Volume 11, Issue 2 (4-2023)
J. Pediatr. Rev 2023, 11(2): 117-124 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nickavar A, Valavi E, Sadigh N. Urine Neutrophil Gelatinase Associated Lipocalin as a Predictor of Vesicoureteral Reflux and Renal Parenchymal Damage: A Systematic Review. J. Pediatr. Rev 2023; 11 (2) :117-124
URL: http://jpr.mazums.ac.ir/article-1-514-en.html
URL: http://jpr.mazums.ac.ir/article-1-514-en.html
1- Department of Pediatric Nephrology, School of Medicine, Aliasghar Children’s Hospital, Iran University of Medical Sciences, Tehran, Iran.
2- Chronic Renal Failure Research Center, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
3- Department of Emergency, School of Medicine, Aliasghar Children’s Hospital, Iran University of Medical Sciences, Tehran, Iran. ,n.sadigh@yahoo.com
2- Chronic Renal Failure Research Center, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
3- Department of Emergency, School of Medicine, Aliasghar Children’s Hospital, Iran University of Medical Sciences, Tehran, Iran. ,
Keywords: Vesicoureteral reflux, VUR, Urinary tract infections, UTI, Renal parenchymal damage, Renal scar, Renal scarring
Full-Text [PDF 443 kb]
(1423 Downloads)
| Abstract (HTML) (2987 Views)
Full-Text: (885 Views)
Introduction
Congenital anomalies of the kidney and urinary tract (CAKUT) are the leading cause of progressive deterioration of renal function and eventual end-stage renal disease [1]. Different renal tubular and glomerular biomarkers have been introduced for diagnosis, treatment monitoring, and detecting the risk of future renal damage in pediatric urologic disorders [2, 3].
Vesicoureteral reflux (VUR) is the most common congenital malformation of the urinary tract, which is defined as a pathologic retrograde of urine backflow from the urinary bladder into the ureter and kidney [4]. Despite the very low prevalence of primary VUR (about 1%) in the general population, it accounts for 30–50% of recurrent urinary tract infections (UTI) in children. About 8.5–18% of children with chronic kidney disease have a history of VUR. Therefore, early diagnosis and appropriate management of VUR prevent its long-term complications such as hypertension, proteinuria, and chronic kidney disease [3, 5].
Currently, the identification of VUR depends on invasive and expensive imaging modalities, with high radiologic burden [3]. Accordingly, voiding cystourethrogram (VCUG) has not been routinely recommended in children between 2-24 months with the first febrile UTI [6]. However, renal scarring might occur in 15-60% of the affected individuals, especially in association with chronic pyelonephritis, which emphasizes VCUG for the detection of VUR and prevention of future reflux nephropathy [4].
Therefore, the introduction of accurate and noninvasive diagnostic biomarkers seems necessary for the early diagnosis of VUR [3]. Conventionally, serum creatinine, creatinine clearance, urine sediment, and radiologic examinations have been considered for the evaluation of renal function and renal scarring, with low sensitivity and specificity [4, 7].
Recently, the measurement of tubular biomarkers has been suggested as the early diagnostic indicators of VUR and renal parenchymal damage (RPD) before the renal pathologic changes. Neutrophil gelatinase-associated lipocalin (NGAL) is one of the recently introduced biomarkers for the diagnosis of VUR. Urine NGAL has been suggested as an early accurate biomarker of acute kidney injury, and progression to chronic kidney disease in recent studies [3]. This systematic review was performed to update our understanding of the currently available evidence regarding the importance of NGAL in children/teenagers with VUR or RPD.
Methods
This systematic review is prepared according to the recommendations of the preferred reporting items for systematic reviews and meta-analyses (PRISMA) 2009 checklist [8].
Eligibility criteria
We considered published studies that evaluated the correlation between uNGAL or uNGAL/Cr excretion and primary VUR in patients under 18 years of age. We excluded studies with cases of associated infectious or inflammatory disorders, acute or chronic kidney disease, and obstructive uropathies. Only cross-sectional, case-control, and cohort studies were included.
Information sources
The following electronic databases were systematically searched: PubMed, Web of Science Core Collection via Clarivate Analytics, Scopus, ProQuest, and Ovid. The grey literature included Google Scholar. We also utilized the “related citations” tool of PubMed to find additional pertinent studies with no date limitation.
Search
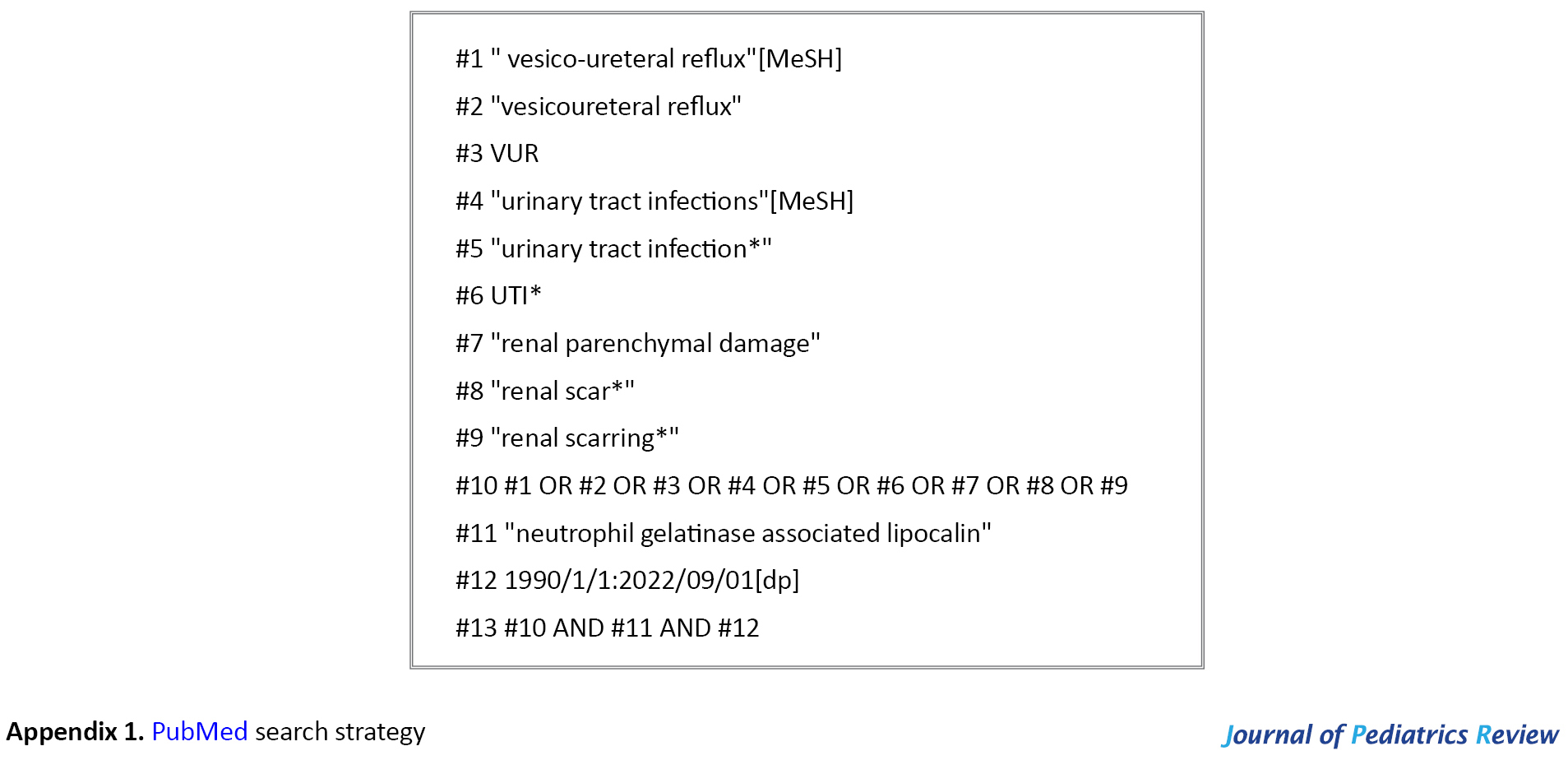
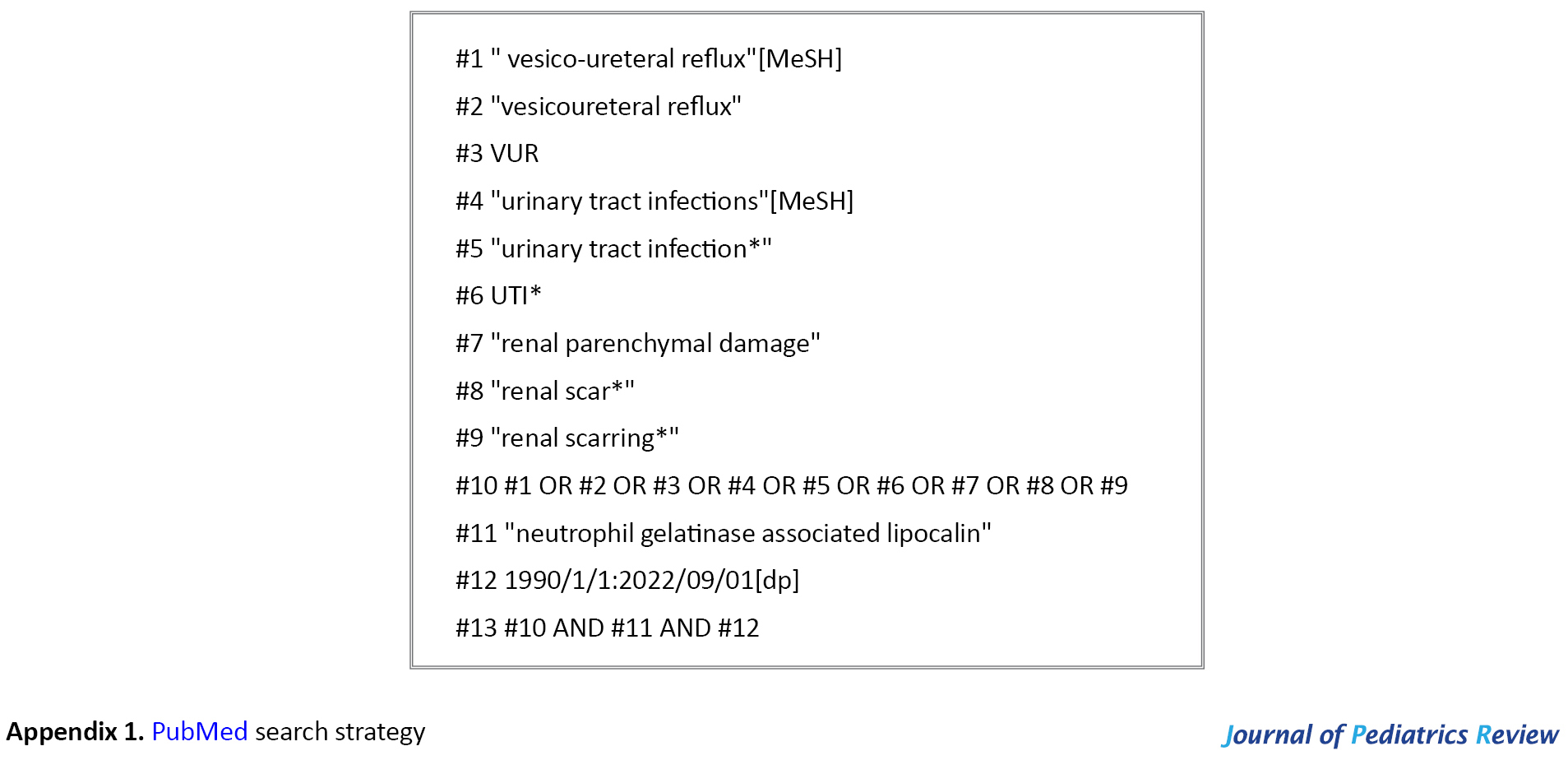
The electronic bibliographic databases were searched in September 2022 using both controlled vocabulary (for PubMed, Medical Subject Headings (MeSH)) and free text words. MeSH terms used in PubMed were “vesico-ureteral reflux” and “urinary tract infections”. Free text words were neutrophil gelatinase-associated lipocalin, renal parenchymal damage, renal scar, and renal scarring. Appendix 1 presents the search strategy for PubMed. The search results from all sources were entered into the EndNote software, version x8.
Study selection
Two authors independently applied the selection criteria to all the retrieved citations and read the titles and abstracts. Afterward, the number of retained articles was compared. In case of disagreement, we used the full text and comments of a senior researcher. Then, the full texts of the articles were reviewed. We considered articles published in English, Spanish, French, German, and Persian. In the case of the non-English language of the document, we used Google Translate service to translate the article into English and consulted with a professional translator, if required.
Results
Study selection
A total of 381 citations were identified by searching the electronic bibliographic databases and the grey literature. Of these, 60 citations were duplicates. Then, 290 citations were excluded during the screening of the titles and abstracts. The full texts of 31 articles were reviewed and finally, 18 articles met the inclusion criteria. Publications were included if they reported on urine NGAL in the setting of RPD or VUR (Figure 1).
.jpg)
Study characteristics
Urine NGAL or urine NGAL/Cr had significantly increased excretion in the majority of children with primary VUR or RPD, with a positive correlation to the severity of VUR in some studies, and no correlation in others (Table 1).
.jpg)
Discussion
NGAL is a member of the lipocalin family, expressed in different human tissues, such as neutrophil granules, monocytes, macrophages, α-intercalated cells of the collecting duct, and renal proximal tubules. NGAL has an important role in the innate immune response by inhibiting bacterial growth. It releases from activated neutrophils and other immune cells to reduce bacterial growth in the early phase of infection [7, 9, 10, 11].
Two forms of NGAL including plasma NGAL (pNGAL) and urine NGAL (uNGAL) have been recognized with different mechanisms of induction and up-regulation. Both pNGAL and uNGAL have been considered as early markers of acute kidney injury. PNGAL is mostly a predictive marker of systemic inflammation, and uNGAL is specific for renal tubular epithelial damage [6, 9]. Both pNGAL and uNGAL levels are low in normal healthy individuals, which increase secondary to high NGAL production and low NGAL reabsorption after acute renal tubular injury, chronic tubulointerstitial damage, or regeneration of renal tubular cells damaged by VUR and or renal scarring. This appears to be mediated by nuclear factor kappa B (NF-KB), which is activated after inflammatory or ischemic tubular damage [7, 9, 12, 13].
It is an early, sensitive, and non-invasive biomarker of acute kidney injury, by the severity of RPD. But, other utilities of uNGAL such as upper and lower urinary tract infection, primary VUR, and RPD have been also suggested in some reports [3].
Our previous study (2020) showed higher mean uNGAL and uNGAL/Cr in 32 patients with VUR, compared with healthy age-matched controls, irrespective of the severity of VUR. In addition, uNGAL/Cr had a significant increase in patients with decreased DMSA renal parenchymal function, compared to those with normal DMSA renal scans. Using the cutoff value of 0.88 ng/mg, uNGAL had 84% sensitivity and 81% specificity for the diagnosis of VUR. Based on AUC (0.86), uNGAL/Cr had acceptable diagnostic accuracy in children with VUR. The results of our study support the evidence that uNGAL/Cr is a sensitive, specific, and accurate biomarker for the diagnosis of children with primary VUR. However, there was no correlation between uNGAL and uNGAL/Cr with renal ultrasound, the severity of VUR, and the DMSA renal scan [3].
Similar to our results, uNGAL/Cr was a sensitive and non-invasive biomarker for predicting renal scar in patients with primary VUR in the Parmaksiz et al. (2016) study, with little correlation to the severity of VUR. UNGAL/Cr had no significant difference in patients with RPD and VUR, compared to those with RPD and no VUR, but higher than complete or incomplete resolved VUR without RPS and the control group. They suggested renal scarring as a determinant factor for uNGAL excretion, which was a non-invasive diagnostic marker for predicting renal scar in reflux nephropathy. They showed de`novo NGAL production secondary to an inflammatory response in damaged renal tubular cells involving renal scarring [4].
Median concentrations of NGAL and microalbumin in 50 patients with congenital uropathies were significantly increased in Lee et al. (2009) study, compared to the healthy controls, and correlated with the progressive deterioration of renal function in children with CAKUT anomalies [2].
As a secondary finding in the study of Seo et al. (2014), serum NGAL concentration was higher in a group of UTI with cortical defect plus VUR compared to that without VUR, but this result was not statistically significant [14].
Ichino et al. (2010) in a study of pediatric patients found uNGAL levels are significantly higher than normal in patients with VUR and renal scarring without evidence of UTI. However, the levels did not correlate with reflux grade [15].
Mean uNGAL/Cr in children with VUR was significantly higher than those without VUR in Eskandarifar et al. study (2021), with 76.5% sensitivity and 73% specificity. They suggested uNGAL/Cr as a rapid and non-invasive biomarker for the diagnosis of VUR, compatible with the severity of VUR [12].
In Jafari et al. study (2013) on 50 infants with prenatal hydronephrosis, uNGAL/Cr was higher in infants with VUR, by the grading of VUR [16].
Amiri et al. (2020) reported higher, although non-significant levels of uNGAL in patients with VUR, especially in patients with severe or bilateral VUR than those with mild or moderate grade and unilateral involvement. UNGAL/Cr was a non-invasive biomarker in the diagnosis of VUR, especially in severe forms. However, there was no significant difference for uNGAL and uNGAL/Cr between patients with and without a renal scar. The severity of VUR had a significant correlation with uNGAL/Cr, by the increasing risk of tissue inflammation and renal scarring with the severity of VUR [5].
Niak et al. (2022) found significantly higher median uNGAL in children with renal scar, but no association with the severity of renal scarring. Follow-up measurement of uNGAL was an indicator for monitoring the progression of renal scars, which does not normalize after the development of renal scar. A significant difference was found in uNGAL/Cr in low-grade and high-grade VUR in its bilateral form. UNGAL was a potential non-invasive biomarker for the presence of renal scar, secondary to its specificity for renal tubular damage. However, uNGAL/Cr was a poor predictor of renal scarring with 60% sensitivity and 61% specificity [7].
However, there are studies in which VUR or RPD is not an independent predictor of uNGAL excretion. In Kiatao et al. study (2015), there was no significant correlation between uNGAL excretion and renal scarring following an episode of UTI [17]. Yim et al. (2014) showed no correlation between uNGAL level with the presence of hydronephrosis in patients with febrile UTIs, VUR, or renal scarring [18]. Yilmaz et al. (2009) reported VUR in 11/30 patients with symptomatic UTI. UNGAL and uNGAL/Cr were not significantly different in patients with or without VUR. In addition, the severity of VUR was not correlated with DMSA renal scan damage [19].
Putting all together, NGAL gene expression and uNGAL excretion are associated with regenerative renal tubular cells, which can be triggered by either active renal infection or in later phases by the process of scar formation. Thus, uNGAL is a potential bedside marker for the early detection of VUR in patients with repeated UTIs. Like every diagnostic test, false positive results can be seen in AKI, CKD, or due to other systemic inflammatory disorders and young infants with active renal cell proliferation, and false negative results due to severely damaged kidneys [17].
In conclusion, there appears to have enough evidence to support a putative role of uNGAL and uNGAL/Cr in the prediction of VUR or RPD. However, available evidence regarding NGAL as a predictor of VUR lacks high-quality studies, and further prospective/cohort studies are recommended for the better assessment of uNGAL in VUR or RPD during a longer period to eliminate the effect of age and acquired/congenital RPD.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors
Authors contributions
Conceptualization and study design: Azar Nickavar and Ehsan Valavi; Analysis, drafting the manuscript: Azar Nickava; Data interpretation: Nader Sadigh; Final approval: Azar Nickavar and Nader Sadigh.
Conflicts of interest
The authors declared no conflict of interest.
References
Congenital anomalies of the kidney and urinary tract (CAKUT) are the leading cause of progressive deterioration of renal function and eventual end-stage renal disease [1]. Different renal tubular and glomerular biomarkers have been introduced for diagnosis, treatment monitoring, and detecting the risk of future renal damage in pediatric urologic disorders [2, 3].
Vesicoureteral reflux (VUR) is the most common congenital malformation of the urinary tract, which is defined as a pathologic retrograde of urine backflow from the urinary bladder into the ureter and kidney [4]. Despite the very low prevalence of primary VUR (about 1%) in the general population, it accounts for 30–50% of recurrent urinary tract infections (UTI) in children. About 8.5–18% of children with chronic kidney disease have a history of VUR. Therefore, early diagnosis and appropriate management of VUR prevent its long-term complications such as hypertension, proteinuria, and chronic kidney disease [3, 5].
Currently, the identification of VUR depends on invasive and expensive imaging modalities, with high radiologic burden [3]. Accordingly, voiding cystourethrogram (VCUG) has not been routinely recommended in children between 2-24 months with the first febrile UTI [6]. However, renal scarring might occur in 15-60% of the affected individuals, especially in association with chronic pyelonephritis, which emphasizes VCUG for the detection of VUR and prevention of future reflux nephropathy [4].
Therefore, the introduction of accurate and noninvasive diagnostic biomarkers seems necessary for the early diagnosis of VUR [3]. Conventionally, serum creatinine, creatinine clearance, urine sediment, and radiologic examinations have been considered for the evaluation of renal function and renal scarring, with low sensitivity and specificity [4, 7].
Recently, the measurement of tubular biomarkers has been suggested as the early diagnostic indicators of VUR and renal parenchymal damage (RPD) before the renal pathologic changes. Neutrophil gelatinase-associated lipocalin (NGAL) is one of the recently introduced biomarkers for the diagnosis of VUR. Urine NGAL has been suggested as an early accurate biomarker of acute kidney injury, and progression to chronic kidney disease in recent studies [3]. This systematic review was performed to update our understanding of the currently available evidence regarding the importance of NGAL in children/teenagers with VUR or RPD.
Methods
This systematic review is prepared according to the recommendations of the preferred reporting items for systematic reviews and meta-analyses (PRISMA) 2009 checklist [8].
Eligibility criteria
We considered published studies that evaluated the correlation between uNGAL or uNGAL/Cr excretion and primary VUR in patients under 18 years of age. We excluded studies with cases of associated infectious or inflammatory disorders, acute or chronic kidney disease, and obstructive uropathies. Only cross-sectional, case-control, and cohort studies were included.
Information sources
The following electronic databases were systematically searched: PubMed, Web of Science Core Collection via Clarivate Analytics, Scopus, ProQuest, and Ovid. The grey literature included Google Scholar. We also utilized the “related citations” tool of PubMed to find additional pertinent studies with no date limitation.
Search
The electronic bibliographic databases were searched in September 2022 using both controlled vocabulary (for PubMed, Medical Subject Headings (MeSH)) and free text words. MeSH terms used in PubMed were “vesico-ureteral reflux” and “urinary tract infections”. Free text words were neutrophil gelatinase-associated lipocalin, renal parenchymal damage, renal scar, and renal scarring. Appendix 1 presents the search strategy for PubMed. The search results from all sources were entered into the EndNote software, version x8.
Study selection
Two authors independently applied the selection criteria to all the retrieved citations and read the titles and abstracts. Afterward, the number of retained articles was compared. In case of disagreement, we used the full text and comments of a senior researcher. Then, the full texts of the articles were reviewed. We considered articles published in English, Spanish, French, German, and Persian. In the case of the non-English language of the document, we used Google Translate service to translate the article into English and consulted with a professional translator, if required.
Results
Study selection
A total of 381 citations were identified by searching the electronic bibliographic databases and the grey literature. Of these, 60 citations were duplicates. Then, 290 citations were excluded during the screening of the titles and abstracts. The full texts of 31 articles were reviewed and finally, 18 articles met the inclusion criteria. Publications were included if they reported on urine NGAL in the setting of RPD or VUR (Figure 1).
.jpg)
Study characteristics
Urine NGAL or urine NGAL/Cr had significantly increased excretion in the majority of children with primary VUR or RPD, with a positive correlation to the severity of VUR in some studies, and no correlation in others (Table 1).
.jpg)
Discussion
NGAL is a member of the lipocalin family, expressed in different human tissues, such as neutrophil granules, monocytes, macrophages, α-intercalated cells of the collecting duct, and renal proximal tubules. NGAL has an important role in the innate immune response by inhibiting bacterial growth. It releases from activated neutrophils and other immune cells to reduce bacterial growth in the early phase of infection [7, 9, 10, 11].
Two forms of NGAL including plasma NGAL (pNGAL) and urine NGAL (uNGAL) have been recognized with different mechanisms of induction and up-regulation. Both pNGAL and uNGAL have been considered as early markers of acute kidney injury. PNGAL is mostly a predictive marker of systemic inflammation, and uNGAL is specific for renal tubular epithelial damage [6, 9]. Both pNGAL and uNGAL levels are low in normal healthy individuals, which increase secondary to high NGAL production and low NGAL reabsorption after acute renal tubular injury, chronic tubulointerstitial damage, or regeneration of renal tubular cells damaged by VUR and or renal scarring. This appears to be mediated by nuclear factor kappa B (NF-KB), which is activated after inflammatory or ischemic tubular damage [7, 9, 12, 13].
It is an early, sensitive, and non-invasive biomarker of acute kidney injury, by the severity of RPD. But, other utilities of uNGAL such as upper and lower urinary tract infection, primary VUR, and RPD have been also suggested in some reports [3].
Our previous study (2020) showed higher mean uNGAL and uNGAL/Cr in 32 patients with VUR, compared with healthy age-matched controls, irrespective of the severity of VUR. In addition, uNGAL/Cr had a significant increase in patients with decreased DMSA renal parenchymal function, compared to those with normal DMSA renal scans. Using the cutoff value of 0.88 ng/mg, uNGAL had 84% sensitivity and 81% specificity for the diagnosis of VUR. Based on AUC (0.86), uNGAL/Cr had acceptable diagnostic accuracy in children with VUR. The results of our study support the evidence that uNGAL/Cr is a sensitive, specific, and accurate biomarker for the diagnosis of children with primary VUR. However, there was no correlation between uNGAL and uNGAL/Cr with renal ultrasound, the severity of VUR, and the DMSA renal scan [3].
Similar to our results, uNGAL/Cr was a sensitive and non-invasive biomarker for predicting renal scar in patients with primary VUR in the Parmaksiz et al. (2016) study, with little correlation to the severity of VUR. UNGAL/Cr had no significant difference in patients with RPD and VUR, compared to those with RPD and no VUR, but higher than complete or incomplete resolved VUR without RPS and the control group. They suggested renal scarring as a determinant factor for uNGAL excretion, which was a non-invasive diagnostic marker for predicting renal scar in reflux nephropathy. They showed de`novo NGAL production secondary to an inflammatory response in damaged renal tubular cells involving renal scarring [4].
Median concentrations of NGAL and microalbumin in 50 patients with congenital uropathies were significantly increased in Lee et al. (2009) study, compared to the healthy controls, and correlated with the progressive deterioration of renal function in children with CAKUT anomalies [2].
As a secondary finding in the study of Seo et al. (2014), serum NGAL concentration was higher in a group of UTI with cortical defect plus VUR compared to that without VUR, but this result was not statistically significant [14].
Ichino et al. (2010) in a study of pediatric patients found uNGAL levels are significantly higher than normal in patients with VUR and renal scarring without evidence of UTI. However, the levels did not correlate with reflux grade [15].
Mean uNGAL/Cr in children with VUR was significantly higher than those without VUR in Eskandarifar et al. study (2021), with 76.5% sensitivity and 73% specificity. They suggested uNGAL/Cr as a rapid and non-invasive biomarker for the diagnosis of VUR, compatible with the severity of VUR [12].
In Jafari et al. study (2013) on 50 infants with prenatal hydronephrosis, uNGAL/Cr was higher in infants with VUR, by the grading of VUR [16].
Amiri et al. (2020) reported higher, although non-significant levels of uNGAL in patients with VUR, especially in patients with severe or bilateral VUR than those with mild or moderate grade and unilateral involvement. UNGAL/Cr was a non-invasive biomarker in the diagnosis of VUR, especially in severe forms. However, there was no significant difference for uNGAL and uNGAL/Cr between patients with and without a renal scar. The severity of VUR had a significant correlation with uNGAL/Cr, by the increasing risk of tissue inflammation and renal scarring with the severity of VUR [5].
Niak et al. (2022) found significantly higher median uNGAL in children with renal scar, but no association with the severity of renal scarring. Follow-up measurement of uNGAL was an indicator for monitoring the progression of renal scars, which does not normalize after the development of renal scar. A significant difference was found in uNGAL/Cr in low-grade and high-grade VUR in its bilateral form. UNGAL was a potential non-invasive biomarker for the presence of renal scar, secondary to its specificity for renal tubular damage. However, uNGAL/Cr was a poor predictor of renal scarring with 60% sensitivity and 61% specificity [7].
However, there are studies in which VUR or RPD is not an independent predictor of uNGAL excretion. In Kiatao et al. study (2015), there was no significant correlation between uNGAL excretion and renal scarring following an episode of UTI [17]. Yim et al. (2014) showed no correlation between uNGAL level with the presence of hydronephrosis in patients with febrile UTIs, VUR, or renal scarring [18]. Yilmaz et al. (2009) reported VUR in 11/30 patients with symptomatic UTI. UNGAL and uNGAL/Cr were not significantly different in patients with or without VUR. In addition, the severity of VUR was not correlated with DMSA renal scan damage [19].
Putting all together, NGAL gene expression and uNGAL excretion are associated with regenerative renal tubular cells, which can be triggered by either active renal infection or in later phases by the process of scar formation. Thus, uNGAL is a potential bedside marker for the early detection of VUR in patients with repeated UTIs. Like every diagnostic test, false positive results can be seen in AKI, CKD, or due to other systemic inflammatory disorders and young infants with active renal cell proliferation, and false negative results due to severely damaged kidneys [17].
In conclusion, there appears to have enough evidence to support a putative role of uNGAL and uNGAL/Cr in the prediction of VUR or RPD. However, available evidence regarding NGAL as a predictor of VUR lacks high-quality studies, and further prospective/cohort studies are recommended for the better assessment of uNGAL in VUR or RPD during a longer period to eliminate the effect of age and acquired/congenital RPD.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors
Authors contributions
Conceptualization and study design: Azar Nickavar and Ehsan Valavi; Analysis, drafting the manuscript: Azar Nickava; Data interpretation: Nader Sadigh; Final approval: Azar Nickavar and Nader Sadigh.
Conflicts of interest
The authors declared no conflict of interest.
References
- Anand S, Bajpai M, Khanna T, Kumar A. Urinary biomarkers as point-of-care tests for predicting progressive deterioration of kidney function in congenital anomalies of kidney and urinary tract: Trefoil Family Factors (TFFs) as the emerging biomarkers. Pediatr Nephrol. 2021; 36(6):1465-72. [DOI:10.1007/s00467-020-04841-8] [PMID]
- Lee RS. Biomarkers for pediatric urological disease. Curr Opin Urol. 2009; 19(4):397-401. [DOI:10.1097/MOU.0b013e32832c90ec] [PMID]
- Nickavar A, Valavi E, Safaeian B, Moosavian M. Validity of urine neutrophile gelatinase-associated lipocalin in children with primary vesicoureteral reflux. Int Urol Nephrol 2020; 52(4):599-602. [DOI:10.1007/s11255-019-02355-3] [PMID]
- Parmaksiz G, Noyan A, Dursun H, Ince E, Anarat R, Cengiz N. Role of new biomarkers for predicting renal scarring in vesicoureteral reflux: NGAL, KIM-1, and L-FABP. Pediatr Nephrol. 2016; 31(1):97- 103. [DOI:10.1007/s00467-015-3194-3] [PMID]
- Amiri R, Faradmal J, Rezaie B, Sedighi I, Sanaei Z, Solgi G. Evaluation of urinary neutrophil gelatinase-associated lipocalin as a biomarker in pediatric vesicoureteral reflux assessment. Iran J Kidney Dis. 2020; 14(5):373-9. [PMID]
- Forster CS, Devarajan P. Neutrophil gelatinase associated lipocalin: Utility in urologic conditions. Pediatr Nephrol. 2017; 32(3):377-81. [PMID] [PMCID]
- Naik PB, Jindal B, Kumaravel S, Halanaik D, Rajappa M, Naredi BK et al. Utility of urinary biomarkers neutrophil gelatinase-associated lipocalin and kidney injury molecule-1 as a marker for diagnosing the presence of renal scar in children with Vesicoureteral Reflux (VUR): A cross-sectional study. J Indian Assoc Pediatr Surg. 2022; 27(1):83-90. [DOI:10.4103/jiaps.JIAPS_334_20] [PMID] [PMCID]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ (Clinical research ed). 2009; 339:b2700. [DOI:10.1136/bmj.b2700] [PMID] [PMCID]
- Moon JH, Yoo KH, Yim HE. Urinary neutrophil gelatinase-associated lipocalin: A marker of urinary tract infection among febrile children. Clin Exp Pediatr. 2021; 64(7):347-54. [DOI:10.3345/cep.2020.01130] [PMID] [PMCID]
- Jung N, Byun HJ, Park JH , Kim JS , Kim HW, Ha JY. Diagnostic accuracy of urinary biomarkers in infants younger than 3 months with urinary tract infection. Korean J Pediatr. 2018; 61(1):24-9. [DOI:10.3345/kjp.2018.61.1.24] [PMID] [PMCID]
- Kim BK, Yim HE , Yoo KH . Plasma neutrophil gelatinase-associated lipocalin: A marker of acute pyelonephritis in children. Pediatr Nephrol. 2017; 32(3):477-84. [PMID]
- Eskandarifar A, Rahehag R, Jafari M. Evaluating the measurement of urinary neutrophil gelatinase associated lipocalin for the diagnosis of vesicoureteral reflux in children. Int J Pediatr. 2021; 9(12):15015-21. [Link]
- Krzemień G, Pańczyk-Tomaszewska M, Kotuła I, Demkow U, Szmigielska A. Serum neutrophil gelatinase-associated lipocalin for predicting acute pyelonephritis in infants with urinary tract infection. Cent Eur J Immunol. 2019; 44(1):45-50. [DOI:10.5114/ceji.2019.84016] [PMID] [PMCID]
- Seo WH, Nam SW, Lee EH, Je BK, Yim HE, Choi BM. A rapid plasma neutrophil gelatinase-associated lipocalin assay for diagnosis of acute pyelonephritis in infants with acute febrile urinary tract infections: A preliminary study. Eur J Pediatr. 2014; 173(2):229-32. [PMID]
- Ichino M, Kusaka M, Kuroyanagi Y, Mori T, Morooba M, Sasaki H et al. Urinary neutrophil gelatinase associated lipocalin is a potential noninvasive marker for renal scarring in patients with vesicoureteral reflux. J Urol. 2010; 183(5):2001-7. [DOI:10.1016/j.juro.2010.01.031] [PMID]
- Mohammad Jafari H, Rafiei A, Abedi M, Aalaee A, Mirabi AM, Abedi E. Urinary neutrophil gelatinase associatedLipocalin is a more prognostic biomarker to distinguish antenatal hydronephrosisin neonates. Res Mol Med. 2013; 1(2):10-6. [DOI:10.18869/acadpub.rmm.1.2.10]
- Kitao T, Kimata T, Yamanouchi S, Kato S, Tsuji S, Kaneko K. Urinary biomarkers for screening for renal scarring in children with febrile urinary tract infection: Pilot study. J Urol. 2015; 194(3):766-71. [DOI:10.1016/j.juro.2015.04.091] [PMID]
- Yim HE, Yim H, Bae ES, Woo SU, Yoo KH. Predictive value of urinary and serum biomarkers in young children with febrile urinary tract infections. Pediatr Nephrol. 2014; 29(11):2181-9. [PMID]
- Yilmaz A, Sevketoglu E, Gedikbasi A, Karyagar S, Kiyak A, Mulazimoglu M ,et al. Early prediction of urinary tract infection with urinary neutrophil gelatinase associated lipocalin. Pediatr Nephrol. 2009; 24(12):2387-92. [DOI:10.1007/s00467-009-1279-6] [PMID]
Type of Study: Review Article |
Subject:
Urology
Received: 2022/12/4 | Accepted: 2023/03/11 | Published: 2023/04/1
Received: 2022/12/4 | Accepted: 2023/03/11 | Published: 2023/04/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |