Volume 7, Issue 2 (4-2019)
J. Pediatr. Rev 2019, 7(2): 89-98 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hendinezhad M A, Babaei A, Gholipour Baradari A, Zamani A. Comparing Supraglottic Airway Devices for Airway Management During Surgery in Children: A Review of Literature. J. Pediatr. Rev 2019; 7 (2) :89-98
URL: http://jpr.mazums.ac.ir/article-1-176-en.html
URL: http://jpr.mazums.ac.ir/article-1-176-en.html
1- Department of Anesthesiology, Nimeshaban Hospital, Mazandaran University of Medical Sciences, Sari, Iran.
2- Department of Anesthesiology, Emam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran. ,Babaeianahita112@gmail.com
3- Department of Anesthesiology, Emam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran.
2- Department of Anesthesiology, Emam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran. ,
3- Department of Anesthesiology, Emam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran.
Keywords: Supraglottic airway device, Children, Fiberoptic Bronchoscopic View (FBV), Oropharyngeal Leakage Pressure (OLP)
Full-Text [PDF 572 kb]
(3919 Downloads)
| Abstract (HTML) (7874 Views)
Full-Text: (4219 Views)
1. Context
Supraglottic Airway Devices (SADs) are widely used for airway management (1). Children who undergo surgeries benefit most from the use of SADs. A variety of SGAs are used for the management of a difficult airway as well as a conduit for tracheal intubation in children (2). Advantages of endotracheal intubation assisted by SADs such as effortless insertion, improved alignment of the glottic opening, and continuous patient oxygenation and ventilation, have been well documented. In addition, hemodynamic stress response to intubation by SADs is less than the conventional methods (3). Such devices could be an excellent alternative for patients with previous history of difficult intubation, limited neck movement, and unstable cervical spine (4). Moreover, SADs facilitate overcoming upper airway obstruction and provide a hands-free airway support with a relatively straightforward path to the larynx (5). However, despite all evidence, choosing the optimal SAD is not a simple decision.
2. Objective
The present review study aimed to examine the literature regarding pediatric SADs, to draw recommendations for future investigations and integrate the evidence.
3. Data Sources
The following steps were taken to thoroughly review the relevant literature. We conducted an electronic search was conducted on MEDLINE, Embase, CINAHL and PubMed databases. We also searched the Cochrane database (CENTRAL), and Web of Science up to July 1, 2017.
4. Study Selection
Studies on subgroups like those comparing devices in children and reports of their usage were included. The keywords used for the search strategy were “supraglottic device”, “supraglottic airway device”, “laryngeal mask”, “children”, “child,” and “pediatric”. A review of reference lists of articles was performed to identify further references. Two authors independently scanned the titles and abstracts identified by the above-mentioned search strategies. All randomized trials comparing any types of supraglottic airway devices in children were included. Similarly, cost-effectiveness analysis and case reports of rare complications in the emergency ward were also included in this review to consider every chance of adverse effects for clinicians.
5. Data Extraction
Of 112 potential studies, 53 full texts of papers were accessible. Initially, the full text versions of potentially eligible studies selected by at least one reviewer were assessed. Any disagreement was resolved through discussion. Papers in English were considered eligible. Then, the extracted data were sorted into prepared data extraction tables. We extracted such data as patients’ frequency, type of Laryngeal Mask Airway (LMA), study design and predominant findings. Finally, a structured narrative summary of the studies was conducted using 30 papers related to the supraglottic devices for children.
6. Results
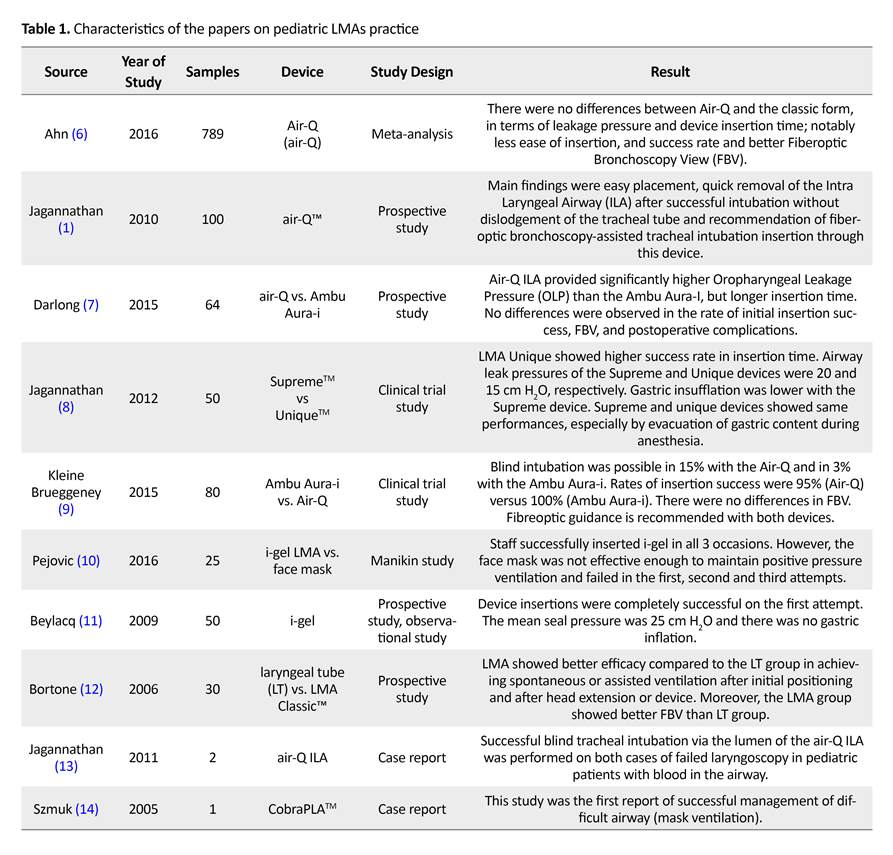
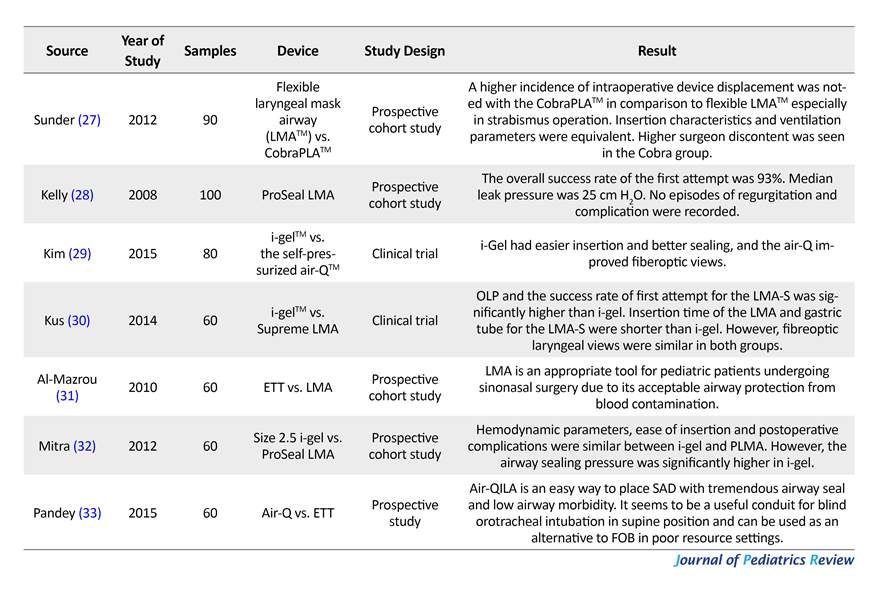
A comprehensive search was conducted. The following SADs were included in the review: LMA Classic, LMA ProSealTM, LMA Supreme, LMA FlexibleTM, LMA Unique, i-gel, Laryngeal TubeTM, self-pressurized air-QTM, Cobra perilaryngeal airwayTM, and Ambu Aura-iTM. In total, 30 papers related to supraglottic devices for children were identified. These qualitative studies were conducted in various settings, including accident and emergency department or operating rooms. A review of recent literature is presented in Table 1 and further discussed in the article.
A brief review of the recent literature indicate that SADs such as the i-gel, LMA ProSeal and Cobra perilaryngeal airway demonstrate higher OLP in most studies focusing on OLP. Evidence also revealed that the risk of device failure may be lower with LMA ProSeal, LMA-Classic and LMA-Unique (34-36), but higher with i-gel (37, 38). Moreover, the risk of blood staining of the device was greatly lower with i-gel compared to LMA-Classic and LMA ProSeal. In summary, the LMA ProSeal seems to be the best supraglottic airway device for children because of its high OLP and low risk of insertion failure. Also, i-gel appears to be a very functional tool.
6.1. Outcome measures for rating success in LMA insertion
6.1.1. Cuff pressure
When the supraglottic cuff pressure is more than the mucosal perfusion pressure, postoperative pharyngolaryngeal symptoms such as a sore throat (dysphagia or dysphonia) or local mucosal trauma and nerve injuries are expected (39). SGAs with inflatable cuffs are prone to over inflation and may cause pressures higher than 60 cm H2O (40). Elevated pressures do not provide better seal, and are conversely liable to cause more morbidity (41, 42).
6.1.2. Oropharyngeal Seal Pressure (OSP)
An effective glottic seal is necessary for efficient ventilation. Moreover, an appropriate seal facilitates the maintenance of preferred anaesthetic depth without polluting the environment with the leaked gases. It also decreases leak into the esophagus, preventing rise in intragastric pressure and the risk of regurgitation (43).
6.1.3. Fiberoptic view through a supraglottic device
Most studies have correlated the Fiberoptic BronchosCopy (FOB) view through the SGA with the ease of intubation and ventilation (36). However, the FOB scoring is challenged, as a dependable tool for SGA positioning (17) (Figure 1). The usage of fiberoptic score was suggested by Cook and Cranshaw (44). Left to right view: View I (I = ideal), View H (H: too high), and View L (L: too low), respectively; Arrow: lingual tonsils. Further evidence about FOB in different studies are demonstrated in Table 1 A full glottic view (although it seems unnecessary) is recommended for primary ventilation, to avoid possible trauma.
6.1.4. Problems and failures
Airway obstruction can arise due to malposition, obstruction by the epiglottis, laryngospasm, biting, or kinking of the tube. Light plane of anesthesia can also lead to laryngospasm and airway obstruction in children (37). Lingual edema and aspiration of stomach contents are other potential complications. The younger and smaller the child, the higher the risk of developing problems in this area (25, 30). Higher experience significantly decreases such problems (18).
7. Discussion
The main findings of the current study were as follows: i-gel, LMA ProSeal, and Cobra perilaryngeal airway had a higher OLP than the other devices; the risk of device failure may be lower with LMA-ProSeal, LMA-Classic, and LMA-Unique (34, 35), but higher with i-gel (37, 38). On the other hand, most studies demonstrated that the risk of blood staining device was considerably lower with using i-gel, compared to the LMA-Classic and LMA-ProSeal (40). However, high quality randomized trials are required to confirm the results regarding laryngeal tube.
Supraglottic Airway Devices (SADs) are widely used for airway management (1). Children who undergo surgeries benefit most from the use of SADs. A variety of SGAs are used for the management of a difficult airway as well as a conduit for tracheal intubation in children (2). Advantages of endotracheal intubation assisted by SADs such as effortless insertion, improved alignment of the glottic opening, and continuous patient oxygenation and ventilation, have been well documented. In addition, hemodynamic stress response to intubation by SADs is less than the conventional methods (3). Such devices could be an excellent alternative for patients with previous history of difficult intubation, limited neck movement, and unstable cervical spine (4). Moreover, SADs facilitate overcoming upper airway obstruction and provide a hands-free airway support with a relatively straightforward path to the larynx (5). However, despite all evidence, choosing the optimal SAD is not a simple decision.
2. Objective
The present review study aimed to examine the literature regarding pediatric SADs, to draw recommendations for future investigations and integrate the evidence.
3. Data Sources
The following steps were taken to thoroughly review the relevant literature. We conducted an electronic search was conducted on MEDLINE, Embase, CINAHL and PubMed databases. We also searched the Cochrane database (CENTRAL), and Web of Science up to July 1, 2017.
4. Study Selection
Studies on subgroups like those comparing devices in children and reports of their usage were included. The keywords used for the search strategy were “supraglottic device”, “supraglottic airway device”, “laryngeal mask”, “children”, “child,” and “pediatric”. A review of reference lists of articles was performed to identify further references. Two authors independently scanned the titles and abstracts identified by the above-mentioned search strategies. All randomized trials comparing any types of supraglottic airway devices in children were included. Similarly, cost-effectiveness analysis and case reports of rare complications in the emergency ward were also included in this review to consider every chance of adverse effects for clinicians.
5. Data Extraction
Of 112 potential studies, 53 full texts of papers were accessible. Initially, the full text versions of potentially eligible studies selected by at least one reviewer were assessed. Any disagreement was resolved through discussion. Papers in English were considered eligible. Then, the extracted data were sorted into prepared data extraction tables. We extracted such data as patients’ frequency, type of Laryngeal Mask Airway (LMA), study design and predominant findings. Finally, a structured narrative summary of the studies was conducted using 30 papers related to the supraglottic devices for children.
6. Results
A comprehensive search was conducted. The following SADs were included in the review: LMA Classic, LMA ProSealTM, LMA Supreme, LMA FlexibleTM, LMA Unique, i-gel, Laryngeal TubeTM, self-pressurized air-QTM, Cobra perilaryngeal airwayTM, and Ambu Aura-iTM. In total, 30 papers related to supraglottic devices for children were identified. These qualitative studies were conducted in various settings, including accident and emergency department or operating rooms. A review of recent literature is presented in Table 1 and further discussed in the article.
A brief review of the recent literature indicate that SADs such as the i-gel, LMA ProSeal and Cobra perilaryngeal airway demonstrate higher OLP in most studies focusing on OLP. Evidence also revealed that the risk of device failure may be lower with LMA ProSeal, LMA-Classic and LMA-Unique (34-36), but higher with i-gel (37, 38). Moreover, the risk of blood staining of the device was greatly lower with i-gel compared to LMA-Classic and LMA ProSeal. In summary, the LMA ProSeal seems to be the best supraglottic airway device for children because of its high OLP and low risk of insertion failure. Also, i-gel appears to be a very functional tool.
6.1. Outcome measures for rating success in LMA insertion
6.1.1. Cuff pressure
When the supraglottic cuff pressure is more than the mucosal perfusion pressure, postoperative pharyngolaryngeal symptoms such as a sore throat (dysphagia or dysphonia) or local mucosal trauma and nerve injuries are expected (39). SGAs with inflatable cuffs are prone to over inflation and may cause pressures higher than 60 cm H2O (40). Elevated pressures do not provide better seal, and are conversely liable to cause more morbidity (41, 42).
6.1.2. Oropharyngeal Seal Pressure (OSP)
An effective glottic seal is necessary for efficient ventilation. Moreover, an appropriate seal facilitates the maintenance of preferred anaesthetic depth without polluting the environment with the leaked gases. It also decreases leak into the esophagus, preventing rise in intragastric pressure and the risk of regurgitation (43).
6.1.3. Fiberoptic view through a supraglottic device
Most studies have correlated the Fiberoptic BronchosCopy (FOB) view through the SGA with the ease of intubation and ventilation (36). However, the FOB scoring is challenged, as a dependable tool for SGA positioning (17) (Figure 1). The usage of fiberoptic score was suggested by Cook and Cranshaw (44). Left to right view: View I (I = ideal), View H (H: too high), and View L (L: too low), respectively; Arrow: lingual tonsils. Further evidence about FOB in different studies are demonstrated in Table 1 A full glottic view (although it seems unnecessary) is recommended for primary ventilation, to avoid possible trauma.
6.1.4. Problems and failures
Airway obstruction can arise due to malposition, obstruction by the epiglottis, laryngospasm, biting, or kinking of the tube. Light plane of anesthesia can also lead to laryngospasm and airway obstruction in children (37). Lingual edema and aspiration of stomach contents are other potential complications. The younger and smaller the child, the higher the risk of developing problems in this area (25, 30). Higher experience significantly decreases such problems (18).
7. Discussion
The main findings of the current study were as follows: i-gel, LMA ProSeal, and Cobra perilaryngeal airway had a higher OLP than the other devices; the risk of device failure may be lower with LMA-ProSeal, LMA-Classic, and LMA-Unique (34, 35), but higher with i-gel (37, 38). On the other hand, most studies demonstrated that the risk of blood staining device was considerably lower with using i-gel, compared to the LMA-Classic and LMA-ProSeal (40). However, high quality randomized trials are required to confirm the results regarding laryngeal tube.
A variety of modern SGAs for using in children have emerged. It is important to introduce those into practice and assess the potential advantages and disadvantages of each device through clinical evaluations. Table 1 summarizes the discussed SGAs and outlined potential areas of concern. Despite the variety of modern devices, the cLMA, ProSeal, and Unique are still the best devices in pediatric use for different conditions. The cLMA has been the standard SGA for many years. However, many other first generation devices have been available in small sizes with further features and better performance, since 2003 (18, 30, 45). For example, Cobra PLA was designed to be placed in the hypopharynx and composed of a breathing tube with a wide distal end and a number of slots or bars (46).
A cuff is attached proximal to the wide part, and serves to seal off the distal end from the upper airway when it is inflated and a softened ‘tongue’, which bends for better passage (16). Variations of LMAs like ProSeal, Unique, Supreme, and iLMA have been marketed in practice and discussed in the literature (47). The i-gel is rather an exceptional SAD with a gel-like thermoplastic and a non-inflatable cuff (48) which achieves an effective perilaryngeal
A cuff is attached proximal to the wide part, and serves to seal off the distal end from the upper airway when it is inflated and a softened ‘tongue’, which bends for better passage (16). Variations of LMAs like ProSeal, Unique, Supreme, and iLMA have been marketed in practice and discussed in the literature (47). The i-gel is rather an exceptional SAD with a gel-like thermoplastic and a non-inflatable cuff (48) which achieves an effective perilaryngeal
seal because of its feasibility to shape patient’s airway structure (20). In addition, the device is equipped with a bite block and a buccal cavity stabilizer that stop the device malrotation and a gastric channel (22).
The recent studies demonstrated the efficacy and safety of the device, for example, Pejovic in a manikin study, compared i-gel with face mask and reported that the i-gel accomplished a 100% success rate on all occasions by trainees (10). Yeoh, et al. also reported the advantages of size 2 i‑gel™ in children in terms of ease of insertion and low number of attempts on insertion (19). Novel design of i-gel made it a suitable tool with an appropriate OLP and low risk of complication.
LMA Supreme is similar to LMA ProSeal except its single usage and its introducer shaft features. Various studies have declared acceptable airway characteristics of LMA supreme to apply in children (20, 22, 35, 36). Jagannathan et al. (49) and Francksen et al. found it comparable with the LMA ProSeal and i-gel, respectively and recommended it as a useful alternative to ProSeal LMA (50). A prospective cohort study by Gaitini et al. compared the Supreme size II with LMA ProSeal and found it similarly effective on higher oropharyngeal seal pressure during spontaneous ventilation in children (51) that make it an optimal tool in difficult or emergency airway management.
The air-Q™ LMA is also a modern SAD that allows passage of cuffed tracheal tubes and has the option of successive removal. In addition, the airway tube is broader, more rigid, and curved. Air-Q features facilitate the use of ILA as a conduit for tracheal intubation (23). Finally, the Ambu Aura-i is easy to insert and provides equal or better OSP than CLMA and Unique, respectively, in adults (52, 53). It is also a suitable tool for blind endotracheal intubation (44). Therefore, it has become a frequently used device for various short surgical procedures, even in children. These devices are definitely appropriate to apply on children undergoing many surgical procedures. Further research is required to investigate the most appropriate supraglottic airway devices in diverse clinical situations and various conditions among children.
8. Conclusions
The LMA ProSeal and i-gel may be the best optimal supraglottic airway devices for children due to their unique features. However, there is little knowledge in this regard and more research studies must be conducted to recognize the most appropriate supraglottic airway devices in diverse clinical situations and various conditions in children.
Ethical Considerations
Compliance with ethical guidelines
There is no ethical principle to be considered doing this research.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
The authors contributions is as follows: Investigation, writing review and edit: Mir Ahmad Hendinezhad, Anahita Babaei; and Supervision: Afshin Gholipour Baradari.
Conflict of interest
The authors declare no conflict of interest.
References
The recent studies demonstrated the efficacy and safety of the device, for example, Pejovic in a manikin study, compared i-gel with face mask and reported that the i-gel accomplished a 100% success rate on all occasions by trainees (10). Yeoh, et al. also reported the advantages of size 2 i‑gel™ in children in terms of ease of insertion and low number of attempts on insertion (19). Novel design of i-gel made it a suitable tool with an appropriate OLP and low risk of complication.
LMA Supreme is similar to LMA ProSeal except its single usage and its introducer shaft features. Various studies have declared acceptable airway characteristics of LMA supreme to apply in children (20, 22, 35, 36). Jagannathan et al. (49) and Francksen et al. found it comparable with the LMA ProSeal and i-gel, respectively and recommended it as a useful alternative to ProSeal LMA (50). A prospective cohort study by Gaitini et al. compared the Supreme size II with LMA ProSeal and found it similarly effective on higher oropharyngeal seal pressure during spontaneous ventilation in children (51) that make it an optimal tool in difficult or emergency airway management.
The air-Q™ LMA is also a modern SAD that allows passage of cuffed tracheal tubes and has the option of successive removal. In addition, the airway tube is broader, more rigid, and curved. Air-Q features facilitate the use of ILA as a conduit for tracheal intubation (23). Finally, the Ambu Aura-i is easy to insert and provides equal or better OSP than CLMA and Unique, respectively, in adults (52, 53). It is also a suitable tool for blind endotracheal intubation (44). Therefore, it has become a frequently used device for various short surgical procedures, even in children. These devices are definitely appropriate to apply on children undergoing many surgical procedures. Further research is required to investigate the most appropriate supraglottic airway devices in diverse clinical situations and various conditions among children.
8. Conclusions
The LMA ProSeal and i-gel may be the best optimal supraglottic airway devices for children due to their unique features. However, there is little knowledge in this regard and more research studies must be conducted to recognize the most appropriate supraglottic airway devices in diverse clinical situations and various conditions in children.
Ethical Considerations
Compliance with ethical guidelines
There is no ethical principle to be considered doing this research.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
The authors contributions is as follows: Investigation, writing review and edit: Mir Ahmad Hendinezhad, Anahita Babaei; and Supervision: Afshin Gholipour Baradari.
Conflict of interest
The authors declare no conflict of interest.
References
- Jagannathan N, Kozlowski RJ, Sohn LE, Langen KE, Roth AG, Mukherji II, et al. A clinical evaluation of the intubating laryngeal airway as a conduit for tracheal intubation in children. Anesthesia & Analgesia. 2011; 112(1):176-82. [DOI:10.1213/ANE.0b013e3181fe0408] [PMID]
- Henderson J, Popat M, Latto I, Pearce A. Difficult airway society guidelines for management of the unanticipated difficult intubation. Anaesthesia. 2004; 59(7):675-94. [DOI:10.1111/j.1365-2044.2004.03831.x] [PMID]
- Samir EM, Sakr SA. The air-Q as a conduit for fiberoptic aided tracheal intubation in adult patients undergoing cervical spine fixation: A prospective randomized study. Egyptian Journal of Anaesthesia. 2012; 28(2):133-7. [DOI:10.1016/j.egja.2011.12.002]
- Raw D, Beattie J, Hunter J. Anaesthesia for spinal surgery in adults. British Journal of Anaesthesia. 2003; 91(6):886-904. [DOI:10.1093/bja/aeg253] [PMID]
- Brooks P, Ree R, Rosen D, Ansermino M. Canadian pediatric anesthesiologists prefer inhalational anesthesia to manage difficult airways: A survey. Canadian Journal of Anesthesia. 2005; 52(3):285-90. [DOI:10.1007/BF03016065] [PMID]
- Ahn EJ, Choi GJ, Kang H, Baek CW, Jung YH, Woo YC, et al. Comparative efficacy of the air-Q intubating laryngeal airway during general anesthesia in pediatric patients: A systematic review and meta-analysis. BioMed Research International. 2016; 2016:6406391.
- Darlong V, Biyani G, Baidya DK, Pandey R, Punj J, Upadhyay AD. Comparison of air‐Q and Ambu Aura‐i for controlled ventilation in infants: A randomized controlled trial. Pediatric Anesthesia. 2015; 25(8):795-800. [DOI:10.1111/pan.12663] [PMID]
- Jagannathan N, Sohn L, Sawardekar A, Chang E, Langen K, Anderson K. A randomised trial comparing the laryngeal mask airway Supreme™ with the laryngeal mask airway Unique™ in children. Anaesthesia. 2012; 67(2):139-44. [DOI:10.1111/j.1365-2044.2011.06960.x] [PMID]
- Kleine Brueggeney M, Nicolet A, Nabecker S, Seiler S, Stucki F, Greif R, et al. Blind intubation of anaesthetised children with supraglottic airway devices AmbuAura-i and Air-Q cannot be recommended: A randomised controlled trial. European Journal of Anaesthesiology. 2015; 32(9):631-9. [DOI:10.1097/EJA.0000000000000261] [PMID]
- Pejovic NJ, Trevisanuto D, Nankunda J, Tylleskär T. Pilot manikin study showed that a supraglottic airway device improved simulated neonatal ventilation in a low‐resource setting. Acta Paediatrica. 2016; 105(12):1440-3. [DOI:10.1111/apa.13565] [PMID] [PMCID]
- Beylacq L, Bordes M, Semjen F, Cros AM. The I‐gel®, a single‐use supraglottic airway device with a non‐inflatable cuff and an esophageal vent: An observational study in children. Acta Anaesthesiologica Scandinavica. 2009; 53(3):376-9. [DOI:10.1111/j.1399-6576.2008.01869.x] [PMID]
- Bortone L, Ingelmo PM, Ninno GD, Tosi M, Caffini L, Trenchi J, et al. Randomized controlled trial comparing the laryngeal tube and the laryngeal mask in pediatric patients. Pediatric Anesthesia. 2006; 16(3):251-7. [DOI:10.1111/j.1460-9592.2005.01756.x] [PMID]
- Jagannathan N, Wong DT. Successful tracheal intubation through an intubating laryngeal airway in pediatric patients with airway hemorrhage. Journal of Emergency Medicine. 2011; 41(4):369-73. [DOI:10.1016/j.jemermed.2010.05.066] [PMID]
- Szmuk P, Ezri T, Akca O, Alfery D. Use of a new supraglottic airway device-the CobraPLA-in a ‘difficult to intubate/difficult to ventilate’scenario. Acta Anaesthesiologica Scandinavica. 2005; 49(3):421-3. [DOI:10.1111/j.1399-6576.2005.00618.x] [PMID]
- Baker PA, Brunette KE, Byrnes CA, Thompson J. A prospective randomized trial comparing supraglottic airways for flexible bronchoscopy in children. Pediatric Anesthesia. 2010; 20(9):831-8. [DOI:10.1111/j.1460-9592.2010.03362.x] [PMID]
- Gaitini L, Carmi N, Yanovski B, Tome R, Resnikov I, Gankin I, et al. Comparison of the CobraPLATM (Cobra Perilaryngeal Airway) and the laryngeal mask airway UniqueTM in children under pressure controlled ventilation. Pediatric Anesthesia. 2008; 18(4):313-9. [DOI:10.1111/j.1460-9592.2008.02449.x] [PMID]
- Goyal R, Shukla RN, Kumar G. Comparison of size 2 i‐gel supraglottic airway with LMA‐ProSeal™ and LMA‐Classic™ in spontaneously breathing children undergoing elective surgery. Pediatric Anesthesia. 2012; 22(4):355-9. [DOI:10.1111/j.1460-9592.2011.03757.x] [PMID]
- Hughes C, Place K, Berg S, Mason D. A clinical evaluation of the i‐gelTM supraglottic airway device in children. Pediatric Anesthesia. 2012; 22(8):765-71. [DOI:10.1111/j.1460-9592.2012.03893.x] [PMID]
- Yeoh TY, Chan KB, Yeo LS, Liu EH, Pan TL. An evaluation of the I-gel supraglottic airway in 70 pediatric patients. Journal of Anesthesia. 2015; 29(2):295-8. [DOI:10.1007/s00540-014-1915-6] [PMID]
- Jagannathan N, Sommers K, Sohn LE, Sawardekar A, Shah RD, Mukherji II, et al. A randomized equivalence trial comparing the i‐gel and laryngeal mask airway Supreme in children. Pediatric Anesthesia. 2013; 23(2):127-33. [DOI:10.1111/pan.12078] [PMID]
- Nirupa R, Gombar S, Ahuja V, Sharma P. A randomised trial to compare i-gel and ProSeal™ laryngeal mask airway for airway management in paediatric patients. Indian Journal of Anaesthesia. 2016; 60(10):726-31. [DOI:10.4103/0019-5049.191670] [PMID] [PMCID]
- Jagannathan N, Sohn LE, Chang E, Sawardekar A. A cohort evaluation of the Laryngeal Mask Airway‐Supreme™ in children. Pediatric Anesthesia. 2012; 22(8):759-64. [DOI:10.1111/j.1460-9592.2012.03832.x] [PMID]
- Jagannathan N, Roth AG, Sohn LE, Pak TY, Amin S, Suresh S. The new air‐QTM intubating laryngeal airway for tracheal intubation in children with anticipated difficult airway: A case series. Pediatric Anesthesia. 2009; 19(6):618-22. [DOI:10.1111/j.1460-9592.2009.02990.x] [PMID]
- Jagannathan N, Sohn LE, Mankoo R, Langen KE, Roth AG, Hall SC. Prospective evaluation of the self‐pressurized air‐Q intubating laryngeal airway in children. Pediatric Anesthesia. 2011; 21(6):673-80. [DOI:10.1111/j.1460-9592.2011.03576.x] [PMID]
- Jagannathan N, Sohn LE, Sawardekar A, Gordon J, Shah RD, Mukherji II, et al. A randomized trial comparing the Ambu® Aura‐i™ with the air‐Q™ intubating laryngeal airway as conduits for tracheal intubation in children. Pediatric Anesthesia. 2012; 22(12):1197-204. [DOI:10.1111/pan.12024] [PMID]
- Jain D, Ghai B, Bala I, Gandhi K, Banerjee G. Evaluation of I‐gel™ airway in different head and neck positions in anesthetized paralyzed children. Pediatric Anesthesia. 2015; 325(12):1248-53. [DOI:10.1111/pan.12748] [PMID]
- Sunder RA, Sinha R, Agarwal A, Perumal BCS, Paneerselvam SR. Comparison of Cobra Perilaryngeal Airway (CobraPLA™) with flexible laryngeal mask airway in terms of device stability and ventilation characteristics in pediatric ophthalmic surgery. Journal of Anaesthesiology, Clinical Pharmacology. 2012; 28(3):322-5. [DOI:10.4103/0970-9185.98324] [PMID] [PMCID]
- Kelly F, Sale S, Bayley G, Cook T, Stoddart P, White M. A cohort evaluation of the pediatric ProSeal laryngeal mask airway in 100 children. Pediatric Anesthesia. 2008; 18(10):947-51. [DOI:10.1111/j.1460-9592.2008.02705.x] [PMID]
- Kim MS, Lee JH, Han SW, Im YJ, Kang HJ, Lee JR. A randomized comparison of the i‐gel™ with the self‐pressurized air‐Q™ intubating laryngeal airway in children. Pediatric Anesthesia. 2015; 25(4):405-12. [DOI:10.1111/pan.12609] [PMID]
- Kus A, Gok CN, Hosten T, Gurkan Y, Solak M, Toker K. The LMA-Supreme versus the I-gel in simulated difficult airway in children: A randomised study. European Journal of Anaesthesiology. 2014; 31(5):280-4. [DOI:10.1097/EJA.0000000000000062] [PMID]
- Al Mazrou KA, Abdullah KM, ElGammal MS, Ansari RA, Turkistani A, Abdelmeguid ME. Laryngeal mask airway vs. uncuffed endotracheal tube for nasal and paranasal sinus surgery: Paediatric airway protection. European Journal of Anaesthesiology. 2010; 27(1):16-9. [DOI:10.1097/EJA.0b013e32832c5f09] [PMID]
- Mitra S, Das B, Jamil SN. Comparison of size 2.5 i-gel™ with ProSeal LMA™ in anaesthetised, paralyzed children undergoing elective surgery. North American Journal of Medical Sciences. 2012; 4(10):453-7. [DOI:10.4103/1947-2714.101983] [PMID] [PMCID]
- Pandey RK, Subramanium RK, Darlong V, Lekha C, Garg R, Punj J, et al. Evaluation of glottic view through Air‐Q intubating laryngeal airway in the supine and lateral position and assessing it as a conduit for blind endotracheal intubation in children in the supine position. Pediatric Anesthesia. 2015; 25(12):1241-7. [DOI:10.1111/pan.12746] [PMID]
- Schloss B, Rice J, Tobias JD. The laryngeal mask in infants and children: What is the cuff pressure? International Journal of Pediatric Otorhinolaryngology. 2012; 76(2):284-6. [DOI:10.1016/j.ijporl.2011.11.022] [PMID]
- Ouellette RG. The effect of nitrous oxide on laryngeal mask cuff pressure. American Association of Nurse Anesthetists. 2000; 68(5):411-4. [PMID]
- Ong M, Chambers N, Hullet B, Erb T, Ungern Sternberg V. Laryngeal mask airway and tracheal tube cuff pressures in children: Are clinical endpoints valuable for guiding inflation?. Anaesthesia. 2008; 63(7):738-44. [DOI:10.1111/j.1365-2044.2008.05486.x] [PMID]
- Licina A, Chambers NA, Hullett B, Erb TO, Ungern Sternberg V, Britta S. Lower cuff pressures improve the seal of pediatric laryngeal mask airways. Pediatric Anesthesia. 2008; 18(10):952-6. [DOI:10.1111/j.1460-9592.2008.02706.x] [PMID]
- Augustine SD, Arnold RC, McGrail TW. Laryngeal airway device. Washington: United States Patent; 2000.
- Xue F, Wang Q, Yuan J, Xiong J, Liao X. Is fibreoptic scoring a valuable means to assess proper positioning of the classic laryngeal mask airway in paediatric patients? Anaesthesia and Intensive Care. 2010; 38(3):591-3. [PMID]
- Cook T, Cranshaw J. Randomized crossover comparison of ProSeal® Laryngeal Mask Airway with Laryngeal Tube Sonda® during anaesthesia with controlled ventilation. British Journal of Anaesthesia. 2005; 95(2):261-6. [DOI:10.1093/bja/aei167] [PMID]
- Lopez Gil M, Brimacombe J, Alvarez M. Safety and efficacy of the laryngeal mask airway a prospective survey of 1400 children. Anaesthesia. 1996; 51(10):969-72. [DOI:10.1111/j.1365-2044.1996.tb14968.x] [PMID]
- Mason D, Bingham R. The laryngeal mask airway in children. Anaesthesia. 1990; 45(9):760-3. [DOI:10.1111/j.1365-2044.1990.tb14449.x] [PMID]
- Sanders JC, Olomu PN, Furman JR. Detection, frequency and prediction of problems in the use of the proseal laryngeal mask airway in children. Pediatric Anesthesia. 2008; 18(12):1183-9. [DOI:10.1111/j.1460-9592.2008.02784.x]
- Jagannathan N, Sohn L, Sommers K, Belvis D, Shah RD, Sawardekar A, et al. A randomized comparison of the laryngeal mask airway supreme™ and laryngeal mask airway unique™ in infants and children: Does cuff pressure influence leak pressure?. Pediatric Anesthesia. 2013; 23(10):927-33. [DOI:10.1111/pan.12145] [PMID]
- Shimbori H, Ono K, Miwa T, Morimura N, Noguchi M, Hiroki K. Comparison of the LMA-ProSeal™ and LMA-Classic™ in children. British Journal of Anaesthesia. 2004; 93(4):528-31. [DOI:10.1093/bja/aeh238] [PMID]
- Akça O, Wadhwa A, Sengupta P, Durrani J, Hanni K, Wenke M, et al. The new Perilaryngeal Airway (CobraPLA™) is as efficient as the Laryngeal Mask Airway (LMA™), but provides better airway sealing pressures. Anesthesia and Analgesia. 2004; 99(1):272-8. [DOI:10.1213/01.ANE.0000117003.60213.E9] [PMID] [PMCID]
- Singh I, Gupta M, Tandon M. Comparison of clinical performance of I-Gel™ with LMA—Proseal™ in elective surgeries. Indian Journal of Anaesthesia. 2009; 53(3):302-5. [PMID] [PMCID]
- Levitan R, Kinkle W. Initial anatomic investigations of the I‐gel airway: A novel supraglottic airway without inflatable cuff. Anaesthesia. 2005; 60(10):1022-6. [DOI:10.1111/j.1365-2044.2005.04258.x] [PMID]
- Jagannathan N, Sohn L, Sawardekar A, Gordon J, Langen K, Anderson K. A randomised comparison of the LMA Supreme™ and LMA ProSeal™ in children. Anaesthesia. 2012; 67(6):632-9. [DOI:10.1111/j.1365-2044.2012.07088.x] [PMID]
- Francksen H, Duetschke P, Renner J, Berthold B. A comparison of the i-gel with the LMA Supreme in nonparalysed anaesthetized children: 19AP2-8. European Journal of Anaesthesiology. 2012; 29:231. [DOI:10.1097/00003643-201206001-00769]
- Gaitini L, Yanovski B, Toame R, Carmi N, Somri M. Laryngeal tube suction II versus the ProSeal laryngeal mask in anesthetized children with spontaneous ventilation: 19AP6-3. European Journal of Anaesthesiology. 2007; 24:203. [DOI:10.1097/00003643-200706001-00757]
- Sudhir G, Redfern D, Hall J, Wilkes A, Cann C. A comparison of the disposable Ambu® AuraOnce™ laryngeal mask with the reusable LMA Classic™ laryngeal mask airway. Anaesthesia. 2007; 62(7):719-22. [DOI:10.1111/j.1365-2044.2007.05067.x] [PMID]
- Baidya D, Darlong V, Pandey R, Maitra S, Khanna P. Comparative efficacy and safety of the Ambu® AuraOnce™ laryngeal mask airway during general anaesthesia in adults: A systematic review and meta‐analysis. Anaesthesia. 2014; 69(9):1023-32. [DOI:10.1111/anae.12682] [PMID]
Type of Study: Systematic Review |
Subject:
Anesthesiology
Received: 2018/03/18 | Accepted: 2018/05/15 | Published: 2019/04/1
Received: 2018/03/18 | Accepted: 2018/05/15 | Published: 2019/04/1
References
1. Jagannathan N, Kozlowski RJ, Sohn LE, Langen KE, Roth AG, Mukherji II, et al. A clinical evaluation of the intubating laryngeal airway as a conduit for tracheal intubation in children. Anesthesia & Analgesia. 2011; 112(1):176-82. [DOI:10.1213/ANE.0b013e3181fe0408] [PMID] [DOI:10.1213/ANE.0b013e3181fe0408]
2. Henderson J, Popat M, Latto I, Pearce A. Difficult airway society guidelines for management of the unanticipated difficult intubation. Anaesthesia. 2004; 59(7):675-94. [DOI:10.1111/j.1365-2044.2004.03831.x] [PMID] [DOI:10.1111/j.1365-2044.2004.03831.x]
3. Samir EM, Sakr SA. The air-Q as a conduit for fiberoptic aided tracheal intubation in adult patients undergoing cervical spine fixation: A prospective randomized study. Egyptian Journal of Anaesthesia. 2012; 28(2):133-7. [DOI:10.1016/j.egja.2011.12.002] [DOI:10.1016/j.egja.2011.12.002]
4. Raw D, Beattie J, Hunter J. Anaesthesia for spinal surgery in adults. British Journal of Anaesthesia. 2003; 91(6):886-904. [DOI:10.1093/bja/aeg253] [PMID] [DOI:10.1093/bja/aeg253]
5. Brooks P, Ree R, Rosen D, Ansermino M. Canadian pediatric anesthesiologists prefer inhalational anesthesia to manage difficult airways: A survey. Canadian Journal of Anesthesia. 2005; 52(3):285-90. [DOI:10.1007/BF03016065] [PMID] [DOI:10.1007/BF03016065]
6. Ahn EJ, Choi GJ, Kang H, Baek CW, Jung YH, Woo YC, et al. Comparative efficacy of the air-Q intubating laryngeal airway during general anesthesia in pediatric patients: A systematic review and meta-analysis. BioMed Research International. 2016; 2016:6406391. [DOI:10.1155/2016/6406391] [PMID] [PMCID]
7. Darlong V, Biyani G, Baidya DK, Pandey R, Punj J, Upadhyay AD. Comparison of air‐Q and Ambu Aura‐i for controlled ventilation in infants: A randomized controlled trial. Pediatric Anesthesia. 2015; 25(8):795-800. [DOI:10.1111/pan.12663] [PMID] [DOI:10.1111/pan.12663]
8. Jagannathan N, Sohn L, Sawardekar A, Chang E, Langen K, Anderson K. A randomised trial comparing the laryngeal mask airway Supreme™ with the laryngeal mask airway Unique™ in children. Anaesthesia. 2012; 67(2):139-44. [DOI:10.1111/j.1365-2044.2011.06960.x] [PMID] [DOI:10.1111/j.1365-2044.2011.06960.x]
9. Kleine Brueggeney M, Nicolet A, Nabecker S, Seiler S, Stucki F, Greif R, et al. Blind intubation of anaesthetised children with supraglottic airway devices AmbuAura-i and Air-Q cannot be recommended: A randomised controlled trial. European Journal of Anaesthesiology. 2015; 32(9):631-9. [DOI:10.1097/EJA.0000000000000261] [PMID] [DOI:10.1097/EJA.0000000000000261]
10. Pejovic NJ, Trevisanuto D, Nankunda J, Tylleskär T. Pilot manikin study showed that a supraglottic airway device improved simulated neonatal ventilation in a low‐resource setting. Acta Paediatrica. 2016; 105(12):1440-3. [DOI:10.1111/apa.13565] [PMID] [PMCID] [DOI:10.1111/apa.13565]
11. Beylacq L, Bordes M, Semjen F, Cros AM. The I‐gel®, a single‐use supraglottic airway device with a non‐inflatable cuff and an esophageal vent: An observational study in children. Acta Anaesthesiologica Scandinavica. 2009; 53(3):376-9. [DOI:10.1111/j.1399-6576.2008.01869.x] [PMID] [DOI:10.1111/j.1399-6576.2008.01869.x]
12. Bortone L, Ingelmo PM, Ninno GD, Tosi M, Caffini L, Trenchi J, et al. Randomized controlled trial comparing the laryngeal tube and the laryngeal mask in pediatric patients. Pediatric Anesthesia. 2006; 16(3):251-7. [DOI:10.1111/j.1460-9592.2005.01756.x] [PMID] [DOI:10.1111/j.1460-9592.2005.01756.x]
13. Jagannathan N, Wong DT. Successful tracheal intubation through an intubating laryngeal airway in pediatric patients with airway hemorrhage. Journal of Emergency Medicine. 2011; 41(4):369-73. [DOI:10.1016/j.jemermed.2010.05.066] [PMID] [DOI:10.1016/j.jemermed.2010.05.066]
14. Szmuk P, Ezri T, Akca O, Alfery D. Use of a new supraglottic airway device-the CobraPLA-in a 'difficult to intubate/difficult to ventilate'scenario. Acta Anaesthesiologica Scandinavica. 2005; 49(3):421-3. [DOI:10.1111/j.1399-6576.2005.00618.x] [PMID] [DOI:10.1111/j.1399-6576.2005.00618.x]
15. Baker PA, Brunette KE, Byrnes CA, Thompson J. A prospective randomized trial comparing supraglottic airways for flexible bronchoscopy in children. Pediatric Anesthesia. 2010; 20(9):831-8. [DOI:10.1111/j.1460-9592.2010.03362.x] [PMID] [DOI:10.1111/j.1460-9592.2010.03362.x]
16. Gaitini L, Carmi N, Yanovski B, Tome R, Resnikov I, Gankin I, et al. Comparison of the CobraPLATM (Cobra Perilaryngeal Airway) and the laryngeal mask airway UniqueTM in children under pressure controlled ventilation. Pediatric Anesthesia. 2008; 18(4):313-9. [DOI:10.1111/j.1460-9592.2008.02449.x] [PMID] [DOI:10.1111/j.1460-9592.2008.02449.x]
17. Goyal R, Shukla RN, Kumar G. Comparison of size 2 i‐gel supraglottic airway with LMA‐ProSeal™ and LMA‐Classic™ in spontaneously breathing children undergoing elective surgery. Pediatric Anesthesia. 2012; 22(4):355-9. [DOI:10.1111/j.1460-9592.2011.03757.x] [PMID] [DOI:10.1111/j.1460-9592.2011.03757.x]
18. Hughes C, Place K, Berg S, Mason D. A clinical evaluation of the i‐gelTM supraglottic airway device in children. Pediatric Anesthesia. 2012; 22(8):765-71. [DOI:10.1111/j.1460-9592.2012.03893.x] [PMID] [DOI:10.1111/j.1460-9592.2012.03893.x]
19. Yeoh TY, Chan KB, Yeo LS, Liu EH, Pan TL. An evaluation of the I-gel supraglottic airway in 70 pediatric patients. Journal of Anesthesia. 2015; 29(2):295-8. [DOI:10.1007/s00540-014-1915-6] [PMID] [DOI:10.1007/s00540-014-1915-6]
20. Jagannathan N, Sommers K, Sohn LE, Sawardekar A, Shah RD, Mukherji II, et al. A randomized equivalence trial comparing the i‐gel and laryngeal mask airway Supreme in children. Pediatric Anesthesia. 2013; 23(2):127-33. [DOI:10.1111/pan.12078] [PMID] [DOI:10.1111/pan.12078]
21. Nirupa R, Gombar S, Ahuja V, Sharma P. A randomised trial to compare i-gel and ProSeal™ laryngeal mask airway for airway management in paediatric patients. Indian Journal of Anaesthesia. 2016; 60(10):726-31. [DOI:10.4103/0019-5049.191670] [PMID] [PMCID] [DOI:10.4103/0019-5049.191670]
22. Jagannathan N, Sohn LE, Chang E, Sawardekar A. A cohort evaluation of the Laryngeal Mask Airway‐Supreme™ in children. Pediatric Anesthesia. 2012; 22(8):759-64. [DOI:10.1111/j.1460-9592.2012.03832.x] [PMID] [DOI:10.1111/j.1460-9592.2012.03832.x]
23. Jagannathan N, Roth AG, Sohn LE, Pak TY, Amin S, Suresh S. The new air‐QTM intubating laryngeal airway for tracheal intubation in children with anticipated difficult airway: A case series. Pediatric Anesthesia. 2009; 19(6):618-22. [DOI:10.1111/j.1460-9592.2009.02990.x] [PMID] [DOI:10.1111/j.1460-9592.2009.02990.x]
24. Jagannathan N, Sohn LE, Mankoo R, Langen KE, Roth AG, Hall SC. Prospective evaluation of the self‐pressurized air‐Q intubating laryngeal airway in children. Pediatric Anesthesia. 2011; 21(6):673-80. [DOI:10.1111/j.1460-9592.2011.03576.x] [PMID] [DOI:10.1111/j.1460-9592.2011.03576.x]
25. Jagannathan N, Sohn LE, Sawardekar A, Gordon J, Shah RD, Mukherji II, et al. A randomized trial comparing the Ambu® Aura‐i™ with the air‐Q™ intubating laryngeal airway as conduits for tracheal intubation in children. Pediatric Anesthesia. 2012; 22(12):1197-204. [DOI:10.1111/pan.12024] [PMID] [DOI:10.1111/pan.12024]
26. Jain D, Ghai B, Bala I, Gandhi K, Banerjee G. Evaluation of I‐gel™ airway in different head and neck positions in anesthetized paralyzed children. Pediatric Anesthesia. 2015; 325(12):1248-53. [DOI:10.1111/pan.12748] [PMID] [DOI:10.1111/pan.12748]
27. Sunder RA, Sinha R, Agarwal A, Perumal BCS, Paneerselvam SR. Comparison of Cobra Perilaryngeal Airway (CobraPLA™) with flexible laryngeal mask airway in terms of device stability and ventilation characteristics in pediatric ophthalmic surgery. Journal of Anaesthesiology, Clinical Pharmacology. 2012; 28(3):322-5. [DOI:10.4103/0970-9185.98324] [PMID] [PMCID] [DOI:10.4103/0970-9185.98324]
28. Kelly F, Sale S, Bayley G, Cook T, Stoddart P, White M. A cohort evaluation of the pediatric ProSeal laryngeal mask airway in 100 children. Pediatric Anesthesia. 2008; 18(10):947-51. [DOI:10.1111/j.1460-9592.2008.02705.x] [PMID] [DOI:10.1111/j.1460-9592.2008.02705.x]
29. Kim MS, Lee JH, Han SW, Im YJ, Kang HJ, Lee JR. A randomized comparison of the i‐gel™ with the self‐pressurized air‐Q™ intubating laryngeal airway in children. Pediatric Anesthesia. 2015; 25(4):405-12. [DOI:10.1111/pan.12609] [PMID] [DOI:10.1111/pan.12609]
30. Kus A, Gok CN, Hosten T, Gurkan Y, Solak M, Toker K. The LMA-Supreme versus the I-gel in simulated difficult airway in children: A randomised study. European Journal of Anaesthesiology. 2014; 31(5):280-4. [DOI:10.1097/EJA.0000000000000062] [PMID] [DOI:10.1097/EJA.0000000000000062]
31. Al Mazrou KA, Abdullah KM, ElGammal MS, Ansari RA, Turkistani A, Abdelmeguid ME. Laryngeal mask airway vs. uncuffed endotracheal tube for nasal and paranasal sinus surgery: Paediatric airway protection. European Journal of Anaesthesiology. 2010; 27(1):16-9. [DOI:10.1097/EJA.0b013e32832c5f09] [PMID] [DOI:10.1097/EJA.0b013e32832c5f09]
32. Mitra S, Das B, Jamil SN. Comparison of size 2.5 i-gel™ with ProSeal LMA™ in anaesthetised, paralyzed children undergoing elective surgery. North American Journal of Medical Sciences. 2012; 4(10):453-7. [DOI:10.4103/1947-2714.101983] [PMID] [PMCID] [DOI:10.4103/1947-2714.101983]
33. Pandey RK, Subramanium RK, Darlong V, Lekha C, Garg R, Punj J, et al. Evaluation of glottic view through Air‐Q intubating laryngeal airway in the supine and lateral position and assessing it as a conduit for blind endotracheal intubation in children in the supine position. Pediatric Anesthesia. 2015; 25(12):1241-7. [DOI:10.1111/pan.12746] [PMID] [DOI:10.1111/pan.12746]
34. Schloss B, Rice J, Tobias JD. The laryngeal mask in infants and children: What is the cuff pressure? International Journal of Pediatric Otorhinolaryngology. 2012; 76(2):284-6. [DOI:10.1016/j.ijporl.2011.11.022] [PMID] [DOI:10.1016/j.ijporl.2011.11.022]
35. Ouellette RG. The effect of nitrous oxide on laryngeal mask cuff pressure. American Association of Nurse Anesthetists. 2000; 68(5):411-4. [PMID]
36. Ong M, Chambers N, Hullet B, Erb T, Ungern Sternberg V. Laryngeal mask airway and tracheal tube cuff pressures in children: Are clinical endpoints valuable for guiding inflation?. Anaesthesia. 2008; 63(7):738-44. [DOI:10.1111/j.1365-2044.2008.05486.x] [PMID] [DOI:10.1111/j.1365-2044.2008.05486.x]
37. Licina A, Chambers NA, Hullett B, Erb TO, Ungern Sternberg V, Britta S. Lower cuff pressures improve the seal of pediatric laryngeal mask airways. Pediatric Anesthesia. 2008; 18(10):952-6. [DOI:10.1111/j.1460-9592.2008.02706.x] [PMID] [DOI:10.1111/j.1460-9592.2008.02706.x]
38. Augustine SD, Arnold RC, McGrail TW. Laryngeal airway device. Washington: United States Patent; 2000.
39. Xue F, Wang Q, Yuan J, Xiong J, Liao X. Is fibreoptic scoring a valuable means to assess proper positioning of the classic laryngeal mask airway in paediatric patients? Anaesthesia and Intensive Care. 2010; 38(3):591-3. [PMID] [PMID]
40. Cook T, Cranshaw J. Randomized crossover comparison of ProSeal® Laryngeal Mask Airway with Laryngeal Tube Sonda® during anaesthesia with controlled ventilation. British Journal of Anaesthesia. 2005; 95(2):261-6. [DOI:10.1093/bja/aei167] [PMID] [DOI:10.1093/bja/aei167]
41. Lopez Gil M, Brimacombe J, Alvarez M. Safety and efficacy of the laryngeal mask airway a prospective survey of 1400 children. Anaesthesia. 1996; 51(10):969-72. [DOI:10.1111/j.1365-2044.1996.tb14968.x] [PMID] [DOI:10.1111/j.1365-2044.1996.tb14968.x]
42. Mason D, Bingham R. The laryngeal mask airway in children. Anaesthesia. 1990; 45(9):760-3. [DOI:10.1111/j.1365-2044.1990.tb14449.x] [PMID] [DOI:10.1111/j.1365-2044.1990.tb14449.x]
43. Sanders JC, Olomu PN, Furman JR. Detection, frequency and prediction of problems in the use of the proseal laryngeal mask airway in children. Pediatric Anesthesia. 2008; 18(12):1183-9. [DOI:10.1111/j.1460-9592.2008.02784.x] [DOI:10.1111/j.1460-9592.2008.02784.x]
44. Jagannathan N, Sohn L, Sommers K, Belvis D, Shah RD, Sawardekar A, et al. A randomized comparison of the laryngeal mask airway supreme™ and laryngeal mask airway unique™ in infants and children: Does cuff pressure influence leak pressure?. Pediatric Anesthesia. 2013; 23(10):927-33. [DOI:10.1111/pan.12145] [PMID] [DOI:10.1111/pan.12145]
45. Shimbori H, Ono K, Miwa T, Morimura N, Noguchi M, Hiroki K. Comparison of the LMA-ProSeal™ and LMA-Classic™ in children. British Journal of Anaesthesia. 2004; 93(4):528-31. [DOI:10.1093/bja/aeh238] [PMID] [DOI:10.1093/bja/aeh238]
46. Akça O, Wadhwa A, Sengupta P, Durrani J, Hanni K, Wenke M, et al. The new Perilaryngeal Airway (CobraPLA™) is as efficient as the Laryngeal Mask Airway (LMA™), but provides better airway sealing pressures. Anesthesia and Analgesia. 2004; 99(1):272-8. [DOI:10.1213/01.ANE.0000117003.60213.E9] [PMID] [PMCID] [DOI:10.1213/01.ANE.0000117003.60213.E9]
47. Singh I, Gupta M, Tandon M. Comparison of clinical performance of I-Gel™ with LMA—Proseal™ in elective surgeries. Indian Journal of Anaesthesia. 2009; 53(3):302-5. [PMID] [PMCID] [PMID] [PMCID]
48. Levitan R, Kinkle W. Initial anatomic investigations of the I‐gel airway: A novel supraglottic airway without inflatable cuff. Anaesthesia. 2005; 60(10):1022-6. [DOI:10.1111/j.1365-2044.2005.04258.x] [PMID] [DOI:10.1111/j.1365-2044.2005.04258.x]
49. Jagannathan N, Sohn L, Sawardekar A, Gordon J, Langen K, Anderson K. A randomised comparison of the LMA Supreme™ and LMA ProSeal™ in children. Anaesthesia. 2012; 67(6):632-9. [DOI:10.1111/j.1365-2044.2012.07088.x] [PMID] [DOI:10.1111/j.1365-2044.2012.07088.x]
50. Francksen H, Duetschke P, Renner J, Berthold B. A comparison of the i-gel with the LMA Supreme in nonparalysed anaesthetized children: 19AP2-8. European Journal of Anaesthesiology. 2012; 29:231. [DOI:10.1097/00003643-201206001-00769] [DOI:10.1097/00003643-201206001-00769]
51. Gaitini L, Yanovski B, Toame R, Carmi N, Somri M. Laryngeal tube suction II versus the ProSeal laryngeal mask in anesthetized children with spontaneous ventilation: 19AP6-3. European Journal of Anaesthesiology. 2007; 24:203. [DOI:10.1097/00003643-200706001-00757] [DOI:10.1097/00003643-200706001-00757]
52. Sudhir G, Redfern D, Hall J, Wilkes A, Cann C. A comparison of the disposable Ambu® AuraOnce™ laryngeal mask with the reusable LMA Classic™ laryngeal mask airway. Anaesthesia. 2007; 62(7):719-22. [DOI:10.1111/j.1365-2044.2007.05067.x] [PMID] [DOI:10.1111/j.1365-2044.2007.05067.x]
53. Baidya D, Darlong V, Pandey R, Maitra S, Khanna P. Comparative efficacy and safety of the Ambu® AuraOnce™ laryngeal mask airway during general anaesthesia in adults: A systematic review and meta‐analysis. Anaesthesia. 2014; 69(9):1023-32. [DOI:10.1111/anae.12682] [PMID] [DOI:10.1111/anae.12682]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |