Volume 10, Issue 2 (4-2022)
J. Pediatr. Rev 2022, 10(2): 155-160 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghandi Y, Mehrabi S, Safaei M. Electrocardiography Adverse Effects Systemic Glucantime in a Child With Cutaneous Leishmaniosis: A Case Report and Brief Review. J. Pediatr. Rev 2022; 10 (2) :155-160
URL: http://jpr.mazums.ac.ir/article-1-387-en.html
URL: http://jpr.mazums.ac.ir/article-1-387-en.html
1- Department of Pediatrics, Clinical Research Development Center of Amirkabir Hospital, Arak University of Medical Sciences, Arak, Iran. , drghandi1351@gmail.com
2- Student Research Committee, Arak University of Medical Sciences, Arak, Iran.
2- Student Research Committee, Arak University of Medical Sciences, Arak, Iran.
Full-Text [PDF 394 kb]
(613 Downloads)
| Abstract (HTML) (1500 Views)
Full-Text: (527 Views)
1. Introduction
Antimonial compounds are the most common choice for the treatment of cutaneous Leishmaniosis (CL). In most countries, patients with CL are treated with meglumine antimoniate (glucantime) as its efficacy has been approved in the treatment of Leishmaniosis. Although all patients with CL do not need the treatment, they are usually treated due to the anticipated morbidities [1]. The suggested mechanisms are inhibition of fatty acid oxidation, glucose uptake, and glucose oxidation, which reduce the production of adenosine triphosphate (ATP) and Guanosine Triphosphate (GTP) in the amastigotes and lead to the death of protozoa. Owing to the poor absorption of the drug from the GI tract, it is parenterally administrated at a dosage of 15 to 20 mgSb+5/kg/day, for 10-day periods with equivalent intervals until the lesions are cured.
Antimonial toxicities are common and the symptoms are myalgia, joint stiffness, anorexia, bradycardia, and also electrocardiogram (ECG) changes, such as prolonged QT interval and inverted T wave [2]. The therapy can be continued as long as there are no ST-segment changes, prolonged PR interval > 500 ms, and significant arrhythmias in the ECG. Due to the potential cardiac side effects of glucantime, patients who receive this drug are recommended to be monitored before and during the treatment. There are many patients who received high doses of glucantime (30 to 60 mg/kg/day) without any side effects; however, death has been reported in some of them [3].
2. Case report
A 7-year-old girl was admitted to the hospital with the complaint of skin lesions on her left leg from ten months ago. At first, the lesions had been suspected of coetaneous leishmania, and the positive culture of the biopsy specimen approved the diagnosis. The patient had received glucantime as a treatment for two 15-day periods. The first time it was administrated by subcutaneous injection at the dose of 10-15 mg/kg/day and the second time, it was injected intramuscularly at the same dose. Unfortunately, she had not responded to the treatment and was referred to the pediatric clinic for the third time.
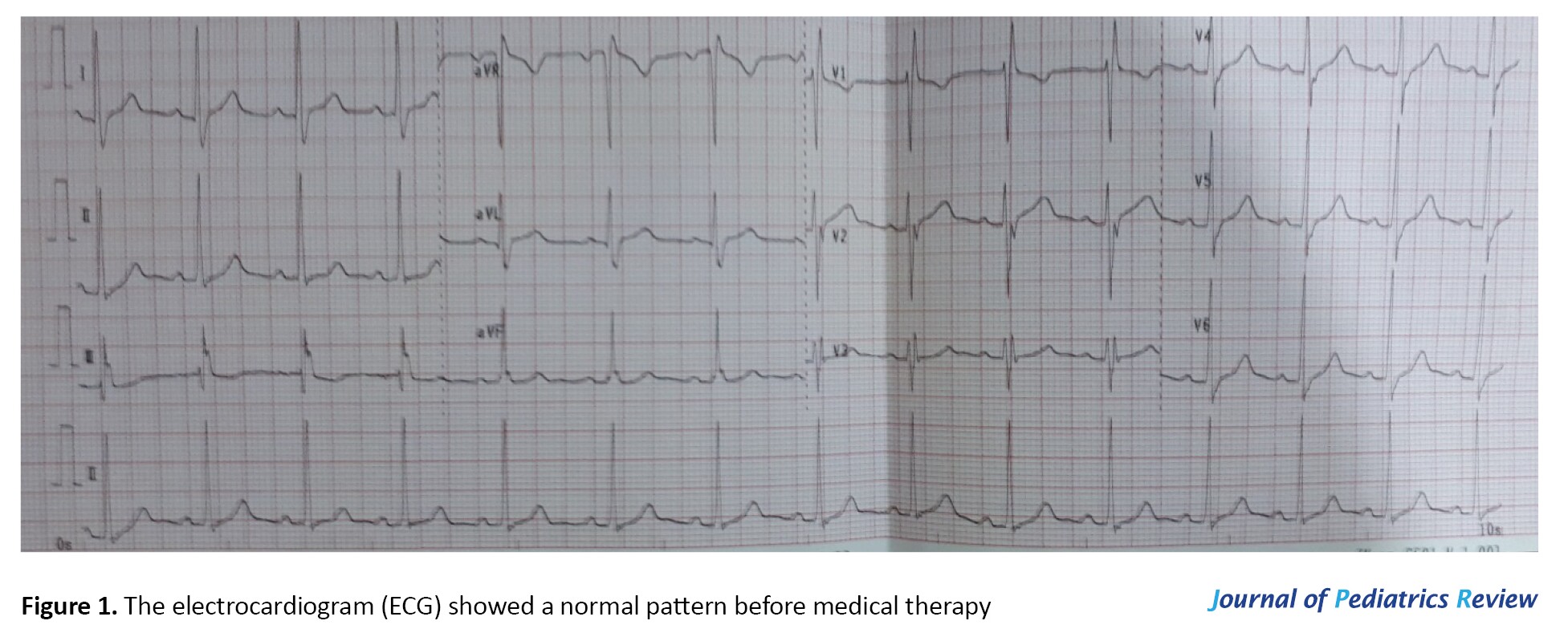
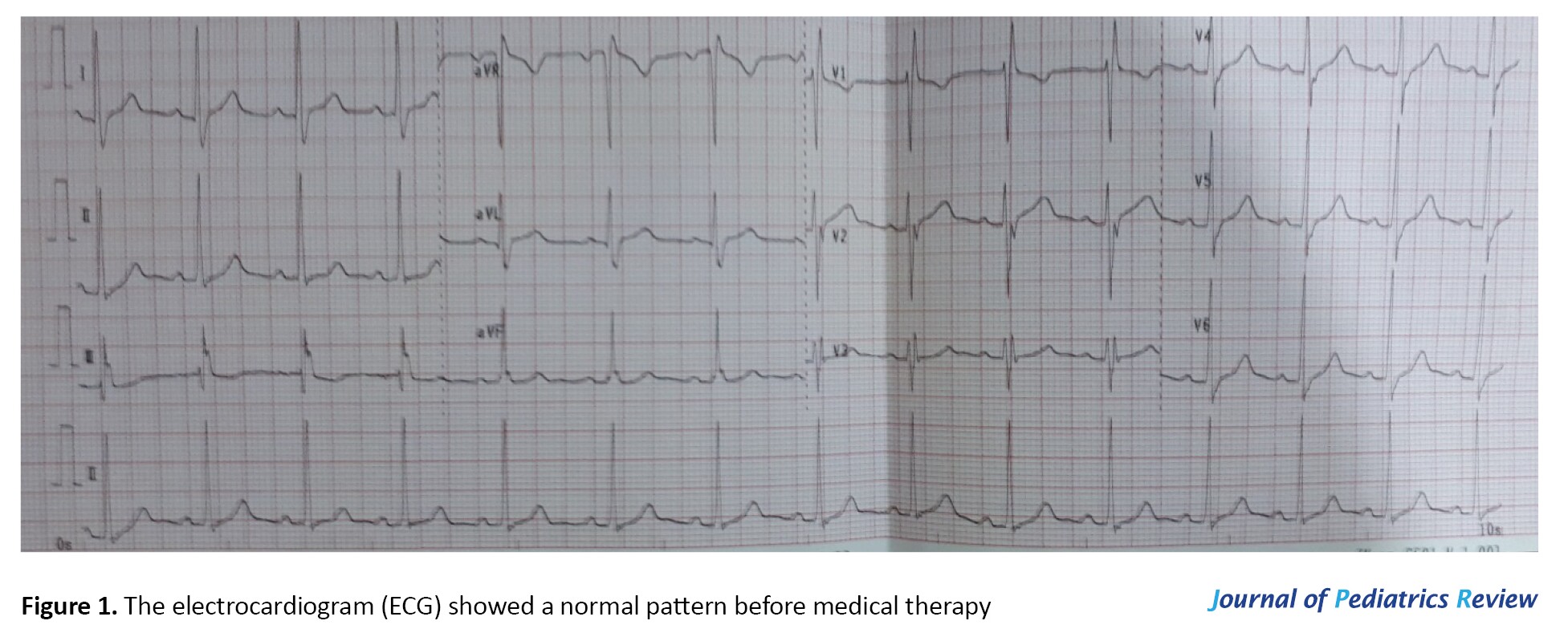
During the examination, multiple hyperkeratosis nodules were detected on the leg. There was also no other medical history with possible interaction with glucantime. Due to the cardiac side effects of glucantime, cardiology consultation was requested and an ECG was performed for the patients during the administration of treatment for the third time. There was just one recorded ECG available, which had been taken prior to the treatment (ten months ago) for the first time and it was completely normal (Figure 1).
Several ECG changes were detected, including first-degree block, Right Bundle Branch Block (RBBB), and QTc prolongation (Figure 2 A-B). Further cardiac evaluations were performed, echocardiography was normal (ejection fraction=69%) and structural diseases, such as (atrial septal defect) ASD2, (Total anomalous pulmonary venous return) TAPVC (Arrhythmogenic right ventricular dysplasia/cardiomyopathy) or ARVD/C were not detected. Based on the 24-hour Holter monitoring, there were no significant ventricular arrhythmias, such as Ventricular tachycardia (VT), Ventricular fibrillation (VF), and Premature Ventricular Contractions (PVC). The modified Bruce stress test was not performed as the patient refused to cooperate.

The cardiologist stopped the treatment with glucantime to improve the ECG changes, and an ECG was taken every week. Even though prolonged QT interval and RBBB improved after a month, the first-degree block was present for ten months and showed no improvement (Figure 3).

Discussion and review of the literature
A very few studies have been conducted on the cardiotoxicity of glucantime in pediatric patients, in which prolonged QT (QTc=460 ms), inverted T, bradycardia, ST-segment changes, and LBBB have been reported. In the current study, the patient with no history of cardiac abnormalities showed prolonged QT, first-degree block, and RBBB.
In a systematic review by Oliveira et al., the most frequent cardiac side effects of cutaneous Leishmaniosis treatment were QTc prolongation and ventricular repolarization disturbances [4]. They showed that ECG abnormalities developed during 54% of the treatment courses. The frequency with which abnormalities occurred was increasing and related to the total daily dose of antimony (Sb). The frequency with which ECG abnormalities developed was also related to the duration of treatment and passing time. The most common ECG abnormalities were flattening and/or inversion of T waves. They reported that prolongation of the corrected QT interval occurred in all treated for more than 30 days or with more than 20mg Sb/kg/d. One patient died suddenly during the fourth week of treatment with 60 mg Sb/kg/d, and two patients died of measles after nine or ten days of treatment with 30 mg Sb/kg/d. QT prolongation and a concave ST segment developed in all three patients who died [2]. They concluded that minor ECG abnormalities are common when sodium stibogluconate is used at doses above 20 mg Sb/kg/d for more than 15 days, and life-threatening arrhythmias may occur if very high doses are used [2].
Lawn et al. (2006) described an 81-year-old patient with hypertension and cardiomegaly who underwent the treatment of leishmania and presented ventricular arrhythmias. The arrhythmias were associated with the use of a thiazide diuretic that caused a reduction in plasma potassium levels during treatment [5].
Lawn et al. reported that the risk of QTc prolongation and arrhythmias is important for the identification of changes before and during treatment. They evaluated serial ECGs from 60 patients available for analysis, and none of these developed adverse clinical events. Abnormalities developed in the ECGs of 32 patients (53%), 27 years among males and 23 years among females. They discovered that T wave flattening developed in the ECGs of 31 patients (52%) and, in general, persisted throughout the remaining treatment course. The median duration between starting treatment and onset of T wave changes was 14 days (range 3-23 days). Among these patients, biphasic or inverted T waves were seen in 8 patients (13%). No patients developed ST-segment changes. First-degree heart block was observed in one patient on days 7-9 of treatment but resolved spontaneously. The mean QTc progressively increased during treatment from a baseline of 389 msec to 404 msec after three weeks of treatment. Six patients treated for CL developed significant asymptomatic QTc prolongation in the third week of treatment and were all potentially at higher risk of arrhythmias. No electrolyte abnormalities were detected among these patients and none developed adverse events. No patients treated for ≥28 days for ML developed significant QTc prolongation. Therefore, they offered that treatment should be discontinued if the QTc interval prolongation exceeds 450 ms [5].
Sadeghian et al. reported electrocardiographic changes among 130 patients who received glucantime for the treatment of leishmania. Their results indicated QTc prolongation in 19% of the patients, bradycardia in 10.6%, ST depression in 6.1%, minimal ST elevation in 3%, inverted T wave in 7.4%, PVC in 2.99%, PAC in 0.7%, and LBBB in 0.7% of them. First-degree and second-degree blocks were not detected. All these changes reversed soon, except in one case with LBBB, which lasted for a month after the treatment was stopped [6].
Another study by Ribeiro et al. showed that the only cardiac side effect of administrating short-term and low-dose glucantime (15 mg/kg/day) was prolonged QT [7].
They studied the cardiotoxicity of low-dose, short-term therapy with meglumine in cutaneous Leishmaniosis in 62 CL patients. A standard ECG was obtained before and immediately after the first cycle of treatment (15 mg Sb5+ kg-1 day-1). There were no significant differences in qualitative ECG variables before and after meglumine treatment. However, the corrected QT interval was clearly prolonged after antimonial therapy. QTc augmentation exceeded 40 ms in 12 patients, of whom seven patients developed marked QTc interval enlargement (500 ms) after meglumine therapy. This unrecognized cardiac toxicity induced by short-term, low-dose antimonial therapy has potentially important clinical implications [6]. They expressed that because sudden death was related to QTc prolongation over 500 ms induced by high-dose antimonial therapy, routine electrocardiographic monitoring should be done even in CL patients treated with short-term, low-dose meglumine schedules. They suggested that until further studies are conducted to establish the interactions between pentavalent antimonials and other drugs, special care is recommended when using meglumine in combination with other medications, in particular with drugs that also increase the QTc interval [6].
Because significant cardiac toxicity caused by low-dose and short-term use of glucantime is rare, its administration is considered safe. It is proposed that cardiac monitoring would not be necessary for patients receiving 10 mgSsb5+/kg/day up to 30 days or 20mgSb5+/kg/ day up to 20 days [3]. On the other hand, in certain studies, weekly ECG monitoring is recommended for patients treated for more than 20 days [8].
In a study by Zeballos et al., 45% of the patients who were treated with glucantime had echocardiographic changes in electrocardiography (T wave and ST-segment changes), which reversed two months after stopping the treatment [8].
In some studies, administration of glucantime 20mg/kg/day for 30 days for the treatment of visceral Leishmaniosis has been considered safe, and the only significant cardiac side effect was bradycardia, which was reversible. It is suggested that in conditions with low-level health facilities, pulse rate monitoring during antimonial therapy would help to detect cardiotoxicity [9].
Oliveiraa et al. in a systematic review showed that electrocardiographic QTc interval prolongation and a mild to moderate increase in liver and pancreatic enzymes were additional adverse effects of pentavalent antimonials. Therefore, if not detected early, may cause sudden and fatal arrhythmia and was the most frequent electrocardiographic adverse effect. They believed that weekly ECG monitoring should be sufficient to prevent this condition. They, therefore, suggested ECG and serum potassium monitoring be performed at least once a week in older patients or those with cardiac conditions [4].
There was no case of hospitalization or death due to arrhythmias. However, prolonged QTc interval and ST-segment changes were the most common electrocardiographic abnormalities in patients. In our case, there were three cardiac complications during treatment and one of them was not improved. In all relevant studies, there is not a report of RBBB in patients who received glucantime. In the present study, RBBB was one of the ECG changes and it was present for six months. It should be more cautiously evaluated in the EKG of glucantime-treated patients.
3. Conclusion
According to the results, ECG changes, including RBBB, first-degree block, and prolonged QT were detected in a child treated with glucantime for two treatment periods. It indicates the necessity of ECG monitoring prior to and during the treatment with this drug. Moreover, RBBB has not been commonly reported in other cases and other studies. Thus, it should be considered as one of the cardiac side effects of glucantime and needs more attention.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any specific grant fromfunding agencies in the public, commercial, or not-forprofit sectors.
Authors' contributions
All authors contributed in preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
References
Antimonial compounds are the most common choice for the treatment of cutaneous Leishmaniosis (CL). In most countries, patients with CL are treated with meglumine antimoniate (glucantime) as its efficacy has been approved in the treatment of Leishmaniosis. Although all patients with CL do not need the treatment, they are usually treated due to the anticipated morbidities [1]. The suggested mechanisms are inhibition of fatty acid oxidation, glucose uptake, and glucose oxidation, which reduce the production of adenosine triphosphate (ATP) and Guanosine Triphosphate (GTP) in the amastigotes and lead to the death of protozoa. Owing to the poor absorption of the drug from the GI tract, it is parenterally administrated at a dosage of 15 to 20 mgSb+5/kg/day, for 10-day periods with equivalent intervals until the lesions are cured.
Antimonial toxicities are common and the symptoms are myalgia, joint stiffness, anorexia, bradycardia, and also electrocardiogram (ECG) changes, such as prolonged QT interval and inverted T wave [2]. The therapy can be continued as long as there are no ST-segment changes, prolonged PR interval > 500 ms, and significant arrhythmias in the ECG. Due to the potential cardiac side effects of glucantime, patients who receive this drug are recommended to be monitored before and during the treatment. There are many patients who received high doses of glucantime (30 to 60 mg/kg/day) without any side effects; however, death has been reported in some of them [3].
2. Case report
A 7-year-old girl was admitted to the hospital with the complaint of skin lesions on her left leg from ten months ago. At first, the lesions had been suspected of coetaneous leishmania, and the positive culture of the biopsy specimen approved the diagnosis. The patient had received glucantime as a treatment for two 15-day periods. The first time it was administrated by subcutaneous injection at the dose of 10-15 mg/kg/day and the second time, it was injected intramuscularly at the same dose. Unfortunately, she had not responded to the treatment and was referred to the pediatric clinic for the third time.
During the examination, multiple hyperkeratosis nodules were detected on the leg. There was also no other medical history with possible interaction with glucantime. Due to the cardiac side effects of glucantime, cardiology consultation was requested and an ECG was performed for the patients during the administration of treatment for the third time. There was just one recorded ECG available, which had been taken prior to the treatment (ten months ago) for the first time and it was completely normal (Figure 1).
Several ECG changes were detected, including first-degree block, Right Bundle Branch Block (RBBB), and QTc prolongation (Figure 2 A-B). Further cardiac evaluations were performed, echocardiography was normal (ejection fraction=69%) and structural diseases, such as (atrial septal defect) ASD2, (Total anomalous pulmonary venous return) TAPVC (Arrhythmogenic right ventricular dysplasia/cardiomyopathy) or ARVD/C were not detected. Based on the 24-hour Holter monitoring, there were no significant ventricular arrhythmias, such as Ventricular tachycardia (VT), Ventricular fibrillation (VF), and Premature Ventricular Contractions (PVC). The modified Bruce stress test was not performed as the patient refused to cooperate.

The cardiologist stopped the treatment with glucantime to improve the ECG changes, and an ECG was taken every week. Even though prolonged QT interval and RBBB improved after a month, the first-degree block was present for ten months and showed no improvement (Figure 3).

Discussion and review of the literature
A very few studies have been conducted on the cardiotoxicity of glucantime in pediatric patients, in which prolonged QT (QTc=460 ms), inverted T, bradycardia, ST-segment changes, and LBBB have been reported. In the current study, the patient with no history of cardiac abnormalities showed prolonged QT, first-degree block, and RBBB.
In a systematic review by Oliveira et al., the most frequent cardiac side effects of cutaneous Leishmaniosis treatment were QTc prolongation and ventricular repolarization disturbances [4]. They showed that ECG abnormalities developed during 54% of the treatment courses. The frequency with which abnormalities occurred was increasing and related to the total daily dose of antimony (Sb). The frequency with which ECG abnormalities developed was also related to the duration of treatment and passing time. The most common ECG abnormalities were flattening and/or inversion of T waves. They reported that prolongation of the corrected QT interval occurred in all treated for more than 30 days or with more than 20mg Sb/kg/d. One patient died suddenly during the fourth week of treatment with 60 mg Sb/kg/d, and two patients died of measles after nine or ten days of treatment with 30 mg Sb/kg/d. QT prolongation and a concave ST segment developed in all three patients who died [2]. They concluded that minor ECG abnormalities are common when sodium stibogluconate is used at doses above 20 mg Sb/kg/d for more than 15 days, and life-threatening arrhythmias may occur if very high doses are used [2].
Lawn et al. (2006) described an 81-year-old patient with hypertension and cardiomegaly who underwent the treatment of leishmania and presented ventricular arrhythmias. The arrhythmias were associated with the use of a thiazide diuretic that caused a reduction in plasma potassium levels during treatment [5].
Lawn et al. reported that the risk of QTc prolongation and arrhythmias is important for the identification of changes before and during treatment. They evaluated serial ECGs from 60 patients available for analysis, and none of these developed adverse clinical events. Abnormalities developed in the ECGs of 32 patients (53%), 27 years among males and 23 years among females. They discovered that T wave flattening developed in the ECGs of 31 patients (52%) and, in general, persisted throughout the remaining treatment course. The median duration between starting treatment and onset of T wave changes was 14 days (range 3-23 days). Among these patients, biphasic or inverted T waves were seen in 8 patients (13%). No patients developed ST-segment changes. First-degree heart block was observed in one patient on days 7-9 of treatment but resolved spontaneously. The mean QTc progressively increased during treatment from a baseline of 389 msec to 404 msec after three weeks of treatment. Six patients treated for CL developed significant asymptomatic QTc prolongation in the third week of treatment and were all potentially at higher risk of arrhythmias. No electrolyte abnormalities were detected among these patients and none developed adverse events. No patients treated for ≥28 days for ML developed significant QTc prolongation. Therefore, they offered that treatment should be discontinued if the QTc interval prolongation exceeds 450 ms [5].
Sadeghian et al. reported electrocardiographic changes among 130 patients who received glucantime for the treatment of leishmania. Their results indicated QTc prolongation in 19% of the patients, bradycardia in 10.6%, ST depression in 6.1%, minimal ST elevation in 3%, inverted T wave in 7.4%, PVC in 2.99%, PAC in 0.7%, and LBBB in 0.7% of them. First-degree and second-degree blocks were not detected. All these changes reversed soon, except in one case with LBBB, which lasted for a month after the treatment was stopped [6].
Another study by Ribeiro et al. showed that the only cardiac side effect of administrating short-term and low-dose glucantime (15 mg/kg/day) was prolonged QT [7].
They studied the cardiotoxicity of low-dose, short-term therapy with meglumine in cutaneous Leishmaniosis in 62 CL patients. A standard ECG was obtained before and immediately after the first cycle of treatment (15 mg Sb5+ kg-1 day-1). There were no significant differences in qualitative ECG variables before and after meglumine treatment. However, the corrected QT interval was clearly prolonged after antimonial therapy. QTc augmentation exceeded 40 ms in 12 patients, of whom seven patients developed marked QTc interval enlargement (500 ms) after meglumine therapy. This unrecognized cardiac toxicity induced by short-term, low-dose antimonial therapy has potentially important clinical implications [6]. They expressed that because sudden death was related to QTc prolongation over 500 ms induced by high-dose antimonial therapy, routine electrocardiographic monitoring should be done even in CL patients treated with short-term, low-dose meglumine schedules. They suggested that until further studies are conducted to establish the interactions between pentavalent antimonials and other drugs, special care is recommended when using meglumine in combination with other medications, in particular with drugs that also increase the QTc interval [6].
Because significant cardiac toxicity caused by low-dose and short-term use of glucantime is rare, its administration is considered safe. It is proposed that cardiac monitoring would not be necessary for patients receiving 10 mgSsb5+/kg/day up to 30 days or 20mgSb5+/kg/ day up to 20 days [3]. On the other hand, in certain studies, weekly ECG monitoring is recommended for patients treated for more than 20 days [8].
In a study by Zeballos et al., 45% of the patients who were treated with glucantime had echocardiographic changes in electrocardiography (T wave and ST-segment changes), which reversed two months after stopping the treatment [8].
In some studies, administration of glucantime 20mg/kg/day for 30 days for the treatment of visceral Leishmaniosis has been considered safe, and the only significant cardiac side effect was bradycardia, which was reversible. It is suggested that in conditions with low-level health facilities, pulse rate monitoring during antimonial therapy would help to detect cardiotoxicity [9].
Oliveiraa et al. in a systematic review showed that electrocardiographic QTc interval prolongation and a mild to moderate increase in liver and pancreatic enzymes were additional adverse effects of pentavalent antimonials. Therefore, if not detected early, may cause sudden and fatal arrhythmia and was the most frequent electrocardiographic adverse effect. They believed that weekly ECG monitoring should be sufficient to prevent this condition. They, therefore, suggested ECG and serum potassium monitoring be performed at least once a week in older patients or those with cardiac conditions [4].
There was no case of hospitalization or death due to arrhythmias. However, prolonged QTc interval and ST-segment changes were the most common electrocardiographic abnormalities in patients. In our case, there were three cardiac complications during treatment and one of them was not improved. In all relevant studies, there is not a report of RBBB in patients who received glucantime. In the present study, RBBB was one of the ECG changes and it was present for six months. It should be more cautiously evaluated in the EKG of glucantime-treated patients.
3. Conclusion
According to the results, ECG changes, including RBBB, first-degree block, and prolonged QT were detected in a child treated with glucantime for two treatment periods. It indicates the necessity of ECG monitoring prior to and during the treatment with this drug. Moreover, RBBB has not been commonly reported in other cases and other studies. Thus, it should be considered as one of the cardiac side effects of glucantime and needs more attention.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any specific grant fromfunding agencies in the public, commercial, or not-forprofit sectors.
Authors' contributions
All authors contributed in preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
References
- Sundar S, Chakravarty J. An update on pharmacotherapy for leishmaniasis. Expert Opinion on Pharmacotherapy. 2015; 16(2):237-52. [DOI:10.1517/14656566.2015.973850] [PMID] [PMCID]
- Chulay JD, Spencer HC, Mugambi M. Electrocardiographic changes during treatment of leishmaniasis with pentavalent antimony (sodium stibogluconate). The American journal of Tropical Medicine and Hygiene. 1985; 34(4):702-9. [DOI:10.4269/ajtmh.1985.34.702] [PMID]
- Third Annual Course on Lasers in Cutaneous and Cosmetic Surgery, 7-9 June 1996, University of California, San Francisco, California. Clinical and Experimental Dermatology. 1996; 1:80. [DOI:10.1111/j.1365-2230.1996.tb00024.x]
- Oliveira LF, Schubach AO, Martins MM, Passos SL, Oliveira RV, Marzochi MC, et al. Systematic review of the adverse effects of cutaneous leishmaniasis treatment in the New World. Acta Tropica. 2011; 118(2):87-96. [DOI:10.1016/j.actatropica.2011.02.007] [PMID]
- Lawn SD, Armstrong M, Chilton D, Whitty CJ. Electrocardiographic and biochemical adverse effects of sodium stibogluconate during treatment of cutaneous and mucosal leishmaniasis among returned travellers. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2006; 100(3):264-9. [DOI:10.1016/j.trstmh.2005.03.012] [PMID]
- Sadeghian G, Ziaei H, Sadeghi M. Electrocardiographic changes in patients with cutaneous leishmaniasis treated with systemic glucantime. Annals Academy of Medicine Singapore. 2008; 37(11):916-8. [PMID]
- Ribeiro AL, Drummond JB, Volpini AC, Andrade AC, Passos VM. Electrocardiographic changes during low-dose, short-term therapy of cutaneous leishmaniasis with the pentavalent antimonial meglumine. Brazilian Journal of Medical and Biological Research. 1999; 32(3):297-301. [PMID]
- Antezana G, Zeballos R, Mendoza C, Lyevre P, Valda L, Cardenas F, et al. Electrocardiographic alterations during treatment of mucocutaneous leishmaniasis with meglumine antimoniate and allopurinol. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1992; 86(1):31-3. [DOI:10.1016/0035-9203(92)90427-E]
- Berhe N, Abraham Y, Hailu A, Ali A, Mengistu G, Tsige K, et al. Electrocardiographic findings in Ethiopians on pentavalent antimony therapy for visceral leishmaniasis. East African Medical Journal. 2001; 78(11):608-10. [PMID]
Type of Study: Case Report and Review of Literature |
Subject:
Cardiology
Received: 2021/02/14 | Accepted: 2022/04/20 | Published: 2022/04/25
Received: 2021/02/14 | Accepted: 2022/04/20 | Published: 2022/04/25
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |