Volume 12, Issue 2 (4-2024)
J. Pediatr. Rev 2024, 12(2): 183-190 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Azizi M, Ahmadi I, Ghasempouri S K, Milani H, Monjazeb Marvdashti L, Elyasi F. Attention Deficit Hyperactivity Disorder: Case Report and Literature Review on Vaginal Button Battery Insertion. J. Pediatr. Rev 2024; 12 (2) :183-190
URL: http://jpr.mazums.ac.ir/article-1-572-en.html
URL: http://jpr.mazums.ac.ir/article-1-572-en.html
Marzieh Azizi1 

 , Imaneh Ahmadi2
, Imaneh Ahmadi2 

 , Seyed Khosro Ghasempouri3
, Seyed Khosro Ghasempouri3 

 , Hamed Milani4
, Hamed Milani4 

 , Leila Monjazeb Marvdashti5
, Leila Monjazeb Marvdashti5 

 , Forouzan Elyasi *6
, Forouzan Elyasi *6 




 , Imaneh Ahmadi2
, Imaneh Ahmadi2 

 , Seyed Khosro Ghasempouri3
, Seyed Khosro Ghasempouri3 

 , Hamed Milani4
, Hamed Milani4 

 , Leila Monjazeb Marvdashti5
, Leila Monjazeb Marvdashti5 

 , Forouzan Elyasi *6
, Forouzan Elyasi *6 


1- Sexual and Reproductive Health Research Center, Mazandaran University of Medical Sciences, Sari, Iran.
2- Department of Obstetrics and Gynecology, Imam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran.
3- Department of Emergency Medicine, Ghaemshahr Razi Hospital, Mazandaran University of Medical Sciences, Sari, Iran.
4- Faculty of Medicine, Mazandaran University of Medical Sciences, Sari, Iran.
5- Food Health Research Center, Hormozgan University of Medical Sciences, Bandar Abbas, Iran.
6- Sexual and Reproductive Health Research Center, Addiction Institute, Mazandaran University of Medical Sciences, Sari, Iran. ,forouzan.elyasi@gmail.com
2- Department of Obstetrics and Gynecology, Imam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran.
3- Department of Emergency Medicine, Ghaemshahr Razi Hospital, Mazandaran University of Medical Sciences, Sari, Iran.
4- Faculty of Medicine, Mazandaran University of Medical Sciences, Sari, Iran.
5- Food Health Research Center, Hormozgan University of Medical Sciences, Bandar Abbas, Iran.
6- Sexual and Reproductive Health Research Center, Addiction Institute, Mazandaran University of Medical Sciences, Sari, Iran. ,
Full-Text [PDF 769 kb]
(1072 Downloads)
| Abstract (HTML) (2598 Views)
Full-Text: (738 Views)
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is childhood’s most common neurobehavioral disorder and the most prevalent chronic health problem affecting school-aged children [1]. According to published literature, the prevalence of ADHD varies significantly due to considerable changes in its diagnostic criteria over time but is reported in 3% to 5% of school-age children [2]. The main symptoms of ADHD are characterized by inattention, hyperactivity, and impulsivity [3]. Children with ADHD may experience significant functional disabilities, such as school difficulties, inability to have appropriate interpersonal relationships with family and peers, low self-esteem, and academic underachievement [1]. Studies revealed that ADHD is frequently comorbid with psychiatric disorders [4, 5] and showed a significant relationship between psychiatric disorders and genitourinary insertion of foreign bodies [6].
Vaginal foreign body (VFB) is an uncommon cause of referral to pediatric and gynecology clinics, usually occurring in ages 3-9 years [7-9]. VFB can present with diverse symptoms, such as vaginal bleeding, severe inflammation, sub-abdominal and suprapubic pain, frequency, burning sensation and dysuria. Among these symptoms, vaginal bleeding is the most reliable symptom of VFB in children [10]. The occurrence of VBF, such as battery insertion in pre-pubertal girls, is responsible for approximately 4% to 10% of the outpatient visits in pediatric and gynecologic wards [11, 12, 13]. Based on the published case reports, although the most commonly inserted VFB in children is small pieces of toilet paper [9, 13-15], other objects, including small nuts, safety pins, hair pins, buttons, crayons, pencils, and disc button lithium battery [7, 9, 10, 14]. Various factors, such as developmental delays, chronic mental or physical disabilities and parents with drug abuse are associated with a higher risk of VFB insertion among children [8].
Although in rare cases, the possibility of an intravaginal foreign body is doubted in pre-pubertal girls by physicians in the emergency wards [7, 16], the availability of electronic instruments requiring batteries in daily life has rapidly increased during the last decade [8]. VFB may be inserted by the child herself during playing due to curiosity of exploring the nature of the body or due to ignorance, sexual stimulation, sexual abuse, psychiatric disorders, and sometimes self-harm [8, 11, 14]. Long-term remaining of foreign bodies in the vagina may lead to severe tissue damage due to the building of sodium hydroxide as a result of the electronic discharge of batteries [8] and also significant morbidities, such as systemic infection and secondary problems, such as perforation, traumatic ulceration of vaginal walls, fistula creation, fibrosis, vaginal stenosis even complete obstruction of the vagina [12, 13]. Accordingly, this study provides a case presentation on vaginal button battery insertion with comorbid ADHD.
Case Presentation
An eight-year-old, second-grade elementary school girl was referred to the general educational hospital in the north with the chief complaint of inserting a VFB. On the night of the event, the child removed a small disc battery of her toys and inserted it into her vagina. Then, she told this action to her parents and was referred to the hospital. The patient was admitted to the gynecology ward, and because of her history of ADHD, psychiatric counseling was considered for her. In the psychiatrist’s assessment, she confirmed that the child had no psychiatric disorders, had normal intelligence, and could communicate with them. According to the obtained history from the patient’s mother, the child was referred to a psychiatrist due to hyperactivity and considerable negligence in the first grade elementary and was treated with Ritalin due to ADHD. She did not take any other medications. Also, the mother mentioned the considerable behavioral changes in her child when she was four years old, but no drug was prescribed for her at that time. In addition, the child’s mother reveals a history of past genital touch in the child.
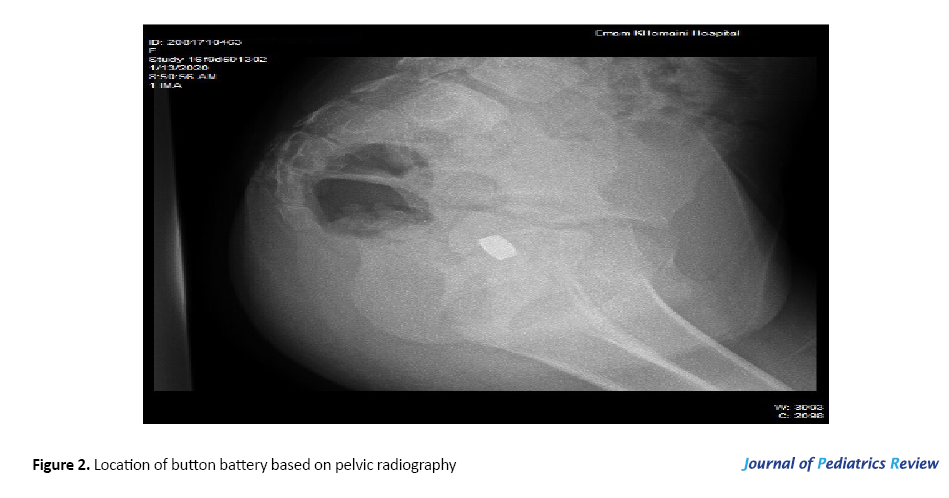
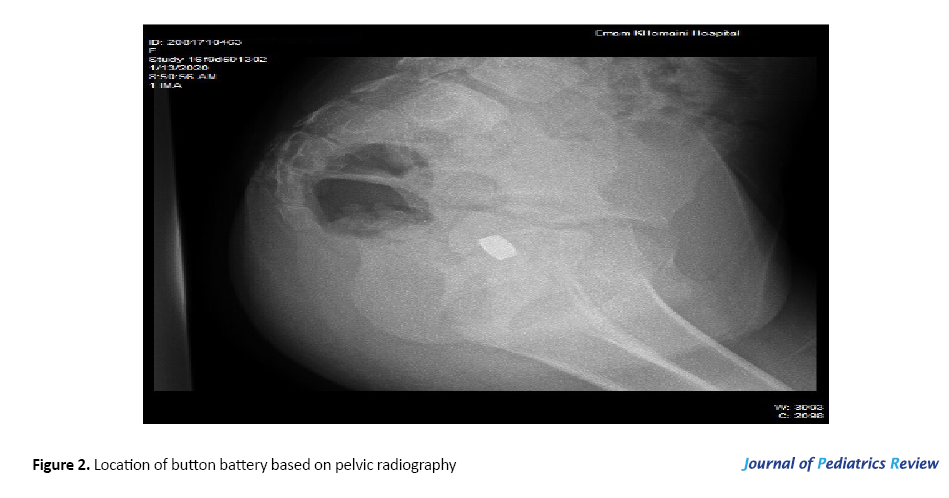
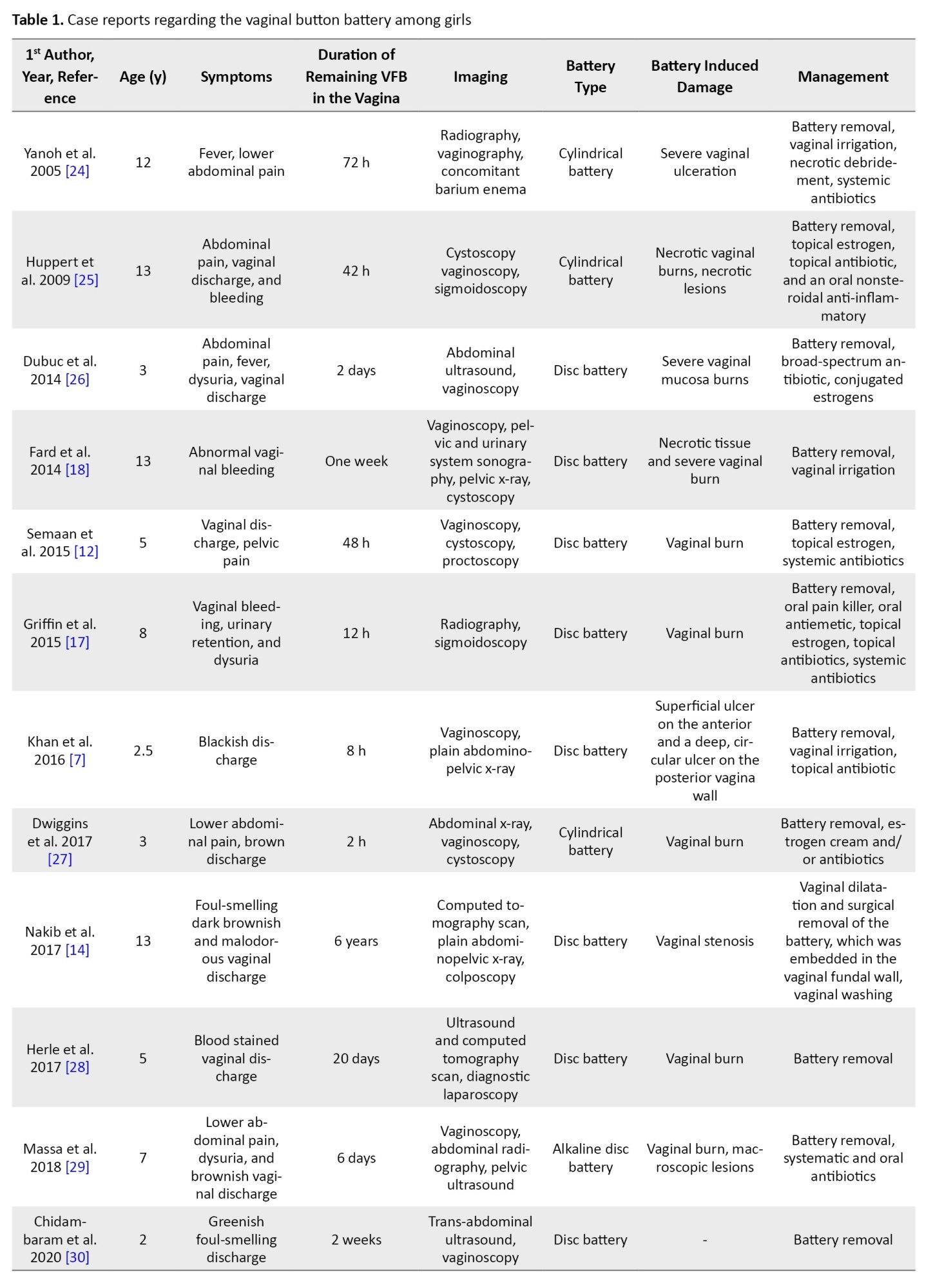
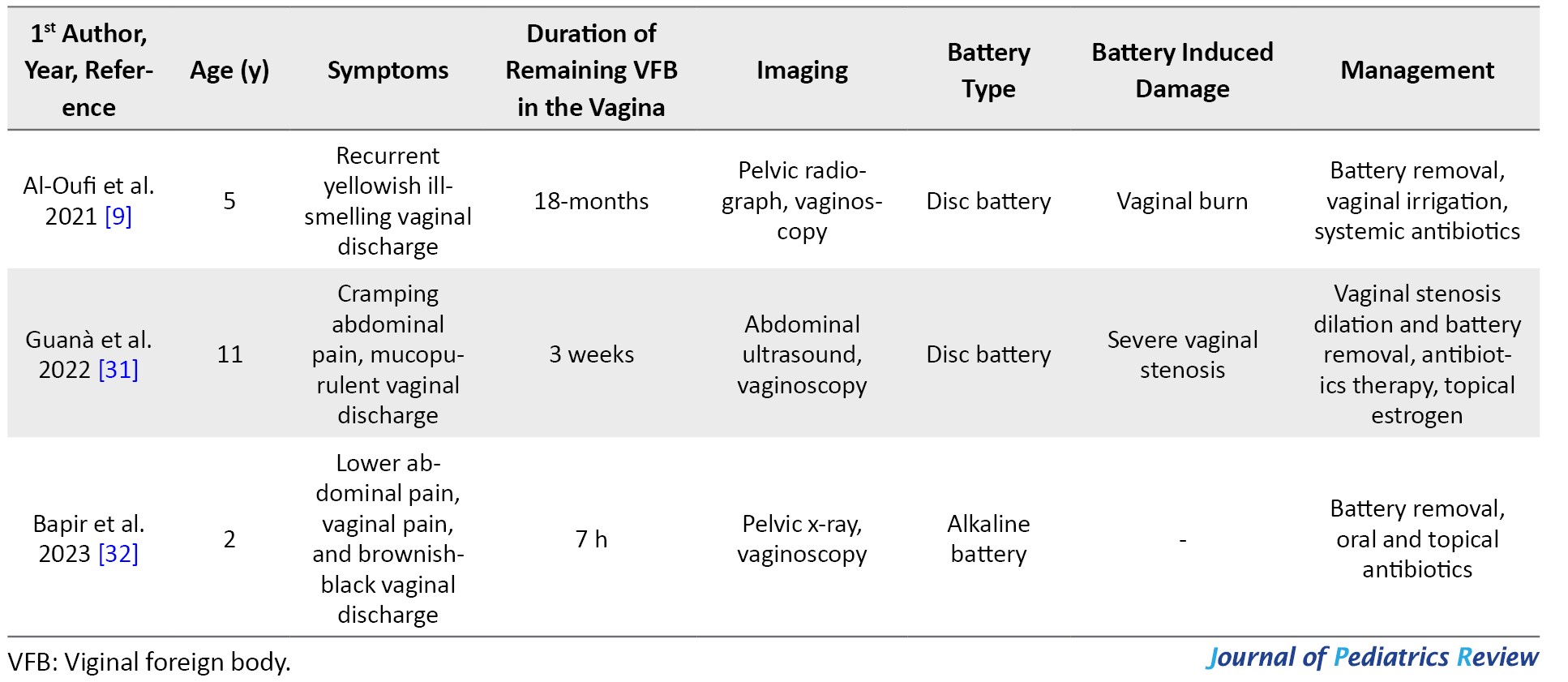
The patient’s abdomen was soft in physical examination and had a rebound tenderness complaint. Also, the entrance of the vagina was erythematosus, and vaginal discharge was seen. Due to the child’s virginity, no internal examination was performed by a physician. The urine culture and colony count results showed no growth after 48 h. The electrolyte analysis was in a normal range. The range of sodium and potassium was 143 and 4.1 mEq/L, respectively. In urine analysis, 12-14 white blood cells were seen, and other items were normal. The results of the complete blood count test showed a high level of white blood cells (11.3×103 g/dL) and a low level of mean corpuscular volume (74.9 fL) and mean corpuscular hemoglobin (25.1 pg). Pelvic radiography was conducted to specify the location of the button battery (Figures 1 and 2).

After general anesthesia, the patient underwent dorsal lithotomy. The rectal examination was first followed after Prep Drep and the battery was touched in the upper segment of the rectum. Initially, 30 mL of fluid was injected but was ineffective, and 10 mL of the lubricant was reinjected. Then, the battery was gently removed from the wall by rectal examination and milking from the upper.
In the recovery room, the patient was sleepy and febrile with an unknown source of infection and did not communicate visually or verbally. Due to continuous fever, infectious counseling was requested. The pediatric contagious specialist controlled the patient’s fever by prescribing ceftriaxone 1 g intramuscular twice daily and clindamycin 300 mg intravenously every 8 h Ter die sumendum. Also, acetaminophen 300 mg was prescribed intravenous on the condition that the patient’s body temperature was higher than 38 °C. Laboratory tests, such as complete blood cell, C reactive protein, erythrocyte sedimentation rate, urinalysis, ulcerative colitis, and chest x-ray were requested for the patient and the vital signs were checked regularly. Conservative treatment continued for up to 72 h, and the child was transferred to the pediatric ward of another hospital. The child was febrile (38-39 °C) over residency in the hospital. The patient was admitted to another hospital’s infectious service under the treatment of Meropenem antibiotic therapy for 48 h. She was discharged with good general health without fever and recommended outpatient referral to a psychiatric clinic to manage ADHD.
Literature review
The comprehensive literature search was conducted in Google Scholar and PubMed with the following keywords: “Vaginal battery” OR “vaginal button battery” OR “vaginal battery insertion” AND “girl.”
Case reports conducted regarding the insertion of vaginal battery as a VFB in girls were searched and reported in Table 1.
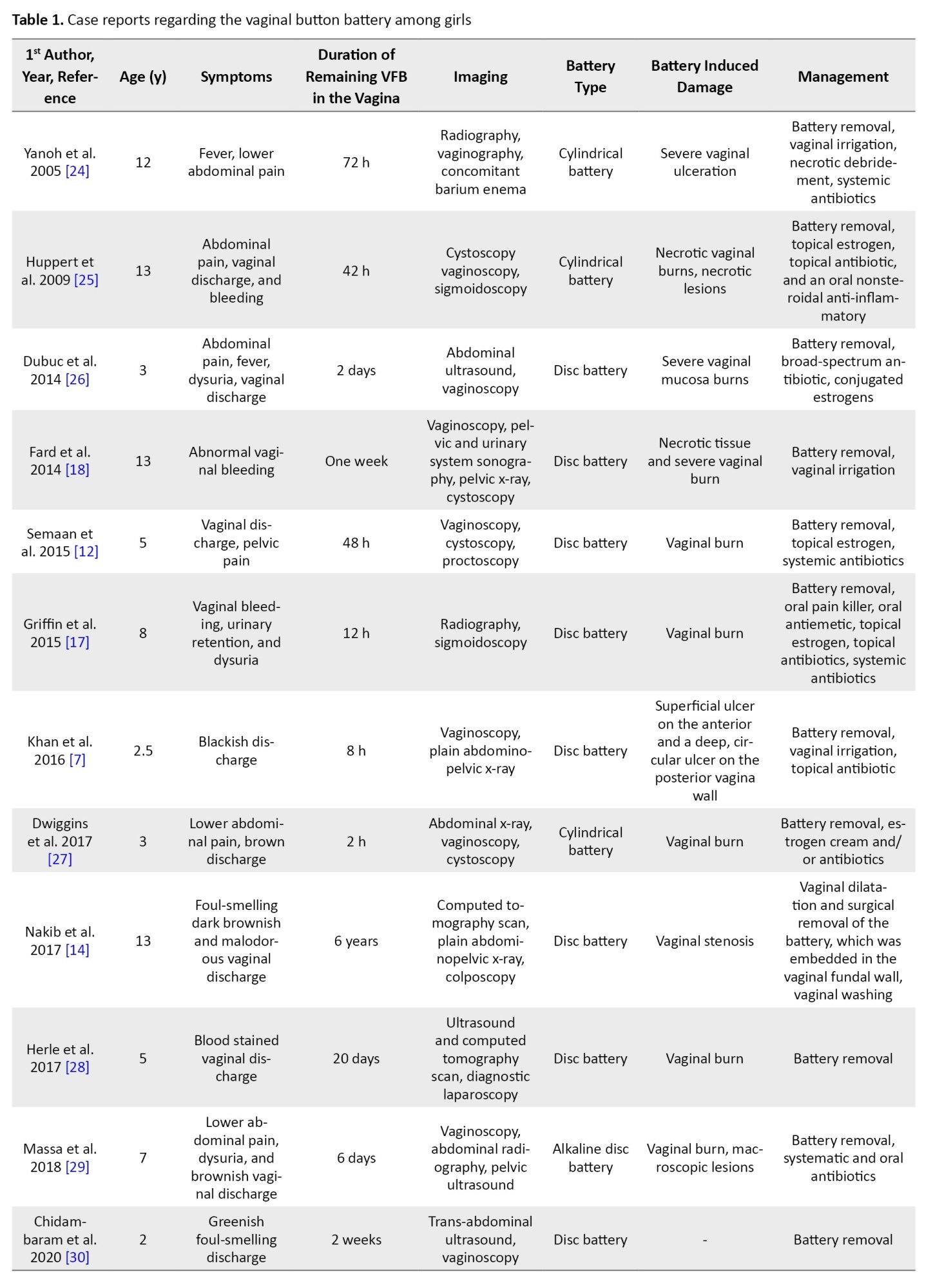
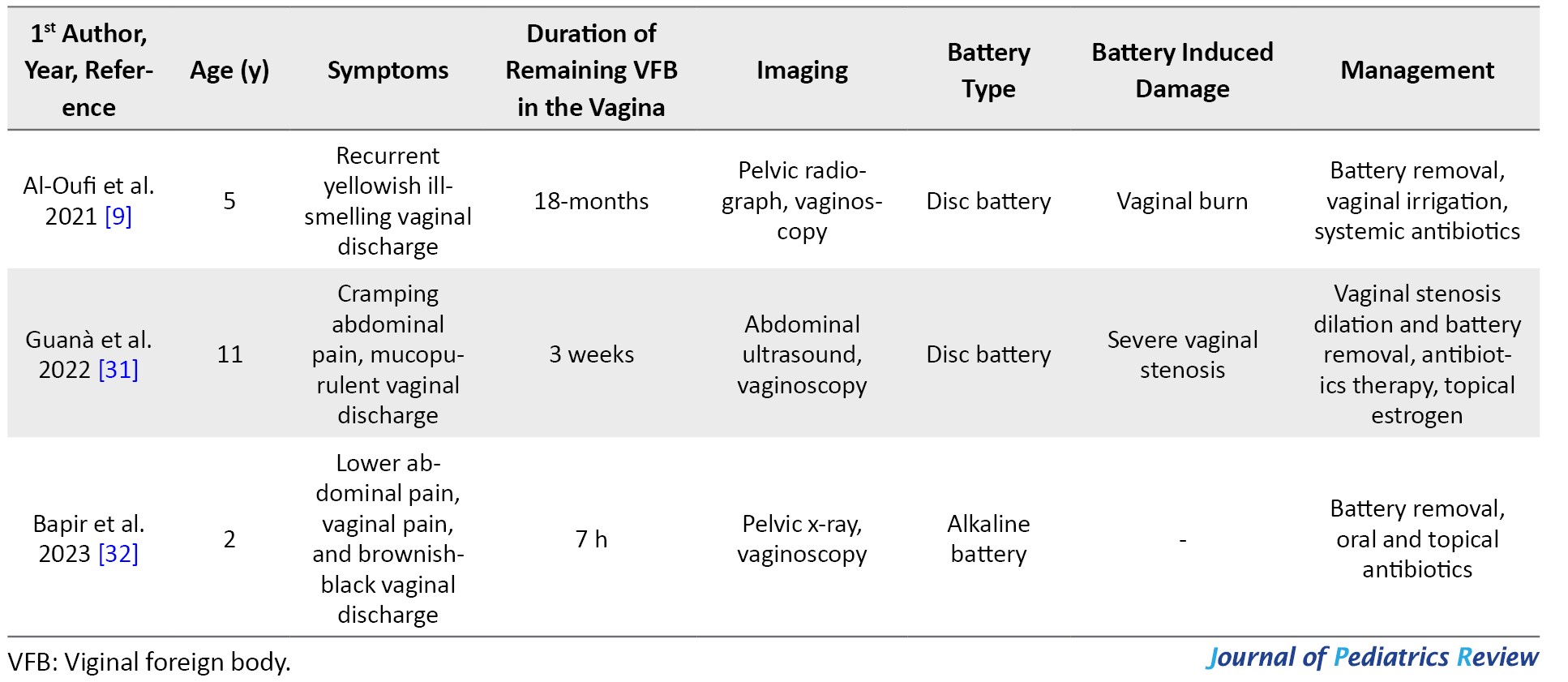
The inclusion criteria were case report studies that uniquely reported the battery as a VFB in the child girls, and other cases reported that VFB were objects except for batteries, such as toilet paper, pen, or other objects were excluded from the literature review section of this study. In addition, English articles with no publication year limitation were considered in this section. The included studies were published from 2005 until 2023.
Discussion
In this case report, an 8-year-old child was introduced who, out of curiosity and due to ADHD, tried to insert a battery in her vagina. Because the child immediately informed her parents, her assessment had no diagnostic challenge. The main challenge was the therapeutic issues and possible chemical damage to the vagina and its complications. This issue in our study case may be attributed to the reality that the child with ADHD may experience the external and internal world in highly idiosyncratic, distorted ways and attempt to adapt to those perceptions. In cases of vaginal battery insertion due to the alkaline type of batteries, the physician needs to roll out the possibility of vaginal burns, perforation, and fistula after suspected vaginal battery insertion [17].
In this case report, the entrance of the child girl’s vagina was erythematosus, and vaginal discharge was seen. Chronic vaginal discharge in children is a significant concern among pediatricians, urologists, and gynecologists [13, 18]. Persistent or recurrent foul-smelling vaginal discharge in a girl may have occurred as a result of several causes, such as primary vaginitis or vulvovaginitis, vulvar skin disease (lichen sclerosis), endocrine abnormalities, vaginal neoplasm, the possibility of undisclosed sexual abuse and also VFB [13, 18, 19].
The symptoms of VFB are often similar to cases of vaginitis and respond temporarily to antibiotics; therefore, foreign bodies are usually treated first medically [14, 20]. Overall, gynecological problems exclusively in pediatric age groups require different management [13], and early identification and timely appropriate management are key issues to achieve better clinical outcomes in these cases and reduce the complications in the children [8]. To distinguish between trauma, carcinoma, and VFB, the patient or her parents should be asked about the recent injuries and a previous history of VFBs [21]. Based on the results of a study, up to 40% of foreign body insertions remain unwitnessed [22]. However, most of these VFB insertions are likely accidental [8].
In some cases, the presence of VFB may indicate sexual abuse. Due to the children being unable to provide a history of an inserted VFB and sexual abuse, the possibility of sexual abuse should be noted and explored in the referred children with complaints of VFB [10]. The child should also be assessed psychologically due to the possibility of emotional and behavioral problems [13, 21]. Our study considered her consultation-liaison psychiatry evaluation to evaluate the case’s psychological status.
In our case, pelvic radiography was performed to diagnose the VFB in the child, and then the VFB was removed under sonography. Therapeutic management was considered according to the place of foreign bodies in the vagina. A low-situated VFB near the introitus can be visualized by separating the labia gently and can be removed easily by small Allis forceps under direct visualization [16, 20]. Initial efforts for removing the VFB in these cases included vaginal irrigation with normal saline; in return, a distally placed foreign body in the vagina may need an examination under anesthesia and removal by a vaginoscope. After removal, the vagina should be irrigated with a povidone-iodine solution [11].
Along with examination, various imaging techniques, such as pelvic ultrasonography, pelvic radiography, vaginoscopy, and magnetic resonance imaging may help explore the internal foreign bodies in vaginal and cervical canals [10, 11]. In pediatric patients, transabdominal ultrasound is preferred over transvaginal ultrasound due to the lack of radiation, increased availability and decreased invasiveness [23]. A literature review showed that pelvic ultrasound might fail to visualize non-metallic or metallic VFBs [14], so in this condition, magnetic resonance imaging is considered the best technique for evaluating VFBs in children [10].
The results indicated that vaginal examination using the knee-chest position is the first appropriate step which often successfully discloses the presence of the foreign body and leads to the removal of approximately one-third of the cases [14]. In our patients, the lithotomy position was performed for the first examination. Also, obtaining informed consent before performing a pelvic exam on children’s parents is essential. Assessment for VFB requires questions about issues that may be sensitive to the patient and the personal aspect of a genital exam regarding the patient’s privacy should be noted [20]. In our case, written consent was obtained from the child’s father before the child’s examination. For pharmacological management of similar cases, the consumption of topical estrogen treatment after battery removal and long-term follow-up is suggested to ensure complete vaginal healing without any fistula and record the complications of vaginal stenosis [12, 14].
Psychosomatic psychiatrists play a vital role in children’s psychological well-being and in managing these emergency circumstances. Providing emotional and psychological support by considering counseling sessions and informing families regarding their child’s condition are examples of healthcare providers’ most important activities, especially psychiatrists and emergency ward nurses. Also, presenting education for parents about keeping their children safe by putting all small objects out of reach and about the way of preventing the reoccurrence of these events, especially in children who had multiple episodes of foreign body ingestions, are essential pieces of advice that psychiatrists should consider in the general hospitals [8].
Conclusion
The results of this study highlighted the critical effect of interdisciplinary cooperation among gynecology specialists, pediatric clinicians, psychosomatic psychiatrists, midwives, and nurses in dealing with cases of VFB associated with a wide range of emotional and behavioral disorders, such as ADHD. Meanwhile, in ADHD children, mothers need assistance raising the child, alleviating the child’s disease’s effects, helping stabilize family interactions, and managing their stress and grief reactions. Hence, in ADHD cases, parents should be educated regarding home safety measures and advised to provide appropriate toys for children to minimize accidental insertions.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles are considered in this article.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization and psychiatric evaluation: Forouzan Elyasi; Case management: Imaneh Ahmadi; Direction of the case: Seyed Khosro Ghasempouri; Writing the original draft: Marzieh Azizi and Hamed Milani; Review & editing: Hamed Milani, Leila Monjazeb Marvdashti and Marzieh Azizi; Final approval: All authors.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors acknowledge Mazandaran University of Medical Sciences and all hospital staff involved in patient treatment.
References
Attention-deficit/hyperactivity disorder (ADHD) is childhood’s most common neurobehavioral disorder and the most prevalent chronic health problem affecting school-aged children [1]. According to published literature, the prevalence of ADHD varies significantly due to considerable changes in its diagnostic criteria over time but is reported in 3% to 5% of school-age children [2]. The main symptoms of ADHD are characterized by inattention, hyperactivity, and impulsivity [3]. Children with ADHD may experience significant functional disabilities, such as school difficulties, inability to have appropriate interpersonal relationships with family and peers, low self-esteem, and academic underachievement [1]. Studies revealed that ADHD is frequently comorbid with psychiatric disorders [4, 5] and showed a significant relationship between psychiatric disorders and genitourinary insertion of foreign bodies [6].
Vaginal foreign body (VFB) is an uncommon cause of referral to pediatric and gynecology clinics, usually occurring in ages 3-9 years [7-9]. VFB can present with diverse symptoms, such as vaginal bleeding, severe inflammation, sub-abdominal and suprapubic pain, frequency, burning sensation and dysuria. Among these symptoms, vaginal bleeding is the most reliable symptom of VFB in children [10]. The occurrence of VBF, such as battery insertion in pre-pubertal girls, is responsible for approximately 4% to 10% of the outpatient visits in pediatric and gynecologic wards [11, 12, 13]. Based on the published case reports, although the most commonly inserted VFB in children is small pieces of toilet paper [9, 13-15], other objects, including small nuts, safety pins, hair pins, buttons, crayons, pencils, and disc button lithium battery [7, 9, 10, 14]. Various factors, such as developmental delays, chronic mental or physical disabilities and parents with drug abuse are associated with a higher risk of VFB insertion among children [8].
Although in rare cases, the possibility of an intravaginal foreign body is doubted in pre-pubertal girls by physicians in the emergency wards [7, 16], the availability of electronic instruments requiring batteries in daily life has rapidly increased during the last decade [8]. VFB may be inserted by the child herself during playing due to curiosity of exploring the nature of the body or due to ignorance, sexual stimulation, sexual abuse, psychiatric disorders, and sometimes self-harm [8, 11, 14]. Long-term remaining of foreign bodies in the vagina may lead to severe tissue damage due to the building of sodium hydroxide as a result of the electronic discharge of batteries [8] and also significant morbidities, such as systemic infection and secondary problems, such as perforation, traumatic ulceration of vaginal walls, fistula creation, fibrosis, vaginal stenosis even complete obstruction of the vagina [12, 13]. Accordingly, this study provides a case presentation on vaginal button battery insertion with comorbid ADHD.
Case Presentation
An eight-year-old, second-grade elementary school girl was referred to the general educational hospital in the north with the chief complaint of inserting a VFB. On the night of the event, the child removed a small disc battery of her toys and inserted it into her vagina. Then, she told this action to her parents and was referred to the hospital. The patient was admitted to the gynecology ward, and because of her history of ADHD, psychiatric counseling was considered for her. In the psychiatrist’s assessment, she confirmed that the child had no psychiatric disorders, had normal intelligence, and could communicate with them. According to the obtained history from the patient’s mother, the child was referred to a psychiatrist due to hyperactivity and considerable negligence in the first grade elementary and was treated with Ritalin due to ADHD. She did not take any other medications. Also, the mother mentioned the considerable behavioral changes in her child when she was four years old, but no drug was prescribed for her at that time. In addition, the child’s mother reveals a history of past genital touch in the child.
The patient’s abdomen was soft in physical examination and had a rebound tenderness complaint. Also, the entrance of the vagina was erythematosus, and vaginal discharge was seen. Due to the child’s virginity, no internal examination was performed by a physician. The urine culture and colony count results showed no growth after 48 h. The electrolyte analysis was in a normal range. The range of sodium and potassium was 143 and 4.1 mEq/L, respectively. In urine analysis, 12-14 white blood cells were seen, and other items were normal. The results of the complete blood count test showed a high level of white blood cells (11.3×103 g/dL) and a low level of mean corpuscular volume (74.9 fL) and mean corpuscular hemoglobin (25.1 pg). Pelvic radiography was conducted to specify the location of the button battery (Figures 1 and 2).

After general anesthesia, the patient underwent dorsal lithotomy. The rectal examination was first followed after Prep Drep and the battery was touched in the upper segment of the rectum. Initially, 30 mL of fluid was injected but was ineffective, and 10 mL of the lubricant was reinjected. Then, the battery was gently removed from the wall by rectal examination and milking from the upper.
In the recovery room, the patient was sleepy and febrile with an unknown source of infection and did not communicate visually or verbally. Due to continuous fever, infectious counseling was requested. The pediatric contagious specialist controlled the patient’s fever by prescribing ceftriaxone 1 g intramuscular twice daily and clindamycin 300 mg intravenously every 8 h Ter die sumendum. Also, acetaminophen 300 mg was prescribed intravenous on the condition that the patient’s body temperature was higher than 38 °C. Laboratory tests, such as complete blood cell, C reactive protein, erythrocyte sedimentation rate, urinalysis, ulcerative colitis, and chest x-ray were requested for the patient and the vital signs were checked regularly. Conservative treatment continued for up to 72 h, and the child was transferred to the pediatric ward of another hospital. The child was febrile (38-39 °C) over residency in the hospital. The patient was admitted to another hospital’s infectious service under the treatment of Meropenem antibiotic therapy for 48 h. She was discharged with good general health without fever and recommended outpatient referral to a psychiatric clinic to manage ADHD.
Literature review
The comprehensive literature search was conducted in Google Scholar and PubMed with the following keywords: “Vaginal battery” OR “vaginal button battery” OR “vaginal battery insertion” AND “girl.”
Case reports conducted regarding the insertion of vaginal battery as a VFB in girls were searched and reported in Table 1.
The inclusion criteria were case report studies that uniquely reported the battery as a VFB in the child girls, and other cases reported that VFB were objects except for batteries, such as toilet paper, pen, or other objects were excluded from the literature review section of this study. In addition, English articles with no publication year limitation were considered in this section. The included studies were published from 2005 until 2023.
Discussion
In this case report, an 8-year-old child was introduced who, out of curiosity and due to ADHD, tried to insert a battery in her vagina. Because the child immediately informed her parents, her assessment had no diagnostic challenge. The main challenge was the therapeutic issues and possible chemical damage to the vagina and its complications. This issue in our study case may be attributed to the reality that the child with ADHD may experience the external and internal world in highly idiosyncratic, distorted ways and attempt to adapt to those perceptions. In cases of vaginal battery insertion due to the alkaline type of batteries, the physician needs to roll out the possibility of vaginal burns, perforation, and fistula after suspected vaginal battery insertion [17].
In this case report, the entrance of the child girl’s vagina was erythematosus, and vaginal discharge was seen. Chronic vaginal discharge in children is a significant concern among pediatricians, urologists, and gynecologists [13, 18]. Persistent or recurrent foul-smelling vaginal discharge in a girl may have occurred as a result of several causes, such as primary vaginitis or vulvovaginitis, vulvar skin disease (lichen sclerosis), endocrine abnormalities, vaginal neoplasm, the possibility of undisclosed sexual abuse and also VFB [13, 18, 19].
The symptoms of VFB are often similar to cases of vaginitis and respond temporarily to antibiotics; therefore, foreign bodies are usually treated first medically [14, 20]. Overall, gynecological problems exclusively in pediatric age groups require different management [13], and early identification and timely appropriate management are key issues to achieve better clinical outcomes in these cases and reduce the complications in the children [8]. To distinguish between trauma, carcinoma, and VFB, the patient or her parents should be asked about the recent injuries and a previous history of VFBs [21]. Based on the results of a study, up to 40% of foreign body insertions remain unwitnessed [22]. However, most of these VFB insertions are likely accidental [8].
In some cases, the presence of VFB may indicate sexual abuse. Due to the children being unable to provide a history of an inserted VFB and sexual abuse, the possibility of sexual abuse should be noted and explored in the referred children with complaints of VFB [10]. The child should also be assessed psychologically due to the possibility of emotional and behavioral problems [13, 21]. Our study considered her consultation-liaison psychiatry evaluation to evaluate the case’s psychological status.
In our case, pelvic radiography was performed to diagnose the VFB in the child, and then the VFB was removed under sonography. Therapeutic management was considered according to the place of foreign bodies in the vagina. A low-situated VFB near the introitus can be visualized by separating the labia gently and can be removed easily by small Allis forceps under direct visualization [16, 20]. Initial efforts for removing the VFB in these cases included vaginal irrigation with normal saline; in return, a distally placed foreign body in the vagina may need an examination under anesthesia and removal by a vaginoscope. After removal, the vagina should be irrigated with a povidone-iodine solution [11].
Along with examination, various imaging techniques, such as pelvic ultrasonography, pelvic radiography, vaginoscopy, and magnetic resonance imaging may help explore the internal foreign bodies in vaginal and cervical canals [10, 11]. In pediatric patients, transabdominal ultrasound is preferred over transvaginal ultrasound due to the lack of radiation, increased availability and decreased invasiveness [23]. A literature review showed that pelvic ultrasound might fail to visualize non-metallic or metallic VFBs [14], so in this condition, magnetic resonance imaging is considered the best technique for evaluating VFBs in children [10].
The results indicated that vaginal examination using the knee-chest position is the first appropriate step which often successfully discloses the presence of the foreign body and leads to the removal of approximately one-third of the cases [14]. In our patients, the lithotomy position was performed for the first examination. Also, obtaining informed consent before performing a pelvic exam on children’s parents is essential. Assessment for VFB requires questions about issues that may be sensitive to the patient and the personal aspect of a genital exam regarding the patient’s privacy should be noted [20]. In our case, written consent was obtained from the child’s father before the child’s examination. For pharmacological management of similar cases, the consumption of topical estrogen treatment after battery removal and long-term follow-up is suggested to ensure complete vaginal healing without any fistula and record the complications of vaginal stenosis [12, 14].
Psychosomatic psychiatrists play a vital role in children’s psychological well-being and in managing these emergency circumstances. Providing emotional and psychological support by considering counseling sessions and informing families regarding their child’s condition are examples of healthcare providers’ most important activities, especially psychiatrists and emergency ward nurses. Also, presenting education for parents about keeping their children safe by putting all small objects out of reach and about the way of preventing the reoccurrence of these events, especially in children who had multiple episodes of foreign body ingestions, are essential pieces of advice that psychiatrists should consider in the general hospitals [8].
Conclusion
The results of this study highlighted the critical effect of interdisciplinary cooperation among gynecology specialists, pediatric clinicians, psychosomatic psychiatrists, midwives, and nurses in dealing with cases of VFB associated with a wide range of emotional and behavioral disorders, such as ADHD. Meanwhile, in ADHD children, mothers need assistance raising the child, alleviating the child’s disease’s effects, helping stabilize family interactions, and managing their stress and grief reactions. Hence, in ADHD cases, parents should be educated regarding home safety measures and advised to provide appropriate toys for children to minimize accidental insertions.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles are considered in this article.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization and psychiatric evaluation: Forouzan Elyasi; Case management: Imaneh Ahmadi; Direction of the case: Seyed Khosro Ghasempouri; Writing the original draft: Marzieh Azizi and Hamed Milani; Review & editing: Hamed Milani, Leila Monjazeb Marvdashti and Marzieh Azizi; Final approval: All authors.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors acknowledge Mazandaran University of Medical Sciences and all hospital staff involved in patient treatment.
References
- van den Berg AE, van den Berg CG. A comparison of children with ADHD in a natural and built setting. Child Care Health Dev. 2011; 37(3):430-9. [DOI:10.1111/j.1365-2214.2010.01172.x] [PMID]
- Polanczyk G, Rohde LA. Epidemiology of attention-deficit/hyperactivity disorder across the lifespan. Curr Opin Psychiatry. 2007; 20(4):386-92. [DOI:10.1097/YCO.0b013e3281568d7a] [PMID]
- Trevisanuto D, Parotto M, Doglioni N, Zanardo V, Micaglio M. Upper esophageal lesion following laryngeal mask airway resuscitation in a very low birth weight infant. Resuscitation. 2011; 82(9):1251-2. [DOI:10.1016/j.resuscitation.2011.05.015] [PMID]
- Pliszka SR. Comorbid psychiatric disorders in children with ADHD. In: Barkley RA, editor. Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed. New York: The Guilford; 2015. [Link]
- Van Steensel FJ, Bögels SM, de Bruin EI. Psychiatric comorbidity in children with autism spectrum disorders: A comparison with children with ADHD. J Child Fam Stud. 2013; 22(3):368-76. [DOI:10.1007/s10826-012-9587-z] [PMID] [PMCID]
- Rodríguez D, Thirumavalavan N, Pan S, Apoj M, Butaney M, Gross MS, et al. Epidemiology of genitourinary foreign bodies in the united states emergency room setting and its association with mental health disorders. Int J Impot Res. 2020; 32(4):426-33. [DOI:10.1038/s41443-019-0194-z] [PMID] [PMCID]
- Khan YA, Mahmood M, Taqi E. Disc battery-An unusual vaginal foreign body in a child. APSP J Case Rep. 2016; 7(4):29. [DOI:10.21699/ajcr.v7i4.467] [PMID] [PMCID]
- Kodituwakku R, Palmer S, Paul SP. Management of foreign body ingestions in children: Button batteries and magnets. Br J Nurs. 2017; 26(8):456-61. [DOI:10.12968/bjon.2017.26.8.456] [PMID]
- Al-Oufi D, Alkharboush HM, Younis ND, Abu-Zaid A. Disk battery as a vaginal foreign body in a five-year-old preadolescent child. Cureus. 2021; 13(3):e13727. [DOI:10.7759/cureus.13727] [PMID] [PMCID]
- Chinawa J, Obu H, Uwaezuoke S. Foreign body in vagina: An uncommon cause of vaginitis in children. Ann Med Health Sci Res. 2013; 3(1):102-4. [DOI:10.4103/2141-9248.109463] [PMID] [PMCID]
- Chaurasia A, Gupta V, Mishra A. Vaginal foreign body in a 6 year old girl: A game for the child but a challenge for the gynaecologist. Int J Reprod Contracept Obstet Gynecol. 2015; 4:518-20. [Link]
- Semaan A, Klein T, Vahdad MR, Boemers TM, Pohle R. Severe vaginal burns in a 5-year-old girl due to an alkaline battery in the vagina. J Pediatr Adolesc Gynecol. 2015; 28(5):e147-8. [DOI:10.1016/j.jpag.2014.12.001] [PMID]
- Pallavee P, Samal S, Sabita P. Foreign body in vagina: A cause of persistent vaginal discharge in children. Int J Reprod Contracept Obstet Gynecol. 2013; 2(2):224-5. [Link]
- Nakib G, Calcaterra V, Pelizzo G. Longstanding presence of a vaginal foreign body (battery): Severe stenosis in a 13-year-old girl. J Pediatr Adolesc Gynecol. 2017; 30(1):e15-8. [DOI:10.1016/j.jpag.2016.08.015] [PMID]
- Ma W, Sun YF, Liu JH, He DW, Lin T, Wei GH. Vaginal foreign bodies in children: A single-center retrospective 10-year analysis. Pediatr Surg Int. 2022; 38(4):637-41. [DOI:10.1007/s00383-022-05075-5] [PMID]
- Deligeoroglou E, Deliveliotou A, Laggari V, Tsimaris P, Creatsas G. Vaginal foreign body in childhood: A multidisciplinary approach. J Paediatr Child Health. 2006; 42(10):649-51. [DOI:10.1111/j.1440-1754.2006.00945.x] [PMID]
- Griffin K, Brent R, Vollenhoven B, Swanson AE. Vaginal burn from alkaline battery in an 8-year-old. J Pediatr Adolesc Gynecol. 2015; 28(4):e99-100. [DOI:10.1016/j.jpag.2014.08.010] [PMID]
- Fard SE, Hojati HN, Paydary K, Tajali A, Kajbafzadeh AM. Vaginal bleeding due to insertion of button battery: A case report and review of literature. Thrita. 2014; 3(1):e15853. [DOI:10.5812/thrita.15853]
- Langevin R, Marshall C, Wallace A, Gagné ME, Kingsland E, Temcheff C. Disentangling the associations between attention deficit hyperactivity disorder and child sexual abuse: A systematic review. Trauma Violence Abuse. 2023; 24(2):369-89. [DOI:10.1177/15248380211030234] [PMID] [PMCID]
- Macones GA, Cahill A, Pare E, Stamilio DM, Ratcliffe S, Stevens E, et al. Obstetric outcomes in women with two prior cesarean deliveries: Is vaginal birth after cesarean delivery a viable option? Am J Obstet Gynecol. 2005; 192(4):1223-8; discussion 1228-9. [DOI:10.1016/j.ajog.2004.12.082] [PMID]
- Paradise JE, Willis ED. Probability of vaginal foreign body in girls with genital complaints. Am J Dis Child. 1985; 139(5):472-6. [DOI:10.1001/archpedi.1985.02140070046031] [PMID]
- Preece JM, Cornette L, El-Hindy N. Simple management of isolated proptosis at birth. Arch Dis Child Fetal Neonatal Ed. 2005; 90(3):F234. [DOI:10.1136/adc.2005.071365] [PMID] [PMCID]
- Chiorean L, Schreiber-Dietrich D, Braden B, Cui XW, Buchhorn R, Chang JM, et al. Ultrasonographic imaging of inflammatory bowel disease in pediatric patients. World J Gastroenterol. 2015; 21(17):5231-41. [DOI:10.3748/wjg.v21.i17.5231] [PMID] [PMCID]
- Yanoh K, Yonemura Y. Severe vaginal ulcerations secondary to insertion of an alkaline battery. J Trauma. 2005; 58(2):410-2. [DOI:10.1097/01.TA.0000068993.90723.46] [PMID]
- Huppert J, Griffeth S, Breech L, Hillard P. Vaginal burn injury due to alkaline batteries. J Pediatr Adolesc Gynecol. 2009; 22(5):e133-6. [DOI:10.1016/j.jpag.2008.10.009] [PMID]
- Dubuc E, Ralph C, Kives S. Severe vaginal burns caused by a battery: A case report. J Pediatr Adolesc Gynecol. 2014; 27(2):e34-5. [Link]
- Dwiggins M, Chan S, Benoit J, Trotman G. Vaginal burns after brief exposure to an alkaline battery in a pre-pubertal girl. J Pediatr Adolesc Gynecol. 2016; 29(2):183-4. [DOI:10.1016/j.jpag.2016.01.060]
- Herle K, Bal HS. A rare cause of vaginal discharge in a pre-pubertal girl. APSP J Case Rep. 2017; 8(4):25. [DOI:10.21699/ajcr.v8i4.605]
- Massa AC, Tavares M, Carvalho T, Simões M. A 7-year-old girl with vaginal burn from exposure to an alkaline battery (Rapariga de 7 anos com queimadura vaginal por exposição a pilhas alcalinas). Acta Obstet Ginecol Port. 2018; 12(3):224-7. [Link]
- Chidambaram VC, Pallavee P. Foreign body in vagina: A cause of persistent vaginal discharge in a prepubescent child. Int J Reprod Contracept Obstet Gynecol. 2020; 9(9):3883-5. [Link]
- Guanà R, Carpino A, Garbagni G, Morchio C, Garofalo S, Pane A, et al. Endoscopic treatment of a severe vaginal stenosis following battery insertion in an 11-year-old girl. European J Pediatr Surg Rep. 2022; 10(01):e135-40. [DOI:10.1055/a-1920-5849] [PMID] [PMCID]
- Bapir R, Ahmed NHA, Othman S, Mohammed DH, Mohammed SH, Rahim HM, et al. Vaginal discharge in a 2-year-old patient caused by an alkaline battery: A case report. J Pediatr Surg Case Rep. 2023; 91:102589. [DOI:10.1016/j.epsc.2023.102589]
Type of Study: Case & Review |
Subject:
Gynecology and Obstetrics
Received: 2023/09/30 | Accepted: 2024/03/27 | Published: 2024/04/1
Received: 2023/09/30 | Accepted: 2024/03/27 | Published: 2024/04/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






