Volume 11, Issue 3 (7-2023)
J. Pediatr. Rev 2023, 11(3): 279-288 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kahouei M, Momeni M, Pahlevanynejad S, Rahaei F, Soltani-Kermanshahi M, Yaghoobi S S. Improving Healthcare Delivery to Patients With Coronavirus by Enhancing Digital Health Literacy of Healthcare Providers: Implications for Healthcare Policymakers. J. Pediatr. Rev 2023; 11 (3) :279-288
URL: http://jpr.mazums.ac.ir/article-1-448-en.html
URL: http://jpr.mazums.ac.ir/article-1-448-en.html
Mehdi Kahouei1 

 , Marjan Momeni2
, Marjan Momeni2 

 , Shahrbanoo Pahlevanynejad *3
, Shahrbanoo Pahlevanynejad *3 

 , Fatemeh Rahaei4
, Fatemeh Rahaei4 

 , Mojtaba Soltani-Kermanshahi1
, Mojtaba Soltani-Kermanshahi1 

 , Samira Sadat Yaghoobi5
, Samira Sadat Yaghoobi5 




 , Marjan Momeni2
, Marjan Momeni2 

 , Shahrbanoo Pahlevanynejad *3
, Shahrbanoo Pahlevanynejad *3 

 , Fatemeh Rahaei4
, Fatemeh Rahaei4 

 , Mojtaba Soltani-Kermanshahi1
, Mojtaba Soltani-Kermanshahi1 

 , Samira Sadat Yaghoobi5
, Samira Sadat Yaghoobi5 


1- Social Determinants of Health Research Center, Semnan University of Medical Sciences, Semnan, Iran.
2- Department of Rehabilitation, School of Rehabilitation, Semnan University of Medical Sciences, Semnan, Iran.
3- Department of Health Information Technology, School of Allied Medical Sciences, Semnan University of Medical Sciences, Semnan, Iran. ,shpahlevany@gmail.com
4- Deputy of Research and Technology, Semnan University of Medical Sciences, Semnan, Iran.
5- Department of Health Information Technology, Velayat Hospital, Semnan University of Medical Sciences, Semnan, Iran.
2- Department of Rehabilitation, School of Rehabilitation, Semnan University of Medical Sciences, Semnan, Iran.
3- Department of Health Information Technology, School of Allied Medical Sciences, Semnan University of Medical Sciences, Semnan, Iran. ,
4- Deputy of Research and Technology, Semnan University of Medical Sciences, Semnan, Iran.
5- Department of Health Information Technology, Velayat Hospital, Semnan University of Medical Sciences, Semnan, Iran.
Full-Text [PDF 654 kb]
(1522 Downloads)
| Abstract (HTML) (3370 Views)
Full-Text: (729 Views)
Introduction
Roughly 80 years after the MERS-CoV outbreak, the novel coronavirus 2019 (COVID-19) epidemic in Wuhan City, Hubei Province, China, has occurred as a worldwide outbreak and turned into a critical community health problem [1]. On January 30, 2020, the World Health Organization (WHO) announced COVID-19 as a community health crisis of worldwide concern [2]. Amazingly, in the first week of March, COVID-19 was declared a pandemic. Since March 12, 2020, over 125000 patients have been reported in 118 countries, with more than 4600 mortalities [3].
The transmission of the MERS infection happened in healthcare settings in a few countries [4, 5]. In healthcare settings, nursing and allied health staff (NAHS) are essential with patient interaction and significant resources for contact with contaminated cases. In this manner, NAHS is expected to be in high danger of infection [6]. Hence, the staff should be taught and prepared in disease prevention and control and retrain their abilities regularly [7].
The WHO started a few online instructional courses and materials on COVID-19 in different dialects to fortify preventive procedures, bring issues to light, and train and prepare NAHS [3]. Al Sahafi and Cheng’s study in Saudi Arabia was performed among healthcare workers to assess their familiarity with the MERS coronavirus since the healthcare workers’ awareness of emerging MERS coronavirus was poor [8]. Right now, the immense assorted variety of data accessible through the Internet, containing unconfirmed pernicious data, can spread rapidly and misguide NAHS [9]. Alsulaiman’s investigation indicated that around 39% of students went first to the Internet, most likely Google and Yahoo, to look for coronavirus data [10].
COVID-19 is a worldwide subject of conversation in the media and among people, particularly among NAHS and patients. Using online social media during an emergency can give quick and clear messages, increasing quality [11]. An investigation by Ruggiero and Vos shows that checking and examining online social networks during an emergency is one of the most significant strides in dealing with a crisis [12].
False impressions among NAHS defer controlling endeavors to deliver important treatment [13], lead to the quick spread of contamination in clinical settings [1], and endanger patients’ lives. Relying on valid sources is key to accepting clear data about the emerging COVID-19 contamination and is basic for NAHS readiness and reaction. Specifically, health specialists and researchers have cautioned that extensive incorrect information about COVID-19 is a solemn concern causing xenophobia [14]. This finding is in line with the Pew research report that discovered individuals have less certainty and belief in the data they get from web-based social networks [15]. People must develop complex capacities to find, understand, and assess trustworthy data about their health status [16]. Digital health literacy is the capacity to look for and comprehend health data from an electronic resource, apply the acquired knowledge, and resolve a health issue [17].
Unenviably, contamination control measures are fundamental for preventing disease spread in healthcare settings [18]. Human behavior is affected by information and insight. Contamination counteraction and prevention rely upon awareness and obedience to NAHS at all levels [6]. A study in South Korea found that poor healthcare workers’ knowledge about the transmission methods affects the fast spread of the disease in hospitals [19]. Having the composite abilities of digital health literacy permits health clients not exclusively to increase the accessibility of health data but to accomplish positive-health results, for example, health practices, self-management of health requirements, and comprehension of the infection [20, 21].
COVID-19 infection in Iran was officially confirmed on February 18, 2020. On March 4, 2020, the Ministry of Health and Medical Education executed a series of preventive measures to constrain the spread of COVID-19. The Ministry sent instant messages by cell phone to refresh the general population’s awareness. On April 11, 2020, the Ministry of Health and Medical Education of Iran announced that 58266 patients with COVID-19 had been identified in the country, of whom 3603 died and 22011 recovered [21]. In this regard, NAHS ought to know about all processes concerning the prevention of COVID-19. Hence they should assess COVID-19-related data and utilize logical and accurate content as data sources.
Purpose of the present study
This study investigates the impact of digital health literacy and other determinants on NAHS preventive behaviors of COVID-19 infection. The specific research hypotheses were as follows:
H1: The NAHS sociodemographic characteristics directly and positively affect their preventive behaviors.
H2: The NAHS digital health literacy has a direct and positive relationship with their preventive behaviors.
This study can strongly commend efficient strategies to control COVID-19 infections in healthcare settings.
Methods
Study design
This cross-sectional study was conducted for 3 months (from February 2020 to May 2020) and surveyed allied health and nursing staff working in healthcare settings, whether full or part-time, at Semnan University of Medical Sciences, Iran. All the allied health and nursing staff working in healthcare settings of Semnan University of Medical Sciences, like other staff across the country, were trained by a national education system, had access to the Internet, and were using the COVID-19 infection prevention protocol prepared by the Health Ministry of Iran. All workers, including nurses, allied health, and administrative staff, were eligible to participate in this study. Students and participants who did not use the Internet were excluded from the study.
Study sample
Considering digital health literacy as the principal variable, preventive behaviors (94.2%) from the nearest study, and the “coefficient of determination” or “R-squared value” of digital health literacy on other variables, 187 study subjects were estimated as the sample size by the PASS software [22, 23]. The total number of estimated samples was multiplied by 1.5 (design effect) to address the variation among different stages [24, 25]. A 10% attrition rate was also assumed, and the final sample size increased to 310 participants. In our calculation, type I error and power were reported as 5% and 80%, respectively.
Study outcomes
The sociodemographic characteristics such as age, sex, job, education level, general health, an underlying disease (such as heart disease, pulmonary disease, and diabetes), having old people (older than 65 years) in the family, and English language skills were recorded. Our primary outcomes were evaluating nursing and allied health staff’s digital health literacy and preventive behaviors from COVID-19 infection.
Study instruments
Since this topic was relatively new in COVID-19 and there was a lack of a comprehensive and standard tool for examining COVID-19 perspectives on this topic, a researcher-made questionnaire (preventive behaviors) and a validated questionnaire (digital health literacy) were used for data collection. The descriptions of our instruments are as below.
The first questionnaire was used to measure digital health literacy. In this study, the Persian version of digital health literacy was validated (Cronbach α=0.886) by Bazm et al. [25]. The digital health literacy questionnaire involves an 8-item self-reported measure of perceived digital health literacy: “I know what health resources are available on the internet”, “I know where to find helpful health resources on the internet”, “I know how to find helpful information about health resources on the internet”, “I know how to use the health information I find on the internet to help me”, “I know how to use the Internet to answer my health questions”, “I have the skills I need to evaluate the health resources I find on the internet”, “I can tell high quality from low-quality health resources on the internet”, and “I feel confident in using information from the internet to make health decisions.” Participants signify their level of agreement with e-health statements on a 5-point Likert-type scale (strongly disagree=1, disagree=2, somewhat=3, agree =4, and strongly agree=5). The range of total scores of the questionnaire was from 8 to 40. In this study, the level of digital health literacy was classified into three levels [26]: Insufficient digital health literacy (score <24) based on the two lower scores of the 5-point Likert scale (“strongly disagree” and “disagree”), border digital health literacy (24≤ score <32) based on the scale score of “somewhat”, and sufficient digital health literacy (score ≥32) based on the two higher scores of the 5-point Likert scale (“agree” and “strongly agree”).
The preventive behaviors questionnaire was closed-ended. The initial questionnaire was implemented by reviewing related texts, articles and interviewing experts. The questionnaire has 15 multiple-choice questions to assess the participants’ preventive behaviors for COVID-19: “I wash my hands when in contact with objects”, “I cover my mouth when I sneeze or cough”, “I avoid shaking hands and kissing”, “I use a mask in crowded areas”, “I use masks in contaminated areas”, “I avoid an unnecessary presence in crowded areas”, “I avoid unnecessary trips”, “I disinfect objects and surfaces that are often touched”, “I avoid people who are suspected of having the disease”, “If someone in my family has COVID-19, I will take precautionary measures”, “I avoid close contact with others”, “I refer suspicious cases of COVID-19 to health care centers”, “I avoid contact with animals that carry the virus”, “I avoid eating mammals and fish raw or undercooked”, and “If I have a cough, fever, or shortness of breath, see a doctor right away”. The behavior score was measured for each item on a 4-point Likert-type scale, where never=1, seldom=2, sometimes=3, and always=4. A low score was considered poor behavior, while a high score was considered good behavior.
We also asked about some sociodemographic characteristics of the participants, such as age, sex, job, education level, general health, an underlying disease (such as heart disease, pulmonary disease, and diabetes), having old people (older than 65 years) in the family, and English language skills.
The authors developed and validated the researcher-made questionnaires in three steps: Developing the initial questionnaire, evaluating their face and content validity, and examining the tool’s reliability in a pilot study.
Initial questionnaire
The original questionnaire was developed after reviewing relevant texts and articles [5, 6, 8] and interviewing some experts to determine the important items related to the study topic. After converting each item into a separate question, the researcher developed the initial questionnaire with the same number of questions.
Face validity
The face validity of the initial questionnaire was ensured using a qualitative method by6 experts in epidemiology, virology, microbiology, health, librarianship, and Persian Language. They were asked to write their comments about the difficulty, inappropriateness, and ambiguity of the phrases or words.
Content validity
Content validity examines whether the full content of a construct is represented in a measure or if some dimensions are left out [26]. To test the content validity, 10 experts were asked to evaluate the questionnaire, and the results were used to calculate the content validity ratio (CVR) and content validity index (CVI). Since the number of specialists was 10, the cut-off point for CVR was taken to be 0.62.
Reliability
Internal consistency was measured in this study to evaluate the reliability of the questionnaires. Internal consistency examines the complementary nature of items through a search for contradictions and measurement errors. The internal consistency of the overall scores was calculated along with the Cronbach α in 30 nursing staff working in healthcare settings. A high positive value of Cronbach α (0.7) suggests that the questionnaire scores are consistent [27]. Further revisions were also made, and some statements were rephrased. The final questionnaires were distributed among the allied health and nursing staff in healthcare settings and returned to the researcher.
Statistical analysis
Data were reviewed daily for completeness and accuracy, then analyzed using SPSS software, version 21. The Mean±SD or frequency (percentage) was used for data expression. Statistical analyses were performed by calculating Cronbach α and the intraclass correlation analysis. We also used multiple logistic models to explain the relationship between one dependent binary variable and other variables. P<0.05 was considered statistically significant.
Validity and reliability results
Minor changes were made in the initial preventive behaviors questionnaire based on the experts’ comments. Based on the medical expert’s opinions, the CVR values ranged from 0.8 to 0.90, and CVI was 0.9. These results confirmed the questionnaire’s content and face validity. The Cronbach α value was 0.97 with a 95% confidence interval (95% CI, 0.95%-0.98%). These results showed the establishment of questionnaire internal consistency. The questionnaire was finalized with 15 items with a range of total scores from 15 to 60 and a cut-off point 45 (a score <45 was considered low, and a score ≥45 was considered high). The questionnaires were distributed among the study subjects and were returned to the researcher. The completion of the questionnaires by the study subjects ranged from 10 to 20 minutes.
Results
A total of 310 allied health and nursing staff working in healthcare settings were randomly selected from 7 centers; 3 were excluded from the study for different reasons (unwillingness to continue or incomplete questionnaire). The data of 307 persons were ultimately analyzed. The study subjects’ mean (min-max) age was 35.80(21-55) years. The results also showed that 221 study subjects (72.0%) were female, 138(45.0%) were nurses, 238(77.5%) had bachelor’s degrees, 256(86.3%) had good status in health, 286(93.2%) lacked an underlying disease, 227(73.9%) did not have old people in their family, and 211(68.7%) had moderate skill in English language (Table 1).

Information related to preventive behaviours
The findings indicated that 291 subjects (94.8%) had good preventive behaviors, and 16(5.2%) had poor behaviors. Also, 24.8% reported washing their hands occasionally after contact with objects (Figure 1). Information related to digital health literacy
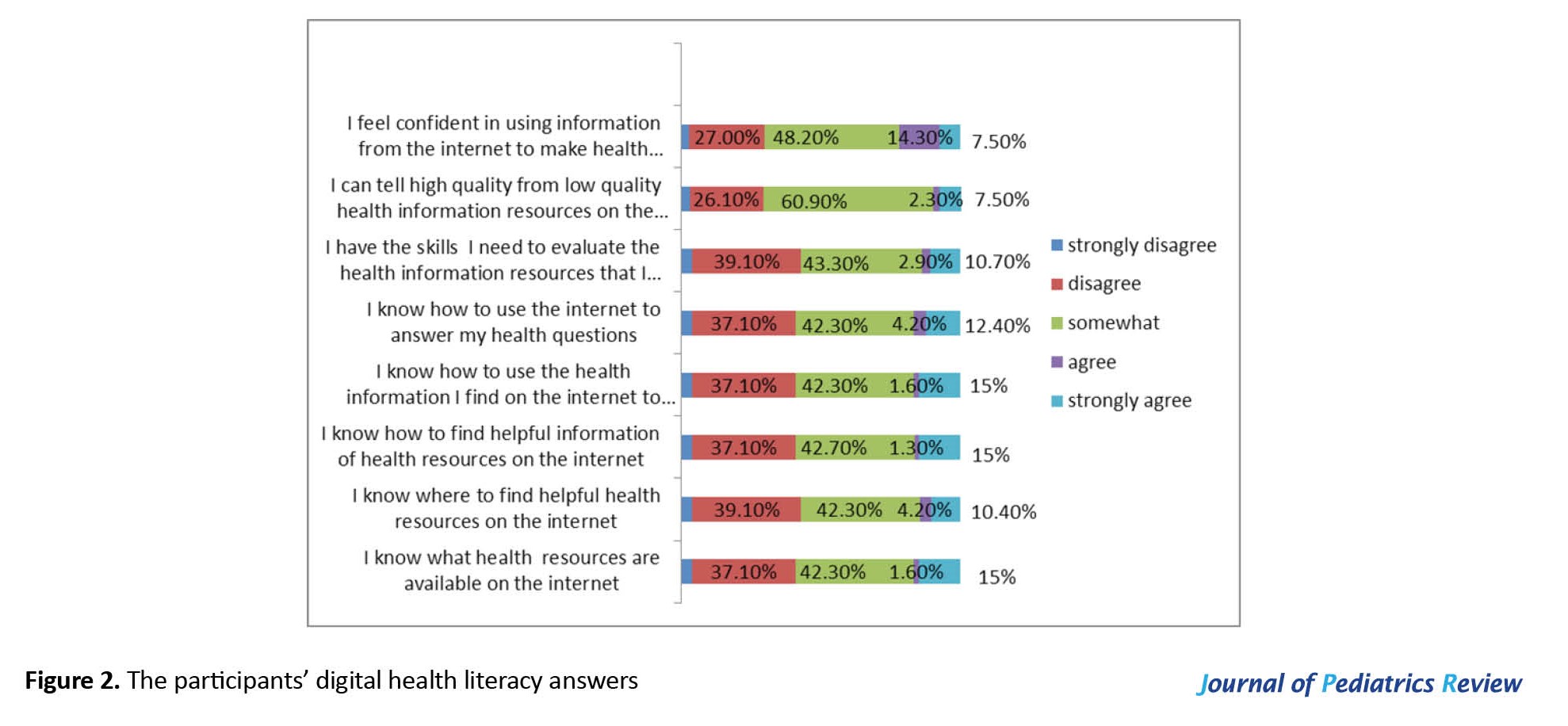
Their mean digital health literacy (min-max) was 22.8(8-40). The results showed that 42 subjects (13.7%) had sufficient digital health literacy, 137(44.6%) had borderline digital health literacy, and 128(41.7%) had insufficient digital health literacy. Also, 4.2% and 10.4% of the participants reported that they respectively agreed and strongly agreed to know where to find helpful health information resources on the Internet. About 2.9% and 10.7% agreed and strongly agreed to have skills to evaluate the health information resources they find on the Internet (Figure 2).
Relationship between sociodemographic characteristics and digital health literacy with preventive behaviors
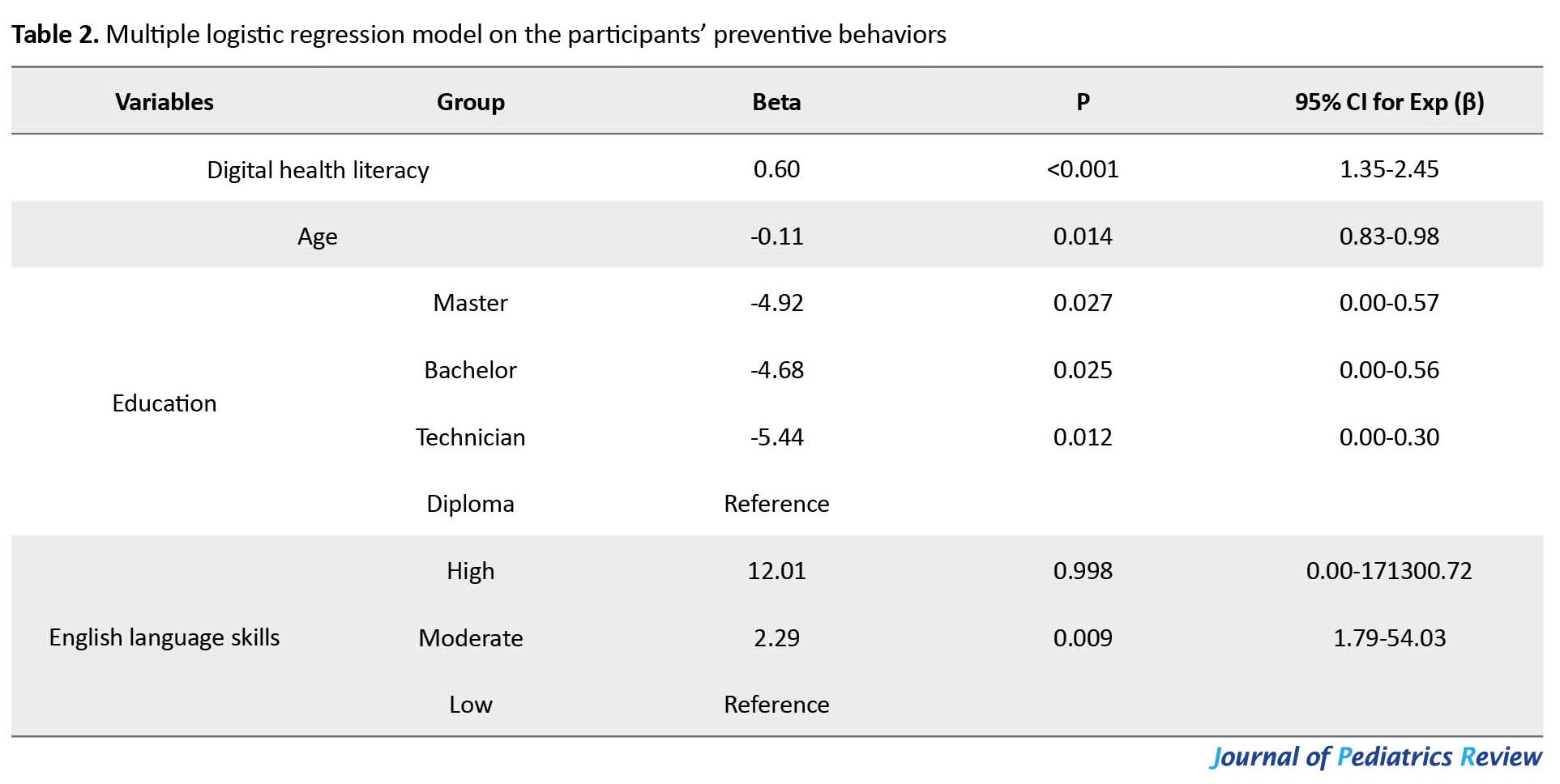
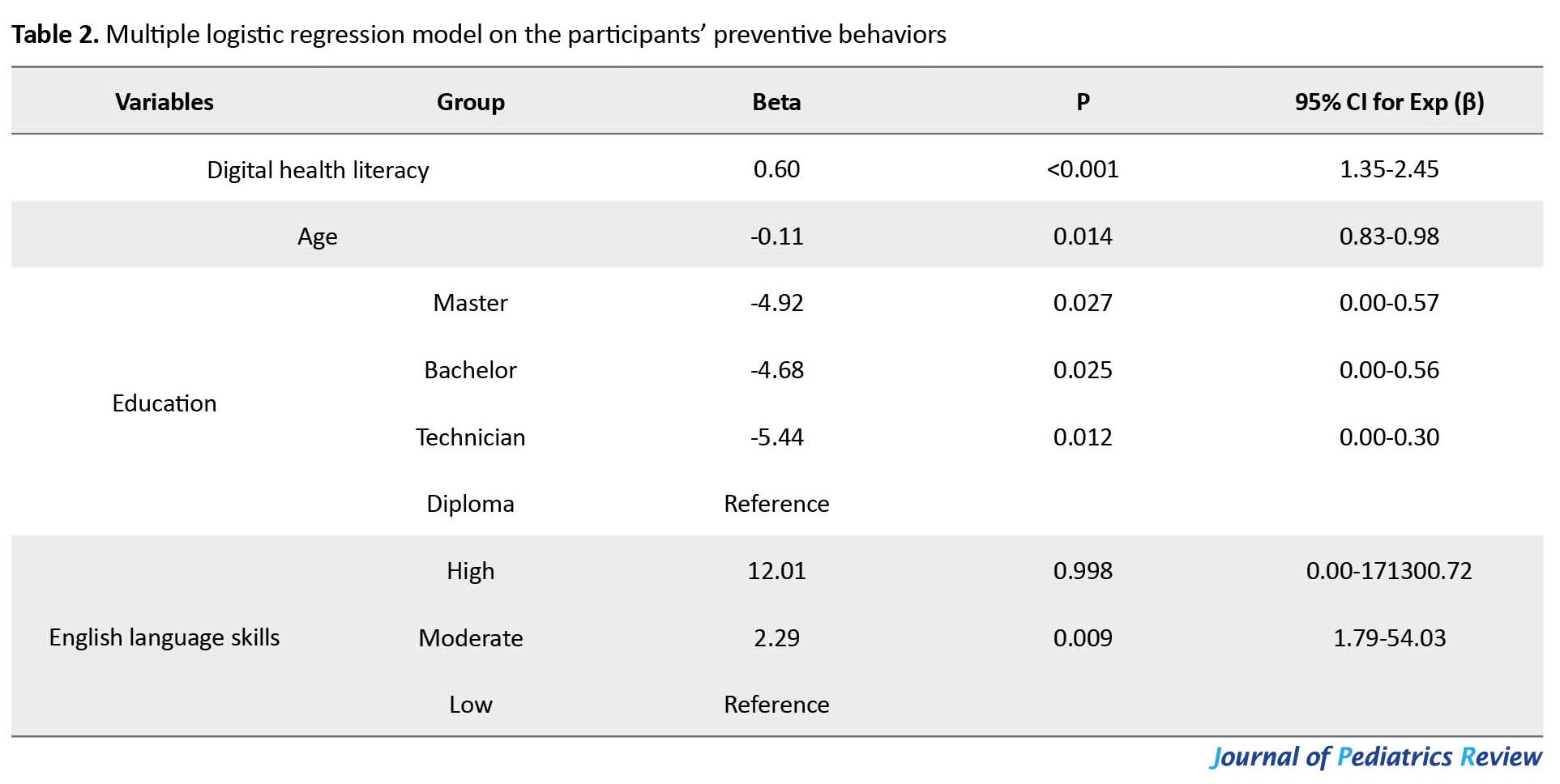
In this article, we implemented a multiple logistic regression model with dependent variable preventive behaviors (as binary). The main independent variable was digital health literacy, but we used other sociodemographic variables to adjust the effects. We performed a backward elimination method to find the final model. In the backward method, all independent variables are entered into the equation first, and each one is deleted one at a time if they do not contribute to the regression equation. The final model showed significant direct and positive relationships between digital health literacy (Beta=0.60; 95% CI, 1.35%-2.45%; P<0.001) and English language skills (Beta=2.29; 95% CI, 1.79%-54.03%; P=0.009) with preventive behaviors (Table 2).
Discussion
This research is the first study about the impact of digital health literacy on NAHS’ preventive behavior on COVID-19.
The NAHS preventive practices about COVID-19
Our study showed that about a quarter (24.8%) of the study subjects reported that sometimes they washed their hands. These findings inferred that protective measures in preventing COVID-19 infection should be reinforced. Alhomoud and Alhomoud’s examination indicated that some participants could not comply with health behaviors, especially washing hands with cleanser and water or disinfectant after sneezing/coughing and wearing a face mask in busy places [28].
The results indicated that self-reported adherence to preventive behaviors was surprisingly acceptable (94.8%). Al Alkot’s study suggests that most healthcare workers accurately distinguished the preventive measures that should be applied when managing patients to avoid disease transmission [29]. Sometimes, self-statement adherence overestimates watched practice [8].
The NAHS digital health literacy
The findings showed that a few study subjects (13.7%) had sufficient digital health literacy, and some (14.6%) knew where to find helpful online health information resources. Nursing informatics educators can help the NAHS get to health data sources for health advancement through the Internet. Likewise, by validating the messages, nursing informatics specialists can enhance the validity of awareness campaigns, as comprehended by the people focused on the campaign [30].
Emergency and crisis hazard communication models recommend that it is urgent to comprehend the populace’s hazard impression and the data resources that the people entrust them [31]. Exaggeration of dangers regularly occurs via web-based media, where profoundly passionate and frequently bogus data are shared [32].
The findings indicated that less than a quarter (13.6%) of the study subjects had the skill to evaluate the health information resources on the Internet. The findings showed that some workers in healthcare institutions need valid health data sources regarding COVID-19. The failure of the vast majority of workers to distinguish quality sources may result in indecisive decision-making to prevent disease. Balkhy et al.’s study shows that most participants are suspicious of the Saudi Ministry of Health reports about swine influenza. People with this view show undue resistance, indifference, and triviality to all recommendations [32]. It appears that informing and replying to fake information should be evidence-based and lead to rational behaviors. It also requires a precise assessment of the correctness and validity of the most ordinarily observed websites on COVID-19-related issues.
The results also showed that English language skills were a determinant (Beta=2.29, P=0.009) for preventive behaviors. This finding accepts hypothesis 1 of this study. In other words, the results showed that having moderate English language skills increases the odds of having good preventive behaviors (2.29 score). It suggests that higher English language skills help comprehend information in another language. This finding also indicates that people fluent in another language can acquire data about sickness and protective behaviors from various information resources, which cannot be promptly available to low English language skills.
The results also showed that digital health literacy was a determinant (Beta=0.60, P<0.001) for preventive behaviors. This finding accepts hypothesis 2 of this study. In other words, with a one-unit increase in digital health literacy score, the odds of having good preventive behaviors increase to 1.60. It suggests that digital health literacy is significant for accepting the preventive measures that limit the hazard exposure for the infection. Hypothetically, the health behavior style of an individual might be useful in leading individuals from awareness and comprehension of the infection’s seriousness to activity [34].
This study shows that workers with insufficient digital health literacy are more vulnerable to COVID-19 infection in healthcare settings. In any case, it suggests that a targeted health education approach is prescribed to promote digital health literacy. This should be possible by addressing society using effective and online health information sources.
The findings of this study provide intuition when planning upcoming interventions to increase digital health literacy and preventive behavior regarding COVID-19 for vulnerable individuals among workers in healthcare settings. We believe this study’s results have potentially significant implications.
Implication for nursing practice
Strengthening the workers’ digital health literacy permits them to better educate patients and accomplish positive-health results, such as health practices, self-management of health requirements, and comprehension of the infection.
Implications for the improvement of instructive interventions
The findings showed that the perception of the workers’ digital health literacy would add to the capacity of interventional and educational plans to find gaps in their knowledge. Also, nursing educators’ endeavors ought to vary according to the features of the workers.
Implications for policymakers
The outcomes gave valuable information and knowledge to help policymakers design strategic plans for COVID-19 disease control. Also, the key to improving digital health literacy is distinguishing health information-seeking behaviors; for instance, the specific source and selection of channel/media may impact receptivity to and effect of the messages.
Implications for research
Finally, this study indicates that integrating knowledge about the workers’ digital health literacy and preventive behavior from COVID-19 is basic in healthcare settings. Designing a research plan to give the intellectual base and direct upcoming practice in instructing about COVID-19 is likewise crucial.
Conclusion
This study showed that consolidating workers’ digital health literacy can reduce the spread of COVID-19 infections in healthcare settings. Nursing informatics specialists and educators are proposed to prepare e-health policies to advance digital health literacy in healthcare settings. Also, there was an acknowledgment in the workers of the requirement for additional instruction and training, especially in the utilization of valid online health information sources. Continuing endeavors coordinated by nursing managers are required and should concentrate on these issues.
Limitations and future studies
This study has a few limitations that should be considered. First, the data in this survey are self-reported and somewhat reliant on the study subjects’ honesty; accordingly, it might be subject to recall bias. Second, our small sample size may have constrained our capacity to identify other significant differences that may influence the connections among variables. Further research is expected to evaluate these connections in larger samples of NAHS. Third, despite these limitations, this study was the first investigation to include significant data in the endeavors for COVID-19 control as it emphasizes the strength and weaknesses in digital health literacy and preventive behavior of the NAHS regarding COVID-19. Also, the results aid policymakers in planning upcoming interventions. Finally, it is also an issue considering the generalization of this study’s results to all NAHS because of the inadequate study sample, which has been limited to the NAHS of a region. Given the nursing staff’s role in patient education, future work needs to do as insufficient digital health literacy is increasingly prevalent in society. In addition, future investigations are required to examine the quality and correctness of health data found on the Internet. Likewise, investigating and comprehending the cultural components of health training and advancement is essential.
Ethical Considerations
Compliance with ethical guidelines
The Ethics Committee of Semnan University of Medical Sciences approved the study (Code: I.R.SEMUMS.REC.1398.295). A cover letter was prepared for distribution with the survey document, which described the purpose of the study and explained that a response to the survey would indicate the participant’s consent to participate in the research. It also assured participants’ confidentiality of their responses.
Funding
The Semnan University of Medical Sciences funded this research.
Authors contributions
Conceptualization and supervision: Mehdi Kahouei, Marjan Momeni and Shahrbanoo Pahlevanynejad; Methodology: Mehdi Kahouei, Marjan Momeni, Shahrbanoo Pahlevanynejad and Mojtaba Soltani-Kermanshahi; Funding acquisition and resources: Mehdi Kahouei, Marjan Momeni, Mojtaba Soltani-Kermanshahi, Shahrbanoo Pahlevanynejad; Investigation, data collection, writing original draft, review & editing: All authors; Data analysis: Mehdi Kahouei; Mojtaba Soltani-Kermanshahi and Fatemeh Rahaei.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
We thank all participants who made this study possible through their assistance and guidance in this research.
References
Roughly 80 years after the MERS-CoV outbreak, the novel coronavirus 2019 (COVID-19) epidemic in Wuhan City, Hubei Province, China, has occurred as a worldwide outbreak and turned into a critical community health problem [1]. On January 30, 2020, the World Health Organization (WHO) announced COVID-19 as a community health crisis of worldwide concern [2]. Amazingly, in the first week of March, COVID-19 was declared a pandemic. Since March 12, 2020, over 125000 patients have been reported in 118 countries, with more than 4600 mortalities [3].
The transmission of the MERS infection happened in healthcare settings in a few countries [4, 5]. In healthcare settings, nursing and allied health staff (NAHS) are essential with patient interaction and significant resources for contact with contaminated cases. In this manner, NAHS is expected to be in high danger of infection [6]. Hence, the staff should be taught and prepared in disease prevention and control and retrain their abilities regularly [7].
The WHO started a few online instructional courses and materials on COVID-19 in different dialects to fortify preventive procedures, bring issues to light, and train and prepare NAHS [3]. Al Sahafi and Cheng’s study in Saudi Arabia was performed among healthcare workers to assess their familiarity with the MERS coronavirus since the healthcare workers’ awareness of emerging MERS coronavirus was poor [8]. Right now, the immense assorted variety of data accessible through the Internet, containing unconfirmed pernicious data, can spread rapidly and misguide NAHS [9]. Alsulaiman’s investigation indicated that around 39% of students went first to the Internet, most likely Google and Yahoo, to look for coronavirus data [10].
COVID-19 is a worldwide subject of conversation in the media and among people, particularly among NAHS and patients. Using online social media during an emergency can give quick and clear messages, increasing quality [11]. An investigation by Ruggiero and Vos shows that checking and examining online social networks during an emergency is one of the most significant strides in dealing with a crisis [12].
False impressions among NAHS defer controlling endeavors to deliver important treatment [13], lead to the quick spread of contamination in clinical settings [1], and endanger patients’ lives. Relying on valid sources is key to accepting clear data about the emerging COVID-19 contamination and is basic for NAHS readiness and reaction. Specifically, health specialists and researchers have cautioned that extensive incorrect information about COVID-19 is a solemn concern causing xenophobia [14]. This finding is in line with the Pew research report that discovered individuals have less certainty and belief in the data they get from web-based social networks [15]. People must develop complex capacities to find, understand, and assess trustworthy data about their health status [16]. Digital health literacy is the capacity to look for and comprehend health data from an electronic resource, apply the acquired knowledge, and resolve a health issue [17].
Unenviably, contamination control measures are fundamental for preventing disease spread in healthcare settings [18]. Human behavior is affected by information and insight. Contamination counteraction and prevention rely upon awareness and obedience to NAHS at all levels [6]. A study in South Korea found that poor healthcare workers’ knowledge about the transmission methods affects the fast spread of the disease in hospitals [19]. Having the composite abilities of digital health literacy permits health clients not exclusively to increase the accessibility of health data but to accomplish positive-health results, for example, health practices, self-management of health requirements, and comprehension of the infection [20, 21].
COVID-19 infection in Iran was officially confirmed on February 18, 2020. On March 4, 2020, the Ministry of Health and Medical Education executed a series of preventive measures to constrain the spread of COVID-19. The Ministry sent instant messages by cell phone to refresh the general population’s awareness. On April 11, 2020, the Ministry of Health and Medical Education of Iran announced that 58266 patients with COVID-19 had been identified in the country, of whom 3603 died and 22011 recovered [21]. In this regard, NAHS ought to know about all processes concerning the prevention of COVID-19. Hence they should assess COVID-19-related data and utilize logical and accurate content as data sources.
Purpose of the present study
This study investigates the impact of digital health literacy and other determinants on NAHS preventive behaviors of COVID-19 infection. The specific research hypotheses were as follows:
H1: The NAHS sociodemographic characteristics directly and positively affect their preventive behaviors.
H2: The NAHS digital health literacy has a direct and positive relationship with their preventive behaviors.
This study can strongly commend efficient strategies to control COVID-19 infections in healthcare settings.
Methods
Study design
This cross-sectional study was conducted for 3 months (from February 2020 to May 2020) and surveyed allied health and nursing staff working in healthcare settings, whether full or part-time, at Semnan University of Medical Sciences, Iran. All the allied health and nursing staff working in healthcare settings of Semnan University of Medical Sciences, like other staff across the country, were trained by a national education system, had access to the Internet, and were using the COVID-19 infection prevention protocol prepared by the Health Ministry of Iran. All workers, including nurses, allied health, and administrative staff, were eligible to participate in this study. Students and participants who did not use the Internet were excluded from the study.
Study sample
Considering digital health literacy as the principal variable, preventive behaviors (94.2%) from the nearest study, and the “coefficient of determination” or “R-squared value” of digital health literacy on other variables, 187 study subjects were estimated as the sample size by the PASS software [22, 23]. The total number of estimated samples was multiplied by 1.5 (design effect) to address the variation among different stages [24, 25]. A 10% attrition rate was also assumed, and the final sample size increased to 310 participants. In our calculation, type I error and power were reported as 5% and 80%, respectively.
Study outcomes
The sociodemographic characteristics such as age, sex, job, education level, general health, an underlying disease (such as heart disease, pulmonary disease, and diabetes), having old people (older than 65 years) in the family, and English language skills were recorded. Our primary outcomes were evaluating nursing and allied health staff’s digital health literacy and preventive behaviors from COVID-19 infection.
Study instruments
Since this topic was relatively new in COVID-19 and there was a lack of a comprehensive and standard tool for examining COVID-19 perspectives on this topic, a researcher-made questionnaire (preventive behaviors) and a validated questionnaire (digital health literacy) were used for data collection. The descriptions of our instruments are as below.
The first questionnaire was used to measure digital health literacy. In this study, the Persian version of digital health literacy was validated (Cronbach α=0.886) by Bazm et al. [25]. The digital health literacy questionnaire involves an 8-item self-reported measure of perceived digital health literacy: “I know what health resources are available on the internet”, “I know where to find helpful health resources on the internet”, “I know how to find helpful information about health resources on the internet”, “I know how to use the health information I find on the internet to help me”, “I know how to use the Internet to answer my health questions”, “I have the skills I need to evaluate the health resources I find on the internet”, “I can tell high quality from low-quality health resources on the internet”, and “I feel confident in using information from the internet to make health decisions.” Participants signify their level of agreement with e-health statements on a 5-point Likert-type scale (strongly disagree=1, disagree=2, somewhat=3, agree =4, and strongly agree=5). The range of total scores of the questionnaire was from 8 to 40. In this study, the level of digital health literacy was classified into three levels [26]: Insufficient digital health literacy (score <24) based on the two lower scores of the 5-point Likert scale (“strongly disagree” and “disagree”), border digital health literacy (24≤ score <32) based on the scale score of “somewhat”, and sufficient digital health literacy (score ≥32) based on the two higher scores of the 5-point Likert scale (“agree” and “strongly agree”).
The preventive behaviors questionnaire was closed-ended. The initial questionnaire was implemented by reviewing related texts, articles and interviewing experts. The questionnaire has 15 multiple-choice questions to assess the participants’ preventive behaviors for COVID-19: “I wash my hands when in contact with objects”, “I cover my mouth when I sneeze or cough”, “I avoid shaking hands and kissing”, “I use a mask in crowded areas”, “I use masks in contaminated areas”, “I avoid an unnecessary presence in crowded areas”, “I avoid unnecessary trips”, “I disinfect objects and surfaces that are often touched”, “I avoid people who are suspected of having the disease”, “If someone in my family has COVID-19, I will take precautionary measures”, “I avoid close contact with others”, “I refer suspicious cases of COVID-19 to health care centers”, “I avoid contact with animals that carry the virus”, “I avoid eating mammals and fish raw or undercooked”, and “If I have a cough, fever, or shortness of breath, see a doctor right away”. The behavior score was measured for each item on a 4-point Likert-type scale, where never=1, seldom=2, sometimes=3, and always=4. A low score was considered poor behavior, while a high score was considered good behavior.
We also asked about some sociodemographic characteristics of the participants, such as age, sex, job, education level, general health, an underlying disease (such as heart disease, pulmonary disease, and diabetes), having old people (older than 65 years) in the family, and English language skills.
The authors developed and validated the researcher-made questionnaires in three steps: Developing the initial questionnaire, evaluating their face and content validity, and examining the tool’s reliability in a pilot study.
Initial questionnaire
The original questionnaire was developed after reviewing relevant texts and articles [5, 6, 8] and interviewing some experts to determine the important items related to the study topic. After converting each item into a separate question, the researcher developed the initial questionnaire with the same number of questions.
Face validity
The face validity of the initial questionnaire was ensured using a qualitative method by6 experts in epidemiology, virology, microbiology, health, librarianship, and Persian Language. They were asked to write their comments about the difficulty, inappropriateness, and ambiguity of the phrases or words.
Content validity
Content validity examines whether the full content of a construct is represented in a measure or if some dimensions are left out [26]. To test the content validity, 10 experts were asked to evaluate the questionnaire, and the results were used to calculate the content validity ratio (CVR) and content validity index (CVI). Since the number of specialists was 10, the cut-off point for CVR was taken to be 0.62.
Reliability
Internal consistency was measured in this study to evaluate the reliability of the questionnaires. Internal consistency examines the complementary nature of items through a search for contradictions and measurement errors. The internal consistency of the overall scores was calculated along with the Cronbach α in 30 nursing staff working in healthcare settings. A high positive value of Cronbach α (0.7) suggests that the questionnaire scores are consistent [27]. Further revisions were also made, and some statements were rephrased. The final questionnaires were distributed among the allied health and nursing staff in healthcare settings and returned to the researcher.
Statistical analysis
Data were reviewed daily for completeness and accuracy, then analyzed using SPSS software, version 21. The Mean±SD or frequency (percentage) was used for data expression. Statistical analyses were performed by calculating Cronbach α and the intraclass correlation analysis. We also used multiple logistic models to explain the relationship between one dependent binary variable and other variables. P<0.05 was considered statistically significant.
Validity and reliability results
Minor changes were made in the initial preventive behaviors questionnaire based on the experts’ comments. Based on the medical expert’s opinions, the CVR values ranged from 0.8 to 0.90, and CVI was 0.9. These results confirmed the questionnaire’s content and face validity. The Cronbach α value was 0.97 with a 95% confidence interval (95% CI, 0.95%-0.98%). These results showed the establishment of questionnaire internal consistency. The questionnaire was finalized with 15 items with a range of total scores from 15 to 60 and a cut-off point 45 (a score <45 was considered low, and a score ≥45 was considered high). The questionnaires were distributed among the study subjects and were returned to the researcher. The completion of the questionnaires by the study subjects ranged from 10 to 20 minutes.
Results
A total of 310 allied health and nursing staff working in healthcare settings were randomly selected from 7 centers; 3 were excluded from the study for different reasons (unwillingness to continue or incomplete questionnaire). The data of 307 persons were ultimately analyzed. The study subjects’ mean (min-max) age was 35.80(21-55) years. The results also showed that 221 study subjects (72.0%) were female, 138(45.0%) were nurses, 238(77.5%) had bachelor’s degrees, 256(86.3%) had good status in health, 286(93.2%) lacked an underlying disease, 227(73.9%) did not have old people in their family, and 211(68.7%) had moderate skill in English language (Table 1).

Information related to preventive behaviours
The findings indicated that 291 subjects (94.8%) had good preventive behaviors, and 16(5.2%) had poor behaviors. Also, 24.8% reported washing their hands occasionally after contact with objects (Figure 1). Information related to digital health literacy
Their mean digital health literacy (min-max) was 22.8(8-40). The results showed that 42 subjects (13.7%) had sufficient digital health literacy, 137(44.6%) had borderline digital health literacy, and 128(41.7%) had insufficient digital health literacy. Also, 4.2% and 10.4% of the participants reported that they respectively agreed and strongly agreed to know where to find helpful health information resources on the Internet. About 2.9% and 10.7% agreed and strongly agreed to have skills to evaluate the health information resources they find on the Internet (Figure 2).
Relationship between sociodemographic characteristics and digital health literacy with preventive behaviors
In this article, we implemented a multiple logistic regression model with dependent variable preventive behaviors (as binary). The main independent variable was digital health literacy, but we used other sociodemographic variables to adjust the effects. We performed a backward elimination method to find the final model. In the backward method, all independent variables are entered into the equation first, and each one is deleted one at a time if they do not contribute to the regression equation. The final model showed significant direct and positive relationships between digital health literacy (Beta=0.60; 95% CI, 1.35%-2.45%; P<0.001) and English language skills (Beta=2.29; 95% CI, 1.79%-54.03%; P=0.009) with preventive behaviors (Table 2).
Discussion
This research is the first study about the impact of digital health literacy on NAHS’ preventive behavior on COVID-19.
The NAHS preventive practices about COVID-19
Our study showed that about a quarter (24.8%) of the study subjects reported that sometimes they washed their hands. These findings inferred that protective measures in preventing COVID-19 infection should be reinforced. Alhomoud and Alhomoud’s examination indicated that some participants could not comply with health behaviors, especially washing hands with cleanser and water or disinfectant after sneezing/coughing and wearing a face mask in busy places [28].
The results indicated that self-reported adherence to preventive behaviors was surprisingly acceptable (94.8%). Al Alkot’s study suggests that most healthcare workers accurately distinguished the preventive measures that should be applied when managing patients to avoid disease transmission [29]. Sometimes, self-statement adherence overestimates watched practice [8].
The NAHS digital health literacy
The findings showed that a few study subjects (13.7%) had sufficient digital health literacy, and some (14.6%) knew where to find helpful online health information resources. Nursing informatics educators can help the NAHS get to health data sources for health advancement through the Internet. Likewise, by validating the messages, nursing informatics specialists can enhance the validity of awareness campaigns, as comprehended by the people focused on the campaign [30].
Emergency and crisis hazard communication models recommend that it is urgent to comprehend the populace’s hazard impression and the data resources that the people entrust them [31]. Exaggeration of dangers regularly occurs via web-based media, where profoundly passionate and frequently bogus data are shared [32].
The findings indicated that less than a quarter (13.6%) of the study subjects had the skill to evaluate the health information resources on the Internet. The findings showed that some workers in healthcare institutions need valid health data sources regarding COVID-19. The failure of the vast majority of workers to distinguish quality sources may result in indecisive decision-making to prevent disease. Balkhy et al.’s study shows that most participants are suspicious of the Saudi Ministry of Health reports about swine influenza. People with this view show undue resistance, indifference, and triviality to all recommendations [32]. It appears that informing and replying to fake information should be evidence-based and lead to rational behaviors. It also requires a precise assessment of the correctness and validity of the most ordinarily observed websites on COVID-19-related issues.
The results also showed that English language skills were a determinant (Beta=2.29, P=0.009) for preventive behaviors. This finding accepts hypothesis 1 of this study. In other words, the results showed that having moderate English language skills increases the odds of having good preventive behaviors (2.29 score). It suggests that higher English language skills help comprehend information in another language. This finding also indicates that people fluent in another language can acquire data about sickness and protective behaviors from various information resources, which cannot be promptly available to low English language skills.
The results also showed that digital health literacy was a determinant (Beta=0.60, P<0.001) for preventive behaviors. This finding accepts hypothesis 2 of this study. In other words, with a one-unit increase in digital health literacy score, the odds of having good preventive behaviors increase to 1.60. It suggests that digital health literacy is significant for accepting the preventive measures that limit the hazard exposure for the infection. Hypothetically, the health behavior style of an individual might be useful in leading individuals from awareness and comprehension of the infection’s seriousness to activity [34].
This study shows that workers with insufficient digital health literacy are more vulnerable to COVID-19 infection in healthcare settings. In any case, it suggests that a targeted health education approach is prescribed to promote digital health literacy. This should be possible by addressing society using effective and online health information sources.
The findings of this study provide intuition when planning upcoming interventions to increase digital health literacy and preventive behavior regarding COVID-19 for vulnerable individuals among workers in healthcare settings. We believe this study’s results have potentially significant implications.
Implication for nursing practice
Strengthening the workers’ digital health literacy permits them to better educate patients and accomplish positive-health results, such as health practices, self-management of health requirements, and comprehension of the infection.
Implications for the improvement of instructive interventions
The findings showed that the perception of the workers’ digital health literacy would add to the capacity of interventional and educational plans to find gaps in their knowledge. Also, nursing educators’ endeavors ought to vary according to the features of the workers.
Implications for policymakers
The outcomes gave valuable information and knowledge to help policymakers design strategic plans for COVID-19 disease control. Also, the key to improving digital health literacy is distinguishing health information-seeking behaviors; for instance, the specific source and selection of channel/media may impact receptivity to and effect of the messages.
Implications for research
Finally, this study indicates that integrating knowledge about the workers’ digital health literacy and preventive behavior from COVID-19 is basic in healthcare settings. Designing a research plan to give the intellectual base and direct upcoming practice in instructing about COVID-19 is likewise crucial.
Conclusion
This study showed that consolidating workers’ digital health literacy can reduce the spread of COVID-19 infections in healthcare settings. Nursing informatics specialists and educators are proposed to prepare e-health policies to advance digital health literacy in healthcare settings. Also, there was an acknowledgment in the workers of the requirement for additional instruction and training, especially in the utilization of valid online health information sources. Continuing endeavors coordinated by nursing managers are required and should concentrate on these issues.
Limitations and future studies
This study has a few limitations that should be considered. First, the data in this survey are self-reported and somewhat reliant on the study subjects’ honesty; accordingly, it might be subject to recall bias. Second, our small sample size may have constrained our capacity to identify other significant differences that may influence the connections among variables. Further research is expected to evaluate these connections in larger samples of NAHS. Third, despite these limitations, this study was the first investigation to include significant data in the endeavors for COVID-19 control as it emphasizes the strength and weaknesses in digital health literacy and preventive behavior of the NAHS regarding COVID-19. Also, the results aid policymakers in planning upcoming interventions. Finally, it is also an issue considering the generalization of this study’s results to all NAHS because of the inadequate study sample, which has been limited to the NAHS of a region. Given the nursing staff’s role in patient education, future work needs to do as insufficient digital health literacy is increasingly prevalent in society. In addition, future investigations are required to examine the quality and correctness of health data found on the Internet. Likewise, investigating and comprehending the cultural components of health training and advancement is essential.
Ethical Considerations
Compliance with ethical guidelines
The Ethics Committee of Semnan University of Medical Sciences approved the study (Code: I.R.SEMUMS.REC.1398.295). A cover letter was prepared for distribution with the survey document, which described the purpose of the study and explained that a response to the survey would indicate the participant’s consent to participate in the research. It also assured participants’ confidentiality of their responses.
Funding
The Semnan University of Medical Sciences funded this research.
Authors contributions
Conceptualization and supervision: Mehdi Kahouei, Marjan Momeni and Shahrbanoo Pahlevanynejad; Methodology: Mehdi Kahouei, Marjan Momeni, Shahrbanoo Pahlevanynejad and Mojtaba Soltani-Kermanshahi; Funding acquisition and resources: Mehdi Kahouei, Marjan Momeni, Mojtaba Soltani-Kermanshahi, Shahrbanoo Pahlevanynejad; Investigation, data collection, writing original draft, review & editing: All authors; Data analysis: Mehdi Kahouei; Mojtaba Soltani-Kermanshahi and Fatemeh Rahaei.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
We thank all participants who made this study possible through their assistance and guidance in this research.
References
- Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents. 2020; 55(3):105924.[DOI:10.1016/j.ijantimicag.2020.105924] [PMID] [PMCID]
- Eurosurveillance editorial team. Note from the editors: World Health Organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Euro Surveill. 2020; 25(5):200131e. [DOI:10.2807/1560-7917.ES.2020.25.5.200131e] [PMID]
- Landry MD, Tupetz A, Jalovcic D, Sheppard P, Jesus TS, Raman SR. The novel coronavirus (COVID-19): Making a connection between infectious disease outbreaks and rehabilitation. Physiother Can. 2020; 72(4):325-7. [DOI:10.3138/ptc-2020-0019] [PMID] [PMCID]
- Memish ZA, Zumla AI, Assiri A. Middle East respiratory syndrome coronavirus infections in health care workers. N Engl J Med. 2013; 369(9):884-6.[DOI:10.1056/NEJMc1308698] [PMID]
- Assiri A, McGeer A, Perl TM, Price CS, Al Rabeeah AA, Cummings DA, et al. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med. 2013; 369(5):407-16. [DOI:10.1056/NEJMoa1306742] [PMID] [PMCID]
- Asaad A, El-Sokkary R, Alzamanan M, El-Shafei M. Knowledge and attitudes towards Middle East respiratory sydrome-coronavirus (MERS-CoV) among health care workers in south-western Saudi Arabia. East Mediterr Health J. 2020; 26(4):435-42. [DOI:10.26719/emhj.19.079] [PMID]
- Chang D, Xu H, Rebaza A, Sharma L, Dela Cruz CS. Protecting health-care workers from subclinical coronavirus infection. Lancet Respir Med. 2020; 8(3):e13. [DOI:10.1016/S2213-2600(20)30066-7] [PMID]
- Alsahafi AJ, Cheng AC. Knowledge, attitudes and behaviours of healthcare workers in the kingdom of Saudi Arabia to MERS Coronavirus and other emerging infectious diseases. Int J Environ Res Public Health. 2016; 13(12):1214. [DOI:10.3390/ijerph13121214] [PMID] [PMCID]
- Kharma MY, Alalwani MS, Amer MF, Tarakji B, Aws G. Assessment of the awareness level of dental students toward Middle East Respiratory Syndrome-coronavirus. J Int Soc Prev Community Dent. 2015; 5(3):163-9.[DOI:10.4103/2231-0762.159951] [PMID] [PMCID]
- Alsulaiman SA. Health crisis in the kingdom of Saudi Arabia: A study of Saudis’ knowledge of Coronavirus, attitudes toward the ministry of health’s coronavirus preventive campaigns, and trust in coronavirus messages in the media. [PhD Thesis]. Bowling Green: Bowling Green State University; 2018. [Link]
- Bazrafshani A, Panahi S, Sharifi H, Merghati-Khoei E. The role of online social networks in improving health literacy and medication adherence among people living with HIV/AIDS in Iran: Development of a conceptual model. Plos one. 2022; 17(6):e0261304. [DOI:10.1371/journal.pone.0261304] [PMID]
- Ruggiero A, Vos M. Social media monitoring for crisis communication: Process, methods and trends in the scientific literature. Online J Commun Media Technol. 2014; 4(1):105-30. [DOI:10.29333/ojcmt/2457]
- Hoffman SJ, Silverberg SL. Delays in global disease outbreak responses: Lessons from H1N1, Ebola, and Zika. Am J Public Health. 2018; 108(3):329-33. [DOI:10.2105/AJPH.2017.304245] [PMID] [PMCID]
- Shimizu K. 2019-nCoV, fake news, and racism. Lancet. 2020; 395(10225):685-6. [DOI:10.1016/S0140-6736(20)30357-3] [PMID]
- Kohut A, Doherty C, Dimock M, Keeter S. Press widely criticized, but trusted more than other information sources. Views of the news media: 1985-2011. Washington: The Pew Research Center; 2011. [Link]
- Yee KC, Wong MC, Turner P. Understanding how clinical judgement and communicative practices interact with the use of an electronic clinical handover system. In: Grain H, Schaper LK, editors. Health information: Digital health service delivery-the future is now. Amesterdam: IOS Press; 2013. [Link]
- Norman CD, Skinner HA. eHEALS: The ehealth literacy scale. J Med Internet Res. 2006; 8(4):e27.[DOI:10.2196/jmir.8.4.e27] [PMID] [PMCID]
- Joshi RM. Middle East respiratory syndrome Coronavirus (MERS-CoV): Perceptions, predictions, preventions and the pilgrimage. Clin Mic. 2012; 02(06):1000e113. [DOI:10.4172/2327-5073.1000e113]
- Kim SG. [Healthcare workers infected with Middle East respiratory syndrome coronavirus and infection control (Korean)]. J Korean Med Assoc. 2015; 58(7):647-54. [DOI:10.5124/jkma.2015.58.7.647]
- Knapp C, Madden V, Wang H, Sloyer P, Shenkman E. Internet use and ehealth literacy of low-income parents whose children have special health care needs. J Med Internet Res. 2011; 13(3):e75. [DOI:10.2196/jmir.1697] [PMID] [PMCID]
- Mitsutake S, Shibata A, Ishii K, Oka K. Associations of ehealth literacy with health behavior among adult internet users. J Med Internet Res. 2016; 18(7):e192. [DOI:10.2196/jmir.5413] [PMID] [PMCID]
- Hintze J. User’s guide I quick start, proportions, and diagnostic tests. Power analysis and sample size (PASS). Singapore: National Council of Social Service; 2006. [Link]
- Taghrir MH, Borazjani R, Shiraly R. COVID-19 and Iranian medical students; A survey on their related-knowledge, preventive behaviors and risk perception. Arch Iran Med. 2020; 23(4):249-54. [DOI:10.34172/aim.2020.06] [PMID]
- Boddy CR. Sample size for qualitative research. Qual Mark Res An Int J. 2016; 19(4):426-32. [DOI:10.1108/QMR-06-2016-0053]
- Bazm S, Mirzaei M, Fallahzadeh H, Bazm R. Validity and reliability of Iranian version of eHealth literacy scale. J Commun Health Res. 2016; 5(2):121-30. [Link]
- Brinkman WP. Design of a Questionnaire Instrument. New York: Nova Publisher; 2009. [Link]
- Cronbach LJ. Coefficient alpha and the internal structure of tests. Plksychometrika. 1951; 16(3):297-334. [DOI:10.1007/BF02310555]
- Alhomoud F, Alhomoud F. Your health essential for your Hajj: Muslim pilgrims' knowledge, attitudes and practices regarding Middle East respiratory syndrome coronavirus (MERS-CoV) during Hajj season. J Infect Chemother. 2017; 23(5):286-92. [DOI:10.1016/j.jiac.2017.01.006] [PMID] [PMCID]
- Alkot M, Albouq MA, Shakuri MA, Subahi MS. Knowledge, attitude, and practice toward MERS-CoV among primary healthcare workers in Makkah Al-Mukarramah: An intervention study. Int J Med Sci Public Heal. 2016; 5(5):952-59. [DOI:10.5455/ijmsph.2016.24012016345]
- Hoda J. Identification of information types and sources by the public for promoting awareness of Middle East respiratory syndrome coronavirus in Saudi Arabia. Health Educ Res. 2016; 31(1):12-23. [DOI:10.1093/her/cyv061] [PMID] [PMCID]
- Kamau E, Ongus J, Gitau G, Galgalo T, Lowther SA, Bitek A, et al. Knowledge and practices regarding Middle East respiratory syndrome Coronavirus among camel handlers in a Slaughterhouse, Kenya, 2015. Zoonoses Public Health. 2019; 66(1):169-73. [DOI:10.1111/zph.12524] [PMID] [PMCID]
- Vosoughi S, Roy D, Aral S. The spread of true and false news online. Science. 2018; 359(6380):1146-51. [DOI:10.1126/science.aap9559] [PMID]
- Balkhy HH, Abolfotouh MA, Al-Hathlool RH, Al-Jumah MA. Awareness, attitudes, and practices related to the swine influenza pandemic among the Saudi public. BMC Infect Dis. 2010; 10:42. [DOI:10.1186/1471-2334-10-42] [PMID] [PMCID]
- Sudha P, Reddy B, Kumar S. Problem solving coping style in relation to personality type, health behavior and life satisfaction among cardiovascular patients. Indian J Health Wellbeing. 2017; 8(12):1493-6. [Link]
Type of Study: Original Article |
Subject:
Infectious Diseases
Received: 2021/12/19 | Accepted: 2023/03/5 | Published: 2023/07/1
Received: 2021/12/19 | Accepted: 2023/03/5 | Published: 2023/07/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |