pediatric Orthopaedics. 2001; 21(1):27-30. [PMID] [DOI:10.1097/00004694-200101000-00007] [DOI:10.1097/00004694-200101000-00007]
19. Berger R.A. Hand Surgery. Philadelphia: Lippincott Williams & Wilkins, 2004.
20. Farber JS, Bryan CR. The anterior interosseous nerve syndrome. Journal of Bone and Joint Surgery. 1968; 50(3):521-3. [DOI:10.2106/00004623-196850030-00011] [DOI:10.2106/00004623-196850030-00011]
21. Lake PA. Anterior interosseous nerve syndrome. Journal of Neurosurgery. 1974; 41(3):306-9. [PMID] [DOI:10.3171/jns.1974.41.3.0306] [DOI:10.3171/jns.1974.41.3.0306]
22. Lipscomb PR, Burleson RJ. Vascular and neural complications in supracondylar fractures of the humerus in children. The Journal of Bone and Joint Surgery; American Volume. 1955; 37(3):487-92. [DOI:10.2106/00004623-195537030-00004] [DOI:10.2106/00004623-195537030-00004]
23. Joist A, Joosten U, Wetterkamp D, Neuber M, Probst A, Rieger H. Anterior interosseous nerve compression after supracondylar fracture of the humerus: A metaanalysis. Journal of Neurosurgery. 1999; 90(6):1053-6. [PMID] [DOI:10.3171/jns.1999.90.6.1053] [DOI:10.3171/jns.1999.90.6.1053]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |