Volume 8, Issue 2 (4-2020)
J. Pediatr. Rev 2020, 8(2): 101-106 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ahmadzadeh Amiri A, Sheikhrezaee M R, Ahmadzadeh Amiri A. Myopia Progression in Low Birth Weight Infants: A Narrative Review. J. Pediatr. Rev 2020; 8 (2) :101-106
URL: http://jpr.mazums.ac.ir/article-1-243-en.html
URL: http://jpr.mazums.ac.ir/article-1-243-en.html
1- Department of Pediatric, Bahrami-Hospital, Tehran University of Medical Sciences, Tehran, Iran.
2- Department of Ophthalmology, Clinical Research Development Unit, Bu-Ali Sina Hospital, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran.
3- Department of Ophthalmology, Clinical Research Development Unit, Bu-Ali Sina Hospital, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran. ,ahmadzdh@yahoo.com
2- Department of Ophthalmology, Clinical Research Development Unit, Bu-Ali Sina Hospital, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran.
3- Department of Ophthalmology, Clinical Research Development Unit, Bu-Ali Sina Hospital, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran. ,
Full-Text [PDF 378 kb]
(2104 Downloads)
| Abstract (HTML) (6274 Views)
Full-Text: (3048 Views)
1. Context
The introduction of the intensive care units into newborn nurseries has significantly increased the survival rate of preterm infants, and notable worry that the incidence of severe neurosensory disabilities might increase, too (1, 2). Several studies have shown that the occurrence of myopia in children born prematurely (gestational age [GA] ≤37 weeks) is negatively correlated with GA and birth weight (3-6).
Refractive errors include myopia (spherical equivalent ≥-0.75 diopters [D] extreme), high myopia (spherical equivalent ≥-6.00 D extreme), moderate or mild myopia (-0.75 to -5.99 D), emmetropia (no refractive error, -0.74 to +0.99 D), hypermetropia (long-sightedness, +1.0 D extreme), astigmatism (≥1 D cylinder), and anisometropia (≥1 D difference in the mean spherical equivalent refraction between the two eyes) (7-9). Relative mild to moderate myopia currently affects 25% of populations in western countries, at least 5% in Africa, and up to 80% in Eastern Asia. In contrast, high myopia (very severe and pathologic) affects less than 3% of the worldwide population (10).
Researchers emphasize the association between myopia and low birth weight for gestational age, gender, greater maternal age, maternal smoking, and higher paternal occupational social class confidently. There was some evidence that even a short period of breastfeeding decreases myopia progression (10).
Low Birth Weight (LBW) infants (birth weight less than 2500 g) are exposed to three risk factors that affect their visual outcome: the presence of Retinopathy of Prematurity (ROP), neurological comorbidities, and preterm birth itself. However, little evidence exists about the myopic progression in growing children who were born with low birth weight. In this study, we only present and discuss the findings of recent investigations that assessed the impact of LBW on myopia development during childhood and changes over a wide range of ages.
2. Evidence Acquisition
A PubMed literature search limited to the English language from 1997-2019 was conducted using the following search terms: “low birth weight infant", “myopia", “prematurity", and “refractive error". Herein, we provide the qualitative results taken out from research studies and discuss them.
In the next step, the extracted articles were reviewed to exclude those refractive errors related primarily to normal birth weight, adult cases without any childbirth history, and studies on non-refractive low vision subjects (as these were not the scope of this review). For the aim of this review, case-control, randomized controlled trials, cohort studies, evidence from meta-analyses, and systematic reviews were considered. Case reports or case series would be included only if there were defined as evidence by more than two articles to unify uncommon findings as an index of future research. We excluded articles considering skillful viewpoints and letters to the editors. A total of 615 potentially relevant records were identified. Following the exclusion of 308 reports, 307 full-text papers were retrieved for gloss inspection. Finally, 31 articles matched the eligibility criteria.
3. Results
Risk factors assessment
Patients with LBW often encounter visual impairment. Refractive status is related to multiple optical components: corneal curvature, anterior chamber depth, lens thickness, vitreous thickness, and axial length.
Ouyang et al. showed that the strongest predictors of myopic development are indices of immaturity: short GA and LBW, of which the prematurity and LBW are more important than the others. They concluded that the birth weight had a negative relationship with corneal astigmatism, astigmatism, and corneal refractive power, while it had a positive association with the corneal radius of curvature, vitreous thickness, and ocular axial length (11).
Regarding the conclusions mentioned above, Chen et al. found that the myopia cases who were born prematurely had significantly shallower anterior chamber depth and thicker lens (12). Moreover, O’Connor et al. showed that the refractive state is relatively constant over the first decade of life with a shift towards myopia of 1 diopter in LBW children (13). Particularly more, in premature children, both with and without ROP, elevated corneal curvature, reduced anterior chamber depth, increased lens thickness, and decreased axial eye length have been observed (14, 15).
Also, Zhu et al. revealed in a case-control study that the incidence of myopia was significantly different in preterm children with ROP, preterm children without ROP, and in full-term children aged 6 years (14.29%, 6.73%, and 2.22% respectively). These figures were higher than those reported in children aged 3-5 years (15, 16).
The introduction of the intensive care units into newborn nurseries has significantly increased the survival rate of preterm infants, and notable worry that the incidence of severe neurosensory disabilities might increase, too (1, 2). Several studies have shown that the occurrence of myopia in children born prematurely (gestational age [GA] ≤37 weeks) is negatively correlated with GA and birth weight (3-6).
Refractive errors include myopia (spherical equivalent ≥-0.75 diopters [D] extreme), high myopia (spherical equivalent ≥-6.00 D extreme), moderate or mild myopia (-0.75 to -5.99 D), emmetropia (no refractive error, -0.74 to +0.99 D), hypermetropia (long-sightedness, +1.0 D extreme), astigmatism (≥1 D cylinder), and anisometropia (≥1 D difference in the mean spherical equivalent refraction between the two eyes) (7-9). Relative mild to moderate myopia currently affects 25% of populations in western countries, at least 5% in Africa, and up to 80% in Eastern Asia. In contrast, high myopia (very severe and pathologic) affects less than 3% of the worldwide population (10).
Researchers emphasize the association between myopia and low birth weight for gestational age, gender, greater maternal age, maternal smoking, and higher paternal occupational social class confidently. There was some evidence that even a short period of breastfeeding decreases myopia progression (10).
Low Birth Weight (LBW) infants (birth weight less than 2500 g) are exposed to three risk factors that affect their visual outcome: the presence of Retinopathy of Prematurity (ROP), neurological comorbidities, and preterm birth itself. However, little evidence exists about the myopic progression in growing children who were born with low birth weight. In this study, we only present and discuss the findings of recent investigations that assessed the impact of LBW on myopia development during childhood and changes over a wide range of ages.
2. Evidence Acquisition
A PubMed literature search limited to the English language from 1997-2019 was conducted using the following search terms: “low birth weight infant", “myopia", “prematurity", and “refractive error". Herein, we provide the qualitative results taken out from research studies and discuss them.
In the next step, the extracted articles were reviewed to exclude those refractive errors related primarily to normal birth weight, adult cases without any childbirth history, and studies on non-refractive low vision subjects (as these were not the scope of this review). For the aim of this review, case-control, randomized controlled trials, cohort studies, evidence from meta-analyses, and systematic reviews were considered. Case reports or case series would be included only if there were defined as evidence by more than two articles to unify uncommon findings as an index of future research. We excluded articles considering skillful viewpoints and letters to the editors. A total of 615 potentially relevant records were identified. Following the exclusion of 308 reports, 307 full-text papers were retrieved for gloss inspection. Finally, 31 articles matched the eligibility criteria.
3. Results
Risk factors assessment
Patients with LBW often encounter visual impairment. Refractive status is related to multiple optical components: corneal curvature, anterior chamber depth, lens thickness, vitreous thickness, and axial length.
Ouyang et al. showed that the strongest predictors of myopic development are indices of immaturity: short GA and LBW, of which the prematurity and LBW are more important than the others. They concluded that the birth weight had a negative relationship with corneal astigmatism, astigmatism, and corneal refractive power, while it had a positive association with the corneal radius of curvature, vitreous thickness, and ocular axial length (11).
Regarding the conclusions mentioned above, Chen et al. found that the myopia cases who were born prematurely had significantly shallower anterior chamber depth and thicker lens (12). Moreover, O’Connor et al. showed that the refractive state is relatively constant over the first decade of life with a shift towards myopia of 1 diopter in LBW children (13). Particularly more, in premature children, both with and without ROP, elevated corneal curvature, reduced anterior chamber depth, increased lens thickness, and decreased axial eye length have been observed (14, 15).
Also, Zhu et al. revealed in a case-control study that the incidence of myopia was significantly different in preterm children with ROP, preterm children without ROP, and in full-term children aged 6 years (14.29%, 6.73%, and 2.22% respectively). These figures were higher than those reported in children aged 3-5 years (15, 16).
However, the refractive outcome of preterm birth is not confined to this condition, and an increase in all forms of refractive errors have also been reported in other studies. In this regard, Fledelius reported that some cases of early myopia, also called myopia of prematurity, later showed a reduction in the degree of myopia over 1-2 years (17). However, Quinn et al. demonstrated that changes in refractive error distribution occur primarily between 3 months and 1 year and include a decrease in the proportion of eyes with hyperopia and an increase correlated with high degrees of myopia (18).
In other words, in a 3.5-year ophthalmological follow-up study of 248 preterm infants, Holmström et al. compared the subjects with the risk of refractive errors. Holmstörm stressed that how prematurity, such as cryo-treated infants, was more significantly associated with the onset of myopia compared with the infants born at term (19). Moreover, a cross-sectional study in 10-year-old prematurely born Swedish children revealed that these children had a higher prevalence of hypermetropia of more than 3 D, or myopia of -1 D or less, astigmatism of 1 D or more, and anisometropia of 1 D or more compared with those born at term (20).
A recent cohort study of very LBW infants at 27-29 years in New Zealand identified that a history of untreated ROP was associated with a greater likelihood of high myopia (>5D) progression (21).
A Randomized controlled clinical trial study demonstrated that nearly 70% of the eyes with high-risk pre-threshold ROP are prone to myopia during childhood and that the proportion with high myopia increases between the ages of 6 months and 3 years (22). Another report of this early treatment for retinopathy of prematurity trial group also showed that approximately two-thirds of eyes with high-risk pre-threshold ROP during the neonatal period are likely to be myopic into the 6 years of life. They also confirmed that conventional management, in comparison with the earlier treatment of eyes with high-risk pre-threshold ROP, did not impress more refractive errors’ development (23).
The Apgar score is broadly used as an index of the health status of neonates immediately at birth and can be used as a predicting mortality factor in extremely low birth weight infants (24). Comparing with the term infants, premature neonates are more susceptible to birth problems. This finding highlighted the Pan et al. result that showed the influence of the low Apgar score and the risk for the child of developing myopia (25).
According to the National Vital Statistics Report, the risk of preterm birth was 12 times higher in twins than singletons (26). Given the results of Avnon et al. study, comparison of refraction errors between preterm infants from singletons and multiples pregnancy disclosed no differences at the age of 6 months old, while at the ages of 8-12 years, multiples had significantly more myopic refractive errors (27).
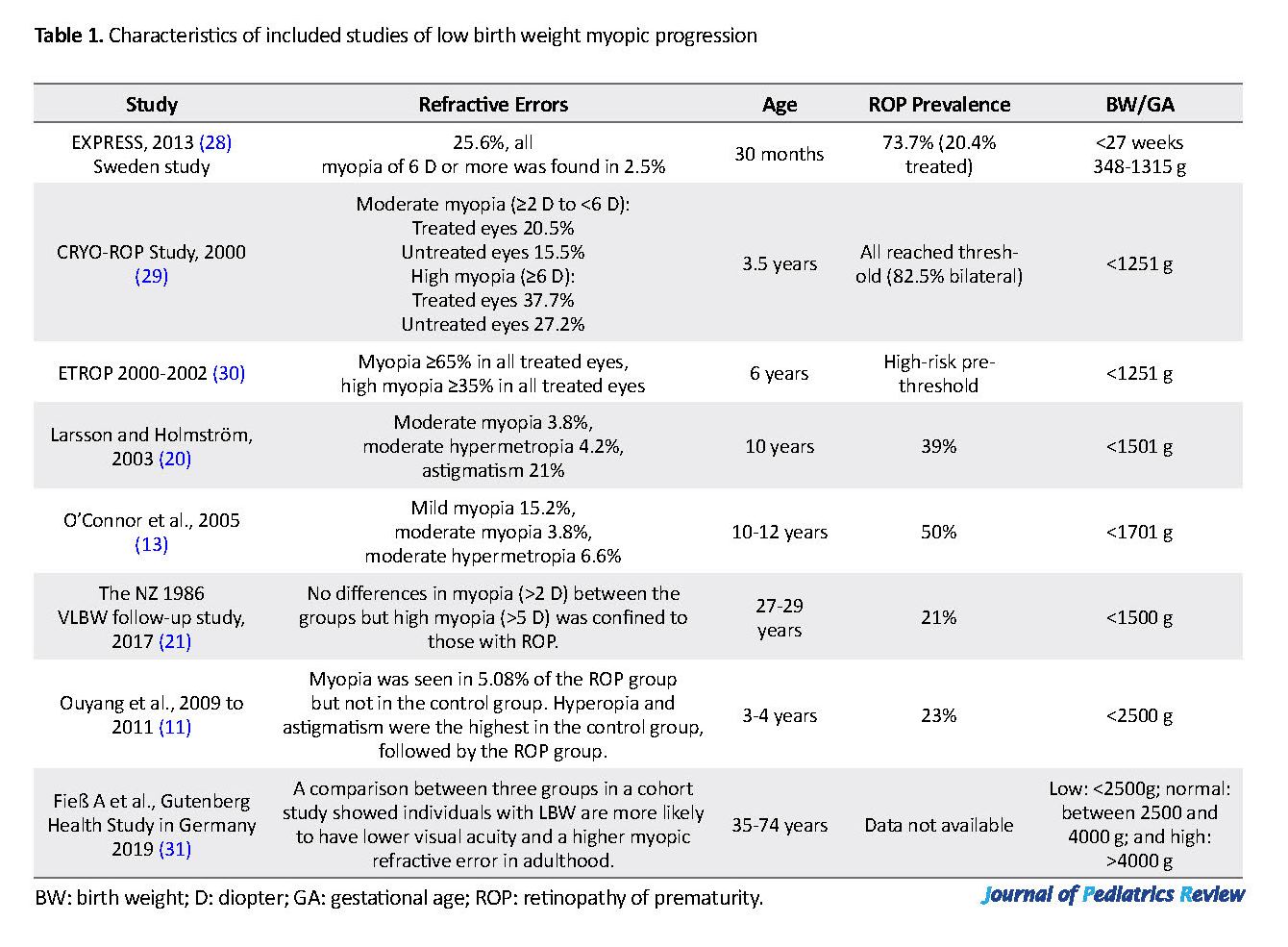
Hence, we should consider myopia as a more complex pattern, where prematurity and low birth weight are crucial to its development ase. Table 1 presents earlier studies implicated refractive states with and without ROP according to the age of examination to the progression of myopia. The study samples varied from infancy to adult age group.
Impact on the ocular structure and refractive status
More immature preterm newborns are more likely to develop adverse visual effects other than those imputable to ROP. The shortened gestational periods up to 40% points out that other features of the visual system, e.g., cerebral white matter is vulnerable to disturbances (32).
Emmetropization is the mechanism in the development of the eye, whereby ocular growth happens in a harmonized manner to make an eye without refractive error (33). This precise visually set process is threatened in a preterm baby because of the following reasons: first, the effect of being born with an LBW and second, as a sequel of ROP.
The shortened intrauterine period in preterm birth deprives the fetus of a protective environment that normally promotes visual growth and development. Fledelius reported that the eyes of preterm babies, even without ROP, do not grow naturally (34).
Studies have shown that the anterior segment of the eye which plays a fundamental role in focusing the light onto the retina, was different between term and preterm infants; corneas of preterm children are more curved, and the lens is thicker, both of which increase the focusing power of the eye, leading to low degree myopia. This is not due to ROP and is referred to as the myopia of prematurity (34, 35).
4. Conclusions
This review indicates an association between LBW and altered ocular geometry in the long term, and suggest that birth weight and the associated factors are essential in refractive errors evolution. Severe ROP increases the risk of myopia. A mild degree of ROP does not contribute more than prematurity to this defect. Early treatment of ROP may improve retinal pathology but could not influence refractive error development, although it is clear that the incidence of myopia varies when the zone of ROP or comorbidity is noted. In general, premature newborns, with or without ROP, are susceptible to myopia. These findings support the importance of repeated assessment of refractive errors over the first decade of life in infants with LBW.
Ethical Considerations
Compliance with ethical guidelines
This research had no ethical consideration.
Funding
There is no specific grant received doing this research.
Authors contributions
All authors contributed to the literature search, compiling and approving the final manuscript.
Conflict of interest
The authors have no financial or personal relations that could state a conflict of interest.
Acknowledgements
The authors would like to thank the Clinical Research Development Unit of Bu-Ali Sina Hospital for cooperation in search strategies.
References
Picciolini O, Squarza C, Fontana C, Giannì ML, Cortinovis I, Gangi S, et al. Neurodevelopmental outcome of extremely low birth weight infants at 24 months corrected age: A comparison between Griffiths and Bayley Scales. BMC Pediatrics. 2015; 15:139. [DOI:10.1186/s12887-015-0457-x] [PMID] [PMCID]
Raju TNK, Buist AS, Blaisdell CJ, Moxey‐Mims M, Saigal S. Adults born preterm: A review of general health and system‐specific outcomes. Acta Pædiatrica. 2017; 106(9):1409-37 [DOI:10.1111/apa.13880] [PMID]
Fledelius HC. Ophthalmic changes from age of 10 to 18 years: A longitudinal study of sequels to low birth weight. I. Refraction. Acta Ophthalmologica (copenhagen). 1980; 58(6):889-98. [DOI:10.1111/j.1755-3768.1980.tb08314.x] [PMID]
O’Connor AR, Stephenson TJ, Johnson A,Tobin MJ, Moseley MJ, Ratib S, et al. Long term ophthalmic outcome of low birth weight children with and without retinopathy of prematurity. Pediatrics. 2002; 109(1):12-8. [DOI:10.1542/peds.109.1.12] [PMID]
Stephenson T, Wright S, O’Connor A, Fielder A, Johnson A, Ratib S, et al. Children born weighing less than 1701 g: Visual and cognitive outcomes at 11-14 years. Archives of Disease in Childhood. Fetal and Neonatal Edition. 2007; 92(4):F265-70. [DOI:10.1136/adc.2006.104000] [PMID] [PMCID]
Rodríguez-Abrego G, Sotelo-Dueñas HM. [Myopia prevalence among school-age children in a suburban population (Mexican)]. Medical Magazine of the Mexican Social Security Institute. 2009; 47(1):39-44. [PMID]
Dandona R, Dandona L. Refractive error blindness. Bulletin of the World Health Organization. 2001; 79(3):237-43. [DOI:10.1590/S0042-96862001000300013]
Deng L, Gwiazda JE. Anisometropia in children from infancy to 15 years. Investigative Ophthalmology & Visual Science. 2012; 53(7):3782-7 [DOI:10.1167/iovs.11-8727] [PMID] [PMCID]
Kempen JH, Mitchell P, Lee KE, Tielsch JM, Broman AT, Taylor HR, et al. Eye diseases prevalence research group: Prevalence of refractive errors among adults in the United States, Western Europe, and Australia. Archives of Ophthalmology. 2004; 122(4):495-505. [DOI:10.1001/archopht.122.4.495] [PMID]
Rahi JS, Cumberland PM, Peckham CS. Myopia over the Life course: prevalence and early life influences in the 1958 British birth cohort. Ophthalmology. 2011; 118(5):797-804 [DOI:10.1016/j.ophtha.2010.09.025] [PMID]
Ouyang LJ, Yin ZQ, Ke N, Chen XK, Liu Q, Fang J, et al. Refractive status and optical components of premature babies with or without retinopathy of prematurity at 3-4 years old. International Journal of Clinical and Experimental Medicine. 2015; 8(7):11854-61. [PMCID] [PMID]
Chen TC, Tsai TH, Shih YF, Yeh PT, Yang CH, Hu FC, et al. Long-term evaluation of refractive status and optical components in eyes of children born prematurely. Investigative Ophthalmology & Visual Science. 2010; 51(12):6140-8. [DOI:10.1167/iovs.10-5234] [PMID]
O’Connor AR, Stephenson TJ, Johnson A, Tobin MJ, Ratib S, Fielder AR. Change of refractive state and eye size in children of birth weight less than 1701 g. British Journal of Ophthalmology. 2006; 90(4):456-60. [DOI:10.1136/bjo.2005.083535] [PMID] [PMCID]
Iwase S, Kaneko H, Fujioka C, Sugimoto K, Kondo M, Takai Y, et al. A long-term follow-up of patients with retinopathy of prematurity treated with photocoagulation and cryotherapy. Nagoya Journal of Medical Science. 2014; 76(1-2):121-8. [PMCID] [PMID]
Zhu X, Zhao R, Wang Y, Ouyang L, Yang J, Li Y, et al. Refractive state and optical compositions of preterm children with and without retinopathy of prematurity in the first 6 years of life. Medicine (Baltimore). 2017; 96(45):e8565. [DOI:10.1097/MD.0000000000008565] [PMID] [PMCID]
Xia YY, Gao X, Yin ZQ, Chen L, Liu Q, Chen X, et al. Refractive status and optical components in premature babies with and without retinopathy of prematurity at 5 years old. International Journal of Clinical and Experimental Medicine. 2017; 10(2):3263-71.
Fledelius HC. Myopia of prematurity, clinical patterns. Acta Ophthalmologica (Scandinavia). 1995; 73(5):402-6. [DOI:10.1111/j.1600-0420.1995.tb00297.x] [PMID]
Quinn GE, Dobson V, Kivlin J, Kaufman LM, Repka MX, Reynolds JD, et al. Prevalence of myopia between 3 months and 5 1/2 years in preterm infants with and without retinopathy of prematurity. Cryotherapy for Retinopathy of Prematurity Cooperative Group Ophthalmology. 1998; 105(7):1292-300. [DOI:10.1016/S0161-6420(98)97036-1]
Holmstrom G, el Azazi M, Kugelberg U. Ophthalmological long term follow up of preterm infants: A population based, prospective study of the refraction and its development. British Journal of Ophthalmology. 1998; 82(11):1265-71 [DOI:10.1136/bjo.82.11.1265] [PMID] [PMCID]
Larsson EK, Rydberg AC, Holmstrom GE. A population-based study of the refractive outcome in 10-year-old preterm and full-term children. Archives of Ophthalmology. 2003; 121(10):1430-6. [DOI:10.1001/archopht.121.10.1430] [PMID]
Darlow BA, Elder MJ, Kimber B, Martin J, Horwood LJ. Vision in former very low birth weight young adults with and without retinopathy of prematurity compared with term born controls: The NZ 1986 VLBW follow-up study. British Journal of Ophthalmology. 2018; 102(8):1041-6. [DOI:10.1136/bjophthalmol-2017-311345] [PMID]
Quinn GE, Dobson V, Davitt BV, Hardy RJ, Tung B, Pedroza C, et al. Progression of myopia and high myopia in the early treatment for retinopathy of prematurity study: Findings to 3 years of age. Ophthalmology. 2008; 115(6):1058-64. [DOI:10.1016/j.ophtha.2007.07.028] [PMID]
Quinn GE, Dobson V, Davitt BV, Wallace DK, Hardy RJ, Tung B, et al. Progression of myopia and high myopia in the early treatment for retinopathy of prematurity study: Findings at 4 to 6 years of age. Journal of American Association for Pediatric Ophthalmology and Strabismus. 2013; 17(2):124-8. [DOI:10.1016/j.jaapos.2012.10.025] [PMID] [PMCID]
Park JH, Chang YS, Ahn SY, Sung SI, Park WS. Predicting mortality in extremely low birth weight infants: Comparison between gestational age, birth weight, Apgar score, CRIB II score, initial and lowest serumalbumin levels. PLoS One. 2018; 13(2):e0192232. [DOI:10.1371/journal.pone.0192232] [PMID] [PMCID]
Pan CW, Qian DJ, Zhu H, Yu JJ, Liu H. Apgar score and reduced vision in children aged 3 to 6 years. Graefe’s Archive for Clinical and Experimental Ophthalmology. 2017; 255(2):401-5. [DOI:10.1007/s00417-016-3506-8] [PMID]
Fielder A, Blencowe H, O’Connor A, Gilbert C. Impact of retinopathy of prematurity on ocular structures and visual functions. Archives of Disease in Childhood; Fetal and Neonatal Edition. 2015; 100(2):F179-84. [DOI:10.1136/archdischild-2014-306207] [PMID]
Fuchs F, Senat MV. Multiple gestations and preterm birth. Seminars in Fetal & Neonatal Medicine. 2016; 21(2):113-20 [DOI:10.1016/j.siny.2015.12.010] [PMID]
Levy N, Shinwell ES, Leiba H. Long-term refractive status of preterm infants from singleton and multiple pregnancies. Journal of Maternal-Fetal and Neonatal Medicine. 2017; 30(19):2276-80. [DOI:10.1080/14767058.2016.1245719] [PMID]
Holmström GE, Kallen K, Hellstrom A, Jakobsson PG, Serenius F, Stjernqvist K, et al. Ophthalmologic outcome at 30 months’ corrected age of a prospective Swedish cohort of children born before 27 weeks of gestation: The extremely preterm infants in Sweden study. JAMA Ophthalmology. 2014; 132(2):182-9. [DOI:10.1001/jamaophthalmol.2013.5812] [PMID]
Quinn GE, Dobson V, Siatkowski R, Hardy RJ, Kivlin J, Palmer EA, et al. Does cryotherapy affect refractive error? Results from treated versus control eyes in the cryotherapy for retinopathy of prematurity trial. Ophthalmology. 2001; 108(2):343-7. [DOI:10.1016/S0161-6420(00)00527-3]
Davitt BV, Quinn GE, Wallace DK, Dobson V, Hardy RJ, Tung B, et al. Astigmatism progression in the early treatment for retinopathy of prematurity study to 6 years of age. Ophthalmology. 2011; 118(12):2326-9. [DOI:10.1016/j.ophtha.2011.06.006] [PMID] [PMCID]
Fieß A, Schuster AK, Nickels S, Elflein HM, Schulz A, Beutel ME, et al. Association of low birth weight with myopic refractive error and lower visual acuity in adulthood: Results from the population-based Gutenberg Health Study (GHS). British Journal of Ophthalmology. 2019; 103(1):99-105. [DOI:10.1136/bjophthalmol-2017-311774] [PMID]
Costeloe KL, Hennessy EM, Haider S, Stacey F, Marlow N, Draper ES. Short term outcomes after extreme preterm birth in England: Comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). British Medical Journal. 2012; 345:e7976. [DOI:10.1136/bmj.e7976] [PMID] [PMCID]
Mutti DO, Sinnott LT, Lynn Mitchell G, Jordan LA, Friedman NE, Frane SL, et al. Ocular component development during infancy and early childhood. Optometry and Vision Science. 2018; 95(11):976-85. [DOI:10.1097/OPX.0000000000001296] [PMID] [PMCID]
Fledelius HC. Pre-term delivery and subsequent ocular development: A 7-10 year follow-up of children screened 1982-84 for ROP; 4) Oculometric-and other metric considerations. Acta Ophthalmologica. 1996; 74(3):301-5 [DOI:10.1111/j.1600-0420.1996.tb00097.x] [PMID]
In other words, in a 3.5-year ophthalmological follow-up study of 248 preterm infants, Holmström et al. compared the subjects with the risk of refractive errors. Holmstörm stressed that how prematurity, such as cryo-treated infants, was more significantly associated with the onset of myopia compared with the infants born at term (19). Moreover, a cross-sectional study in 10-year-old prematurely born Swedish children revealed that these children had a higher prevalence of hypermetropia of more than 3 D, or myopia of -1 D or less, astigmatism of 1 D or more, and anisometropia of 1 D or more compared with those born at term (20).
A recent cohort study of very LBW infants at 27-29 years in New Zealand identified that a history of untreated ROP was associated with a greater likelihood of high myopia (>5D) progression (21).
A Randomized controlled clinical trial study demonstrated that nearly 70% of the eyes with high-risk pre-threshold ROP are prone to myopia during childhood and that the proportion with high myopia increases between the ages of 6 months and 3 years (22). Another report of this early treatment for retinopathy of prematurity trial group also showed that approximately two-thirds of eyes with high-risk pre-threshold ROP during the neonatal period are likely to be myopic into the 6 years of life. They also confirmed that conventional management, in comparison with the earlier treatment of eyes with high-risk pre-threshold ROP, did not impress more refractive errors’ development (23).
The Apgar score is broadly used as an index of the health status of neonates immediately at birth and can be used as a predicting mortality factor in extremely low birth weight infants (24). Comparing with the term infants, premature neonates are more susceptible to birth problems. This finding highlighted the Pan et al. result that showed the influence of the low Apgar score and the risk for the child of developing myopia (25).
According to the National Vital Statistics Report, the risk of preterm birth was 12 times higher in twins than singletons (26). Given the results of Avnon et al. study, comparison of refraction errors between preterm infants from singletons and multiples pregnancy disclosed no differences at the age of 6 months old, while at the ages of 8-12 years, multiples had significantly more myopic refractive errors (27).
Hence, we should consider myopia as a more complex pattern, where prematurity and low birth weight are crucial to its development ase. Table 1 presents earlier studies implicated refractive states with and without ROP according to the age of examination to the progression of myopia. The study samples varied from infancy to adult age group.
Impact on the ocular structure and refractive status
More immature preterm newborns are more likely to develop adverse visual effects other than those imputable to ROP. The shortened gestational periods up to 40% points out that other features of the visual system, e.g., cerebral white matter is vulnerable to disturbances (32).
Emmetropization is the mechanism in the development of the eye, whereby ocular growth happens in a harmonized manner to make an eye without refractive error (33). This precise visually set process is threatened in a preterm baby because of the following reasons: first, the effect of being born with an LBW and second, as a sequel of ROP.
The shortened intrauterine period in preterm birth deprives the fetus of a protective environment that normally promotes visual growth and development. Fledelius reported that the eyes of preterm babies, even without ROP, do not grow naturally (34).
Studies have shown that the anterior segment of the eye which plays a fundamental role in focusing the light onto the retina, was different between term and preterm infants; corneas of preterm children are more curved, and the lens is thicker, both of which increase the focusing power of the eye, leading to low degree myopia. This is not due to ROP and is referred to as the myopia of prematurity (34, 35).
4. Conclusions
This review indicates an association between LBW and altered ocular geometry in the long term, and suggest that birth weight and the associated factors are essential in refractive errors evolution. Severe ROP increases the risk of myopia. A mild degree of ROP does not contribute more than prematurity to this defect. Early treatment of ROP may improve retinal pathology but could not influence refractive error development, although it is clear that the incidence of myopia varies when the zone of ROP or comorbidity is noted. In general, premature newborns, with or without ROP, are susceptible to myopia. These findings support the importance of repeated assessment of refractive errors over the first decade of life in infants with LBW.
Ethical Considerations
Compliance with ethical guidelines
This research had no ethical consideration.
Funding
There is no specific grant received doing this research.
Authors contributions
All authors contributed to the literature search, compiling and approving the final manuscript.
Conflict of interest
The authors have no financial or personal relations that could state a conflict of interest.
Acknowledgements
The authors would like to thank the Clinical Research Development Unit of Bu-Ali Sina Hospital for cooperation in search strategies.
References
Picciolini O, Squarza C, Fontana C, Giannì ML, Cortinovis I, Gangi S, et al. Neurodevelopmental outcome of extremely low birth weight infants at 24 months corrected age: A comparison between Griffiths and Bayley Scales. BMC Pediatrics. 2015; 15:139. [DOI:10.1186/s12887-015-0457-x] [PMID] [PMCID]
Raju TNK, Buist AS, Blaisdell CJ, Moxey‐Mims M, Saigal S. Adults born preterm: A review of general health and system‐specific outcomes. Acta Pædiatrica. 2017; 106(9):1409-37 [DOI:10.1111/apa.13880] [PMID]
Fledelius HC. Ophthalmic changes from age of 10 to 18 years: A longitudinal study of sequels to low birth weight. I. Refraction. Acta Ophthalmologica (copenhagen). 1980; 58(6):889-98. [DOI:10.1111/j.1755-3768.1980.tb08314.x] [PMID]
O’Connor AR, Stephenson TJ, Johnson A,Tobin MJ, Moseley MJ, Ratib S, et al. Long term ophthalmic outcome of low birth weight children with and without retinopathy of prematurity. Pediatrics. 2002; 109(1):12-8. [DOI:10.1542/peds.109.1.12] [PMID]
Stephenson T, Wright S, O’Connor A, Fielder A, Johnson A, Ratib S, et al. Children born weighing less than 1701 g: Visual and cognitive outcomes at 11-14 years. Archives of Disease in Childhood. Fetal and Neonatal Edition. 2007; 92(4):F265-70. [DOI:10.1136/adc.2006.104000] [PMID] [PMCID]
Rodríguez-Abrego G, Sotelo-Dueñas HM. [Myopia prevalence among school-age children in a suburban population (Mexican)]. Medical Magazine of the Mexican Social Security Institute. 2009; 47(1):39-44. [PMID]
Dandona R, Dandona L. Refractive error blindness. Bulletin of the World Health Organization. 2001; 79(3):237-43. [DOI:10.1590/S0042-96862001000300013]
Deng L, Gwiazda JE. Anisometropia in children from infancy to 15 years. Investigative Ophthalmology & Visual Science. 2012; 53(7):3782-7 [DOI:10.1167/iovs.11-8727] [PMID] [PMCID]
Kempen JH, Mitchell P, Lee KE, Tielsch JM, Broman AT, Taylor HR, et al. Eye diseases prevalence research group: Prevalence of refractive errors among adults in the United States, Western Europe, and Australia. Archives of Ophthalmology. 2004; 122(4):495-505. [DOI:10.1001/archopht.122.4.495] [PMID]
Rahi JS, Cumberland PM, Peckham CS. Myopia over the Life course: prevalence and early life influences in the 1958 British birth cohort. Ophthalmology. 2011; 118(5):797-804 [DOI:10.1016/j.ophtha.2010.09.025] [PMID]
Ouyang LJ, Yin ZQ, Ke N, Chen XK, Liu Q, Fang J, et al. Refractive status and optical components of premature babies with or without retinopathy of prematurity at 3-4 years old. International Journal of Clinical and Experimental Medicine. 2015; 8(7):11854-61. [PMCID] [PMID]
Chen TC, Tsai TH, Shih YF, Yeh PT, Yang CH, Hu FC, et al. Long-term evaluation of refractive status and optical components in eyes of children born prematurely. Investigative Ophthalmology & Visual Science. 2010; 51(12):6140-8. [DOI:10.1167/iovs.10-5234] [PMID]
O’Connor AR, Stephenson TJ, Johnson A, Tobin MJ, Ratib S, Fielder AR. Change of refractive state and eye size in children of birth weight less than 1701 g. British Journal of Ophthalmology. 2006; 90(4):456-60. [DOI:10.1136/bjo.2005.083535] [PMID] [PMCID]
Iwase S, Kaneko H, Fujioka C, Sugimoto K, Kondo M, Takai Y, et al. A long-term follow-up of patients with retinopathy of prematurity treated with photocoagulation and cryotherapy. Nagoya Journal of Medical Science. 2014; 76(1-2):121-8. [PMCID] [PMID]
Zhu X, Zhao R, Wang Y, Ouyang L, Yang J, Li Y, et al. Refractive state and optical compositions of preterm children with and without retinopathy of prematurity in the first 6 years of life. Medicine (Baltimore). 2017; 96(45):e8565. [DOI:10.1097/MD.0000000000008565] [PMID] [PMCID]
Xia YY, Gao X, Yin ZQ, Chen L, Liu Q, Chen X, et al. Refractive status and optical components in premature babies with and without retinopathy of prematurity at 5 years old. International Journal of Clinical and Experimental Medicine. 2017; 10(2):3263-71.
Fledelius HC. Myopia of prematurity, clinical patterns. Acta Ophthalmologica (Scandinavia). 1995; 73(5):402-6. [DOI:10.1111/j.1600-0420.1995.tb00297.x] [PMID]
Quinn GE, Dobson V, Kivlin J, Kaufman LM, Repka MX, Reynolds JD, et al. Prevalence of myopia between 3 months and 5 1/2 years in preterm infants with and without retinopathy of prematurity. Cryotherapy for Retinopathy of Prematurity Cooperative Group Ophthalmology. 1998; 105(7):1292-300. [DOI:10.1016/S0161-6420(98)97036-1]
Holmstrom G, el Azazi M, Kugelberg U. Ophthalmological long term follow up of preterm infants: A population based, prospective study of the refraction and its development. British Journal of Ophthalmology. 1998; 82(11):1265-71 [DOI:10.1136/bjo.82.11.1265] [PMID] [PMCID]
Larsson EK, Rydberg AC, Holmstrom GE. A population-based study of the refractive outcome in 10-year-old preterm and full-term children. Archives of Ophthalmology. 2003; 121(10):1430-6. [DOI:10.1001/archopht.121.10.1430] [PMID]
Darlow BA, Elder MJ, Kimber B, Martin J, Horwood LJ. Vision in former very low birth weight young adults with and without retinopathy of prematurity compared with term born controls: The NZ 1986 VLBW follow-up study. British Journal of Ophthalmology. 2018; 102(8):1041-6. [DOI:10.1136/bjophthalmol-2017-311345] [PMID]
Quinn GE, Dobson V, Davitt BV, Hardy RJ, Tung B, Pedroza C, et al. Progression of myopia and high myopia in the early treatment for retinopathy of prematurity study: Findings to 3 years of age. Ophthalmology. 2008; 115(6):1058-64. [DOI:10.1016/j.ophtha.2007.07.028] [PMID]
Quinn GE, Dobson V, Davitt BV, Wallace DK, Hardy RJ, Tung B, et al. Progression of myopia and high myopia in the early treatment for retinopathy of prematurity study: Findings at 4 to 6 years of age. Journal of American Association for Pediatric Ophthalmology and Strabismus. 2013; 17(2):124-8. [DOI:10.1016/j.jaapos.2012.10.025] [PMID] [PMCID]
Park JH, Chang YS, Ahn SY, Sung SI, Park WS. Predicting mortality in extremely low birth weight infants: Comparison between gestational age, birth weight, Apgar score, CRIB II score, initial and lowest serumalbumin levels. PLoS One. 2018; 13(2):e0192232. [DOI:10.1371/journal.pone.0192232] [PMID] [PMCID]
Pan CW, Qian DJ, Zhu H, Yu JJ, Liu H. Apgar score and reduced vision in children aged 3 to 6 years. Graefe’s Archive for Clinical and Experimental Ophthalmology. 2017; 255(2):401-5. [DOI:10.1007/s00417-016-3506-8] [PMID]
Fielder A, Blencowe H, O’Connor A, Gilbert C. Impact of retinopathy of prematurity on ocular structures and visual functions. Archives of Disease in Childhood; Fetal and Neonatal Edition. 2015; 100(2):F179-84. [DOI:10.1136/archdischild-2014-306207] [PMID]
Fuchs F, Senat MV. Multiple gestations and preterm birth. Seminars in Fetal & Neonatal Medicine. 2016; 21(2):113-20 [DOI:10.1016/j.siny.2015.12.010] [PMID]
Levy N, Shinwell ES, Leiba H. Long-term refractive status of preterm infants from singleton and multiple pregnancies. Journal of Maternal-Fetal and Neonatal Medicine. 2017; 30(19):2276-80. [DOI:10.1080/14767058.2016.1245719] [PMID]
Holmström GE, Kallen K, Hellstrom A, Jakobsson PG, Serenius F, Stjernqvist K, et al. Ophthalmologic outcome at 30 months’ corrected age of a prospective Swedish cohort of children born before 27 weeks of gestation: The extremely preterm infants in Sweden study. JAMA Ophthalmology. 2014; 132(2):182-9. [DOI:10.1001/jamaophthalmol.2013.5812] [PMID]
Quinn GE, Dobson V, Siatkowski R, Hardy RJ, Kivlin J, Palmer EA, et al. Does cryotherapy affect refractive error? Results from treated versus control eyes in the cryotherapy for retinopathy of prematurity trial. Ophthalmology. 2001; 108(2):343-7. [DOI:10.1016/S0161-6420(00)00527-3]
Davitt BV, Quinn GE, Wallace DK, Dobson V, Hardy RJ, Tung B, et al. Astigmatism progression in the early treatment for retinopathy of prematurity study to 6 years of age. Ophthalmology. 2011; 118(12):2326-9. [DOI:10.1016/j.ophtha.2011.06.006] [PMID] [PMCID]
Fieß A, Schuster AK, Nickels S, Elflein HM, Schulz A, Beutel ME, et al. Association of low birth weight with myopic refractive error and lower visual acuity in adulthood: Results from the population-based Gutenberg Health Study (GHS). British Journal of Ophthalmology. 2019; 103(1):99-105. [DOI:10.1136/bjophthalmol-2017-311774] [PMID]
Costeloe KL, Hennessy EM, Haider S, Stacey F, Marlow N, Draper ES. Short term outcomes after extreme preterm birth in England: Comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). British Medical Journal. 2012; 345:e7976. [DOI:10.1136/bmj.e7976] [PMID] [PMCID]
Mutti DO, Sinnott LT, Lynn Mitchell G, Jordan LA, Friedman NE, Frane SL, et al. Ocular component development during infancy and early childhood. Optometry and Vision Science. 2018; 95(11):976-85. [DOI:10.1097/OPX.0000000000001296] [PMID] [PMCID]
Fledelius HC. Pre-term delivery and subsequent ocular development: A 7-10 year follow-up of children screened 1982-84 for ROP; 4) Oculometric-and other metric considerations. Acta Ophthalmologica. 1996; 74(3):301-5 [DOI:10.1111/j.1600-0420.1996.tb00097.x] [PMID]
Type of Study: Narrative Review |
Subject:
Ophthalmology
Received: 2019/06/11 | Accepted: 2019/09/14 | Published: 2020/04/1
Received: 2019/06/11 | Accepted: 2019/09/14 | Published: 2020/04/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |