Volume 12, Issue 3 (7-2024)
J. Pediatr. Rev 2024, 12(3): 213-222 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Varvani Farahani P, OZTURK C. Insights Into Pediatric Nursing; an In-depth Examination of Problems and Challenges: A Systematic Review. J. Pediatr. Rev 2024; 12 (3) :213-222
URL: http://jpr.mazums.ac.ir/article-1-610-en.html
URL: http://jpr.mazums.ac.ir/article-1-610-en.html
1- Department of Nursing, Faculty of Health Science, Cyprus International University, Nicosia, Cyprus. , 20222948@std.neu.edu.tr
2- Department of Pediatric Nursing, Faculty of Nursing, Near East University, Mersin, Türkiye.
2- Department of Pediatric Nursing, Faculty of Nursing, Near East University, Mersin, Türkiye.
Full-Text [PDF 517 kb]
(2139 Downloads)
| Abstract (HTML) (4225 Views)
Questions and research objectives
RQ1: Research questions: What are the main problems faced by pediatric nurses in Iran’s healthcare system?; RQ2: What challenges do pediatric nurses encounter in their daily practice, and how do these challenges impact their professional experience and patient care?
The objective of this systematic review was to provide a comprehensive understanding of the issues and difficulties encountered by pediatric nurses in Iran. By systematically evaluating the existing literature, this review aimed to: Identify the key problems and challenges faced by pediatric nurses in the Iranian healthcare system. Assess how these issues impact the quality of patient care and the professional well-being of pediatric nurses. Explore potential areas for improvement within the healthcare system and identify opportunities for enhancing support and training for pediatric nurses. Develop evidence-based recommendations to guide healthcare policymakers and administrators in addressing these challenges effectively.
Search technique
This is a systematic review aimed at investigating published clinical trials, observational, quasi-experimental, and qualitative investigations from January 1, 2015 to May 3, 2023, across nine scientific research databases, including PubMed, ScienceDirect, Wiley Online, Scopus, SciELO, LILACS and Google Scholar, as well as several Persian databases, including Magiran and scientific information database (SID). The keywords used in English and Persian were TS=([“pediatric nursing”] AND [“challenges”] AND [“problems”] AND [“pediatric” OR “children”] AND [“Iran”]). The initial search yielded 965 articles, of which 909 were removed for not meeting the inclusion criteria, leaving 28 articles for analysis.
Inclusion criteria
Studies were considered admissible if they: 1) Were clinical trials, observational studies, quasi-experimental studies, and qualitative studies, 2) Involved pediatric nurses working in any healthcare setting in Iran, 3) Specifically addressed the challenges and problems faced by pediatric nurses in Iran, 4) Were published from 2015 to 2023, 5) were published in English and Persian and 6) Had a code of ethics.
These criteria were established to ensure that the studies included in the review are relevant, high-quality, and specific to the context of pediatric nursing in Iran. By focusing on recent publications and including studies with ethical considerations, the review aimed to provide a comprehensive and accurate assessment of the challenges faced by pediatric nurses.
Exclusion criteria
Exclusion criteria were: 1) Lack of access to full texts, 2) Individual case reports, systematic reviews and meta-analyses and 3) Unrelated objectives.
Quality assessment of the articles
A critical appraisal was performed according to the study design of the articles. The critical appraisal skills program (CASP) was used for analysis. The CASP is a 10-item questionnaire with three possible answers: “Yes,” “no” and “can’t tell.” If eight or more of the criteria on the checklist were met, the study was rated as “good” quality, if five to seven were met, it was rated as “fair” quality, and if fewer than five were met, it was scored as “poor” quality. To ensure consistency and reliability in the critical appraisal process, two independent reviewers conducted the assessments. Any discrepancies in their evaluations were resolved through consensus, guaranteeing a thorough and unbiased analysis. Data were extracted from all papers, which met the eligibility and inclusion criteria for the review.
Data extraction
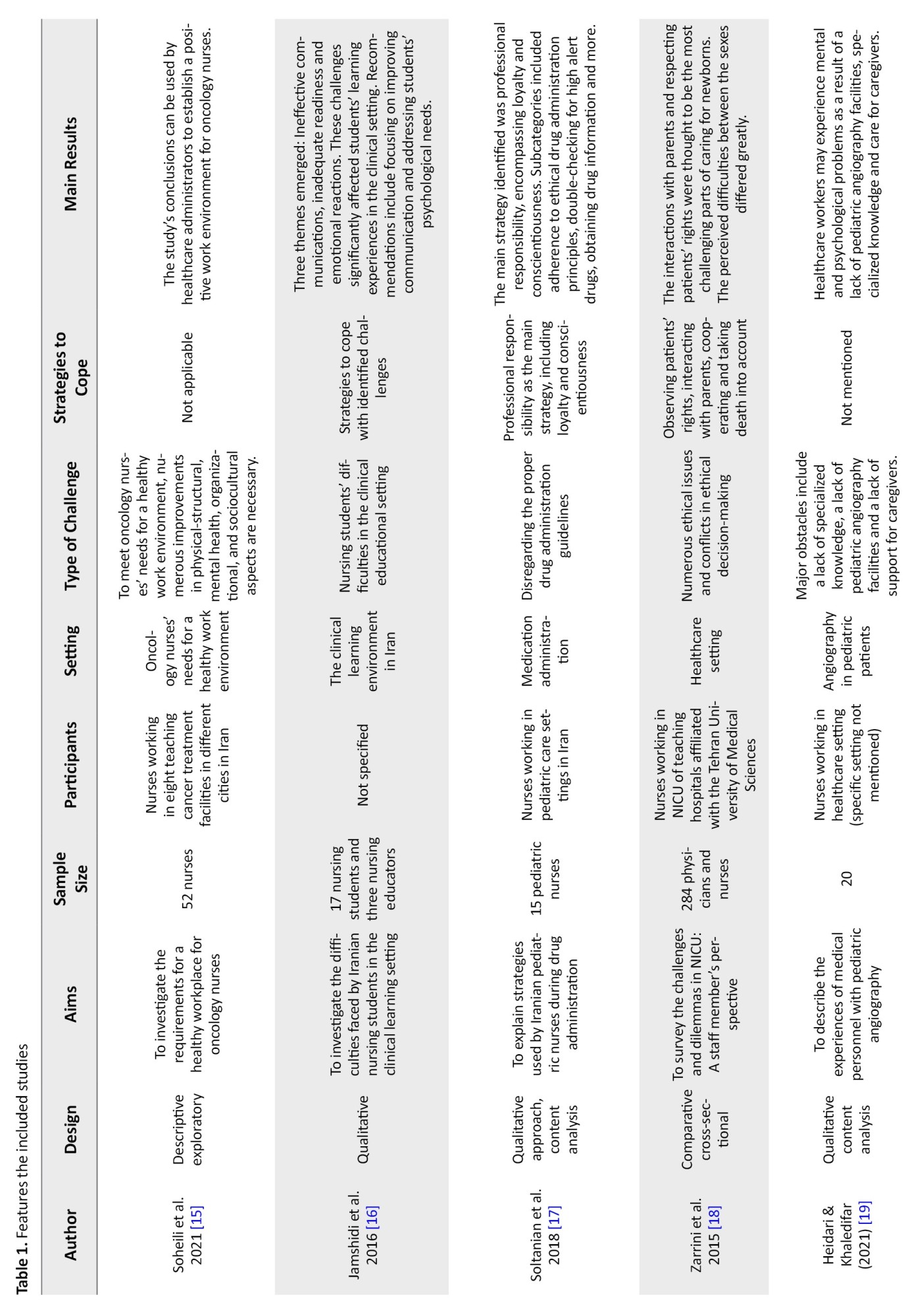
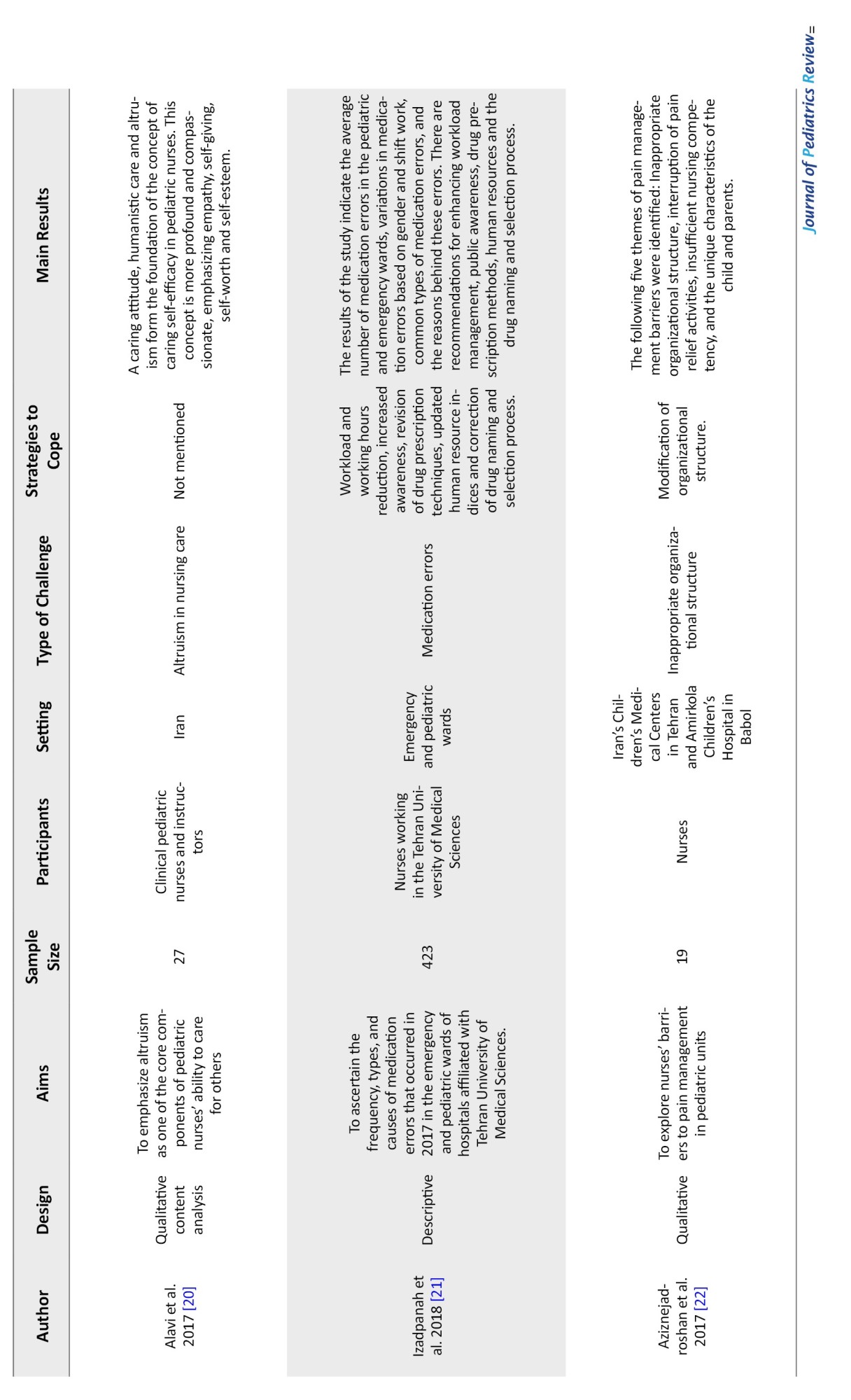
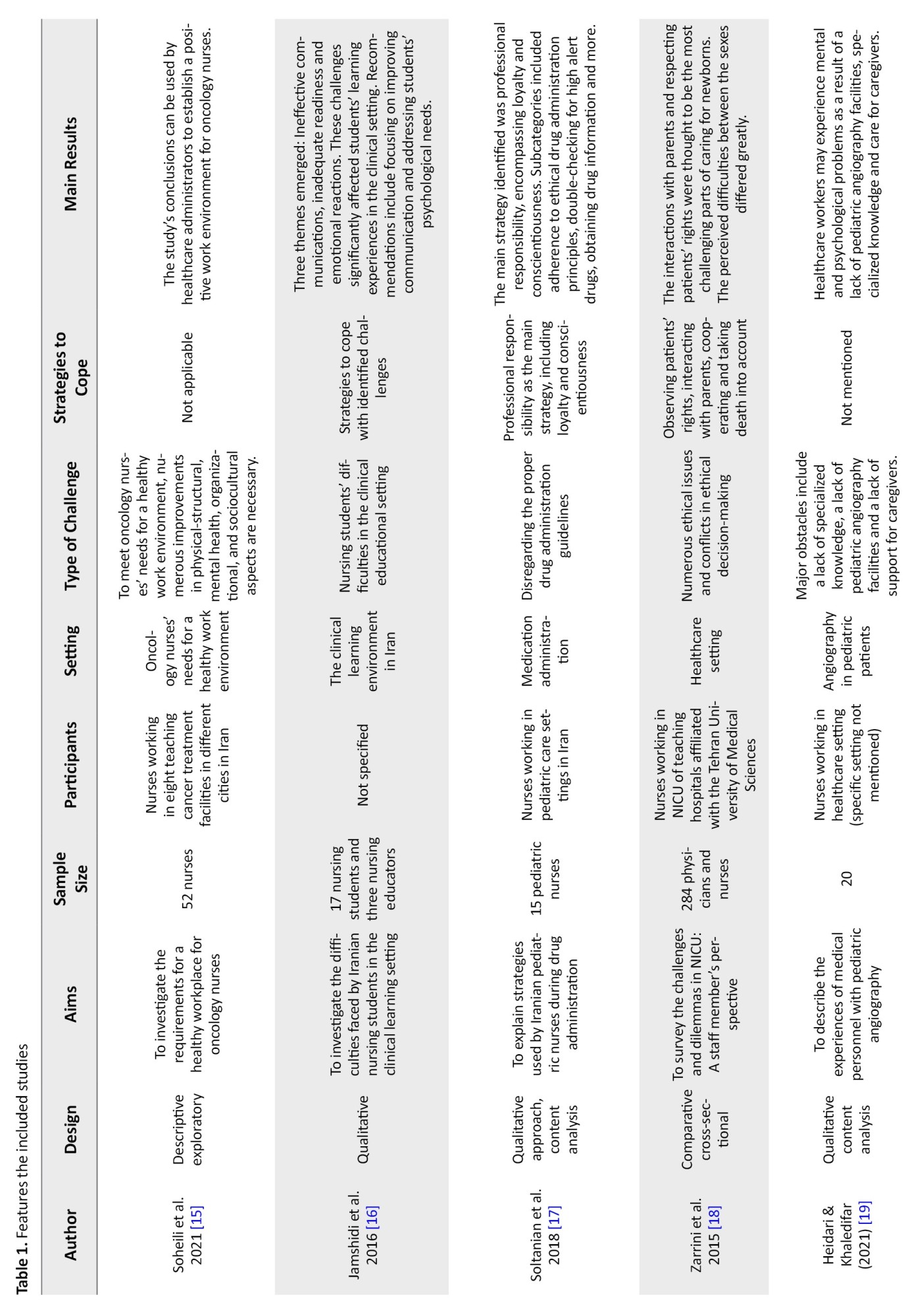
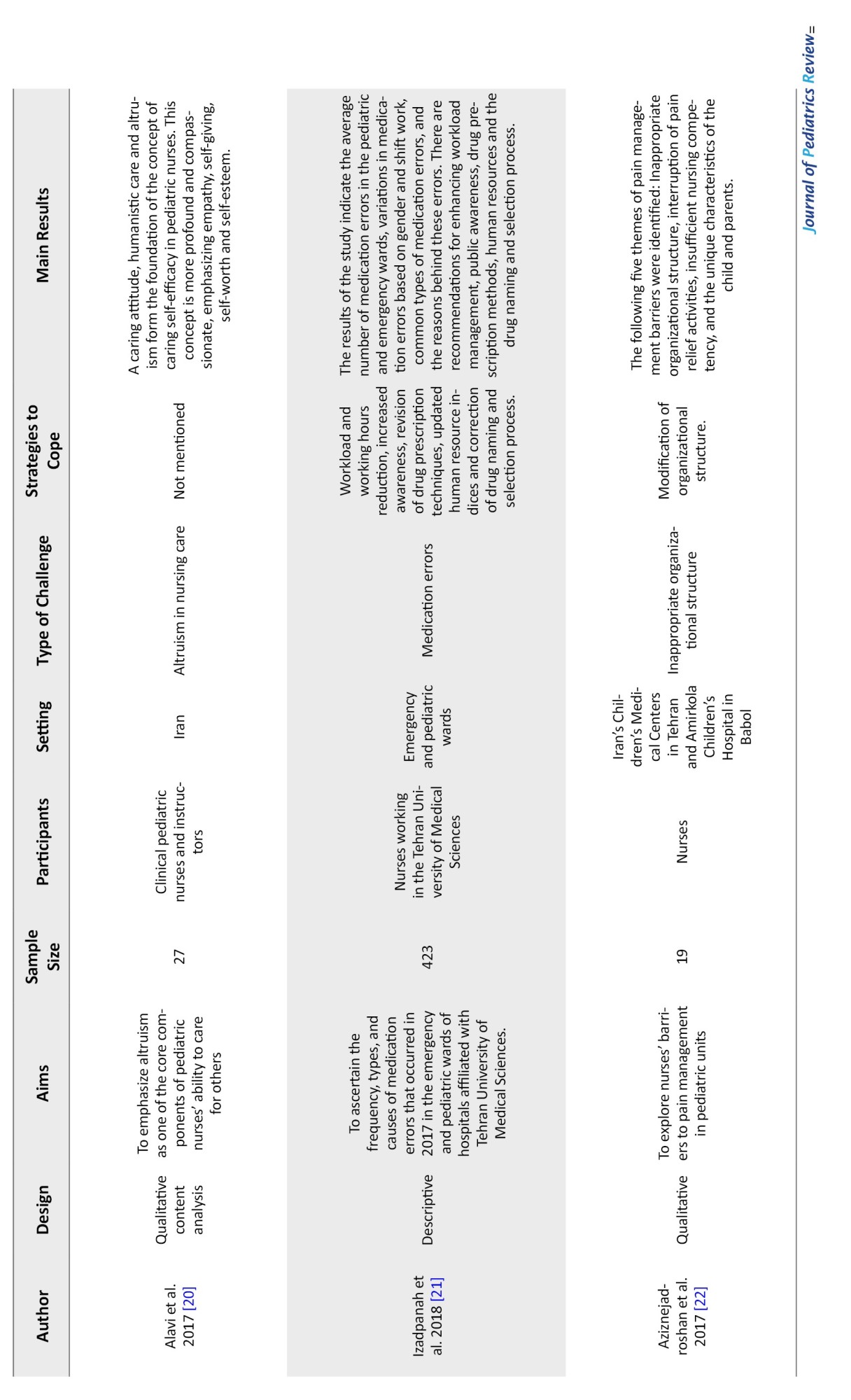
Two authors independently conducted the literature search, followed by the application of the inclusion and exclusion criteria, and screened the studies based on their titles and abstracts. Adhering to the PRISMA checklist ensured a rigorous and transparent review process. The screening process was carried out for duplicates using EndNote software, version X7 (clarivate analytics). After initial screening, the full texts of studies were obtained and examined to ensure eligibility for the development of the data extraction table. Data were extracted from the final set of included full texts, encompassing information, such as the first author, year of publication, study design, purpose, sample size, participant demographics, study setting, challenges and problems faced by pediatric nurses, duration of the studies, intervention used to the challenges and problems, and the reported outcomes associated with the challenges and problems faced by pediatric nurses in Iran (Table 1).
Results
Figure 1 outlines the outcomes of the search strategy. Initially, 965 articles were identified, with 25 duplicates removed, leaving 940 references. After applying initial inclusion criteria to titles, abstracts, and full texts in English and Persian, 31 articles were shortlisted. Upon further review of the full texts of these articles based on inclusion and exclusion criteria, three were excluded. Ultimately, 28 papers were included in the study. Data were systematically extracted from these papers (Table 1). Of the 28 studies, 18 were qualitative studies and one was a descriptive study. The reviews that comprised this study were carried out in various pediatric wards. The total sample sizes of the studies ranged from 15 to 423 subjects, with 17 studies using a sample size of 15–50 subjects and 5 using a sample size of 51–150 subjects. Six of the articles used samples that ranged in size from 151 to 423 people.
A thematic analysis approach was used to combine the study results in order to find recurring themes and patterns. Through this process, several key themes emerged across the studies, providing valuable insights into the subject matter. The identified themes encompassed various aspects of barriers and challenges in pediatric nursing care. These included problems, like a disregard for proper drug administration procedures, medication errors, cultural issues, moral conundrums, language barriers, and organizational limitations.
Some of the key findings
Requirements for a Healthy Workplace: To improve their well-being and deliver the best care possible to children with cancer, oncology nurses expressed the need for a supportive and healthy work environment. Workload, emotional demands and a lack of resources were all mentioned as barriers to a positive work environment [1, 23, 24]. Clinical learning environment challenges: One of the significant challenges faced by pediatric nurses is related to the education and supervision of nursing students during clinical rotations. Pediatric nurses often encounter difficulties, such as balancing patient care with the responsibility of guiding students, ensuring proper supervision and providing meaningful hands-on opportunities for student learning. The presence of students can sometimes increase the workload for nurses, as they must ensure that students are accurately applying theoretical knowledge in a real-world setting. These challenges not only affect the professional development of nursing students but also place additional strain on pediatric nurses, who must manage both educational and clinical responsibilities simultaneously [16, 25, 26].
Problems with specialized units and moral judgment: Staff members working in the neonatal intensive care units (NICU) frequently encountered communication issues, emotional stress, and moral conundrums. These difficulties emphasized the requirement for comforting measures and moral frameworks for making decisions in NICU settings [4, 18, 27-29]. Experiences of healthcare staff in angiography: Technical challenges, emotional stress and the need for specialized training to handle the particular needs of pediatric patients undergoing angiography were all reported by medical staff as being related to angiography in pediatric patients [19]. Altruism and caring self-efficacyaltruism is a crucial component of pediatric nurses’ caring self-efficacy, as it enables them to prioritize their patients’ needs and provide compassionate care. It also positively impacts their sense of self-efficacy and professional fulfillment. Prioritizing the needs of patients and delivering compassionate care should be at the forefront of every nurse’s practice[20, 30, 31]. Medication errors in pediatric wards: Medication errors have been identified as a problem in pediatric wards, with a variety of frequencies, types, and causes. Heavy workload, lack of knowledge or training, distractions, and communication breakdowns were among the factors that contributed to medication errors [17, 21, 32-35]. Barriers to pain management and communication challenge: Effective pain management for pediatric patients was hindered by a lack of training, inadequate assessment tools, side effect anxiety, lack of knowledge, and communication difficulties with young or nonverbal patients [22, 36, 37]. These difficulties brought to light the complexity and multifaceted nature of pediatric patient care, which calls for specialized skills and highlights the need for organizational structure and educational program improvements.
Discussion
According to our knowledge, this systematic review is the first piece of research data to offer insightful information on the obstacles and difficulties pediatric nurses experience when providing care. The core themes that cover many facets of pediatric nursing care were found using the thematic analysis method used to synthesize the study’s data. The themes that were found provided insight into a number of important difficulties facing pediatric nurses. These challenges included failing to follow correct drug administration procedures, taking the wrong prescription, having cultural or moral disagreements, having trouble communicating and having organizational problems.
These findings highlight the complex nature of pediatric nursing and the multifaceted challenges that nurses encounter in their practice. The theme of transition and adaptation revealed that pediatric nurses transferred to adult COVID-19 wards faced challenges with patient management, medical knowledge and emotional strain. This underscores the need for additional support and resources to facilitate the transition of pediatric nurses to adult care settings. Our results largely support studies conducted by Darchen et al. [38], which demonstrated that during the first wave of the pandemic, the main challenges faced by pediatric nurses moving into adult COVID-19 wards were related to their working environments, safety, communication, and care for terminally ill patients.
The theme of a healthy work environment revealed that oncology nurses expressed the need for a supportive and healthy work environment to enhance their well-being and provide optimal care to pediatric oncology patients. Factors, such as workload, emotional demands, and lack of resources were identified as obstacles. Addressing these challenges requires attention to workload management, emotional support and resource allocation in pediatric oncology settings. Similarly, Kleis and Kellogg reported that the pressure to perform despite emotional strain and feelings of being unsupported can lead to secondary traumatic stress in pediatric nurses [39]. Ethical decision-making challenges and challenges in specialized units, particularly NICUs, were another prominent theme. Personnel working in NICUs encountered dilemmas related to communication and ethical considerations [40-42]. In contrast, a study conducted in South Korea examined the moral challenges pediatric nurses encounter when caring for hospitalized children at the bedside. Three themes emerged from the analysis: Difficulty expressing oneself in an authoritative setting, ethical numbness, and negative emotions toward caregivers in the family [43]. The findings emphasize the importance of supportive measures and ethical decision-making frameworks in NICU settings to enhance patient care and support healthcare professionals in navigating complex ethical situations. Medication errors in pediatric wards were identified as a concern, with various contributing factors. These factors include heavy workload, lack of knowledge or training, distractions, and communication breakdowns [44, 45]. Barriers to pain management and communication challenges were also highlighted. Nurses in pediatric units encountered obstacles in effectively managing pain, including inadequate assessment tools, fear of side effects, lack of knowledge or training, and difficulties in communicating with non-verbal or young patients.
Our findings are supported by research conducted by Wuni et al. [46], Alotaibi et al. [47], Kusi Amponsah et al. [48]. Improvements in pain assessment tools, education, and communication skills can help overcome these barriers and ensure effective pain management in pediatric care. The studies demonstrated various coping mechanisms and solutions that nurses employed in response to the identified difficulties. Individual resilience strategies, social support, improved managerial support, and the acquisition of specialized knowledge and skills are some of these tactics. Additionally, the importance of implementing changes within the healthcare system was emphasized, such as workload reduction, awareness-raising campaigns, reevaluating drug prescription methods, and establishing rules and policies. The use of specific inclusion criteria further restricted the already available body of evidence. The drawbacks of the review included the limited data that met our inclusion criteria and the high degree of heterogeneity among the included studies, which was caused by differences in the interventions and outcome metrics. Moreover, restricting the studies to those conducted in Iran may have led to the exclusion of otherwise pertinent papers, thereby limiting the international applicability of our findings.
Conclusion
This systematic study highlights the numerous obstacles faced by pediatric nurses in Iran, which include prescription mistakes, cultural quandaries, moral quandaries, language limitations and organizational limits. These findings highlight the importance of improving healthcare, education and organizational support to advance pediatric nursing practice. This study calls for further research to address these issues and enhance the quality of pediatric nursing care. The implications for nursing and health policy are clear: Proper training, cultural competency and supporting frameworks are necessary to empower pediatric nurses and, as a result, improve patient well-being.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Supervision: Candan Ozturk; Writing the original draft: Pouran Varvani Farahani; Study design, data collection, data analysis, review and editing: All authors.
Conflicts of interest
The authors declared no conflict of interest.
Full-Text: (1508 Views)
Introduction
Pediatric nursing is an essential part of healthcare services, especially in addressing the complex needs of children who are hospitalized [1]. Children in hospitals are especially vulnerable because they frequently need comprehensive care for a variety of physical, mental, emotional and developmental reasons [2]. In healthcare organizations, nurses are recognized as the key human resource because of their critical role in enhancing patient outcomes. Pediatric nurses are the first to provide this specialized care, but their roles come with numerous difficulties and stressors [3, 4].
Pediatric nurses often face challenges, such as performing distressing procedures on children, managing the anxiety and distress of parents and addressing physical and behavioral issues in pediatric patients [5, 6]. In addition, the difficulty of their work includes providing care for critically ill patients and dealing with staffing shortages [7]. Despite these difficulties, pediatric nurses are essential for delivering the high-quality care that hospitalized children need [8]. Their expertise can significantly impact patient outcomes, as they are trained to address the unique needs of children and their families. The health of pediatric patients continues to be a top priority for healthcare organizations, making it critical to acknowledge and support the important work performed by pediatric nurses [9].
Promoting community health is the main goal of the healthcare system, and nurses are essential to achieving this goal. Their professional role involves maximizing patient health, well-being, and overall quality of life [10]. To fulfill these responsibilities effectively, pediatric nurses require ongoing skill development, empowerment, and support [11, 12]. In light of the aforementioned challenges and stressors faced by pediatric nurses in Iran [13], it is evident that there is an urgent need to address these issues through targeted research and policy interventions.
Pediatric nursing is integral to the well-being of hospitalized children, as it involves providing specialized care tailored to their unique physical, emotional and developmental needs. However, the literature reveals a notable gap in understanding the distinct challenges encountered by pediatric nurses, particularly in Iran. While existing studies generally address broader nursing challenges, they often overlook the cultural, organizational, and resource-specific factors that uniquely impact pediatric nursing in this region. A comprehensive understanding of these challenges is crucial for developing targeted interventions that can support pediatric nurses and enhance patient care outcomes. This systematic review aimed to address this literature gap by systematically identifying and categorizing the challenges faced by pediatric nurses in Iran. By elucidating these challenges, the study seeks to foster the professional development of pediatric nurses and provide evidence-based recommendations to healthcare policymakers and administrators. Ultimately, this research aimed to improve the quality of pediatric care and optimize the working conditions for pediatric nurses in Iran, thereby advancing overall healthcare outcomes for children.
Methods
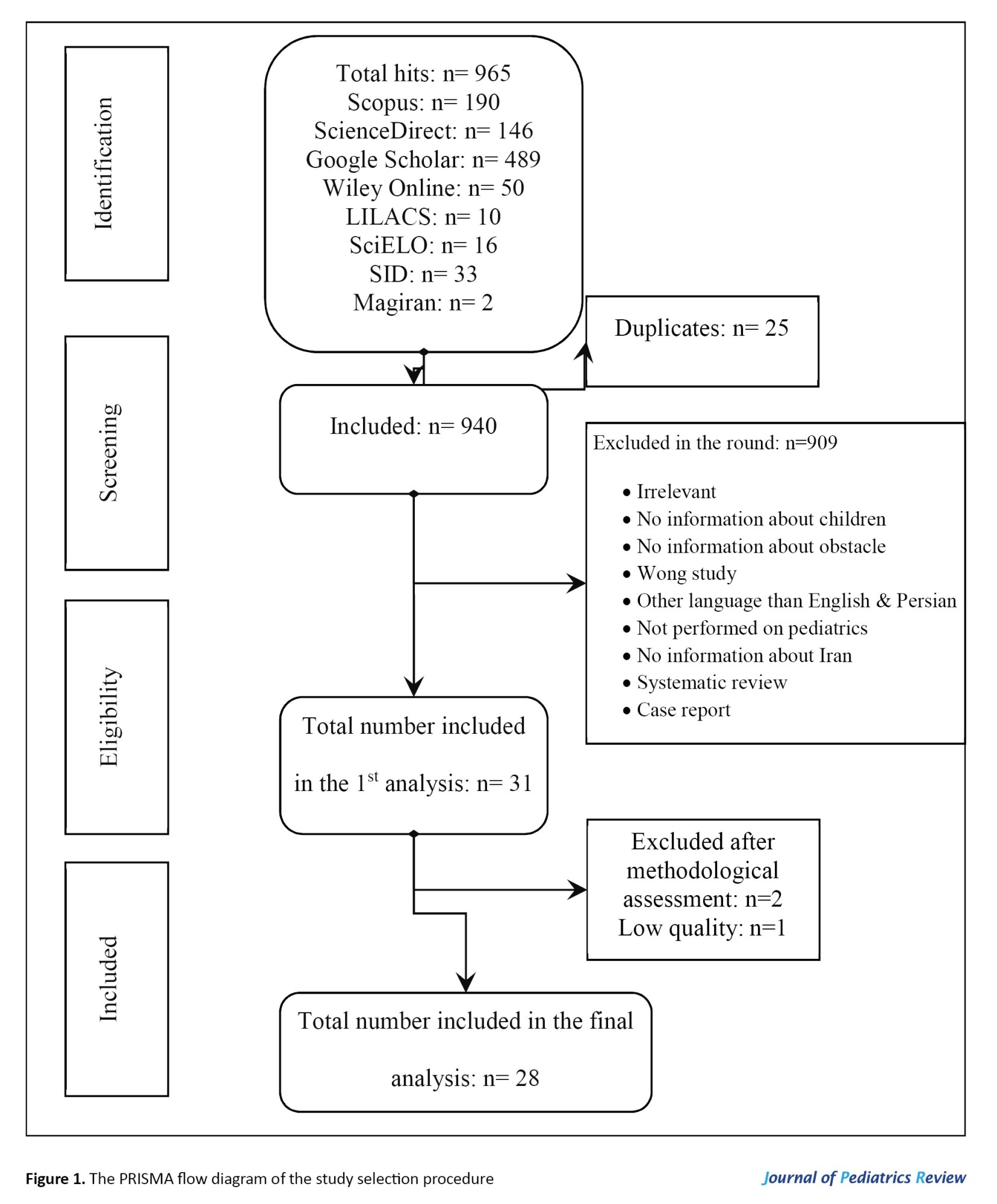
Given the rising volume of literature on the problems and challenges faced by Iranian pediatric nurses, it is essential to assess the cumulative advancements in the field and track the current level of knowledge in this area. We used the preferred reporting items for systematic reviews and meta-analyses (PRISMA) checklist to ensure that the reporting of the systematic review was of high quality [14]. The checklist, which includes four sequential processes (identification, screening, eligibility and inclusion) and 27 elements, is designed to help authors perform more effective systematic reviews (Figure 1).
Pediatric nursing is an essential part of healthcare services, especially in addressing the complex needs of children who are hospitalized [1]. Children in hospitals are especially vulnerable because they frequently need comprehensive care for a variety of physical, mental, emotional and developmental reasons [2]. In healthcare organizations, nurses are recognized as the key human resource because of their critical role in enhancing patient outcomes. Pediatric nurses are the first to provide this specialized care, but their roles come with numerous difficulties and stressors [3, 4].
Pediatric nurses often face challenges, such as performing distressing procedures on children, managing the anxiety and distress of parents and addressing physical and behavioral issues in pediatric patients [5, 6]. In addition, the difficulty of their work includes providing care for critically ill patients and dealing with staffing shortages [7]. Despite these difficulties, pediatric nurses are essential for delivering the high-quality care that hospitalized children need [8]. Their expertise can significantly impact patient outcomes, as they are trained to address the unique needs of children and their families. The health of pediatric patients continues to be a top priority for healthcare organizations, making it critical to acknowledge and support the important work performed by pediatric nurses [9].
Promoting community health is the main goal of the healthcare system, and nurses are essential to achieving this goal. Their professional role involves maximizing patient health, well-being, and overall quality of life [10]. To fulfill these responsibilities effectively, pediatric nurses require ongoing skill development, empowerment, and support [11, 12]. In light of the aforementioned challenges and stressors faced by pediatric nurses in Iran [13], it is evident that there is an urgent need to address these issues through targeted research and policy interventions.
Pediatric nursing is integral to the well-being of hospitalized children, as it involves providing specialized care tailored to their unique physical, emotional and developmental needs. However, the literature reveals a notable gap in understanding the distinct challenges encountered by pediatric nurses, particularly in Iran. While existing studies generally address broader nursing challenges, they often overlook the cultural, organizational, and resource-specific factors that uniquely impact pediatric nursing in this region. A comprehensive understanding of these challenges is crucial for developing targeted interventions that can support pediatric nurses and enhance patient care outcomes. This systematic review aimed to address this literature gap by systematically identifying and categorizing the challenges faced by pediatric nurses in Iran. By elucidating these challenges, the study seeks to foster the professional development of pediatric nurses and provide evidence-based recommendations to healthcare policymakers and administrators. Ultimately, this research aimed to improve the quality of pediatric care and optimize the working conditions for pediatric nurses in Iran, thereby advancing overall healthcare outcomes for children.
Methods
Given the rising volume of literature on the problems and challenges faced by Iranian pediatric nurses, it is essential to assess the cumulative advancements in the field and track the current level of knowledge in this area. We used the preferred reporting items for systematic reviews and meta-analyses (PRISMA) checklist to ensure that the reporting of the systematic review was of high quality [14]. The checklist, which includes four sequential processes (identification, screening, eligibility and inclusion) and 27 elements, is designed to help authors perform more effective systematic reviews (Figure 1).
Questions and research objectives
RQ1: Research questions: What are the main problems faced by pediatric nurses in Iran’s healthcare system?; RQ2: What challenges do pediatric nurses encounter in their daily practice, and how do these challenges impact their professional experience and patient care?
The objective of this systematic review was to provide a comprehensive understanding of the issues and difficulties encountered by pediatric nurses in Iran. By systematically evaluating the existing literature, this review aimed to: Identify the key problems and challenges faced by pediatric nurses in the Iranian healthcare system. Assess how these issues impact the quality of patient care and the professional well-being of pediatric nurses. Explore potential areas for improvement within the healthcare system and identify opportunities for enhancing support and training for pediatric nurses. Develop evidence-based recommendations to guide healthcare policymakers and administrators in addressing these challenges effectively.
Search technique
This is a systematic review aimed at investigating published clinical trials, observational, quasi-experimental, and qualitative investigations from January 1, 2015 to May 3, 2023, across nine scientific research databases, including PubMed, ScienceDirect, Wiley Online, Scopus, SciELO, LILACS and Google Scholar, as well as several Persian databases, including Magiran and scientific information database (SID). The keywords used in English and Persian were TS=([“pediatric nursing”] AND [“challenges”] AND [“problems”] AND [“pediatric” OR “children”] AND [“Iran”]). The initial search yielded 965 articles, of which 909 were removed for not meeting the inclusion criteria, leaving 28 articles for analysis.
Inclusion criteria
Studies were considered admissible if they: 1) Were clinical trials, observational studies, quasi-experimental studies, and qualitative studies, 2) Involved pediatric nurses working in any healthcare setting in Iran, 3) Specifically addressed the challenges and problems faced by pediatric nurses in Iran, 4) Were published from 2015 to 2023, 5) were published in English and Persian and 6) Had a code of ethics.
These criteria were established to ensure that the studies included in the review are relevant, high-quality, and specific to the context of pediatric nursing in Iran. By focusing on recent publications and including studies with ethical considerations, the review aimed to provide a comprehensive and accurate assessment of the challenges faced by pediatric nurses.
Exclusion criteria
Exclusion criteria were: 1) Lack of access to full texts, 2) Individual case reports, systematic reviews and meta-analyses and 3) Unrelated objectives.
Quality assessment of the articles
A critical appraisal was performed according to the study design of the articles. The critical appraisal skills program (CASP) was used for analysis. The CASP is a 10-item questionnaire with three possible answers: “Yes,” “no” and “can’t tell.” If eight or more of the criteria on the checklist were met, the study was rated as “good” quality, if five to seven were met, it was rated as “fair” quality, and if fewer than five were met, it was scored as “poor” quality. To ensure consistency and reliability in the critical appraisal process, two independent reviewers conducted the assessments. Any discrepancies in their evaluations were resolved through consensus, guaranteeing a thorough and unbiased analysis. Data were extracted from all papers, which met the eligibility and inclusion criteria for the review.
Data extraction
Two authors independently conducted the literature search, followed by the application of the inclusion and exclusion criteria, and screened the studies based on their titles and abstracts. Adhering to the PRISMA checklist ensured a rigorous and transparent review process. The screening process was carried out for duplicates using EndNote software, version X7 (clarivate analytics). After initial screening, the full texts of studies were obtained and examined to ensure eligibility for the development of the data extraction table. Data were extracted from the final set of included full texts, encompassing information, such as the first author, year of publication, study design, purpose, sample size, participant demographics, study setting, challenges and problems faced by pediatric nurses, duration of the studies, intervention used to the challenges and problems, and the reported outcomes associated with the challenges and problems faced by pediatric nurses in Iran (Table 1).
Results
Figure 1 outlines the outcomes of the search strategy. Initially, 965 articles were identified, with 25 duplicates removed, leaving 940 references. After applying initial inclusion criteria to titles, abstracts, and full texts in English and Persian, 31 articles were shortlisted. Upon further review of the full texts of these articles based on inclusion and exclusion criteria, three were excluded. Ultimately, 28 papers were included in the study. Data were systematically extracted from these papers (Table 1). Of the 28 studies, 18 were qualitative studies and one was a descriptive study. The reviews that comprised this study were carried out in various pediatric wards. The total sample sizes of the studies ranged from 15 to 423 subjects, with 17 studies using a sample size of 15–50 subjects and 5 using a sample size of 51–150 subjects. Six of the articles used samples that ranged in size from 151 to 423 people.
A thematic analysis approach was used to combine the study results in order to find recurring themes and patterns. Through this process, several key themes emerged across the studies, providing valuable insights into the subject matter. The identified themes encompassed various aspects of barriers and challenges in pediatric nursing care. These included problems, like a disregard for proper drug administration procedures, medication errors, cultural issues, moral conundrums, language barriers, and organizational limitations.
Some of the key findings
Requirements for a Healthy Workplace: To improve their well-being and deliver the best care possible to children with cancer, oncology nurses expressed the need for a supportive and healthy work environment. Workload, emotional demands and a lack of resources were all mentioned as barriers to a positive work environment [1, 23, 24]. Clinical learning environment challenges: One of the significant challenges faced by pediatric nurses is related to the education and supervision of nursing students during clinical rotations. Pediatric nurses often encounter difficulties, such as balancing patient care with the responsibility of guiding students, ensuring proper supervision and providing meaningful hands-on opportunities for student learning. The presence of students can sometimes increase the workload for nurses, as they must ensure that students are accurately applying theoretical knowledge in a real-world setting. These challenges not only affect the professional development of nursing students but also place additional strain on pediatric nurses, who must manage both educational and clinical responsibilities simultaneously [16, 25, 26].
Problems with specialized units and moral judgment: Staff members working in the neonatal intensive care units (NICU) frequently encountered communication issues, emotional stress, and moral conundrums. These difficulties emphasized the requirement for comforting measures and moral frameworks for making decisions in NICU settings [4, 18, 27-29]. Experiences of healthcare staff in angiography: Technical challenges, emotional stress and the need for specialized training to handle the particular needs of pediatric patients undergoing angiography were all reported by medical staff as being related to angiography in pediatric patients [19]. Altruism and caring self-efficacyaltruism is a crucial component of pediatric nurses’ caring self-efficacy, as it enables them to prioritize their patients’ needs and provide compassionate care. It also positively impacts their sense of self-efficacy and professional fulfillment. Prioritizing the needs of patients and delivering compassionate care should be at the forefront of every nurse’s practice[20, 30, 31]. Medication errors in pediatric wards: Medication errors have been identified as a problem in pediatric wards, with a variety of frequencies, types, and causes. Heavy workload, lack of knowledge or training, distractions, and communication breakdowns were among the factors that contributed to medication errors [17, 21, 32-35]. Barriers to pain management and communication challenge: Effective pain management for pediatric patients was hindered by a lack of training, inadequate assessment tools, side effect anxiety, lack of knowledge, and communication difficulties with young or nonverbal patients [22, 36, 37]. These difficulties brought to light the complexity and multifaceted nature of pediatric patient care, which calls for specialized skills and highlights the need for organizational structure and educational program improvements.
Discussion
According to our knowledge, this systematic review is the first piece of research data to offer insightful information on the obstacles and difficulties pediatric nurses experience when providing care. The core themes that cover many facets of pediatric nursing care were found using the thematic analysis method used to synthesize the study’s data. The themes that were found provided insight into a number of important difficulties facing pediatric nurses. These challenges included failing to follow correct drug administration procedures, taking the wrong prescription, having cultural or moral disagreements, having trouble communicating and having organizational problems.
These findings highlight the complex nature of pediatric nursing and the multifaceted challenges that nurses encounter in their practice. The theme of transition and adaptation revealed that pediatric nurses transferred to adult COVID-19 wards faced challenges with patient management, medical knowledge and emotional strain. This underscores the need for additional support and resources to facilitate the transition of pediatric nurses to adult care settings. Our results largely support studies conducted by Darchen et al. [38], which demonstrated that during the first wave of the pandemic, the main challenges faced by pediatric nurses moving into adult COVID-19 wards were related to their working environments, safety, communication, and care for terminally ill patients.
The theme of a healthy work environment revealed that oncology nurses expressed the need for a supportive and healthy work environment to enhance their well-being and provide optimal care to pediatric oncology patients. Factors, such as workload, emotional demands, and lack of resources were identified as obstacles. Addressing these challenges requires attention to workload management, emotional support and resource allocation in pediatric oncology settings. Similarly, Kleis and Kellogg reported that the pressure to perform despite emotional strain and feelings of being unsupported can lead to secondary traumatic stress in pediatric nurses [39]. Ethical decision-making challenges and challenges in specialized units, particularly NICUs, were another prominent theme. Personnel working in NICUs encountered dilemmas related to communication and ethical considerations [40-42]. In contrast, a study conducted in South Korea examined the moral challenges pediatric nurses encounter when caring for hospitalized children at the bedside. Three themes emerged from the analysis: Difficulty expressing oneself in an authoritative setting, ethical numbness, and negative emotions toward caregivers in the family [43]. The findings emphasize the importance of supportive measures and ethical decision-making frameworks in NICU settings to enhance patient care and support healthcare professionals in navigating complex ethical situations. Medication errors in pediatric wards were identified as a concern, with various contributing factors. These factors include heavy workload, lack of knowledge or training, distractions, and communication breakdowns [44, 45]. Barriers to pain management and communication challenges were also highlighted. Nurses in pediatric units encountered obstacles in effectively managing pain, including inadequate assessment tools, fear of side effects, lack of knowledge or training, and difficulties in communicating with non-verbal or young patients.
Our findings are supported by research conducted by Wuni et al. [46], Alotaibi et al. [47], Kusi Amponsah et al. [48]. Improvements in pain assessment tools, education, and communication skills can help overcome these barriers and ensure effective pain management in pediatric care. The studies demonstrated various coping mechanisms and solutions that nurses employed in response to the identified difficulties. Individual resilience strategies, social support, improved managerial support, and the acquisition of specialized knowledge and skills are some of these tactics. Additionally, the importance of implementing changes within the healthcare system was emphasized, such as workload reduction, awareness-raising campaigns, reevaluating drug prescription methods, and establishing rules and policies. The use of specific inclusion criteria further restricted the already available body of evidence. The drawbacks of the review included the limited data that met our inclusion criteria and the high degree of heterogeneity among the included studies, which was caused by differences in the interventions and outcome metrics. Moreover, restricting the studies to those conducted in Iran may have led to the exclusion of otherwise pertinent papers, thereby limiting the international applicability of our findings.
Conclusion
This systematic study highlights the numerous obstacles faced by pediatric nurses in Iran, which include prescription mistakes, cultural quandaries, moral quandaries, language limitations and organizational limits. These findings highlight the importance of improving healthcare, education and organizational support to advance pediatric nursing practice. This study calls for further research to address these issues and enhance the quality of pediatric nursing care. The implications for nursing and health policy are clear: Proper training, cultural competency and supporting frameworks are necessary to empower pediatric nurses and, as a result, improve patient well-being.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Supervision: Candan Ozturk; Writing the original draft: Pouran Varvani Farahani; Study design, data collection, data analysis, review and editing: All authors.
Conflicts of interest
The authors declared no conflict of interest.
References
- Nukpezah RN, Fomani FK, Hasanpour M, Nasrabadi AN. A qualitative study of Ghanaian pediatric oncology nurses’ care practice challenges. BMC Nurs. 2020; [Unpublished]. [DOI:10.21203/rs.3.rs-33095/v2]
- Elbilgahy AA, Sliman AMAF, Hegazy AESA, Mohammed BA. [Improving pediatric critical care nurses’ knowledge and practices regarding restraint application and children’s outcomes (Persian)]. Tanta Sci Nurs J. 2022; 25(2):318-42. [DOI:10.21608/tsnj.2022.236103]
- Cranage K, Foster KN. Mental health nurses’ experience of challenging workplace situations: A qualitative descriptive study. Int J Ment Health Nurs. 2022; 31(3):665-76. [DOI:10.1111/inm.12986]
- Ghasemi E, Negarandeh R, Janani L. Moral distress in Iranian pediatric nurses. Nurs Ethics. 2019; 26(3):663-73. [DOI:10.1177/0969733017722824]
- Kellogg MB, Knight M, Dowling JS, Crawford SL. Secondary traumatic stress in pediatric nurses. J Pediatr Nurs. 2018; 43:97-103. [DOI:10.1016/j.pedn.2018.08.016]
- Berger J, Polivka B, Smoot EA, Owens H. Compassion fatigue in pediatric nurses. J Pediatr Nurs. 2015; 30(6):e11-7. [DOI:10.1016/j.pedn.2015.02.005]
- Mohamed DA, Alatroshi AM. Effectiveness of an educational program on nurses’ practice regarding neonatal sepsis in neonatal and premature care units a quasi-experimental study. Med J Babylon. 19(2):185-90. [DOI:10.4103/MJBL.MJBL_98_21]
- Abdelgadir WI, Sayed SAM, Hassan SA. Nurses competences regarding nursing care of neonatal sepsis 2019. Sch J Appl Med Sci. 2021; 9(10):1547-52. [DOI:10.36347/sjams.2021.v09i10.012]
- Hupp DS, Mastrangelo B, Nelson KA, Weyant DM, Schreiber JB. A Pediatric-specific view on improved nurse-sensitive indicators related to increased BSN or higher rates over time. J Nurs Care Qual. 2022; 37(4):289-94. [DOI:10.1097/NCQ.0000000000000629]
- Oyesanya TO, Snedden TR. Pediatric nurses’ perceived knowledge and beliefs of evidence-based practice in the care of children and adolescents with moderate-to-severe traumatic brain injury. J Spec Pediatr Nurs. 2018; 23(2):e12209. [DOI:10.1111/jspn.12209]
- Alomari A, Wilson V, Solman A, Bajorek B V, Tinsley P. Pediatric nurses’ perceptions of medication safety and medication error: A mixed methods study. Compr Child Adolesc Nurs. 2018; 41(2):110-94. [DOI:10.1080/24694193.2017.1323977]
- Hamama-Raz Y, Hamama L, Pat-Horenczyk R, Stokar YN, Zilberstein T, Bron-Harlev E. Posttraumatic growth and burnout in pediatric nurses: The mediating role of secondary traumatization and the moderating role of meaning in work. Stress Health. 2020; 37(3):442-53. [DOI:10.1002/smi.3007]
- Shoorideh FA, Ashktorab T, Yaghmaei F, Majd HA. Relationship between ICU nurses’ moral distress with burnout and anticipated turnover. Nurs Ethics. 2015; 22(1):64-76. [DOI:10.1177/0969733014534874]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021; 372:n71. [DOI:10.1136/bmj.n71]
- Soheili M, Taleghani F, Jokar F, Eghbali-Babadi M, Sharifi M. Oncology nurses’ needs respecting healthy work environment in Iran: A descriptive exploratory study. Asia Pac J Oncol Nurs. 2021; 8(2):188-96. [DOI:10.4103/apjon.apjon_64_20]
- Jamshidi N, Molazem Z, Sharif F, Torabizadeh C, Najafi Kalyani M. The challenges of nursing students in the clinical learning environment: A qualitative study. Sci World J. 2016; 2016(1):1846178. [DOI:10.1155/2016/1846178]
- Soltanian M, Molazem Z, Mohammadi E, Sharif F, Rakhshan M. Professional responsibility: An ethical concept extracted from practices of Iranian nurses during drug administration. Int J Pharm Res. 2018; 10(3):346-53. [DOI:10.31838/ijpr/2018.10.03.022]
- Kadivar M, Mosayebi Z, Asghari F, Zarrini P. Ethical challenges in the neonatal intensive care units: perceptions of physicians and nurses; An Iranian experience. J Med Ethics Hist Med. 2015; 8:1. [PMID]
- Heidari H, Khaledifar A. Experiences of healthcare staff regarding angiography in infants. IJN. 2021; 12(1):1-7. [Link]
- Alavi A, Zargham-Boroujeni A, Yousefy A, Bahrami M. Altruism, the values dimension of caring self-efficacy concept in Iranian pediatric nurses. J Educ Health Promot. 2017; 6(1):8. [DOI:10.4103/jehp.jehp_142_14]
- Izadpanah F, Nikfar S, Imcheh FB, Amini M, Zargaran M. Assessment of frequency and causes of medication errors in pediatrics and emergency wards of teaching hospitals affiliated to Tehran University of Medical Sciences (24 hospitals). J Med Life. 2018; 11(4):299-305. [DOI:10.25122/jml-2018-0046]
- Aziznejadroshan P, Alhani F, Mohammadi E. Experience of nurses about barriers to pain management in pediatric units: A qualitative study. J Nurs Midwifery Sci. 2017; 4(3):89-96. [DOI:10.4103/JNMS.JNMS_2_17]
- Hajibabaee F, Najafvandzadeh M, Haghighizadeh MH. Job satisfaction and its effective factors among nurses working in pediatric wards. Iran J Nurs. 2016; 29(101):57-66. [DOI:10.29252/ijn.29.101.57]
- Soltanian M, Molazem Z, Mohammadi E, Sharif F, Rakhshan M. Iranian nurses’ experiences on obstacles of safe drug administration: A qualitative study. Glob J Heal Sci. 2016; 8(10):56009. [DOI:10.5539/gjhs.v8n10p88]
- Vosoghi N, Fallahi-Khoshknab M, Hosseini M, Ahmadi F. Nursing care challenges of child violence victims: A qualitative study. Iran J Nurs Midwifery Res. 2021; 26(5):430. [DOI:10.4103/ijnmr.IJNMR_151_20]
- Iranmanesh S, Banazadeh M, Forozy MA. Nursing staff’s perception of barriers in providing end-of-life care to terminally ill pediatric patients in Southeast Iran. Am J Hosp Palliat Med. 2016; 33(2):115-23. [DOI:10.1177/1049909114556878]
- Vosoghi N, Fallahi-Khoshknab M, Hosseini M, Ahmadi F. Iranian Nurses’ experiences of their roles in care provision to the victims of child violence: A qualitative study. Nurs Midwifery Stud. 2021; 10(1):27. [DOI:10.4103/nms.nms_123_19]
- Mehdipour-Rabori R, Nematollahi M, Bagherian B, Esmaelzadeh F. Ethical challenges associated with caring for sick children based on the experiences of nursing students in pediatric wards: A qualitative content analysis. J Qual Res Heal Sci. 2023; 12(1):9-16. [DOI:10.34172/jqr.2023.02]
- Behbodi M, Shafipour V, Amiri M. [Comparison of moral distress severity between pediatric ward and pediatric intensive care unit nurses (Persian)]. J Relig Health. 2018; 6(1):19-28. [Link]
- Ebadinejad Z, Fakhr-Movahedi A. Palliative care strategies of Iranian nurses during children’s death from cancer: A qualitative study. East Mediterr Heal J. 2022;28(7). [DOI:10.26719/emhj.22.047]
- Alavi A, Bahrami M, Zargham-Boroujeni A, Yousefy A. Threats to pediatric nurses' perception of caring self-efficacy: A qualitative study. Iran Red Crescent Med J. 2015; 18(3):e25716. [DOI:10.5812/ircmj.25716] [PMID]
- Mousavi-Roknabadi RS, Momennasab M, Askarian M, Haghshenas A, Marjadi B. Causes of medical errors and its under-reporting amongst pediatric nurses in Iran: A qualitative study. Int J Qual Health Care. 2019; 31(7):541-6. [DOI:10.1093/intqhc/mzy202]
- Miladinia M, Zarea K, Baraz S, Mousavi Nouri E, Pishgooie AH, Gholamzadeh Baeis M. Pediatric nurses’ medication error: The self-reporting of frequency, types and causes. J Pediatr Perspect. 2016; 4(3): 1439-44. [DOI:10.22038/ijp.2016.6593]
- Salmani N, Fallah Tafti B. Frequency, type and causes of medication errors in pediatric wards of hospitals in Yazd, the Central of Iran. Int J Pediatr. 2016; 4(9):3475-87. [Link]
- Ramazani T, Hosseini Almadvari SM, Fallahzadeh H, Dehghani Tafti A. [Type and rate of medication errors and their causes from the perspectives of neonatal and neonatal intensive care units nurses in Yazd hospitals, 2014 (Persian). J Commun Heal. 2017; 10(1):63-71. [Link]
- Beykmirza R, Negarandeh R, Varzeshnejad M. Experiences of Iranian pediatric nurses in providing care to hospitalized children of different language backgrounds: A qualitative study. J Transcult Nurs. 2022; 33(1):79-86. [DOI:10.1177/10436596211016535]
- Abazari P, Namnabati M. Nurses’ experiences from pain management in children in Iranian culture: A phenomenology study. J Educ Health Promot. 2017; 6(1):74. [DOI:10.4103/jehp.jehp_1_16]
- Darchen F, Audouin H, Berger M, Juin-Leonard V. The experiences of pediatric nurses deployed to adult COVID-19 wards. Arch Pediatr. 2023; 30(3):179-86. [DOI:10.1016/j.arcped.2023.01.004]
- Kleis AE, Kellogg MB. Recalling stress and trauma in the workplace: A qualitative study of pediatric nurses. Pediatr Nurs. 2020; 46(1):5. [Link]
- Bucher HU, Klein SD, Hendriks MJ, Baumann-Hölzle R, Berger TM, Streuli JC, et al. Decision-making at the limit of viability: differing perceptions and opinions between neonatal physicians and nurses. BMC Pediatr. 2018; 18:226. [DOI:10.1186/s12887-018-1204-x]
- Mitchell S, Spry JL, Hill E, Coad J, Dale J, Plunkett A. Parental experiences of end of life care decision-making for children with life-limiting conditions in the paediatric intensive care unit: A qualitative interview study. BMJ Open. 2019; 9(5):e028548. [DOI:10.1136/bmjopen-2018-028548]
- Lantos JD. Ethical problems in decision making in the neonatal ICU. N Engl J Med. 2018; 379(19):1851-60. [DOI:10.1056/NEJMra1801063]
- Choe K, Kim Y, Yang Y. Pediatric nurses’ ethical difficulties in the bedside care of children. Nurs Ethics. 2019; 26(2):541-52. [DOI:10.1177/0969733017708330]
- Alrabadi N, Shawagfeh S, Haddad R, Mukattash T, Abuhammad S, Al-rabadi D, et al. Medication errors: A focus on nursing practice. J Pharm Heal Serv Res. 2021; 12(1):78-86. [DOI:10.1093/jphsr/rmaa025]
- Vaziri S, Fakouri F, Mirzaei M, Afsharian M, Azizi M, Arab-Zozani M. Prevalence of medical errors in Iran: A systematic review and meta-analysis. BMC Health Serv Res. 2019; 19(1):622. [DOI:10.1186/s12913-019-4464-8]
- Wuni A, Salia SM, Mohammed Ibrahim M, Iddriss I, Abena Nyarko B, Nabila Seini S, et al. Evaluating knowledge, practices, and barriers of paediatric pain management among nurses in a tertiary health facility in the northern region of ghana: A descriptive cross-sectional study. Pain Res Manage. 2020; 2020(1):8846599. [DOI:10.1155/2020/8846599]
- Alotaibi K, Higgins I, Day J, Chan S. Paediatric pain management: knowledge, attitudes, barriers and facilitators among nurses-integrative review. Int Nurs Rev. 2018; 65(4):524-33. [DOI:10.1111/inr.12465]
- Kusi Amponsah A, Kyei EF, Agyemang JB, Boakye H, Kyei-Dompim J, Ahoto CK, et al. Nursing-related barriers to children’s pain management at selected hospitals in Ghana: A descriptive qualitative study. Pain Res Manage. 2020; 2020(1):7125060. [DOI:10.1155/2020/7125060]
Type of Study: Systematic Review |
Subject:
Pediatrics
Received: 2024/02/21 | Accepted: 2024/09/1 | Published: 2024/07/1
Received: 2024/02/21 | Accepted: 2024/09/1 | Published: 2024/07/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |