Volume 12, Issue 3 (7-2024)
J. Pediatr. Rev 2024, 12(3): 283-294 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Salari S, Shaygan M, Setoodeh G, Ghaemmaghami P. The Predictive Role of Maladaptive Schemas in Chronic Pain of Adolescents. J. Pediatr. Rev 2024; 12 (3) :283-294
URL: http://jpr.mazums.ac.ir/article-1-581-en.html
URL: http://jpr.mazums.ac.ir/article-1-581-en.html
1- Department of Psychiatric Nursing, School of Nursing and Midwifery, Shiraz University of Medical Sciences, Shiraz, Iran.
2- Department of Psychiatric Nursing, School of Nursing and Midwifery, Shiraz University of Medical Sciences, Shiraz, Iran. ,m2620.shaygan@gmail.com
2- Department of Psychiatric Nursing, School of Nursing and Midwifery, Shiraz University of Medical Sciences, Shiraz, Iran. ,
Full-Text [PDF 446 kb]
(714 Downloads)
| Abstract (HTML) (1868 Views)
Full-Text: (766 Views)
Introduction
Recent research findings highlight a concerning increase in the prevalence of chronic pain among children and adolescents. For instance, a comprehensive systematic review indicates that pediatric chronic pain is estimated to affect 11% to 38% of this population [1]. Notably, the prevalence of chronic pain among children and adolescents in Spain, involving a cohort of 1,115 individuals aged 8-18 years old, is notably high at 46% [2]. Similarly, in New Zealand, a substantial proportion of students aged 12-18 years (22.8%) reported experiencing chronic pain for 6 months or more [3].
The most commonly reported complaints by adolescents include stomach pain, back pain, headaches and musculoskeletal pain. Chronic pain exerts negative impacts on various aspects of adolescents’ lives, including school attendance and peer relationships and can even be accompanied by anxiety and depression [4]. It is essential to recognize that pain is not only a physical sensation but also serves as an indicator of the patient’s psychological distress [5]. Therefore, pain evaluations should encompass dynamic and intricate physiological, psychological and social interactions, adopting the bio-psycho-social model [6]. The International Association for the Study of Pain (IASP) has identified psychological factors as diverse predictors of pain intensity. Specifically, experiences during childhood that diminish the sense of safety have been linked to a higher risk of chronic pain in children and adolescents. [7, 8]. Furthermore, research suggests that early-life psychosocial adversities, such as maltreatment, violence, and extreme poverty, can significantly impact a child’s growth trajectory, physical health status, and various body systems throughout his/her life [9]. The results of a study suggest a significant association between childhood trauma and the long-term reporting of pain within the studied populations [10].
Adverse and distressing experiences during childhood and adolescence lead to extensive and enduring patterns, including memories, cognitions, emotions, and physical sensations, known as “maladaptive schemas.” These schemas become activated in response to various stimuli throughout life, leading to distorted interpretations of events and subsequent experiences of distressing emotions, ultimately resulting in maladaptive and harmful behavioral responses. Maladaptive schemas are classified into five domains based on unmet emotional needs during early life: Disconnection/rejection, impaired autonomy/performance, over-vigilance/inhibition, other-directedness, and impaired limits [11, 12]. According to Young et al. model, these maladaptive schemas can contribute to various psychological pathologies [12]. For example, the disconnection/rejection domain emerges from unfulfilled needs for stability, security, love, affection and a sense of belonging. It is associated with mood disorders, such as depression, eating disorders and personality disorders. The impaired autonomy/performance domain arises when an individual’s expectations of him/herself interfere with his/her perceived abilities for independent functioning and successful task performance, often leading to anxiety disorders. Moreover, individuals with impaired limits exhibit deficits and inadequacies in internal constraints and a sense of responsibility toward others or may display a tendency toward long-term life goals, potentially leading to aggression and substance abuse. Additionally, in the other-directedness domain, there is an excessive focus on fulfilling the inclinations, emotions and wishes of others to gain love and acquiescence surrender, often at the cost of disregarding the individual’s requirements. Lastly, the over-vigilance/-inhibition domain emerges from an extreme emphasis on self-restraint, suppression of emotions and impulses, or rigid and internalized rules and expectations, resulting in a loss of happiness, self-expression, peace of mind, close relationships and overall well-being [12–23].
While the connection between chronic pain and emotional problems, including depression, as potential outcomes of maladaptive schemas is gaining recognition [24–26], the exploration of the relationship between maladaptive schemas and chronic pain remains limited. For instance, Heshmati conducted a study on 100 students using a non-probability sampling method, and revealed that disconnection/rejection, over-vigilance/inhibition, and other-directedness were the most related domains to chronic pain in students [27]. Additionally, two recent studies by Vakili et al. and Heshmati et al. with samples of 100 adults and 201 undergraduate students, respectively, reported that depression acted as a mediator in the relationship between maladaptive schemas and chronic pain [28, 29]. In a study involving 300 patients, individuals’ inclination toward employing cognitive emotion regulation strategies mediated the association between maladaptive schemas and the perception of chronic pain [30].
Despite previous studies facing limitations related to small sample sizes [27–29] and convenience sampling [28–30], the present study aimed to overcome these challenges by investigating the predictive role of adolescents’ maladaptive schemas in their chronic pain. Emphasizing the need for further research with larger sample sizes, mainly focusing on less-discussed factors, like psychological experiences during childhood, the study aimed to provide a comprehensive understanding of the interplay between these factors in adolescents and their influence on chronic pain.
Methods
This cross-sectional research was carried out in Shiraz, Iran, from January to June 2021.
Participants
The study comprised youths aged between 12 and 21 years [31]. A total of 1334 adolescents were randomly chosen to participate in the research. Inclusion criteria were the youths who attended educational institutions in Shiraz and were content and capable of completing online-based questionnaires. Adolescents with physical conditions unrelated to pain, persistent mental illnesses, or developmental disorders were excluded from the study, as well as those without parental contact.
Sample size determination
To determine the sample size, the researchers utilized G*Power software, version 3, considering a statistical power of 95% and five variables, and relying on data from a prior study (R2=0.06) [32]. Initially, the calculated sample size was 320 participants. However, given the expectation that at least 30% of adolescents in Shiraz might be afflicted by chronic pain [33], the minimum required sample size was set at 1067. Taking into account an estimated 25% dropout rate, the final sample size was determined to be at least 1,334 adolescents.
Sampling process
The participant selection involved utilizing a systematic sampling method. This entailed the random selection of 840 high school students aged between 12 and 18, as well as 494 college students aged between 18 and 21, to participate in the study. In the initial stage, 16 schools were randomly chosen from various Shiraz districts. From each selected high school, 52 students were included through random sampling. Similarly, 17 faculties were randomly selected from Shiraz, with approximately 29 students recruited from each faculty.
Questionnaires
Chronic pain assessment
In addition to gathering demographic data, including age, gender, birth order, parents’ occupation and educational background, the evaluation of chronic pain utilized three screening queries derived from the 11th revision of the international classification of diseases (ICD-11) [34]:
1) Are you presently experiencing any pain, and if so, is it chronic or occasional? 2) Have you endured this pain or inconvenience for over three months? 3) Does this pain and inconvenience significantly impact your mundane and daily activities?
After providing affirmative responses to all three questions, the adolescents underwent a further assessment to determine their pain’s underlying cause, frequency, history, and intensity [35]. Each adolescent fulfilled the assessment forms independently. In our prior study, we confirmed the quantitative face validity of each item by calculating their impact scores, all of which were ≥1.5. We also conducted both qualitative and quantitative evaluations of content validity, with the content validity ratio (CVR) for the items falling between 0.87 and 1, surpassing the minimum acceptable value. To assess reliability using the re-test method, we had 80 respondents answer the same questions again after two weeks and all the questions demonstrated a correlation coefficient ≥0.74 [33].
Maladaptive cognitive schemas
Assessment of maladaptive cognitive schemas in adolescents was carried out using the Young’s schema questionnaire-short form (YSQ-SF). The short form of this questionnaire comprises 75 items, and participants replied to each item on a 6-point Likert scale, where one indicates “completely untrue of me” and six indicates “describes me perfectly.” The YSQ-SF evaluates 15 maladaptive schemas across five domains: Disconnection/rejection, autonomy/impaired performance, other-directedness, over-vigilance/inhibition and impaired limits. If the total scores for any of these domains exceed 25, it indicates the presence of a maladaptive schema in that area [36]. Multiple studies have provided evidence for the YSQ-SF’s favorable validity and reliability [37 ,38].
In Khosravani et al. research, the Persian version of the instrument employed in this study exhibited strong reliability (Cronbach’s α=0.75-0.91) and confirmed criterion, predictive and discriminant validity [39]. The questionnaire demonstrated excellent internal consistency in the current study, with coefficient omega values of 0.95 for the overall questionnaire, 0.89 for disconnection/rejection, 0.89 for impaired autonomy/performance, 0.80 for other-directedness, 0.81 for over-vigilance/inhibition and 0.82 for impaired limits.
Statistical analysis
In the statistical analysis, descriptive measures (Mean±SD for continuous variables and frequencies and percentages for categorical variables) were used to describe demographic characteristics. A univariate logistic regression approach was utilized to investigate potential predictors (independent variables) associated with chronic pain, including age, gender, birth order, parental career and education and maladaptive schemas.
Variables with significance levels <0.2 or showing a notable association with chronic pain in univariate analyses were selected for hierarchical multiple regression analyses (method: Enter). Demographic characteristics were initially examined for their relationship with chronic pain. Subsequently, parental chronic pain was introduced into the regression model, considering its known impact on pediatric chronic pain [40]. Finally, maladaptive schemas were added to assess their contribution to explaining the variance in chronic pain, controlling for previously entered variables. Adjusted odds ratios and 95% confidence intervals (CI) were calculated and reported. SPSS software, version 22 was used for all statistical analyses, with a predetermined significance level of <0.05.
Results
Sample characteristics
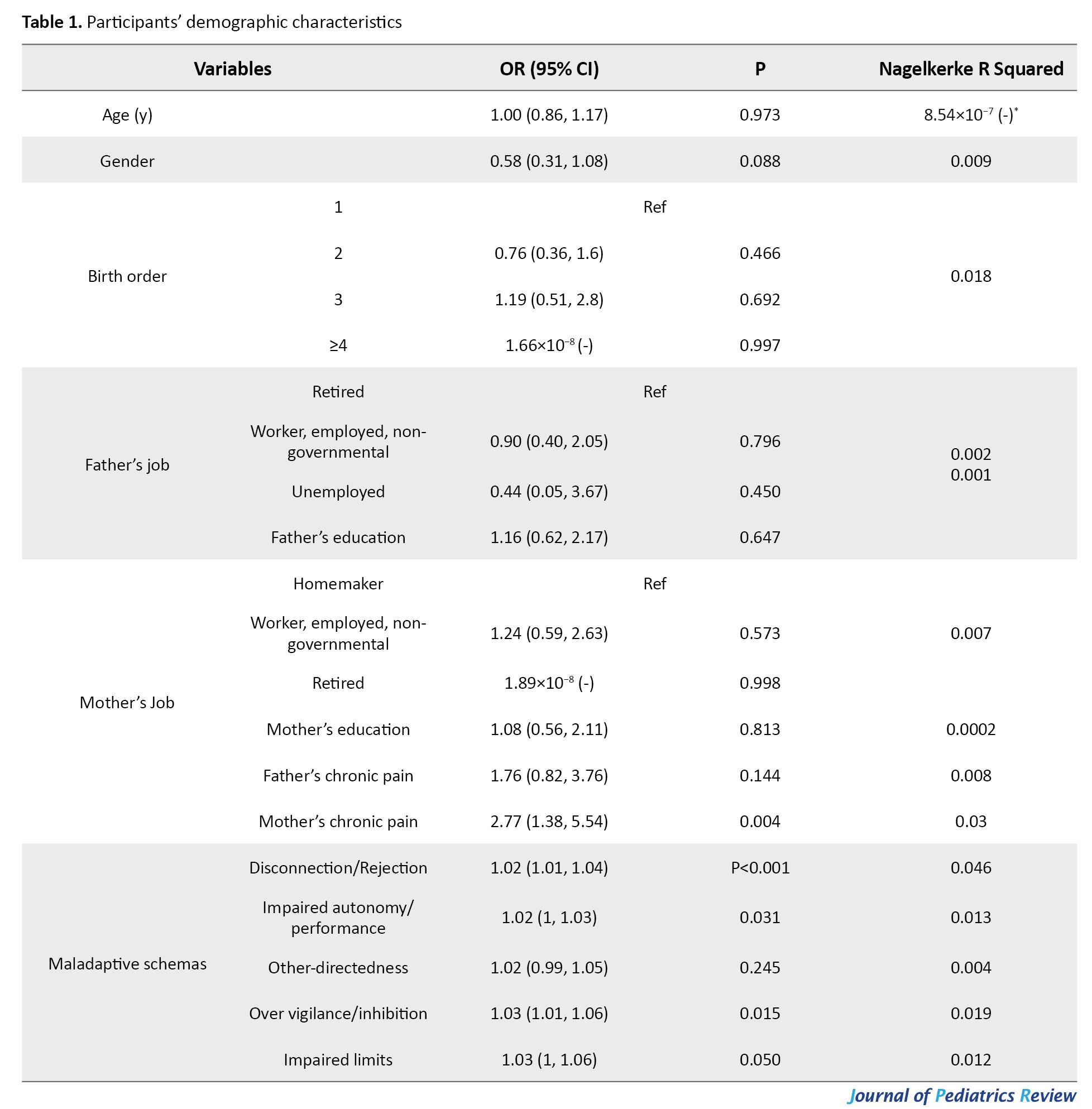
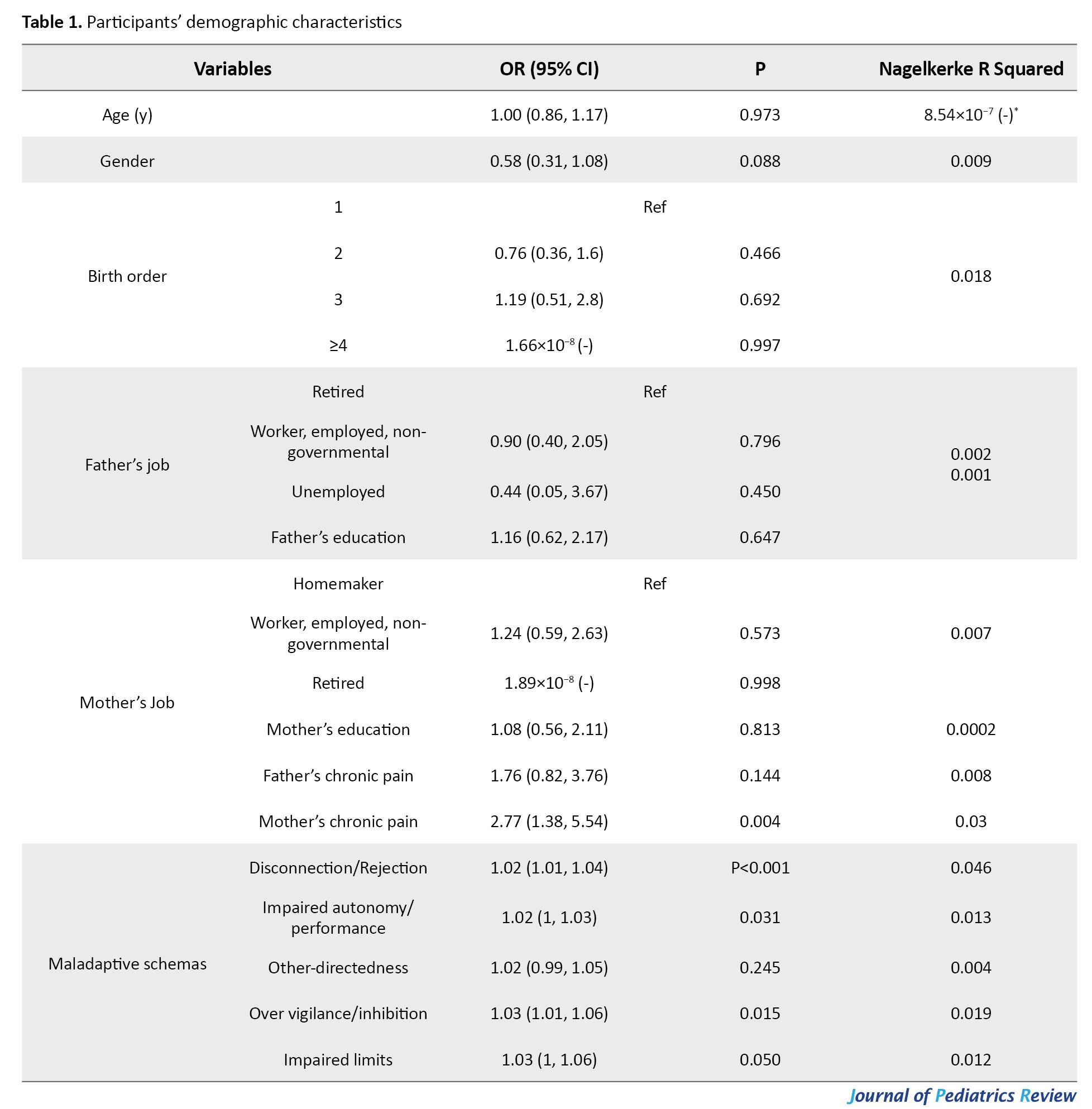
Among the 1333 adolescents invited to participate, 1302 took part in the study, resulting in an impressive response rate of 97.67%. The participants’ Mean±SD age was 16.87±1.94, ranging from 12 to 21 years. Most participants were male (53.70%), and approximately 53.80% were the eldest child in their family. Regarding education, most fathers (62.80%) and mothers (70.70%) had completed a diploma or had a lower education level. Regarding employment, most fathers (80.40%) were employed, while most mothers (80.10%) were housewives. A detailed breakdown of the participants’ demographic characteristics can be found in Table 1.
Characteristics of chronic pain
The pain attributes of the adolescent participants are presented in Table 2.
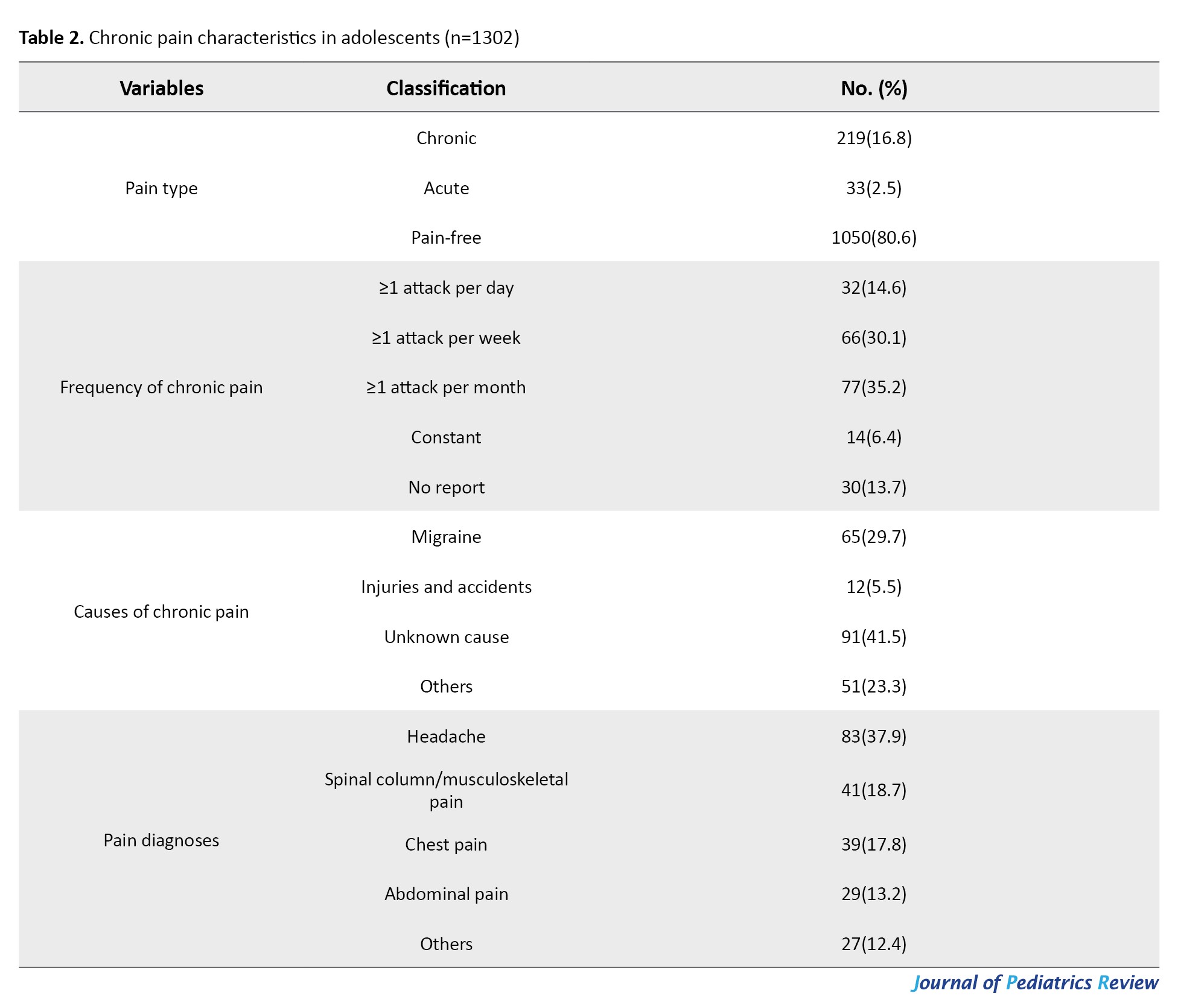
Out of all the participants, 219 adolescents (16.8%) met the ICD-11 criteria for chronic pain. The average pain intensity reported by these individuals over the preceding two weeks was recorded at 4.74±2.48. Among those experiencing chronic pain, the majority (35.2%) reported having pain attacks at least once a month. The most prevalent types of chronic pain reported by adolescents were headaches (37.90%) and musculoskeletal pain related to the spinal column (18.70%).
Univariate logistic regression models
In the analysis using univariate logistic regression with no-chronic pain as the reference group, several factors were examined to assess their correlation with chronic pain. These factors included age, gender, birth order, father’s career, father’s educational status, mother’s career, mother’s educational status, and father’s chronic pain, as well as other-directedness and impaired limits (Table 3).
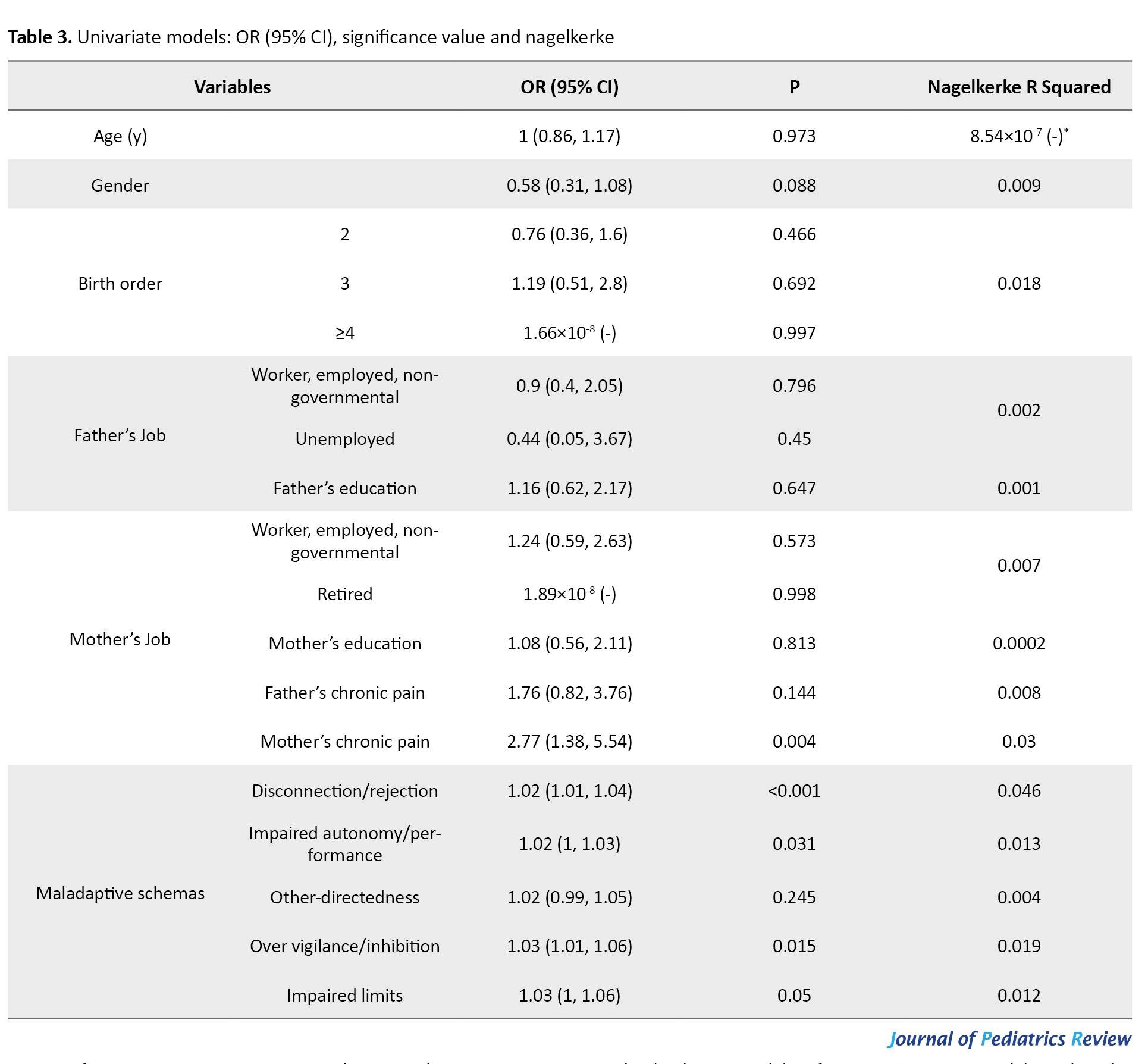
As single predictors, none of these variables showed a significant correlation with chronic pain.
However, three variables demonstrated significant associations with chronic pain. These were the mother’s chronic pain, which explained 3% of the variance, impaired autonomy and performance, which explained 1.3% of the variance, and over-vigilance and inhibition, which explained 1.9% of the variance. Additionally, the “disconnection/rejection” domain exhibited a significant association with chronic pain and displayed the best model fit, explaining 4.6% of the variance (Table 3).
Multiple regression analyses
Table 4 displays the hierarchical logistic regression analysis outcomes, which examined the contributions of variable blocks entered simultaneously in predicting chronic pain.
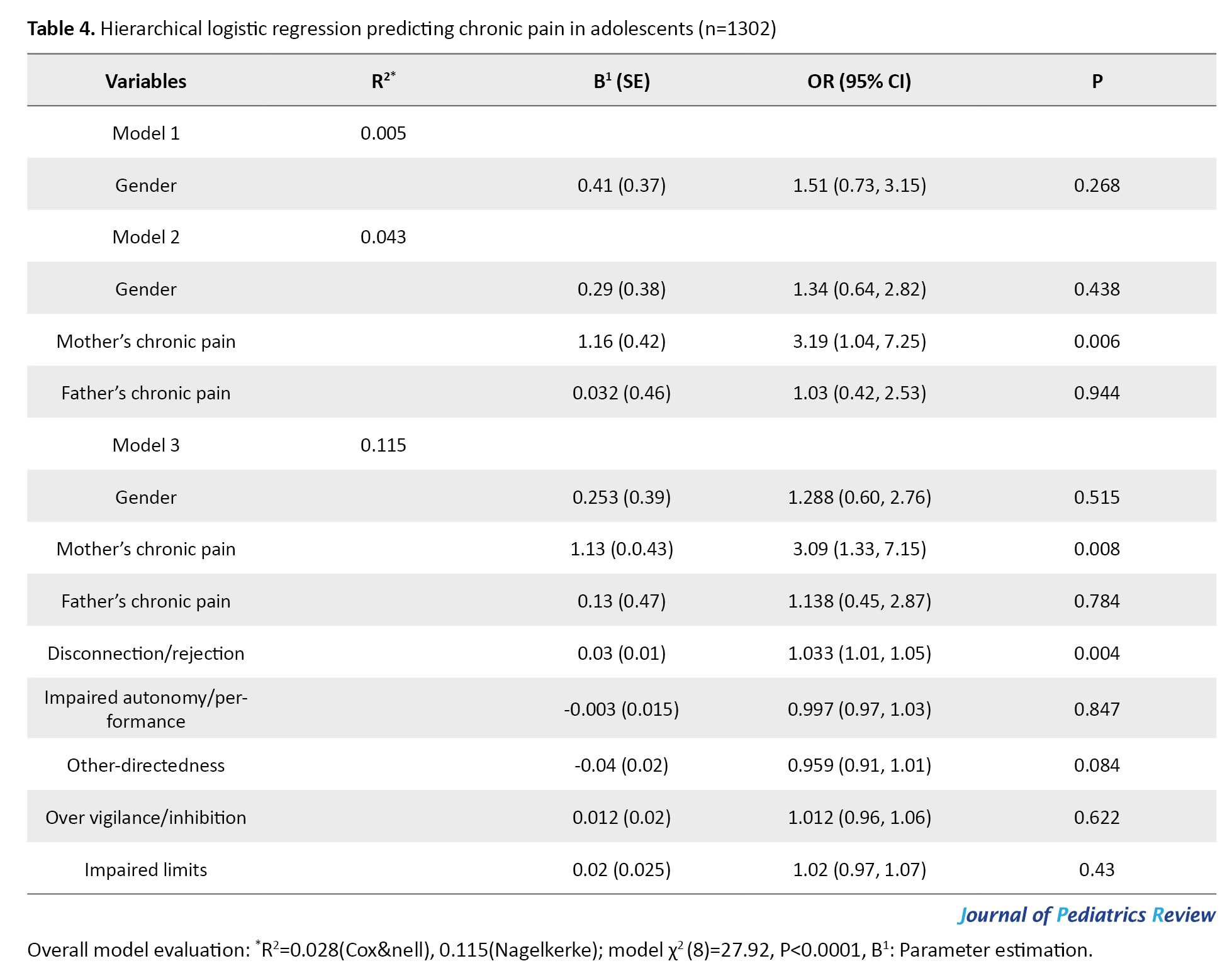
The first step of the hierarchical regression assessed the significance of gender (P<0.2) in the univariate model, revealing that gender did not significantly contribute to chronic pain. In the second step, the model included gender, a mother’s chronic pain and a father’s chronic pain. While the mother’s chronic pain emerged as a significant predictor (b=1.16, P=0.006) in this model, the father’s chronic pain and gender did not show significant associations. This model explained 3.8% of the variance [∆R2=0.043-0.005] compared to the previous model (R2=0.5%). Lastly, the model incorporated schemas. The “disconnection/rejection” domain (OR=0.997, P=0.004) was found to contribute to the prediction of chronic pain. Additionally, a mother’s chronic pain (OR=0.878, P=0.008) continued to be a predictive factor in this model. Including schemas led to a substantial 7.2% [∆R2=0.115-0.043] enhancement in the explained variance, resulting in a total explained variance of 11.5%.
Discussion
This research is directed at exploring the predictive role of various maladaptive schema domains in the development of chronic pain in adolescents. Based on the study outcomes, it was found that chronic pain in mothers can predict chronic pain in adolescents. Additionally, the disconnection/rejection domain was identified as a predictor of chronic pain in adolescents.
Furthermore, the outcomes of this study showed a noticeable conjunction between chronic pain in adolescents and chronic pain in their mothers. According to research findings, the diminished overall health (both mental and physical) of parents was indirectly linked to increased interference with child pain. This connection was mediated first by heightened parent pain catastrophizing, followed by an escalation in both parent protective behaviors and child pain catastrophizing [41]. Children of mothers with chronic pain are at a higher risk of experiencing chronic pain and related harmful mental and somatic health consequences [40, 42]. Stone and Wilson proposed five potential mechanisms in their model for the relationship between chronic pain in parents and chronic pain in children, along with related destructive issues: 1) Genetics, 2) Changes in early neural development, 3) Social learning of pain-specified behaviors (catastrophizing their own or their child’s pain), 4) General parenting and family health, and 5) Exposure to demanding surroundings. Moreover, the model includes three potential mediators: 1) The existence of chronic pain in the other parent, 2) the timing, duration, and location of the parents’ chronic pain, and 3) the features of the children (gender, stage of development, race or ethnicity, and temperament). All of these factors likely impact the expansion of chronic pain and its connected consequences for children of parents with chronic pain. Specifically, chronic pain in mothers may affect the neural development of their children through stress and health behaviors during pre- and perinatal periods [40].
Another finding of this study indicates that, among various factors, the domain of disconnection or rejection can predict chronic pain in adolescents. This finding aligns with Heshmati’s study, which reported the predictive role of the disconnection/rejection domain in chronic pain among university students [27].
Individuals with the disconnection/rejection domain struggle to form secure and satisfying emotional attachments. As a result, they experience various emotions, such as abandonment, distrust, neglect, shame, guilt, and alienation. This cognitive pattern is likely to develop in families characterized by emotional coldness, distance, isolation, unpredictability, and a lack of trust [12]. Among the psychosocial factors that are effective and influential in chronic pain based on the bio-psycho-social model [6], inefficient family system behaviors have been noted [43]. Specific parental characteristics, such as emotional neglect that leads to unmet adolescent needs and the formation of this maladaptive schema domain, are associated with chronic pain [10, 11, 44-47]. The various negative emotions experienced by adolescents in such families, manifesting through this maladaptive schema domain, can all threaten mental health [17, 21–23, 48]. Additionally, Vakili et al. demonstrated in their study that the disconnection/rejection domain mediates chronic pain through depression in chronic pain patients [28]. Furthermore, given the overlap between chronic pain and poor mental health, it has been established that factors, such as decreased quality of life, negative emotions, depression, stress, etc. can lead to chronic pain [49–54].
Moreover, according to Brown’s perspective, maladaptive schemas impact how a person perceives and pays attention to various stimuli, potentially leading to misunderstandings of senses and physical cues [55]. Also, Riebel et al. demonstrated that individuals with somatoform disorders hold self-views of vulnerability and an incapacity to cope with tension [56]. Hence, maladaptive schemas are involved in either initiating or perpetuating pain by misunderstanding physical senses and engaging in catastrophic thinking about physical symptoms.
Another noteworthy point is that individuals with maladaptive schemas are less inclined to seek help to reduce their pain. They believe that no one can assist them, which may lead them to express physical grievances and psychosomatic disorders as a means of attracting attention and care from others, as mentioned by Yang et al. [50]. However, this function is often beyond their conscious awareness, and the secondary gain can positively reinforce and perpetuate pain in these individuals. In other words, individuals with a domain of rejection or abandonment may have an unconscious inclination to experience pain [27]. From another perspective, individuals with such schemas tend to avoid expressing their emotions, thereby describing their physiological aspects, including pain, in physical terms due to limited emotional awareness and verbal ability [28].
To sum up, the current results reveal that the domain of rejection and abandonment holds predictive value for chronic pain in adolescents. This investigation provides a novel perspective on the contributing factors to chronic pain in this age group, elucidating the connection between maladaptive schemas and prevalent physical issues, like chronic pain. As a result, these findings can have implications for schema therapy interventions for patients with chronic pain. By incorporating cognitive, behavioral, and relational approaches, the outcomes of this study can facilitate the modification of maladaptive schemas, ultimately leading to pain reduction in individuals suffering from chronic pain. Furthermore, these discoveries potentially benefit both families and school teachers, as they play pivotal roles in shaping the cognitive schemas of children and adolescents. In this context, fostering close and affectionate relationships with children, providing appropriate emotional support, and setting reasonable and rational expectations can be crucial in minimizing the risk of developing or exacerbating pain in adolescents. Encouraging positive parental behaviors that foster constructive and enriching experiences during childhood and adolescence, while meeting their needs and consequently fostering adaptive schemas [57, 58] can help reduce the likelihood of maladaptive schemas, particularly in the domain of rejection/abandonment [59, 60]. This approach can contribute to building trust, independence, self-esteem, a sense of worth, and an enhanced capacity to form secure relationships in adolescents. All these factors play vital roles in improving their physical and psychological well-being, and a lack of them can lead to physical health disadvantages [61–63]. The results of this study can also offer valuable insights for family therapy, group therapy, and educational programs focused on appropriate interactions with adolescents dealing with chronic pain. Conversely, by implementing policies promoting healthier lifestyles and enhancing overall community well-being, we can anticipate a reduction in chronic pain among families, encompassing both parents and children.
The present study has some restrictions that should be acknowledged. Firstly, chronic pain assessment relied on self-report questionnaires rather than clinical examinations, potentially introducing some degree of response bias to the measured variables [64]. However, it is crucial to consider McCaffrey’s perspective, which argues that pain is subjective and persists for as long as the individual perceives it [65]. Secondly, the study’s cross-sectional design deters us from the foundation of spontaneous relations based on the current findings. To gain a deeper understanding of how adolescents’ psychological characteristics contribute to chronic pain, further prospective longitudinal studies are necessary. Moreover, since the questionnaires were completed online, there is uncertainty regarding whether all adolescents completed them. Additionally, there are other factors not investigated in this study that play a role in influencing chronic pain among adolescents. Therefore, it is strongly advised to conduct further research to explore additional psychosocial variables not considered in this study. Furthermore, replicating this study with diverse samples encompassing various age groups and cultural backgrounds would be advantageous for assessing the generalizability of the findings.
Conclusion
Considering the growing prevalence of chronic pain among adolescents lately, it becomes crucial to recognize the elements that contribute to this issue. One such factor is cognitive schemas in adolescents, although prior research has primarily focused on their impact on psychological well-being rather than chronic pain. Consequently, this study sought to investigate the following question: “Can maladaptive schemas predict the development of chronic pain in adolescents?” The findings of this study indicated that chronic pain in mothers, along with maladaptive schemas related to rumination and avoidance in adolescents, could influence the occurrence of chronic pain in this age group. Interventions aimed at preventing or modifying maladaptive schemas in adolescents could play a pivotal role in effectively managing chronic pain within this population. It is essential for parents and guardians to become familiar with maladaptive schemas, recognize the significance of employing effective communication strategies and acquire the necessary knowledge and skills to address the psychological needs of adolescents. Building upon the insights from this study, implementing cognitive-behavioral educational programs targeted at modifying or reducing maladaptive schemas for parents, guardians, and adolescents could prove instrumental in diminishing the likelihood of developing or exacerbating chronic pain among adolescents.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shiraz University of Medical Sciences (Code: IR.SUMS.REC.1399.1033). Eligible participants were informed about the research’s purpose and were emphasized that their involvement was entirely voluntary. An electronic informed consent form was completed by all the adolescents. Data collection was conducted anonymously, without any reference to individuals’ names.
Funding
This research was financially supported by Shiraz University of Medical Sciences (Grant No.: 22110).
Authors contributions
Conceptualization: Maryam Shaygan and Giti Setoodeh; Study design: Parvin Ghaemmaghami; Investigation: Saghar Salari; Writing the original draft: Saghar Salari and Maryam Shaygan; Review, editing and final approval: All authors.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank all adolescents who participated in this study.
References
Recent research findings highlight a concerning increase in the prevalence of chronic pain among children and adolescents. For instance, a comprehensive systematic review indicates that pediatric chronic pain is estimated to affect 11% to 38% of this population [1]. Notably, the prevalence of chronic pain among children and adolescents in Spain, involving a cohort of 1,115 individuals aged 8-18 years old, is notably high at 46% [2]. Similarly, in New Zealand, a substantial proportion of students aged 12-18 years (22.8%) reported experiencing chronic pain for 6 months or more [3].
The most commonly reported complaints by adolescents include stomach pain, back pain, headaches and musculoskeletal pain. Chronic pain exerts negative impacts on various aspects of adolescents’ lives, including school attendance and peer relationships and can even be accompanied by anxiety and depression [4]. It is essential to recognize that pain is not only a physical sensation but also serves as an indicator of the patient’s psychological distress [5]. Therefore, pain evaluations should encompass dynamic and intricate physiological, psychological and social interactions, adopting the bio-psycho-social model [6]. The International Association for the Study of Pain (IASP) has identified psychological factors as diverse predictors of pain intensity. Specifically, experiences during childhood that diminish the sense of safety have been linked to a higher risk of chronic pain in children and adolescents. [7, 8]. Furthermore, research suggests that early-life psychosocial adversities, such as maltreatment, violence, and extreme poverty, can significantly impact a child’s growth trajectory, physical health status, and various body systems throughout his/her life [9]. The results of a study suggest a significant association between childhood trauma and the long-term reporting of pain within the studied populations [10].
Adverse and distressing experiences during childhood and adolescence lead to extensive and enduring patterns, including memories, cognitions, emotions, and physical sensations, known as “maladaptive schemas.” These schemas become activated in response to various stimuli throughout life, leading to distorted interpretations of events and subsequent experiences of distressing emotions, ultimately resulting in maladaptive and harmful behavioral responses. Maladaptive schemas are classified into five domains based on unmet emotional needs during early life: Disconnection/rejection, impaired autonomy/performance, over-vigilance/inhibition, other-directedness, and impaired limits [11, 12]. According to Young et al. model, these maladaptive schemas can contribute to various psychological pathologies [12]. For example, the disconnection/rejection domain emerges from unfulfilled needs for stability, security, love, affection and a sense of belonging. It is associated with mood disorders, such as depression, eating disorders and personality disorders. The impaired autonomy/performance domain arises when an individual’s expectations of him/herself interfere with his/her perceived abilities for independent functioning and successful task performance, often leading to anxiety disorders. Moreover, individuals with impaired limits exhibit deficits and inadequacies in internal constraints and a sense of responsibility toward others or may display a tendency toward long-term life goals, potentially leading to aggression and substance abuse. Additionally, in the other-directedness domain, there is an excessive focus on fulfilling the inclinations, emotions and wishes of others to gain love and acquiescence surrender, often at the cost of disregarding the individual’s requirements. Lastly, the over-vigilance/-inhibition domain emerges from an extreme emphasis on self-restraint, suppression of emotions and impulses, or rigid and internalized rules and expectations, resulting in a loss of happiness, self-expression, peace of mind, close relationships and overall well-being [12–23].
While the connection between chronic pain and emotional problems, including depression, as potential outcomes of maladaptive schemas is gaining recognition [24–26], the exploration of the relationship between maladaptive schemas and chronic pain remains limited. For instance, Heshmati conducted a study on 100 students using a non-probability sampling method, and revealed that disconnection/rejection, over-vigilance/inhibition, and other-directedness were the most related domains to chronic pain in students [27]. Additionally, two recent studies by Vakili et al. and Heshmati et al. with samples of 100 adults and 201 undergraduate students, respectively, reported that depression acted as a mediator in the relationship between maladaptive schemas and chronic pain [28, 29]. In a study involving 300 patients, individuals’ inclination toward employing cognitive emotion regulation strategies mediated the association between maladaptive schemas and the perception of chronic pain [30].
Despite previous studies facing limitations related to small sample sizes [27–29] and convenience sampling [28–30], the present study aimed to overcome these challenges by investigating the predictive role of adolescents’ maladaptive schemas in their chronic pain. Emphasizing the need for further research with larger sample sizes, mainly focusing on less-discussed factors, like psychological experiences during childhood, the study aimed to provide a comprehensive understanding of the interplay between these factors in adolescents and their influence on chronic pain.
Methods
This cross-sectional research was carried out in Shiraz, Iran, from January to June 2021.
Participants
The study comprised youths aged between 12 and 21 years [31]. A total of 1334 adolescents were randomly chosen to participate in the research. Inclusion criteria were the youths who attended educational institutions in Shiraz and were content and capable of completing online-based questionnaires. Adolescents with physical conditions unrelated to pain, persistent mental illnesses, or developmental disorders were excluded from the study, as well as those without parental contact.
Sample size determination
To determine the sample size, the researchers utilized G*Power software, version 3, considering a statistical power of 95% and five variables, and relying on data from a prior study (R2=0.06) [32]. Initially, the calculated sample size was 320 participants. However, given the expectation that at least 30% of adolescents in Shiraz might be afflicted by chronic pain [33], the minimum required sample size was set at 1067. Taking into account an estimated 25% dropout rate, the final sample size was determined to be at least 1,334 adolescents.
Sampling process
The participant selection involved utilizing a systematic sampling method. This entailed the random selection of 840 high school students aged between 12 and 18, as well as 494 college students aged between 18 and 21, to participate in the study. In the initial stage, 16 schools were randomly chosen from various Shiraz districts. From each selected high school, 52 students were included through random sampling. Similarly, 17 faculties were randomly selected from Shiraz, with approximately 29 students recruited from each faculty.
Questionnaires
Chronic pain assessment
In addition to gathering demographic data, including age, gender, birth order, parents’ occupation and educational background, the evaluation of chronic pain utilized three screening queries derived from the 11th revision of the international classification of diseases (ICD-11) [34]:
1) Are you presently experiencing any pain, and if so, is it chronic or occasional? 2) Have you endured this pain or inconvenience for over three months? 3) Does this pain and inconvenience significantly impact your mundane and daily activities?
After providing affirmative responses to all three questions, the adolescents underwent a further assessment to determine their pain’s underlying cause, frequency, history, and intensity [35]. Each adolescent fulfilled the assessment forms independently. In our prior study, we confirmed the quantitative face validity of each item by calculating their impact scores, all of which were ≥1.5. We also conducted both qualitative and quantitative evaluations of content validity, with the content validity ratio (CVR) for the items falling between 0.87 and 1, surpassing the minimum acceptable value. To assess reliability using the re-test method, we had 80 respondents answer the same questions again after two weeks and all the questions demonstrated a correlation coefficient ≥0.74 [33].
Maladaptive cognitive schemas
Assessment of maladaptive cognitive schemas in adolescents was carried out using the Young’s schema questionnaire-short form (YSQ-SF). The short form of this questionnaire comprises 75 items, and participants replied to each item on a 6-point Likert scale, where one indicates “completely untrue of me” and six indicates “describes me perfectly.” The YSQ-SF evaluates 15 maladaptive schemas across five domains: Disconnection/rejection, autonomy/impaired performance, other-directedness, over-vigilance/inhibition and impaired limits. If the total scores for any of these domains exceed 25, it indicates the presence of a maladaptive schema in that area [36]. Multiple studies have provided evidence for the YSQ-SF’s favorable validity and reliability [37 ,38].
In Khosravani et al. research, the Persian version of the instrument employed in this study exhibited strong reliability (Cronbach’s α=0.75-0.91) and confirmed criterion, predictive and discriminant validity [39]. The questionnaire demonstrated excellent internal consistency in the current study, with coefficient omega values of 0.95 for the overall questionnaire, 0.89 for disconnection/rejection, 0.89 for impaired autonomy/performance, 0.80 for other-directedness, 0.81 for over-vigilance/inhibition and 0.82 for impaired limits.
Statistical analysis
In the statistical analysis, descriptive measures (Mean±SD for continuous variables and frequencies and percentages for categorical variables) were used to describe demographic characteristics. A univariate logistic regression approach was utilized to investigate potential predictors (independent variables) associated with chronic pain, including age, gender, birth order, parental career and education and maladaptive schemas.
Variables with significance levels <0.2 or showing a notable association with chronic pain in univariate analyses were selected for hierarchical multiple regression analyses (method: Enter). Demographic characteristics were initially examined for their relationship with chronic pain. Subsequently, parental chronic pain was introduced into the regression model, considering its known impact on pediatric chronic pain [40]. Finally, maladaptive schemas were added to assess their contribution to explaining the variance in chronic pain, controlling for previously entered variables. Adjusted odds ratios and 95% confidence intervals (CI) were calculated and reported. SPSS software, version 22 was used for all statistical analyses, with a predetermined significance level of <0.05.
Results
Sample characteristics
Among the 1333 adolescents invited to participate, 1302 took part in the study, resulting in an impressive response rate of 97.67%. The participants’ Mean±SD age was 16.87±1.94, ranging from 12 to 21 years. Most participants were male (53.70%), and approximately 53.80% were the eldest child in their family. Regarding education, most fathers (62.80%) and mothers (70.70%) had completed a diploma or had a lower education level. Regarding employment, most fathers (80.40%) were employed, while most mothers (80.10%) were housewives. A detailed breakdown of the participants’ demographic characteristics can be found in Table 1.
Characteristics of chronic pain
The pain attributes of the adolescent participants are presented in Table 2.
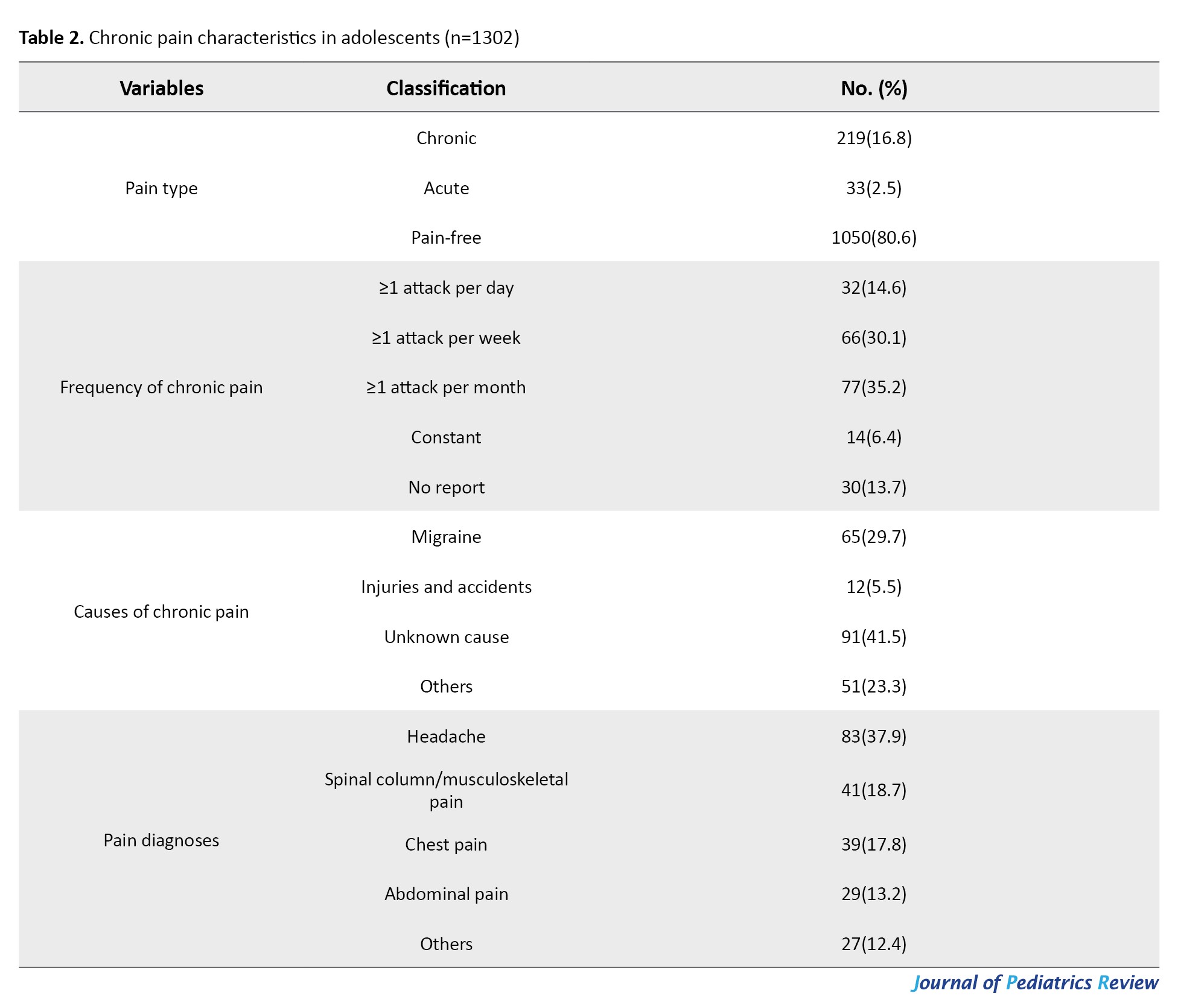
Out of all the participants, 219 adolescents (16.8%) met the ICD-11 criteria for chronic pain. The average pain intensity reported by these individuals over the preceding two weeks was recorded at 4.74±2.48. Among those experiencing chronic pain, the majority (35.2%) reported having pain attacks at least once a month. The most prevalent types of chronic pain reported by adolescents were headaches (37.90%) and musculoskeletal pain related to the spinal column (18.70%).
Univariate logistic regression models
In the analysis using univariate logistic regression with no-chronic pain as the reference group, several factors were examined to assess their correlation with chronic pain. These factors included age, gender, birth order, father’s career, father’s educational status, mother’s career, mother’s educational status, and father’s chronic pain, as well as other-directedness and impaired limits (Table 3).
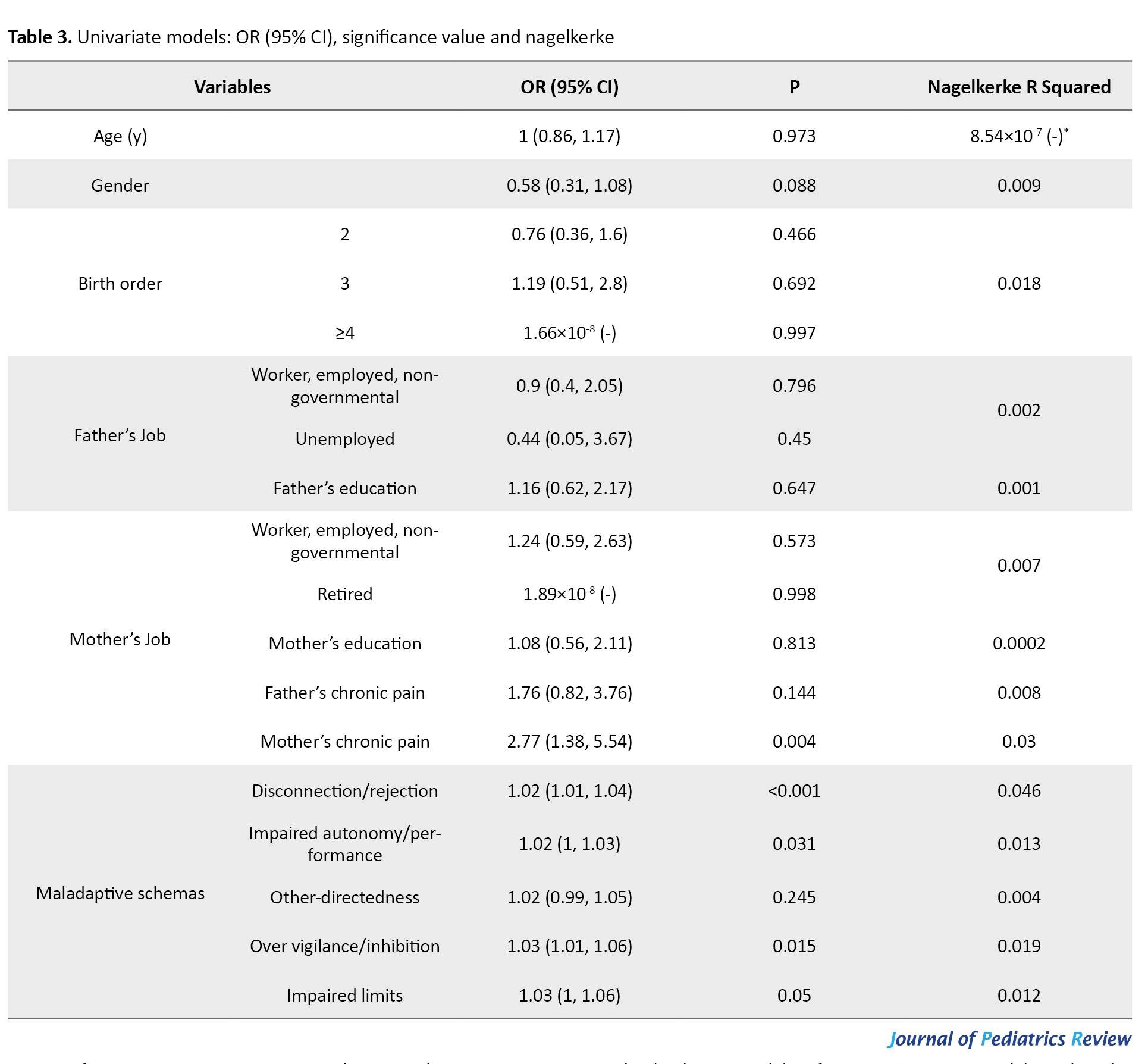
As single predictors, none of these variables showed a significant correlation with chronic pain.
However, three variables demonstrated significant associations with chronic pain. These were the mother’s chronic pain, which explained 3% of the variance, impaired autonomy and performance, which explained 1.3% of the variance, and over-vigilance and inhibition, which explained 1.9% of the variance. Additionally, the “disconnection/rejection” domain exhibited a significant association with chronic pain and displayed the best model fit, explaining 4.6% of the variance (Table 3).
Multiple regression analyses
Table 4 displays the hierarchical logistic regression analysis outcomes, which examined the contributions of variable blocks entered simultaneously in predicting chronic pain.
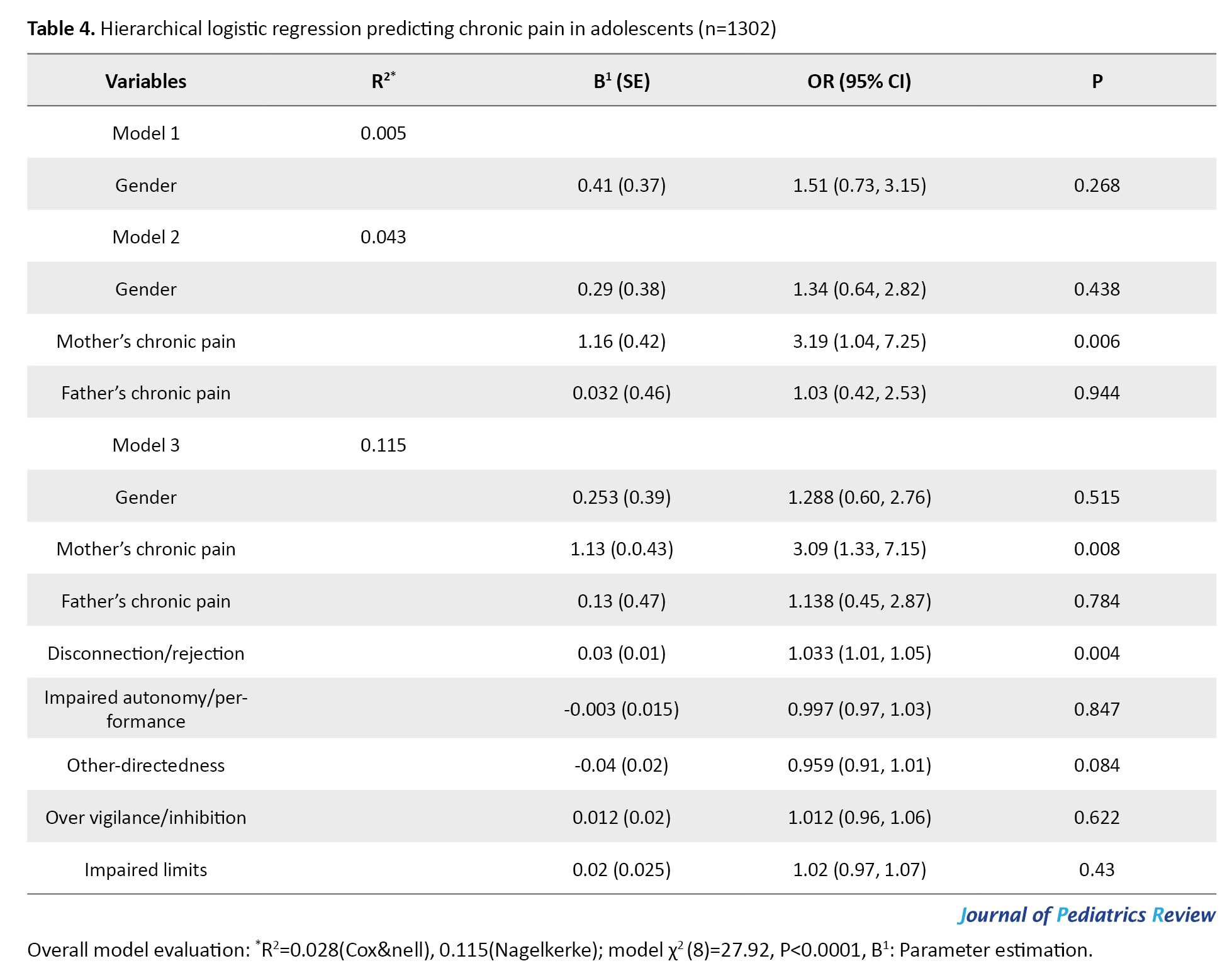
The first step of the hierarchical regression assessed the significance of gender (P<0.2) in the univariate model, revealing that gender did not significantly contribute to chronic pain. In the second step, the model included gender, a mother’s chronic pain and a father’s chronic pain. While the mother’s chronic pain emerged as a significant predictor (b=1.16, P=0.006) in this model, the father’s chronic pain and gender did not show significant associations. This model explained 3.8% of the variance [∆R2=0.043-0.005] compared to the previous model (R2=0.5%). Lastly, the model incorporated schemas. The “disconnection/rejection” domain (OR=0.997, P=0.004) was found to contribute to the prediction of chronic pain. Additionally, a mother’s chronic pain (OR=0.878, P=0.008) continued to be a predictive factor in this model. Including schemas led to a substantial 7.2% [∆R2=0.115-0.043] enhancement in the explained variance, resulting in a total explained variance of 11.5%.
Discussion
This research is directed at exploring the predictive role of various maladaptive schema domains in the development of chronic pain in adolescents. Based on the study outcomes, it was found that chronic pain in mothers can predict chronic pain in adolescents. Additionally, the disconnection/rejection domain was identified as a predictor of chronic pain in adolescents.
Furthermore, the outcomes of this study showed a noticeable conjunction between chronic pain in adolescents and chronic pain in their mothers. According to research findings, the diminished overall health (both mental and physical) of parents was indirectly linked to increased interference with child pain. This connection was mediated first by heightened parent pain catastrophizing, followed by an escalation in both parent protective behaviors and child pain catastrophizing [41]. Children of mothers with chronic pain are at a higher risk of experiencing chronic pain and related harmful mental and somatic health consequences [40, 42]. Stone and Wilson proposed five potential mechanisms in their model for the relationship between chronic pain in parents and chronic pain in children, along with related destructive issues: 1) Genetics, 2) Changes in early neural development, 3) Social learning of pain-specified behaviors (catastrophizing their own or their child’s pain), 4) General parenting and family health, and 5) Exposure to demanding surroundings. Moreover, the model includes three potential mediators: 1) The existence of chronic pain in the other parent, 2) the timing, duration, and location of the parents’ chronic pain, and 3) the features of the children (gender, stage of development, race or ethnicity, and temperament). All of these factors likely impact the expansion of chronic pain and its connected consequences for children of parents with chronic pain. Specifically, chronic pain in mothers may affect the neural development of their children through stress and health behaviors during pre- and perinatal periods [40].
Another finding of this study indicates that, among various factors, the domain of disconnection or rejection can predict chronic pain in adolescents. This finding aligns with Heshmati’s study, which reported the predictive role of the disconnection/rejection domain in chronic pain among university students [27].
Individuals with the disconnection/rejection domain struggle to form secure and satisfying emotional attachments. As a result, they experience various emotions, such as abandonment, distrust, neglect, shame, guilt, and alienation. This cognitive pattern is likely to develop in families characterized by emotional coldness, distance, isolation, unpredictability, and a lack of trust [12]. Among the psychosocial factors that are effective and influential in chronic pain based on the bio-psycho-social model [6], inefficient family system behaviors have been noted [43]. Specific parental characteristics, such as emotional neglect that leads to unmet adolescent needs and the formation of this maladaptive schema domain, are associated with chronic pain [10, 11, 44-47]. The various negative emotions experienced by adolescents in such families, manifesting through this maladaptive schema domain, can all threaten mental health [17, 21–23, 48]. Additionally, Vakili et al. demonstrated in their study that the disconnection/rejection domain mediates chronic pain through depression in chronic pain patients [28]. Furthermore, given the overlap between chronic pain and poor mental health, it has been established that factors, such as decreased quality of life, negative emotions, depression, stress, etc. can lead to chronic pain [49–54].
Moreover, according to Brown’s perspective, maladaptive schemas impact how a person perceives and pays attention to various stimuli, potentially leading to misunderstandings of senses and physical cues [55]. Also, Riebel et al. demonstrated that individuals with somatoform disorders hold self-views of vulnerability and an incapacity to cope with tension [56]. Hence, maladaptive schemas are involved in either initiating or perpetuating pain by misunderstanding physical senses and engaging in catastrophic thinking about physical symptoms.
Another noteworthy point is that individuals with maladaptive schemas are less inclined to seek help to reduce their pain. They believe that no one can assist them, which may lead them to express physical grievances and psychosomatic disorders as a means of attracting attention and care from others, as mentioned by Yang et al. [50]. However, this function is often beyond their conscious awareness, and the secondary gain can positively reinforce and perpetuate pain in these individuals. In other words, individuals with a domain of rejection or abandonment may have an unconscious inclination to experience pain [27]. From another perspective, individuals with such schemas tend to avoid expressing their emotions, thereby describing their physiological aspects, including pain, in physical terms due to limited emotional awareness and verbal ability [28].
To sum up, the current results reveal that the domain of rejection and abandonment holds predictive value for chronic pain in adolescents. This investigation provides a novel perspective on the contributing factors to chronic pain in this age group, elucidating the connection between maladaptive schemas and prevalent physical issues, like chronic pain. As a result, these findings can have implications for schema therapy interventions for patients with chronic pain. By incorporating cognitive, behavioral, and relational approaches, the outcomes of this study can facilitate the modification of maladaptive schemas, ultimately leading to pain reduction in individuals suffering from chronic pain. Furthermore, these discoveries potentially benefit both families and school teachers, as they play pivotal roles in shaping the cognitive schemas of children and adolescents. In this context, fostering close and affectionate relationships with children, providing appropriate emotional support, and setting reasonable and rational expectations can be crucial in minimizing the risk of developing or exacerbating pain in adolescents. Encouraging positive parental behaviors that foster constructive and enriching experiences during childhood and adolescence, while meeting their needs and consequently fostering adaptive schemas [57, 58] can help reduce the likelihood of maladaptive schemas, particularly in the domain of rejection/abandonment [59, 60]. This approach can contribute to building trust, independence, self-esteem, a sense of worth, and an enhanced capacity to form secure relationships in adolescents. All these factors play vital roles in improving their physical and psychological well-being, and a lack of them can lead to physical health disadvantages [61–63]. The results of this study can also offer valuable insights for family therapy, group therapy, and educational programs focused on appropriate interactions with adolescents dealing with chronic pain. Conversely, by implementing policies promoting healthier lifestyles and enhancing overall community well-being, we can anticipate a reduction in chronic pain among families, encompassing both parents and children.
The present study has some restrictions that should be acknowledged. Firstly, chronic pain assessment relied on self-report questionnaires rather than clinical examinations, potentially introducing some degree of response bias to the measured variables [64]. However, it is crucial to consider McCaffrey’s perspective, which argues that pain is subjective and persists for as long as the individual perceives it [65]. Secondly, the study’s cross-sectional design deters us from the foundation of spontaneous relations based on the current findings. To gain a deeper understanding of how adolescents’ psychological characteristics contribute to chronic pain, further prospective longitudinal studies are necessary. Moreover, since the questionnaires were completed online, there is uncertainty regarding whether all adolescents completed them. Additionally, there are other factors not investigated in this study that play a role in influencing chronic pain among adolescents. Therefore, it is strongly advised to conduct further research to explore additional psychosocial variables not considered in this study. Furthermore, replicating this study with diverse samples encompassing various age groups and cultural backgrounds would be advantageous for assessing the generalizability of the findings.
Conclusion
Considering the growing prevalence of chronic pain among adolescents lately, it becomes crucial to recognize the elements that contribute to this issue. One such factor is cognitive schemas in adolescents, although prior research has primarily focused on their impact on psychological well-being rather than chronic pain. Consequently, this study sought to investigate the following question: “Can maladaptive schemas predict the development of chronic pain in adolescents?” The findings of this study indicated that chronic pain in mothers, along with maladaptive schemas related to rumination and avoidance in adolescents, could influence the occurrence of chronic pain in this age group. Interventions aimed at preventing or modifying maladaptive schemas in adolescents could play a pivotal role in effectively managing chronic pain within this population. It is essential for parents and guardians to become familiar with maladaptive schemas, recognize the significance of employing effective communication strategies and acquire the necessary knowledge and skills to address the psychological needs of adolescents. Building upon the insights from this study, implementing cognitive-behavioral educational programs targeted at modifying or reducing maladaptive schemas for parents, guardians, and adolescents could prove instrumental in diminishing the likelihood of developing or exacerbating chronic pain among adolescents.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shiraz University of Medical Sciences (Code: IR.SUMS.REC.1399.1033). Eligible participants were informed about the research’s purpose and were emphasized that their involvement was entirely voluntary. An electronic informed consent form was completed by all the adolescents. Data collection was conducted anonymously, without any reference to individuals’ names.
Funding
This research was financially supported by Shiraz University of Medical Sciences (Grant No.: 22110).
Authors contributions
Conceptualization: Maryam Shaygan and Giti Setoodeh; Study design: Parvin Ghaemmaghami; Investigation: Saghar Salari; Writing the original draft: Saghar Salari and Maryam Shaygan; Review, editing and final approval: All authors.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank all adolescents who participated in this study.
References
- Huckerby L, McDonagh JE, Lee RR. Growing up with chronic pain: A systematic review of the evidence in transitional care for young people with chronic pain. Rheumatol Adv Pract. 2023; 7(Supplement_1):i19-25. [DOI:10.1093/rap/rkad006]
- Miró J, Roman-Juan J, Sánchez-Rodríguez E, Solé E, Castarlenas E, Jensen MP. Chronic pain and high impact chronic pain in children and adolescents: A cross-sectional study. J Pain. 2023; 24(5):812-23. [DOI:10.1016/j.jpain.2022.12.007]
- Farrant B, Denny S, Vroegop P, Fenaughty J, Clark TC. Prevalence, severity and impact of chronic pain among a representative cross-sectional study of New Zealand high school students. J Paediatr Child Health. 2023; 59(1):144-52. [DOI:10.1111/jpc.16263]
- Wakefield EO, Zempsky WT, Puhl RM, Litt MD. Conceptualizing pain-related stigma in adolescent chronic pain: A literature review and preliminary focus group findings. Pain Rep. 2018; 3(Suppl 1):e679. [DOI:10.1097/PR9.0000000000000679]
- Zandi Goharrizi G, Ghorban Jahromi R, Robatmili S, Zare Bahramabadi M. [Causal model of pain intensity based on attachment styles mediated by early maladaptive schemas in patients with chronic pain (Persian)]. Psychol Achiev. 2023; 30(1):315-32. [DOI:10.22055/psy.2022.40920.2856]
- Gatchel RJ. The biopsychosocial model of chronic pain. London: Future Medicine Ltd; 2013. [DOI:10.2217/ebo.13.469]
- Groenewald CB, Murray CB, Palermo TM. Adverse childhood experiences and chronic pain among children and adolescents in the United States. Pain Rep. 2020; 5(5):e839. [DOI:10.1097/PR9.0000000000000839]
- You DS, Albu S, Lisenbardt H, Meagher MW. Cumulative childhood adversity as a risk factor for common chronic pain conditions in young adults. Pain Med. 2019; 20(3):486-94. [DOI:10.1093/pm/pny106]
- Nelson CA, Bhutta ZA, Harris NB, Danese A, Samara M. Adversity in childhood is linked to mental and physical health throughout life. BMJ. 2020; 371:m3048. [DOI:10.1136/bmj.m3048]
- Kascakova N, Furstova J, Hasto J, Madarasova Geckova A, Tavel P. The unholy trinity: Childhood trauma, adulthood anxiety, and long-term pain. Int J Environ Res Public Health. 2020; 17(2):414. [DOI:10.3390/ijerph17020414]
- Pilkington PD, Bishop A, Younan R. Adverse childhood experiences and early maladaptive schemas in adulthood: A systematic review and meta-analysis. Clin Psychol Psychother. 2021; 28(3):569-84. [DOI:10.1002/cpp.2533]
- Young JE, Klosko JS, Weishaar ME. Schema therapy: A practitioner’s guide. New York: Guilford Publications; 2006. [Link]
- Nicol A, Mak AS, Murray K, Walker I, Buckmaster D. The relationships between early maladaptive schemas and youth mental health: A systematic review. Cogn Ther Res. 2020; 44(4):715-51. [DOI:10.1007/s10608-020-10092-6]
- Bach B, Lockwood G, Young JE. A new look at the schema therapy model: Organization and role of early maladaptive schemas. Cogn Behav Ther. 2018; 47(4):328-49. [DOI:10.1080/16506073.2017.1410566]
- Barazandeh H, Kissane DW, Saeedi N, Gordon M. A systematic review of the relationship between early maladaptive schemas and borderline personality disorder/traits. Pers Individ Diff. 2016; 94:130-9. [DOI:10.1016/j.paid.2016.01.021]
- Esmaeilian N, Dehghani M, Koster EH, Hoorelbeke K. Early maladaptive schemas and borderline personality disorder features in a nonclinical sample: A network analysis. Clin Psychol Psychother. 2019; 26(3):388-98. [DOI:10.1002/cpp.2360]
- Davoodi E, Wen A, Dobson KS, Noorbala AA, Mohammadi A, Farahmand Z. Early maladaptive schemas in depression and somatization disorder. J Affect Disord. 2018; 235:82-9. [DOI:10.1016/j.jad.2018.04.017]
- Koçak L. Investigation of the Relationship between Early Maladaptive Schemas and Academic Expectations Stress among High School Students. Türk Psikolojik Danışma ve Rehberlik Dergisi. 2020; 10(57):321-42. [Link]
- Yoosefi A, RajeziEsfahani S, Pourshahbaz A, Dolatshahee B, Assadi A, Maleki F, et al. Early maladaptive schemas in obsessive-compulsive disorder and anxiety disorders. Glob J Health Sci. 2016; 8(10):167. [DOI:10.5539/gjhs.v8n10p167]
- Taylor CDJ, Harper SF. Early maladaptive schema, social functioning and distress in psychosis: A preliminary investigation. Clin Psychol. 2017; 21(2):135-42. [DOI:10.1111/cp.12082]
- Aloi M, Verrastro V, Rania M, Sacco R, Fernández-Aranda F, Jiménez-Murcia S, et al. The potential role of the early maladaptive schema in behavioral addictions among late adolescents and young adults. Front Psychol. 2019; 10:3022. [DOI:10.3389/fpsyg.2019.03022]
- Bishop A, Younan R, Low J, Pilkington PD. Early maladaptive schemas and depression in adulthood: A systematic review and meta-analysis. Clin Psychol Psychother. 2022; 29(1):111-30. [DOI:10.1002/cpp.2630]
- Tariq A, Reid C, Chan SW. A meta-analysis of the relationship between early maladaptive schemas and depression in adolescence and young adulthood. Psychol Med. 2021; 51(8):1233-48. [DOI:10.1017/S0033291721001458]
- Haleem DJ. Targeting Serotonin1A receptors for treating chronic pain and depression. Curr Neuropharmacol. 2019; 17(12):1098-108. [DOI:10.2174/1570159X17666190811161807]
- Boersma K, Södermark M, Hesser H, Flink IK, Gerdle B, Linton SJ. Efficacy of a transdiagnostic emotion-focused exposure treatment for chronic pain patients with comorbid anxiety and depression: A randomized controlled trial. Pain. 2019; 160(8):1708. [DOI:10.1097/j.pain.0000000000001575]
- Meda RT, Nuguru SP, Rachakonda S, Sripathi S, Khan MI, Patel N. Chronic pain-induced depression: A review of prevalence and management. Cureus. 2022; 14(8):e28416. [DOI:10.7759/cureus.28416]
- Heshmati R. [Predicting incidence of chronic pain based on early maladaptive schema (Persian)]. Anesthesiol Pain. 2016; 7(1):49-60. [Link]
- Vakili N, Rezaei F, Hosseini N. The mediating role of depression between early maladaptive schema and pain: A structural equation modelling. Research Square. 2022 [Unpublished]. [DOI:10.21203/rs.3.rs-120596/v1]
- Heshmati R, Zamanizad N, Setayeshi M. [Structural equation modeling of chronic pain determinants: The role of early maladaptive schema and dispositional mindfulness (Persian)]. J Anesthesiol Pain. 2017; 7(4):34-44. [Link]
- Abbasi M, Saberi H, Taheri A. Developing a structural model of pain perception based on early maladaptive schemata mediated by cognitive emotion regulation in people with chronic pain. Iran Evol Educ Psychol. 2023; 5(1):101-17. [DOI:10.52547/ieepj.5.1.101]
- Hardin AP, Hackell JM, Simon GR, Boudreau ADA, Baker CN, Barden GA, et al. Age limit of pediatrics. Pediatrics. 2017; 140(3):e20172151. [DOI:10.1542/peds.2017-2151]
- Saariaho AS, Saariaho TH, Mattila AK, Karukivi M, Joukamaa MI. Alexithymia and early maladaptive schemas in chronic pain patients. Scand J Psychol. 2015; 56(4):428-37. [DOI:10.1111/sjop.12226]
- Shaygan M, Karami Z. Chronic pain in adolescents: The predictive role of emotional intelligence, self-esteem and parenting style. Int J Commun Based Nurs Midwifery. 2020; 8(3):253-63. [DOI:10.30476/ijcbnm.2020.83153.1129] [PMID]
- Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. Chronic pain as a symptom or a disease: The IASP classification of chronic pain for the international classification of diseases (ICD-11). Pain. 2019; 160(1):19-27. [DOI:10.1097/j.pain.0000000000001384]
- Korwisi B, Treede RD, Rief W, Barke A. Evaluation of the international classification of diseases-11 chronic pain classification: study protocol for an ecological implementation field study in low, middle and high-income countries. Pain Rep. 2020; 5(4):e825. [DOI:10.1097/PR9.0000000000000825]
- Young JE, Brown G. Young Schema Questionnaire-Short Form; Version 3. Washington: APA PsycTests; 2005. [DOI:10.1037/t67023-000]
- Waller G, Meyer C, Ohanian V. Psychometric properties of the long and short versions of the young schema questionnaire: Core beliefs among bulimic and comparison women. Cogn Ther Res. 2001; 25(2):137-47. [DOI:10.1023/A:1026487018110]
- Welburn K, Coristine M, Dagg P, Pontefract A, Jordan S. The Schema Questionnaire-Short Form: Factor analysis and relationship between schemas and symptoms. Cogn Ther Res. 2002; 26(4):519-30. [DOI:10.1023/A:1016231902020]
- Khosravani V, Najafi M, Mohammadzadeh A. The young schema questionnaire-short form: A Persian version among a large sample of psychiatric patients. Int J Ment Health Addict. 2020; 18(4):949-67. [DOI:10.1007/s11469-018-9997-2]
- Stone AL, Wilson AC. Transmission of risk from parents with chronic pain to offspring: An integrative conceptual model. Pain. 2016; 157(12):2628-39. [DOI:10.1097/j.pain.0000000000000637]
- Birnie KA, Heathcote LC, Bhandari RP, Feinstein A, Yoon IA, Simons LE. Parent physical and mental health contributions to interpersonal fear avoidance processes in pediatric chronic pain. Pain. 2020; 161(6):1202-11. [DOI:10.1097/j.pain.0000000000001820]
- Higgins KS, Birnie KA, Chambers CT, Wilson AC, Caes L, Clark AJ, et al. Offspring of parents with chronic pain: A systematic review and meta-analysis of pain, health, psychological, and family outcomes. Pain. 2015; 156(11):2256-66. [DOI:10.1097/j.pain.0000000000000293]
- Wiwe Lipsker C. Children and adolescents with chronic pain: parental factors, functioning, and neurodevelopmental comorbidity [doctoral dissertation]. Stockholm: Karolinska Institutet; 2019. [Link]
- Haugh JA, Miceli M, DeLorme J. Maladaptive parenting, temperament, early maladaptive schemas, and depression: A moderated mediation analysis. J Psychopatho Behav Assess. 2017; 39(1):103-16. [DOI:10.1007/s10862-016-9559-5]
- Macedo BBD, von Werne Baes C, Menezes IC, Juruena MF. Child abuse and neglect as risk factors for comorbidity between depression and chronic pain in adulthood. J Nerv Ment Dis. 2019; 207(7):538-45. [DOI:10.1097/NMD.0000000000001031]
- Nelson S, Simons LE, Logan D. The incidence of adverse childhood experiences (ACEs) and their association with pain-related and psychosocial impairment in youth with chronic pain. Clin J Pain. 2018; 34(5):402-8. [DOI:10.1097/AJP.0000000000000549]
- Sójta K, Strzelecki D. Early maladaptive schemas and their impact on parenting: Do dysfunctional schemas pass generationally? A systematic review. J Clin Med. 2023; 12(4):1263. [DOI:10.3390/jcm12041263]
- Ke T, Barlas J. Thinking about feeling: Using trait emotional intelligence in understanding the associations between early maladaptive schemas and coping styles. Psychol Psychother. 2020; 93(1):1-20. [DOI:10.1111/papt.12202]
- Niknejad B, Bolier R, Henderson CR, Delgado D, Kozlov E, Löckenhoff CE, et al. Association between psychological interventions and chronic pain outcomes in older adults: A systematic review and meta-analysis. JAMA Intern Med. 2018; 178(6):830-9. [DOI:10.1001/jamainternmed.2018.0756]
- Yang G, Cao J, Li Y, Cheng P, Liu B, Hao Z, et al. Association between internet addiction and the risk of musculoskeletal pain in Chinese college freshmen-A cross-sectional study. Front Psychol. 2019; 10:1959. [DOI:10.3389/fpsyg.2019.01959]
- Koechlin H, Coakley R, Schechter N, Werner C, Kossowsky J. The role of emotion regulation in chronic pain: A systematic literature review. J Psychosom Res. 2018; 107:38-45. [DOI:10.1016/j.jpsychores.2018.02.002]
- Timmers I, Quaedflieg CW, Hsu C, Heathcote LC, Rovnaghi CR, Simons LE. The interaction between stress and chronic pain through the lens of threat learning. Neurosci Biobehav Rev. 2019; 107:641-55. [DOI:10.1016/j.neubiorev.2019.10.007]
- Goesling J, Lin LA, Clauw DJ. Psychiatry and pain management: at the intersection of chronic pain and mental health. Current psychiatry reports. 2018; 20:12. [DOI:10.1007/s11920-018-0872-4]
- Zelaya CE, Dahlhamer JM, Lucas JW, Connor EM. Chronic pain and high-impact chronic pain among US adults, 2019. 2020; 390:1-8. [Link]Brown RJ. Psychological mechanisms of medically unexplained symptoms: An integrative conceptual model. Psychol Bull. 2004; 130(5):793. [DOI:10.1037/0033-2909.130.5.793]
- Riebel K, Egloff B, Witthöft M. The implicit health-related self-concept in somatoform disorders. J Behav Therapy Exp Psychiatry. 2013; 44(3):335-42. [DOI:10.1016/j.jbtep.2013.02.001]
- Louis JP, Davidson AT, Lockwood G, Wood A. Positive perceptions of parenting and their links to theorized core emotional needs. J Child Fam Stud. 2020; 29:3342-56. [DOI:10.1007/s10826-020-01807-0]
- Louis JP, Wood AM, Lockwood G. Development and validation of the positive parenting schema inventory (PPSI) to complement the young parenting inventory (YPI) for schema therapy (ST). Assessment. 2020; 27(4):766-86. [DOI:10.1177/1073191118798464]
- Esmali Kooraneh A, Amirsardari L. Predicting early maladaptive schemas using baumrind’s parenting styles. Iran J Psychiatry Behav Sci. 2015; 9(2):e952. [DOI:10.17795/ijpbs952]
- Shid Anbarani B, Gol A, Farhadian F, Namvar Tabatabaee S. [Predicting early maladaptive schemas based on childhood affective maltreatment and parenting styles (Persian)]. Rooyesh-e-Ravanshenasi. 2020; 8(11):85-94. [Link]
- Bethell C, Jones J, Gombojav N, Linkenbach J, Sege R. Positive childhood experiences and adult mental and relational health in a statewide sample: Associations across adverse childhood experiences levels. JAMA Pediatr. 2019; 173(11):e193007. [DOI:10.1001/jamapediatrics.2019.3007]
- Francis A, Pai MS, Badagabettu S. Psychological well-being and perceived parenting style among adolescents. Compr Child Adolesc Nurs. 2021; 44(2):134-43. [DOI:10.1080/24694193.2020.1743796]
- Pierce M, Hope HF, Kolade A, Gellatly J, Osam CS, Perchard R, et al. Effects of parental mental illness on children's physical health: Systematic review and meta-analysis. Br J Psychiatry. 2020; 217(1):354-63. [DOI:10.1192/bjp.2019.216]
- Zabeti A, Jafari S. [Structural model of parenting styles, early maladaptive schemas and narcissistic personality traits in adolescents (Persian)]. J Appl Psychol. 2018; 12(2):285-302. [Link]
- McCaffery M. Nursing practice theories related to cognition. bodily pain, and man-environment interactions; Los Angeles: UCLA Students' Store; 1968. [Link]
Type of Study: Original Article |
Subject:
Pediatric Psychology
Received: 2023/10/25 | Accepted: 2024/07/31 | Published: 2024/07/1
Received: 2023/10/25 | Accepted: 2024/07/31 | Published: 2024/07/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









