Volume 13, Issue 2 (4-2025)
J. Pediatr. Rev 2025, 13(2): 145-150 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Edalatkhah R, Sadatmoosavi N, Pourshamsi F. Examining the Association Between Anxiety Severity and Required Sedative Medication Dosage in Children Undergoing Upper Gastrointestinal Endoscopy. J. Pediatr. Rev 2025; 13 (2) :145-150
URL: http://jpr.mazums.ac.ir/article-1-618-en.html
URL: http://jpr.mazums.ac.ir/article-1-618-en.html
1- Hematology and Oncology Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. , Drr.edalatkhah@gmail.com
2- Shahid Sadoughi General Hospital, Shahid Sadoughi University of Medical Sciences, Iran, Yazd.
2- Shahid Sadoughi General Hospital, Shahid Sadoughi University of Medical Sciences, Iran, Yazd.
Full-Text [PDF 344 kb]
(580 Downloads)
| Abstract (HTML) (1598 Views)
Full-Text: (233 Views)
Introduction
Upper gastrointestinal endoscopy (UGE) is an invasive diagnostic-therapeutic procedure commonly employed for the evaluation and management of gastrointestinal disorders. Its utilization in pediatric patients has significantly increased in recent decades [1]. However, this procedure can induce anxiety and fear in both children and their parents [2, 3]. Compared to adults, children are more susceptible to anxiety due to their limited emotional and behavioral development [4].
The advancement and availability of endoscopic technology, coupled with the growing number of endoscopy centers, have led to the widespread use of sedation techniques to enhance patient comfort during the procedure. Intravenous sedation is commonly administered to alleviate anxiety, pain, and discomfort associated with the diagnostic-therapeutic process. However, despite the implementation of intravenous sedation, it may not effectively address pre-endoscopy anxiety in pediatric patients [5].
The significance of preventing and mitigating severe anxiety during medical interventions extends beyond patient comfort, as it can also positively impact procedure duration and minimize potential side effects [3, 6, 7].
Understanding the interplay between anxiety severity and sedation requirements enhances procedural safety and contributes to the development of targeted interventions aimed at alleviating pre-procedural anxiety in children. Thus, further research in this area is essential to establish evidence-based guidelines that can enhance UGE efficacy and safety in pediatric populations.
Methods
This analytical cross-sectional observational study was conducted at Shahid Sadouqi Medical Education Hospital in Yazd City, Iran, from September 2022 to May 2023. The study included children aged 3-7 years who were scheduled for outpatient upper endoscopy.
Inclusion and exclusion criteria
The inclusion criteria were children aged 3-7 years who required elective diagnostic UGE on an outpatient basis, as determined by a pediatric gastroenterology specialist. Meanwhile, children with a history of upper gastrointestinal surgery, previous or recent endoscopy, psychiatric disorders or diseases, anticipated airway problems, allergies to propofol, concurrent treatment during endoscopy, significant systemic illness, mental retardation, and neurodevelopmental delays were excluded from the study.
A total of 50 children were included in the study, according to the sample size determined. The sample size was determined based on a power analysis aiming for 80% power to detect significant differences with a significance level of 0.05. Meanwhile, data collection involved the following procedures.
Pre-endoscopy assessment
Before performing UGE, adherence to fasting guidelines is essential. As per the American Society of Anesthesiologists (ASA), patients should fast for a minimum of 2 h after consuming clear liquids and 6 hours after consuming light meals [8]. The demographic information of the children, including age and gender, was recorded.
Anxiety assessment
Upon arrival at the endoscopy department, the child was directed to the waiting room. Before any treatment procedures, the nurse provided the parents with the preschool anxiety score questionnaire in Persian for completion. The preschool anxiety score questionnaire demonstrates good reliability (0.73 to 0.82) and validity (0.41 to 0.67). In the present study, the Cronbach α coefficient was calculated to be above 0.7 [9]. The questionnaire comprises scores ranging from zero (minimum) to 112 (maximum). Scores between 0-36 indicate low anxiety levels, 37-75 indicate moderate anxiety levels, and scores exceeding 75 indicate high anxiety levels.
Sedation protocol
Before entering the endoscopy room, an intravenous catheter was inserted in the right forearm to facilitate the infusion of 0.9% saline to maintain vein patency. All patients were equipped with a pulse oximeter, a three-lead electrocardiogram, and a non-invasive blood pressure cuff, following which the patient was positioned on their left side, and supplemental oxygen was administered via a nasal cannula. In this study, propofol was the sole sedative used for children, with an initial dose of 2 mg/kg and additional doses of 0.5 mg/kg administered every 3-5 min until deep sedation was achieved. Deep sedation, as required for endoscopy, was determined by assessing the level of consciousness using the University of Michigan sedation scale (UMSS) [10]. The UMSS is an observational tool that ranges from 5 (fully awake) to 4 (unexcitable). For this study, a UMSS score of 3 or 4 was necessary. If deep sedation was not achieved, an additional dose of propofol was administered and documented in the patient’s record. No other medications, including analgesics, were employed in this study. The entire sedation process was conducted by an anesthesiologist who was unaware of the anxiety scores before the endoscopy. Any sedation-related complications, including oxygen saturation <90%, hiccups, snoring, restlessness, and decreased respiratory rate, were recorded.
Endoscopy procedure
The endoscopy procedure was performed by one pediatric gastroenterologist following standard protocols. The duration of the procedure was recorded.
Data analysis
The collected data were analyzed using the SPSS software, version 27. Appropriate statistical tests, including chi-square and t-tests, were employed to perform comparisons. A significance level of P<0.05 was used, indicating statistical significance.
Results
In this study, a total of 50 children (23 boys and 27 girls) aged between 3 to 7 years, with a mean age of 5±2.3 years and 1 month, underwent diagnostic UGE. The main objective was to assess the severity of anxiety among these children (Table 1).
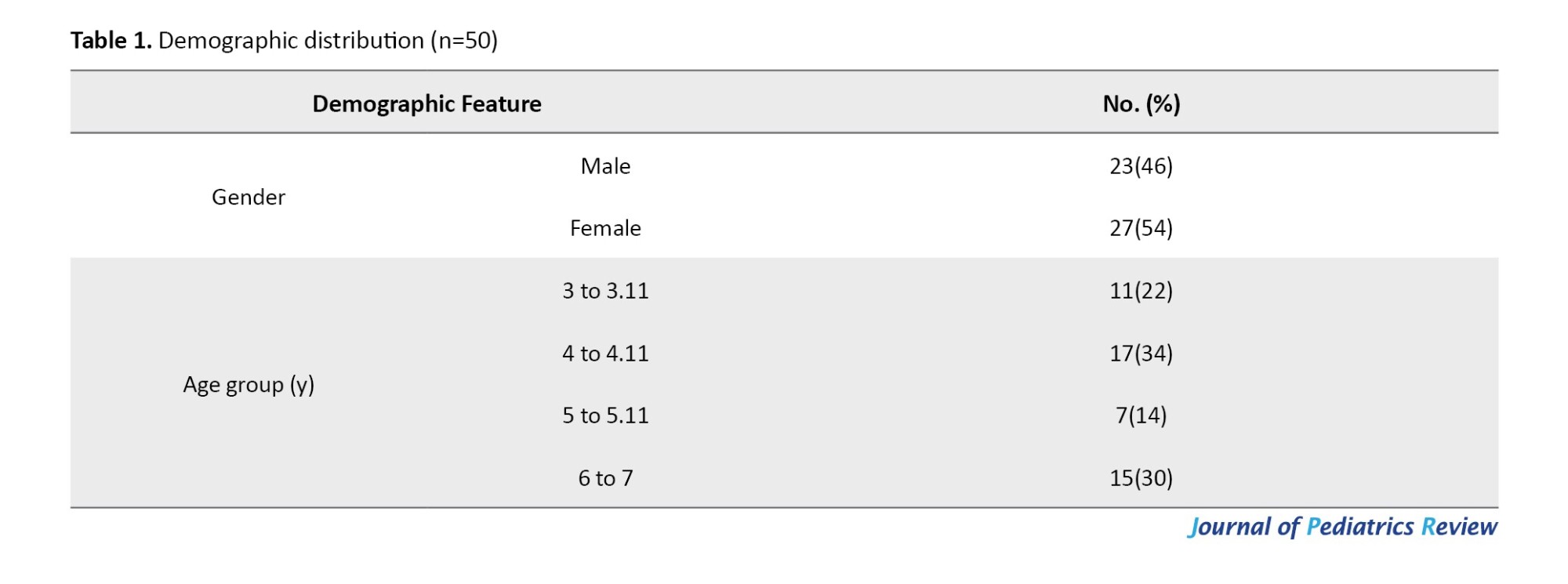
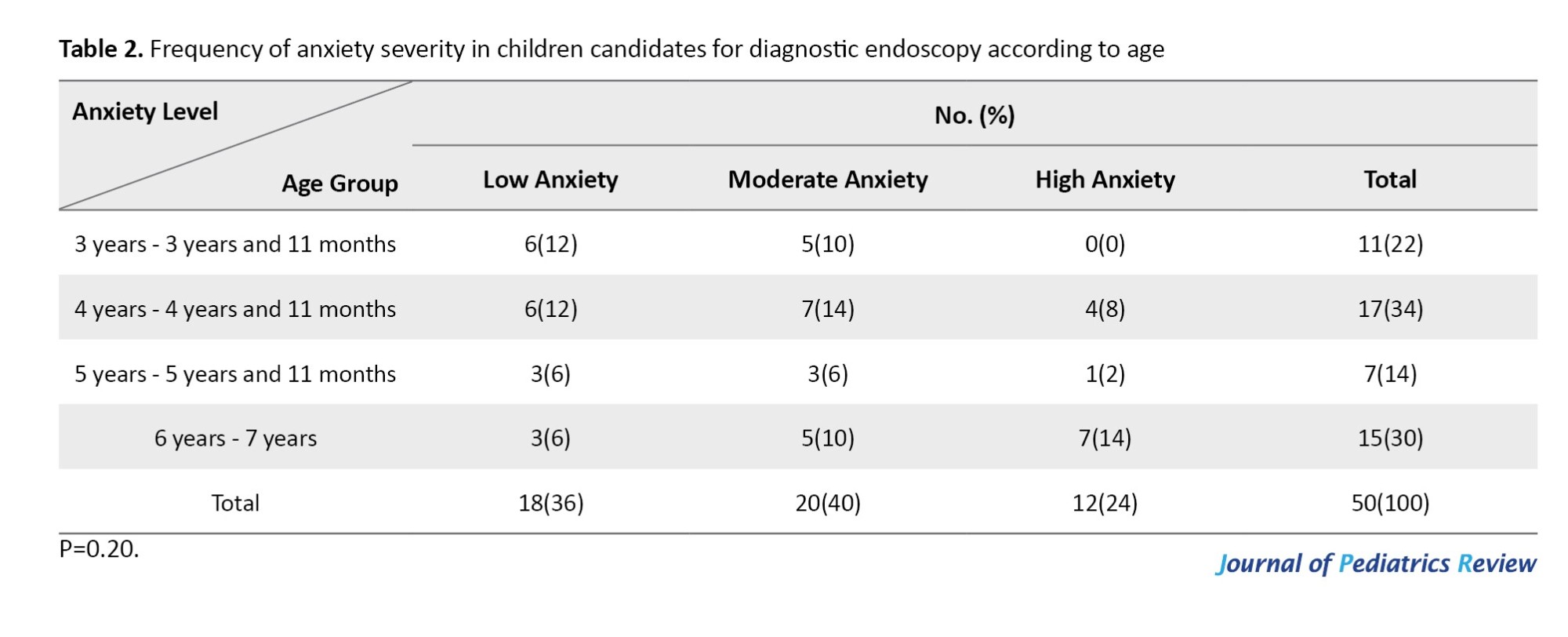
The anxiety scores ranged from 20 to 105, with a mean score of 57.7. Out of the 50 children, 18(36%) exhibited low anxiety levels, 20(40%) showed moderate anxiety levels, and 12(24%) experienced high anxiety levels. Statistical analysis revealed no significant correlation between anxiety levels and age groups (P=0.20; Table 2).
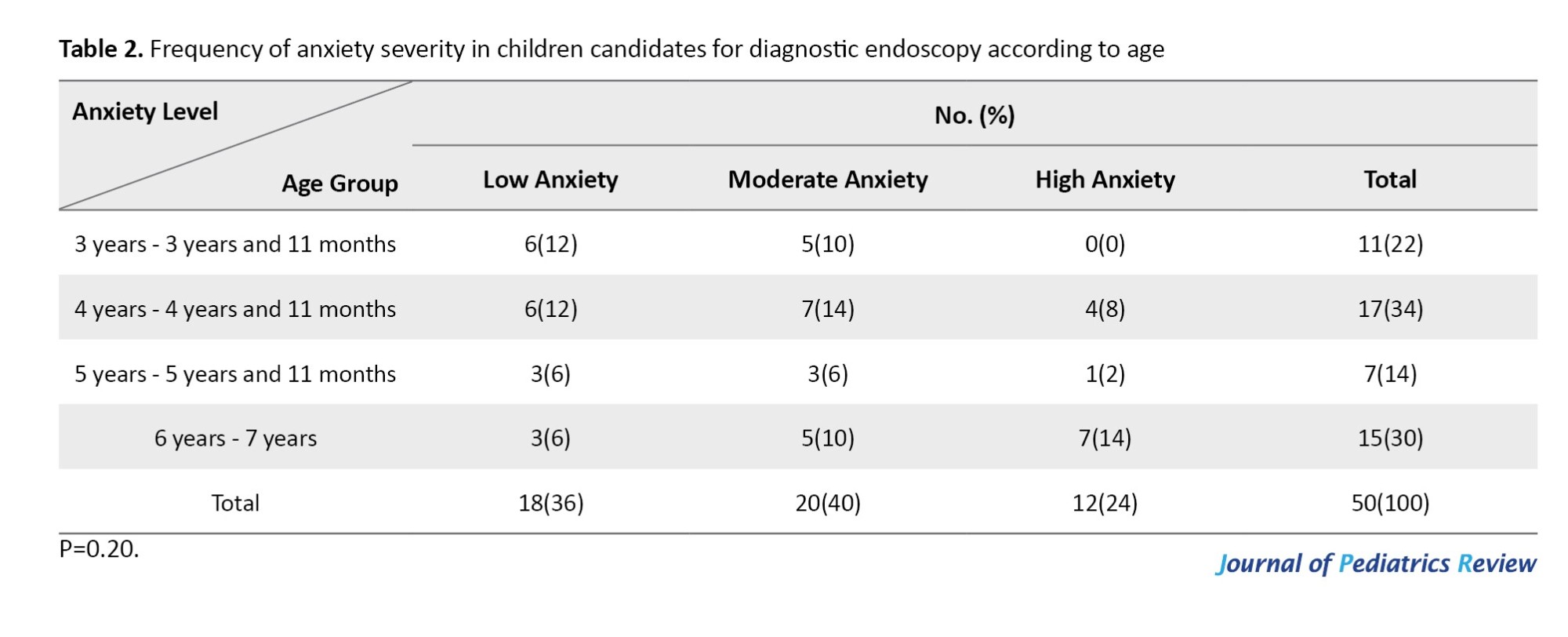
In terms of gender distribution, out of the total sample of 50 children, 23(46%) were boys and 27(54%) were girls. However, no significant relationship was found between the intensity of anxiety and the gender of the children (P=0.766).
Among the 50 children, 30 cases received an additional dose of propofol during the procedure. Out of these 30 cases, 5(10%) had low anxiety, 13(26%) had moderate anxiety, and 12(24%) experienced severe anxiety. A significant association was observed between the anxiety intensity and the requirement for an extra dose of propofol (P<0.001). Restlessness during endoscopy was reported in 30 patients. There was a significant correlation between the intensity of anxiety and the occurrence of irritability during the procedure (P<0.001).
The minimum duration of the endoscopy procedure was 1 minute, while the maximum duration reached 10 min, with a mean duration of 3.66 min. Notably, a statistically significant relationship was found between the intensity of anxiety and the duration of the endoscopy procedure (P=0.027). Specifically, the mean duration of endoscopy for cases with high anxiety intensity was recorded as 4.95±1.95 min, indicating a slightly longer duration compared to other levels of anxiety intensity.
The recovery time after the procedure varied between 5 and 40 min, with a mean recovery time of 20.2±8.4 min. There was a significant association between the intensity of anxiety and the recovery time (P=0.048). Specifically, the mean recovery time for children with high anxiety was 29.72±6.84.
Among the complications associated with sedation, restlessness was the most common, occurring in 19 cases (57.57%). Other complications included a reduction in SPO2 in 7 cases (21.21%), snoring in 5 cases (15.15%), and hiccups in 2 cases (6.07%). Notably, none of the children in this study experienced a decrease in the respiratory rate. Significant relationships were observed between the effects of sedation and the intensity of children’s anxiety, as well as the administration of an additional dose of propofol (P of 0.001 and <0.001, respectively). Specifically, restlessness and hiccups were significantly associated with the intensity of anxiety (P of 0.006 and 0.037, respectively). However, no significant relationships were found between SPO2 reduction, snoring, and the intensity of anxiety (P of 0.183 and 0.083, respectively).
Discussion
This study evaluated the relationship between anxiety severity and the dosage of sedative medication required for children undergoing UGE. The findings demonstrate a significant association between pre-endoscopy anxiety levels and the need for additional doses of Propofol, as well as the duration of the procedure, recovery time, and sedation-related complications.
The results indicated that higher anxiety levels were correlated with an increased requirement for additional doses of propofol. This finding aligns with previous studies that suggest children with elevated anxiety require more sedation to achieve the desired level of comfort during invasive procedures [1]. Notably, our results highlight the critical role that anxiety management can play in optimizing sedation protocols, potentially reducing the need for higher medication doses.
Additionally, this study found a significant relationship between anxiety intensity and both the duration of the endoscopy and the recovery time. Children with high anxiety experienced more prolonged procedures and extended recovery periods. This is consistent with research indicating that anxiety can prolong medical interventions, leading to increased patient discomfort and resource utilization [11]. Understanding this relationship emphasizes the importance of addressing anxiety proactively to enhance procedural efficiency.
Restlessness was the most frequently reported sedation-related complication, and this analysis showed a significant correlation between anxiety levels and the incidence of restlessness during the procedure. This supports findings from similar studies indicating that anxious patients are more likely to experience adverse effects from sedation [8]. The implications of these findings suggest that by mitigating anxiety, we may also reduce the occurrence of such complications, ultimately improving the overall experience for pediatric patients.
While this study focused on a pediatric population, it is essential to acknowledge that much of the existing literature on anxiety and sedation in endoscopic procedures has centered around adults. This gap highlights the need for more targeted research in children to develop age-appropriate interventions. For instance, studies involving adult cohorts, such as those by Osborn et al. (2004) [12], have shown varying associations between anxiety and sedation requirements, underscoring the need for pediatric-specific insights.
The findings of this study suggest that implementing anxiety-reducing interventions before endoscopy could be beneficial. Various techniques, such as pre-procedural counseling, play therapy, or the use of calming music, may help lower anxiety levels and, consequently, reduce the dosage of sedatives required. Future research should explore the effectiveness of these interventions in pediatric settings to establish evidence-based guidelines for practice.
Conclusion
This study indicates a significant association between anxiety severity and the need for additional doses of Propofol in children undergoing UGE. The findings underscore the importance of addressing anxiety in pediatric patients to enhance procedural safety and comfort. Further research is essential to investigate effective strategies for anxiety management in this vulnerable population.
Ethical Considerations
Compliance with ethical guidelines
The study obtained ethical approval from the Research Ethics Committee of Shahid Sadouqi University of Medical Sciences, Yazd, Iran (Code: IR.SSU.MEDICINE.REC.1400.419). Informed consent was obtained from the parents or legal guardians of all participating children. The study adhered to ethical guidelines and regulations, ensuring the confidentiality and privacy of the participants.
Funding
This study was extracted from the general medical doctorate thesis of Fateme Pourshamsi, approved by the School of Medicine, Shahid Sadouqi University of Medical Sciences, Iran, Yazd.
Authors contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflicts of interest
The authors declared no conflict of interest.
References
Upper gastrointestinal endoscopy (UGE) is an invasive diagnostic-therapeutic procedure commonly employed for the evaluation and management of gastrointestinal disorders. Its utilization in pediatric patients has significantly increased in recent decades [1]. However, this procedure can induce anxiety and fear in both children and their parents [2, 3]. Compared to adults, children are more susceptible to anxiety due to their limited emotional and behavioral development [4].
The advancement and availability of endoscopic technology, coupled with the growing number of endoscopy centers, have led to the widespread use of sedation techniques to enhance patient comfort during the procedure. Intravenous sedation is commonly administered to alleviate anxiety, pain, and discomfort associated with the diagnostic-therapeutic process. However, despite the implementation of intravenous sedation, it may not effectively address pre-endoscopy anxiety in pediatric patients [5].
The significance of preventing and mitigating severe anxiety during medical interventions extends beyond patient comfort, as it can also positively impact procedure duration and minimize potential side effects [3, 6, 7].
Understanding the interplay between anxiety severity and sedation requirements enhances procedural safety and contributes to the development of targeted interventions aimed at alleviating pre-procedural anxiety in children. Thus, further research in this area is essential to establish evidence-based guidelines that can enhance UGE efficacy and safety in pediatric populations.
Methods
This analytical cross-sectional observational study was conducted at Shahid Sadouqi Medical Education Hospital in Yazd City, Iran, from September 2022 to May 2023. The study included children aged 3-7 years who were scheduled for outpatient upper endoscopy.
Inclusion and exclusion criteria
The inclusion criteria were children aged 3-7 years who required elective diagnostic UGE on an outpatient basis, as determined by a pediatric gastroenterology specialist. Meanwhile, children with a history of upper gastrointestinal surgery, previous or recent endoscopy, psychiatric disorders or diseases, anticipated airway problems, allergies to propofol, concurrent treatment during endoscopy, significant systemic illness, mental retardation, and neurodevelopmental delays were excluded from the study.
A total of 50 children were included in the study, according to the sample size determined. The sample size was determined based on a power analysis aiming for 80% power to detect significant differences with a significance level of 0.05. Meanwhile, data collection involved the following procedures.
Pre-endoscopy assessment
Before performing UGE, adherence to fasting guidelines is essential. As per the American Society of Anesthesiologists (ASA), patients should fast for a minimum of 2 h after consuming clear liquids and 6 hours after consuming light meals [8]. The demographic information of the children, including age and gender, was recorded.
Anxiety assessment
Upon arrival at the endoscopy department, the child was directed to the waiting room. Before any treatment procedures, the nurse provided the parents with the preschool anxiety score questionnaire in Persian for completion. The preschool anxiety score questionnaire demonstrates good reliability (0.73 to 0.82) and validity (0.41 to 0.67). In the present study, the Cronbach α coefficient was calculated to be above 0.7 [9]. The questionnaire comprises scores ranging from zero (minimum) to 112 (maximum). Scores between 0-36 indicate low anxiety levels, 37-75 indicate moderate anxiety levels, and scores exceeding 75 indicate high anxiety levels.
Sedation protocol
Before entering the endoscopy room, an intravenous catheter was inserted in the right forearm to facilitate the infusion of 0.9% saline to maintain vein patency. All patients were equipped with a pulse oximeter, a three-lead electrocardiogram, and a non-invasive blood pressure cuff, following which the patient was positioned on their left side, and supplemental oxygen was administered via a nasal cannula. In this study, propofol was the sole sedative used for children, with an initial dose of 2 mg/kg and additional doses of 0.5 mg/kg administered every 3-5 min until deep sedation was achieved. Deep sedation, as required for endoscopy, was determined by assessing the level of consciousness using the University of Michigan sedation scale (UMSS) [10]. The UMSS is an observational tool that ranges from 5 (fully awake) to 4 (unexcitable). For this study, a UMSS score of 3 or 4 was necessary. If deep sedation was not achieved, an additional dose of propofol was administered and documented in the patient’s record. No other medications, including analgesics, were employed in this study. The entire sedation process was conducted by an anesthesiologist who was unaware of the anxiety scores before the endoscopy. Any sedation-related complications, including oxygen saturation <90%, hiccups, snoring, restlessness, and decreased respiratory rate, were recorded.
Endoscopy procedure
The endoscopy procedure was performed by one pediatric gastroenterologist following standard protocols. The duration of the procedure was recorded.
Data analysis
The collected data were analyzed using the SPSS software, version 27. Appropriate statistical tests, including chi-square and t-tests, were employed to perform comparisons. A significance level of P<0.05 was used, indicating statistical significance.
Results
In this study, a total of 50 children (23 boys and 27 girls) aged between 3 to 7 years, with a mean age of 5±2.3 years and 1 month, underwent diagnostic UGE. The main objective was to assess the severity of anxiety among these children (Table 1).
The anxiety scores ranged from 20 to 105, with a mean score of 57.7. Out of the 50 children, 18(36%) exhibited low anxiety levels, 20(40%) showed moderate anxiety levels, and 12(24%) experienced high anxiety levels. Statistical analysis revealed no significant correlation between anxiety levels and age groups (P=0.20; Table 2).
In terms of gender distribution, out of the total sample of 50 children, 23(46%) were boys and 27(54%) were girls. However, no significant relationship was found between the intensity of anxiety and the gender of the children (P=0.766).
Among the 50 children, 30 cases received an additional dose of propofol during the procedure. Out of these 30 cases, 5(10%) had low anxiety, 13(26%) had moderate anxiety, and 12(24%) experienced severe anxiety. A significant association was observed between the anxiety intensity and the requirement for an extra dose of propofol (P<0.001). Restlessness during endoscopy was reported in 30 patients. There was a significant correlation between the intensity of anxiety and the occurrence of irritability during the procedure (P<0.001).
The minimum duration of the endoscopy procedure was 1 minute, while the maximum duration reached 10 min, with a mean duration of 3.66 min. Notably, a statistically significant relationship was found between the intensity of anxiety and the duration of the endoscopy procedure (P=0.027). Specifically, the mean duration of endoscopy for cases with high anxiety intensity was recorded as 4.95±1.95 min, indicating a slightly longer duration compared to other levels of anxiety intensity.
The recovery time after the procedure varied between 5 and 40 min, with a mean recovery time of 20.2±8.4 min. There was a significant association between the intensity of anxiety and the recovery time (P=0.048). Specifically, the mean recovery time for children with high anxiety was 29.72±6.84.
Among the complications associated with sedation, restlessness was the most common, occurring in 19 cases (57.57%). Other complications included a reduction in SPO2 in 7 cases (21.21%), snoring in 5 cases (15.15%), and hiccups in 2 cases (6.07%). Notably, none of the children in this study experienced a decrease in the respiratory rate. Significant relationships were observed between the effects of sedation and the intensity of children’s anxiety, as well as the administration of an additional dose of propofol (P of 0.001 and <0.001, respectively). Specifically, restlessness and hiccups were significantly associated with the intensity of anxiety (P of 0.006 and 0.037, respectively). However, no significant relationships were found between SPO2 reduction, snoring, and the intensity of anxiety (P of 0.183 and 0.083, respectively).
Discussion
This study evaluated the relationship between anxiety severity and the dosage of sedative medication required for children undergoing UGE. The findings demonstrate a significant association between pre-endoscopy anxiety levels and the need for additional doses of Propofol, as well as the duration of the procedure, recovery time, and sedation-related complications.
The results indicated that higher anxiety levels were correlated with an increased requirement for additional doses of propofol. This finding aligns with previous studies that suggest children with elevated anxiety require more sedation to achieve the desired level of comfort during invasive procedures [1]. Notably, our results highlight the critical role that anxiety management can play in optimizing sedation protocols, potentially reducing the need for higher medication doses.
Additionally, this study found a significant relationship between anxiety intensity and both the duration of the endoscopy and the recovery time. Children with high anxiety experienced more prolonged procedures and extended recovery periods. This is consistent with research indicating that anxiety can prolong medical interventions, leading to increased patient discomfort and resource utilization [11]. Understanding this relationship emphasizes the importance of addressing anxiety proactively to enhance procedural efficiency.
Restlessness was the most frequently reported sedation-related complication, and this analysis showed a significant correlation between anxiety levels and the incidence of restlessness during the procedure. This supports findings from similar studies indicating that anxious patients are more likely to experience adverse effects from sedation [8]. The implications of these findings suggest that by mitigating anxiety, we may also reduce the occurrence of such complications, ultimately improving the overall experience for pediatric patients.
While this study focused on a pediatric population, it is essential to acknowledge that much of the existing literature on anxiety and sedation in endoscopic procedures has centered around adults. This gap highlights the need for more targeted research in children to develop age-appropriate interventions. For instance, studies involving adult cohorts, such as those by Osborn et al. (2004) [12], have shown varying associations between anxiety and sedation requirements, underscoring the need for pediatric-specific insights.
The findings of this study suggest that implementing anxiety-reducing interventions before endoscopy could be beneficial. Various techniques, such as pre-procedural counseling, play therapy, or the use of calming music, may help lower anxiety levels and, consequently, reduce the dosage of sedatives required. Future research should explore the effectiveness of these interventions in pediatric settings to establish evidence-based guidelines for practice.
Conclusion
This study indicates a significant association between anxiety severity and the need for additional doses of Propofol in children undergoing UGE. The findings underscore the importance of addressing anxiety in pediatric patients to enhance procedural safety and comfort. Further research is essential to investigate effective strategies for anxiety management in this vulnerable population.
Ethical Considerations
Compliance with ethical guidelines
The study obtained ethical approval from the Research Ethics Committee of Shahid Sadouqi University of Medical Sciences, Yazd, Iran (Code: IR.SSU.MEDICINE.REC.1400.419). Informed consent was obtained from the parents or legal guardians of all participating children. The study adhered to ethical guidelines and regulations, ensuring the confidentiality and privacy of the participants.
Funding
This study was extracted from the general medical doctorate thesis of Fateme Pourshamsi, approved by the School of Medicine, Shahid Sadouqi University of Medical Sciences, Iran, Yazd.
Authors contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflicts of interest
The authors declared no conflict of interest.
References
- Gürbulak B, Üçüncü MZ, Yardımcı E, Kırlı E, Tüzüner F. Impact of anxiety on sedative medication dosage in patients undergoing esophagogastroduodenoscopy. Wideochir Inne Tech Maloinwazyjne. 2018; 13(2):192-8. [DOI:10.5114/wiitm.2018.73594] [PMID]
- Bay C, Henriquez R, Villarroel L, Gana JC. Effect of music on pediatric endoscopic examinations: A randomized controlled trial. Endosc Int Open. 2021; 9(4):E599-605.[DOI:10.1055/a-1352-3244] [PMID]
- Riddhiputra P, Ukarapol N. Effect of systematic psychological preparation using visual illustration prior to gastrointestinal endoscopy on the anxiety of both pediatric patients and parents. J Med Assoc Thai. 2006; 89(2):231-5. [PMID]
- Lee JH, Jung HK, Lee GG, Kim HY, Park SG, Woo SC. Effect of behavioral intervention using smartphone application for preoperative anxiety in pediatric patients. Korean J Anesthesiol. 2013; 65(6):508-18. [DOI:10.4097/kjae.2013.65.6.508] [PMID]
- Khiani VS, Soulos P, Gancayco J, Gross CP. Anesthesiologist involvement in screening colonoscopy: Temporal trends and cost implications in the medicare population. Clin Gastroenterol Hepatol. 2012 ; 10(1):58-64.e1. [DOI:10.1016/j.cgh.2011.07.005] [PMID]
- Kara D, Bayrak NA, Volkan B, Uçar C, Cevizci MN, Yildiz S. Anxiety and salivary cortisol levels in children undergoing esophago-gastro-duodenoscopy under sedation. J Pediatr Gastroenterol Nutr. 2019; 68(1):3-6. [DOI:10.1097/MPG.0000000000002142] [PMID]
- Ersöz F, Toros AB, Aydoğan G, Bektaş H, Ozcan O, Arikan S. Assessment of anxiety levels in patients during elective upper gastrointestinal endoscopy and colonoscopy. Turk J Gastroenterol. 2010; 21(1):29-33. [DOI:10.4318/tjg.2010.0044] [PMID]
- Sargın M, Uluer M. The effect of pre-procedure anxiety on sedative requirements for sedation during upper gastrointestinal endoscopy. Turk J Surg. 2020;36(4):368-73. [DOI:10.47717/turkjsurg.2020.4532] [PMID]
- Ghanbari S, Khan Mohammadi M, Khodapanahi MK, Mazaheri MA, Gholamali Lavasani M. [Investigating the psychometric properties of the Preschool Children Anxiety Scale (Persian)]. J Psychol. 2011; 15(3):222-34. [Link]
- Malviya S, Voepel-Lewis T, Tait AR, Merkel S, Tremper K, Naughton N. Depth of sedation in children undergoing computed tomography: Validity and reliability of the University of Michigan Sedation Scale (UMSS). Br J Anaesth. 2002; 88(2):241-5. [DOI:10.1093/bja/88.2.241] [PMID]
- Hekimoğlu Şahin S, Çopuroğlu E, Yamak Altınpulluk E, Süt N, Karamanlıoğlu B, Elter K, et al. Effect of preoperative anxiety on depth of anaesthesia and in vitro fertilization success. Turk J Anaesthesiol Reanim. 2023; 51(5):414-9. [DOI:10.4274/TJAR.2023.22829] [PMID]
- Osborn TM, Sandler NA. The effects of preoperative anxiety on intravenous sedation. Anesth Prog. 2004; 51(2):46-51. [PMID]
Type of Study: Original Article |
Received: 2025/01/2 | Accepted: 2025/03/3 | Published: 2025/04/1
Received: 2025/01/2 | Accepted: 2025/03/3 | Published: 2025/04/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |