Volume 13, Issue 1 (1-2025)
J. Pediatr. Rev 2025, 13(1): 49-56 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Seraji M, Zahmatkeshan M, Momenabadi V, Nejadsadeghi E. Prioritizing Factors Affecting Obesity-prevention Behaviors in Preschoolers, Based on Social Cognitive Theory. J. Pediatr. Rev 2025; 13 (1) :49-56
URL: http://jpr.mazums.ac.ir/article-1-625-en.html
URL: http://jpr.mazums.ac.ir/article-1-625-en.html
1- Health Promotion Research Center, Zahedan University of Medical Sciences, Zahedan, Iran.
2- Noncommunicable Diseases Research Center, Fasa University of Medical Sciences, Fasa, Iran. & Department of Health Information Management, School of Allied Medical Sciences, Fasa University of Medical Sciences, Fasa, Iran.
3- Department of Public Health, School of Health, Bam University of Medical Sciences, Bam, Iran.
4- Department of Public Health, Behbahan Faculty of Medical Sciences, Behbahan, Iran. ,n.sadeghiel1358@yahoo.com
2- Noncommunicable Diseases Research Center, Fasa University of Medical Sciences, Fasa, Iran. & Department of Health Information Management, School of Allied Medical Sciences, Fasa University of Medical Sciences, Fasa, Iran.
3- Department of Public Health, School of Health, Bam University of Medical Sciences, Bam, Iran.
4- Department of Public Health, Behbahan Faculty of Medical Sciences, Behbahan, Iran. ,
Full-Text [PDF 401 kb]
(765 Downloads)
| Abstract (HTML) (1829 Views)
Full-Text: (680 Views)
Introduction
The prevalence of obesity in children around the world is increasing due to lifestyle changes and is expected to reach 70 million children by 2025 [1]. Overweight and obesity among children in Iran have become a public health concern [2-5]. In a study on 2637912 individuals aged 2-15 years, the overall prevalence of obesity in Iranian children was 11.4% [6]. The results of a study that investigated the body mass index (BMI) of under-5 children in 27 provinces of Iran in 2008 showed that the prevalence rates of overweight and obesity in children in rural and urban areas were 6.5% and 7.1%, respectively [7]. In Iran, in the last decade, the prevalence of overweight and obesity in children under 5 years of age has doubled [8]. Also, 6.7% to 10% of all 4-6 years old children living in Behbahan City, Iran, in 2016 were obese and overweight, respectively [9]. In 2010, the overall prevalence rates of obesity and overweight in primary school students in Behbahan were 9.3% and 12.1%, respectively [10].
Childhood obesity has become a global epidemic with medical, psychological, and economic consequences. Overweight and obesity can affect and reduce the quality of life of children [11, 12].
Being overweight during childhood significantly predisposes people to obesity during adulthood [11]. Research shows a close relationship between childhood and adulthood obesity because eating habits are established in the early years of life and continue for the rest of life [12]. Childhood obesity continues into adulthood, and more than 69% of 6-10 years old obese children will become obese adults [13]. In other words, the prevalence of adult obesity in obese children is 2 to 3 times that of non-obese children [5].
Overweight and obesity are largely preventable [4]. Numerous medical, social, and psychological complications of obesity in children and the heavy burden that it imposes on society highlight the need to control and prevent obesity in children [5]. Obesity is recognized as a health priority, and behavioral corrections are needed to resolve it. Changing health behaviors is the best way to reduce illness mortality and improve the quality of life [14]. The experts committee of American Medical Association (AMA) has identified four key lifestyle behaviors that prevent obesity and overweight in children and adolescents, which include replacing sugary drinks (such as artificial juices, fizzy drinks, etc.) with sugar-free drinks (such as water, yogurt drinks, natural fruit juices, and so on.), daily consumption of 5 units of fruits and vegetables, doing at least 60 minutes of physical exercise per day, and reducing sedentary activities (screen) for less than 2 hours per 60 day [15].
The family environment is the first environment that affects the obesity of children, and understanding this effect can help prevent and treat obesity [16, 17]. Parents are an important factor in changing children’s behavior. There is convincing evidence that the family environment plays an important role in children’s obesity-related behaviors. In a systematic review, it has been shown that the family environment is an effective factor in consuming fruits and vegetables, ready meals, soft drinks and fatty foods [18]. Another study showed the effect of direct parental support on the physical activity of children and adolescents [19]. Among family members, the role of mothers in shaping children’s behavioral patterns, such as eating habits and physical activity, is crucial [19].
The cognitive social theory is one of the most efficient theories that predict and explain eating behaviors, especially in children [20]. This theory has been used successfully in examining eating behaviors such as replacing water with fizzy drinks and eating fresh fruits and vegetables [21]. The cognitive social theory is the most common theory used in childhood obesity [22].
Also, among the various behavioral predictors, the constructs of cognitive-social theory have been identified as important determinants of obesity-preventing behaviors [23].
The first important step in planning and designing intervention is problem identification. In determining a problem, it should be identified correctly because improper identification of the problem can lead to the presentation of wrong solutions [24]. According to the research, the present study is the first of its kind, and so far, no research has been done on the prioritization of constructs of cognitive social theory that affect obesity prevention behaviors in 4-6 years of children. Therefore, the present study was conducted to prioritize the constructs of social cognitive theory affecting obesity prevention behaviors in 6-4 years old children from the mothers’ point of view. The findings of this study will help primary care providers and family physicians to have a prioritized framework for family education, especially mothers, in the field of obesity prevention behaviors in children. Hopefully, this study will lead to a better role for primary care doctors and improve their performance quality.
Methods
This cross-sectional study was conducted on 240 children aged 4-6 years living in Behbahan City, Iran, in 2016. A random multi-stage sampling method was used in this study. In the first stage, out of 20 kindergartens in Behbahan, 4 were randomly selected. Then, 60 children aged 4-6 years were randomly selected from each kindergarten. The sample size was calculated with 90% test power and 5% Type I error. The selected 240 children had no health problems according to the children’s health records in the kindergartens. The mothers of the children completed the questionnaires after obtaining their informed consent. Data collection tools consisted of a demographic form and a questionnaire based on social cognitive theory constructs derived from the childhood health program measurement instrument designed by Adam Knowlden et al. [25]. The questionnaire based on social cognitive theory (constructs (environment, outcome expectation, emotional coping, self-control, and self-efficacy) consisted of 4 obesity-prevention behaviors in children, with 64 questions scored on a 5-point Likert-type scale from 0 to 4. This questionnaire was approved by 10 panel members specialized in health education and promotion, yielding a content validity ratio of 0.81 and a content validity index of 0.94. The validity of constructs was also assessed by factor analysis, in which the reagents selected to measure each concept had a desirable and significant factor load. To measure the reliability of the questionnaire in a preliminary study, the Cronbach α coefficient was calculated by interviewing 30 mothers. The internal correlation for each social cognitive theory construct was higher than 0.7. The data analysis was performed using the Friedman test by SPSS software, version 23.
Results
Of 240 participating children, 133(55.4%) were boys and 107(44.6%) were girls. The Mean±SD age of children was 5.13±0.68 years.
Prioritizing the constructs of social-cognitive theory related to physical activity behavior
Prioritizing the constructs of social cognitive theory related to physical activity behavior the value of Friedman test (χ2=288.485) is significant at the error level of <0.01. It should be noted that, with a confidence interval of 0.99, there was a significant difference between the effect of constructs on the behavior of physical activity. According to the results, the average effect of the “outcome expectation” construct was 4.38, which showed the highest effect (Table 1).
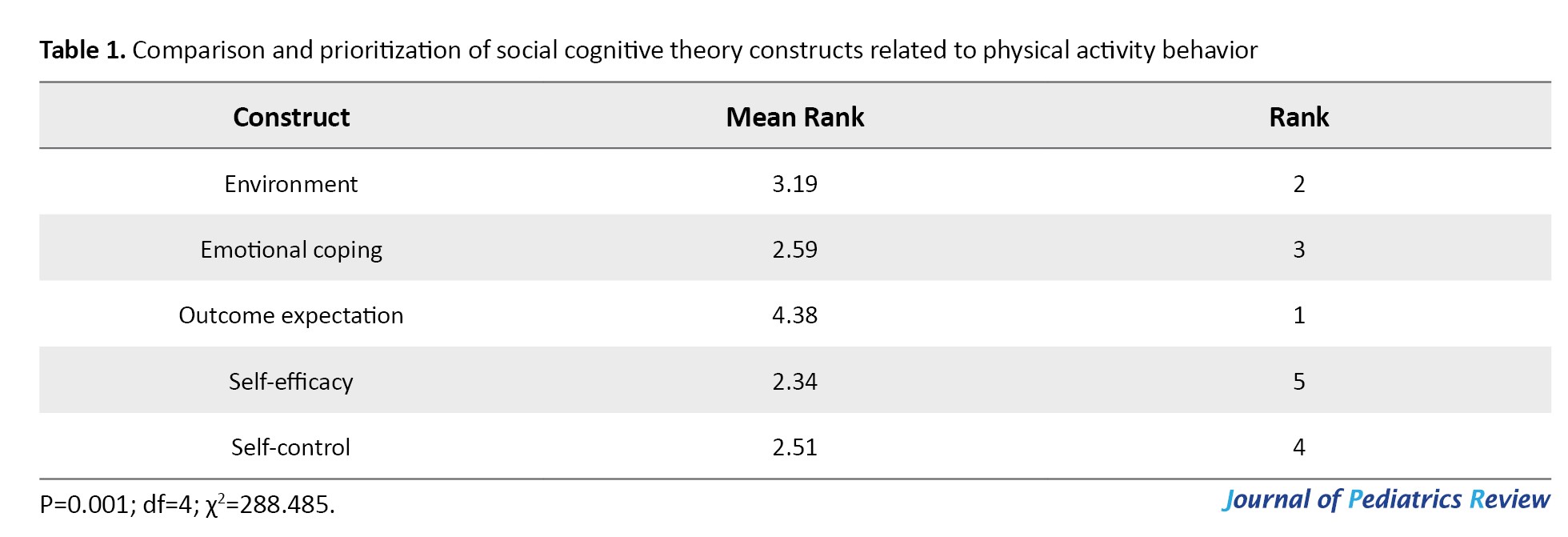
Also, the average effect of “self-efficacy” construct was 2.34, which showed the lowest effect among the factors affecting physical activity behavior (Table 2).
Environment emotional coping outcome expectation self-efficacy
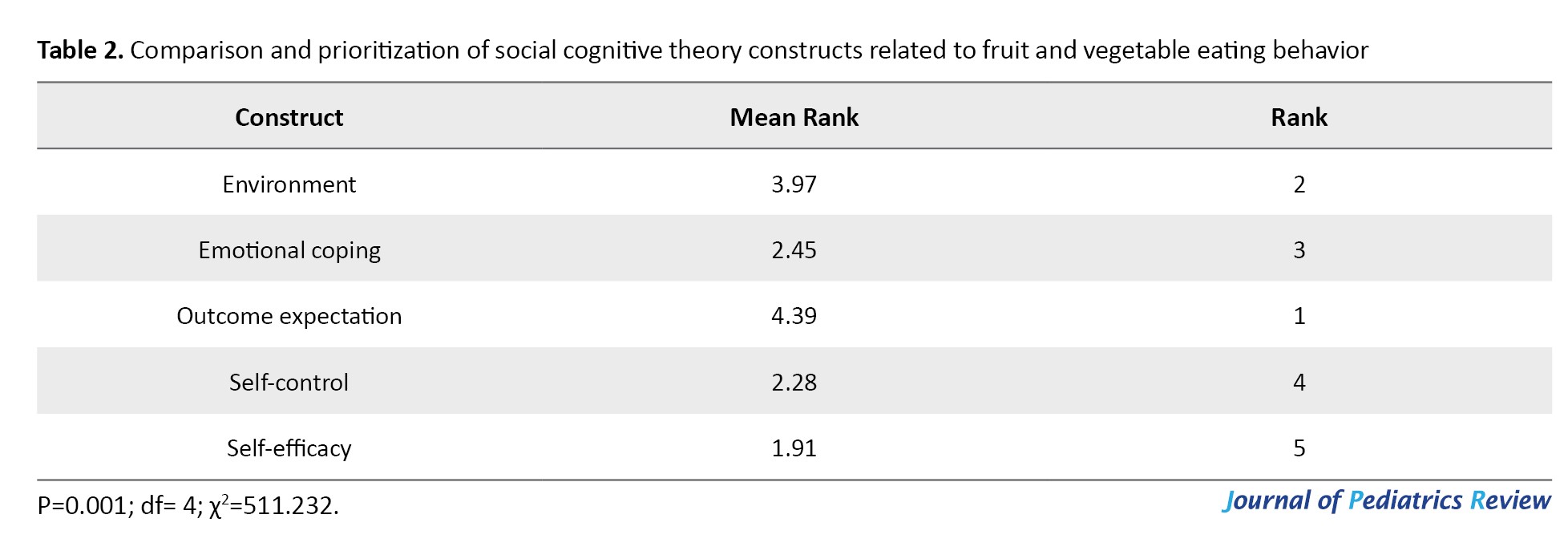
Prioritizing the constructs of social-cognitive theory related to eating fruit and vegetable behavior
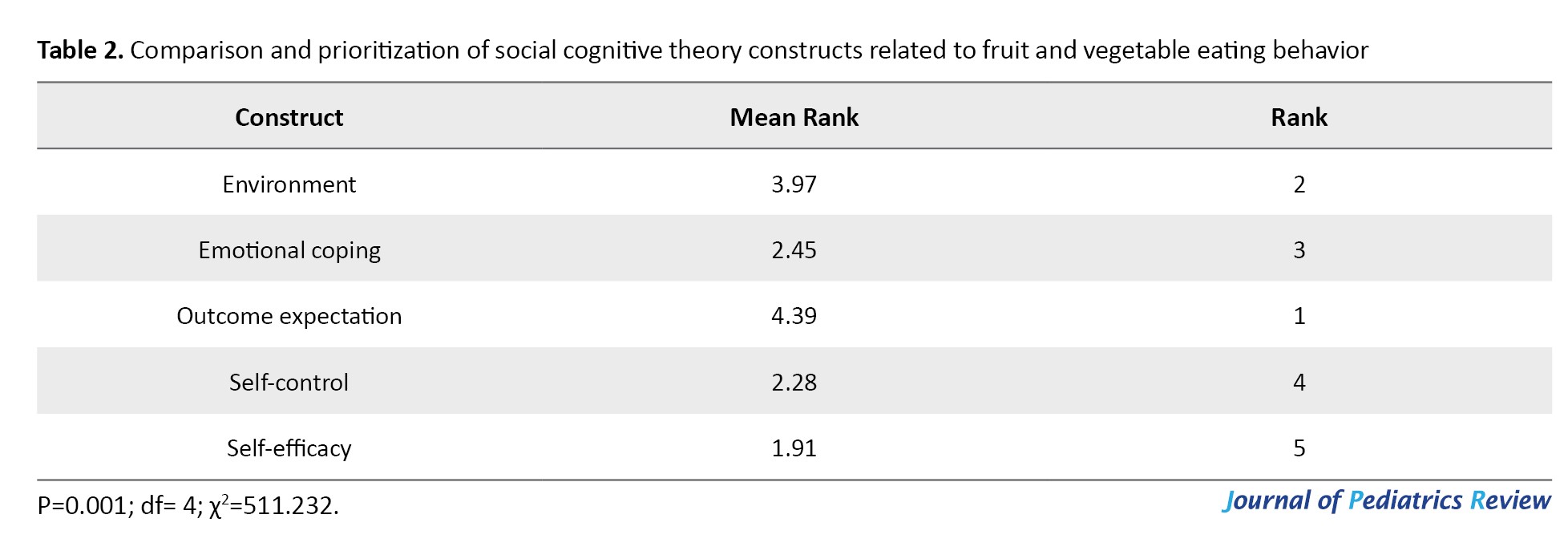
Prioritizing the constructs of social cognitive theory related to eating fruit and vegetables considering the value of the Friedman test (χ2=511.232), which is significant at the error level of <0.01, it should be said that, with the confidence interval of 0.99, there was a significant difference between the effect of constructs on fruit and vegetable eating behavior. According to the results obtained from Table 2, the average effect of the “outcome expectation “construct was 4.39, which showed the highest effect among the factors affecting fruit and vegetable eating behavior. Also, the average “self-efficacy” construct effect was 1.91, which showed the lowest effect among the factors affecting fruit and vegetable eating behavior (Table 2).
Prioritizing the constructs of social cognitive theory related to consumption of sugar-free drinks
Given the value of the Friedman test (χ2=246.460), which is significant at the error level of <0.01, it should be noted that, with the confidence interval of 0.99, there was a significant difference between the effect of constructs on the behavior of consuming sugar-free drinks. According to the results, the average effect of the “outcome expectation” construct was 4.25, which showed the highest effect among the factors affecting the behavior of consuming sugar-free drinks (Table 3).

Also, the average effect of the “self-efficacy” construct was 2.46, which showed the lowest effect among the factors affecting the behavior of consuming sugar-free drinks (Table 3).
Prioritizing the constructs of social cognitive theory related to screen behavior
Considering the value of the Friedman test (χ2=316.137), which is significant at the error level of less than 0.01, it should be noted that, with a confidence interval of 0.99, there was a significant difference between the effect of constructs of screening behavior. According to the results obtained from Table 4, the average effect of the “outcome expectation” construct was 4.19, which showed the highest effect among the factors affecting screen behavior.
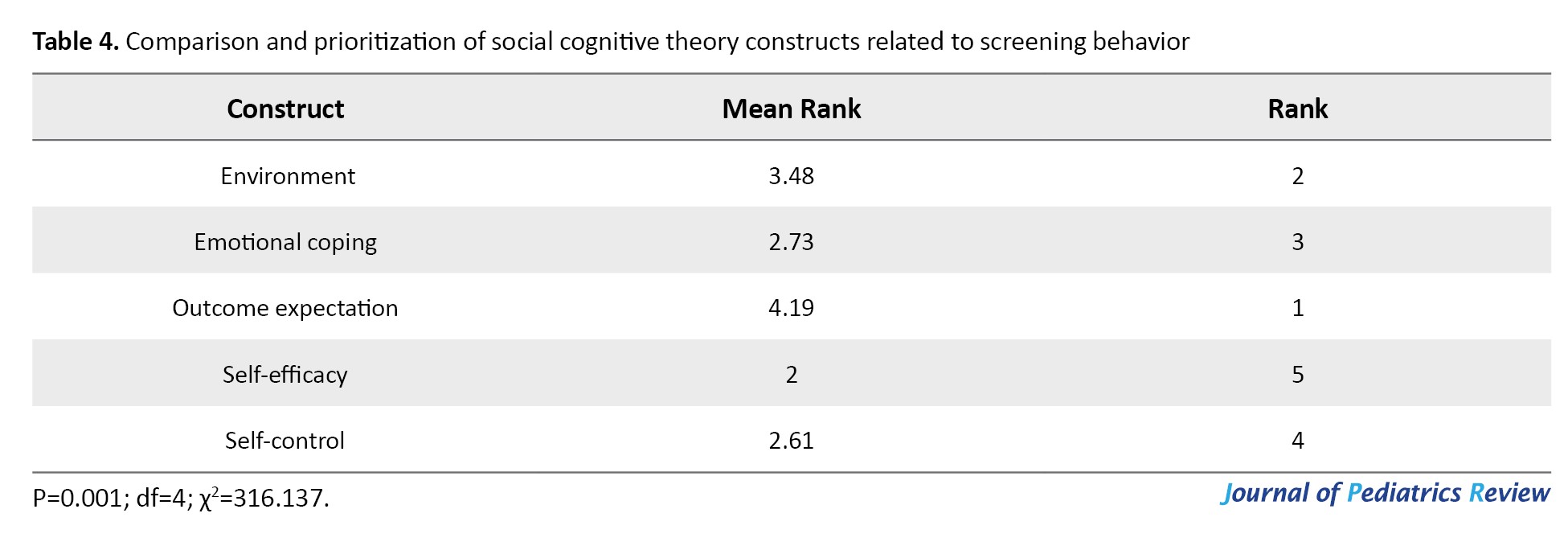
Also, the average effect of the “self-efficacy” construct was 2, which showed the lowest effect among the factors affecting screen behavior (Table 4).
Discussion
Due to the increasing prevalence of childhood obesity, its prevention is desirable. According to studies, cognitive social theory constructs effectively prevent obesity behaviors [20, 21, 26-30]. So far, no study has prioritized the constructs of cognitive social theory that affect obesity-prevention behaviors in children aged 4-6 years. For health policymakers and planners, prioritizing the constructs is important because it provides the structure and guidance for designing proper interventions. Moreover, the extension and design of intervention without prioritizing influential factors leads to its failure. Ignoring need assessment leads to interventions’ failure because decisions about interventions’ design are directly related to critical factors. It is clear that special attention needs to be paid to identifying the factors that influence obesity prevention to avoid the consequences and costs of improper preventive interventions. The present study was conducted to answer this question: “What is the ranking and importance of social cognitive theory constructs that affect the prevention of childhood obesity from the mothers’ point of view?”
Knowing this ranking can be a practical step toward successfully implementing relevant interventions. Unsuccessful implementation of interventions is an issue that threatens the effectiveness of interventions. On the other hand, making rational and wise decisions guarantees the long-term effectiveness of interventions. Health managers should make correct decisions about obesity factors and prioritize their decisions about obesity-prevention interventions because knowing the key variables will help them better manage these variables to improve children’s health. Knowledge of these key factors will increase the predictability of decisions made by healthcare managers and policymakers. Given the limitations of financial resources in health systems, especially in developing countries, it is necessary to identify the most important constructs that affect obesity prevention behaviors. The present study was conducted for this purpose, and we hope it will help planners determine the best strategies.
According to the results of the present study, from the mothers’ point of view, the most important construct of social cognitive theory that affects all 4 obesity-prevention behaviors in 4-6 years old children was the “outcome expectation” construct. This finding confirms that mothers, to promote obesity prevention behaviors in their children, viewed awareness of the desired consequences of their children’s involvement in these behaviors as an important factor. Therefore, to increase obesity-prevention behaviors in 4-6 years old children through the framework of social cognitive theory, adjusting the “outcome expectation” construct is the priority. By motivating mothers to understand the positive consequences of their children’s obesity-prevention behaviors and creating higher-level expectations in them, mothers are more likely to take action to manage their children’s obesity-related behaviors [31]. This finding is consistent with the results of Knowlden et al. [25] and Zolghadr [32] studies.
This study showed that from the mothers’ point of view, in all 4 obesity prevention behaviors in children aged 4-6 years, the environment construct had the second priority. In other words, mothers consider the physical condition surrounding their children very important in preventing obesity. Therefore, to promote obesity-prevention behaviors in 4-6 years old children through the framework of social-cognitive theory, the second priority is modification of the environment construct. Consequently, mothers can develop obesity-prevention behaviors in their children by creating opportunities to overcome obstacles in real-life conditions and creating learning experiences to motivate them to continue their obesity-prevention behaviors. These findings are consistent with the results of a study by Knowlden et al. [25].
Our study showed that from the mothers’ perspective, to increase the behaviors of physical activity and consumption of fruits and vegetables and reduce screening behavior in children, the constructs of “emotional coping” and “goal adjustment” have the third and fourth priority, respectively. However, to increase the behavior of consuming sugar-free drinks in children, the construct of “goal adjustment” has the third priority, and “emotional coping” is the fourth priority. Therefore, to improve the behaviors of physical activity and consumption of fruits and vegetables and reduce screening behavior in children aged 4-6 years through the framework of social cognitive theory, the construct of “emotional coping” has the third priority. In other words, mothers consider it more important for their children to manage and control the emotional and physiological states associated with performing these behaviors than to set goals and create programs to facilitate them. However, the behavior of consuming sugar-free drinks is quite the opposite. Therefore, maternal-centered interventions for preventing obesity in children aged 4-6 years must include techniques for managing children’s emotional and physiological states and skills to regulate goals, monitor progress, and reinforce behavior.
According to the present study, from the mothers’ point of view, the construct of “self-efficacy,” which is the confidence in the ability to follow the behaviors that prevent obesity in children, had the lowest priority. In other words, mothers, to facilitate the prevention of obesity in their children, consider other constructs to be of higher priority than the construct of “self-efficacy.”
It is suggested that primary care providers and family doctors educate the family, especially mothers, in the field of obesity-prevention behaviors in children based on the findings of this research.
The present study is very limitless and noticeable in many ways. This study was conducted in a small geographical area and on a relatively small number of mothers. So, the results of this study can be tested by surveying mothers in different geographical areas, and the results can be assessed. In this study, fathers could not participate, so it is suggested that they participate in other studies. The subject of the present study has a high potential for follow-up and development in future research.
Conclusion
Ignoring the issues of obesity policies and interventions is associated with an increase in the prevalence of obesity, which is at the forefront of prevention programs in terms of relevance and related complications. Reversing the rise of childhood obesity requires the development and evaluation of intervention programs. Policymakers and planners across the country play an important role in combating obesity because of their ability to create policies and programs that affect obesity prevention behaviors. When clarifying a problem, it is important to pay close attention to the indicators, measurements, and other necessary frameworks to make sure that decisions about what is being focused on as a specific problem are made consciously. This study identified and evaluated the most important factors influencing the prevention of obesity in children aged 4-6 years and showed that from the mothers’ point of view, the construct of “outcome expectation” has the highest priority among the constructs of obesity-prevention behaviors in 4-6 years old children. It is hoped that by using the results of this evaluation, we will see the implementation of effective and efficient interventions and, consequently, a reduction in the prevalence of obesity in children aged 4-6 years.
Ethical Considerations
Compliance with ethical guidelines
The Research and Ethics Committee of Tehran University of Medical Sciences, Tehran, Iran approved the study protocol (Code: IR.TUMS.REC.1394.1557).
Funding
The Vice-Chancellor for Research and Technology of Tehran University of Medical Sciences, Tehran, Iran provided the financial resources for this research (Grant No.: 240/1869).
Authors contributions
Conceptualization and study design: Elham Nejadsadeghi; Data analysis and interpretation: Victoria Momenabadi; Statistical analysis: Maryam Zahmatkeshan.Writing the original draft: Maryam Seraji; Review and editing: Elham Nejadsadeghi.
Conflicts of interest
There is no conflict of interest to be declared.
Acknowledgements
The authors would like to express my sincere gratitude to the mothers and children who participated in this study and helped them in this research.
References
The prevalence of obesity in children around the world is increasing due to lifestyle changes and is expected to reach 70 million children by 2025 [1]. Overweight and obesity among children in Iran have become a public health concern [2-5]. In a study on 2637912 individuals aged 2-15 years, the overall prevalence of obesity in Iranian children was 11.4% [6]. The results of a study that investigated the body mass index (BMI) of under-5 children in 27 provinces of Iran in 2008 showed that the prevalence rates of overweight and obesity in children in rural and urban areas were 6.5% and 7.1%, respectively [7]. In Iran, in the last decade, the prevalence of overweight and obesity in children under 5 years of age has doubled [8]. Also, 6.7% to 10% of all 4-6 years old children living in Behbahan City, Iran, in 2016 were obese and overweight, respectively [9]. In 2010, the overall prevalence rates of obesity and overweight in primary school students in Behbahan were 9.3% and 12.1%, respectively [10].
Childhood obesity has become a global epidemic with medical, psychological, and economic consequences. Overweight and obesity can affect and reduce the quality of life of children [11, 12].
Being overweight during childhood significantly predisposes people to obesity during adulthood [11]. Research shows a close relationship between childhood and adulthood obesity because eating habits are established in the early years of life and continue for the rest of life [12]. Childhood obesity continues into adulthood, and more than 69% of 6-10 years old obese children will become obese adults [13]. In other words, the prevalence of adult obesity in obese children is 2 to 3 times that of non-obese children [5].
Overweight and obesity are largely preventable [4]. Numerous medical, social, and psychological complications of obesity in children and the heavy burden that it imposes on society highlight the need to control and prevent obesity in children [5]. Obesity is recognized as a health priority, and behavioral corrections are needed to resolve it. Changing health behaviors is the best way to reduce illness mortality and improve the quality of life [14]. The experts committee of American Medical Association (AMA) has identified four key lifestyle behaviors that prevent obesity and overweight in children and adolescents, which include replacing sugary drinks (such as artificial juices, fizzy drinks, etc.) with sugar-free drinks (such as water, yogurt drinks, natural fruit juices, and so on.), daily consumption of 5 units of fruits and vegetables, doing at least 60 minutes of physical exercise per day, and reducing sedentary activities (screen) for less than 2 hours per 60 day [15].
The family environment is the first environment that affects the obesity of children, and understanding this effect can help prevent and treat obesity [16, 17]. Parents are an important factor in changing children’s behavior. There is convincing evidence that the family environment plays an important role in children’s obesity-related behaviors. In a systematic review, it has been shown that the family environment is an effective factor in consuming fruits and vegetables, ready meals, soft drinks and fatty foods [18]. Another study showed the effect of direct parental support on the physical activity of children and adolescents [19]. Among family members, the role of mothers in shaping children’s behavioral patterns, such as eating habits and physical activity, is crucial [19].
The cognitive social theory is one of the most efficient theories that predict and explain eating behaviors, especially in children [20]. This theory has been used successfully in examining eating behaviors such as replacing water with fizzy drinks and eating fresh fruits and vegetables [21]. The cognitive social theory is the most common theory used in childhood obesity [22].
Also, among the various behavioral predictors, the constructs of cognitive-social theory have been identified as important determinants of obesity-preventing behaviors [23].
The first important step in planning and designing intervention is problem identification. In determining a problem, it should be identified correctly because improper identification of the problem can lead to the presentation of wrong solutions [24]. According to the research, the present study is the first of its kind, and so far, no research has been done on the prioritization of constructs of cognitive social theory that affect obesity prevention behaviors in 4-6 years of children. Therefore, the present study was conducted to prioritize the constructs of social cognitive theory affecting obesity prevention behaviors in 6-4 years old children from the mothers’ point of view. The findings of this study will help primary care providers and family physicians to have a prioritized framework for family education, especially mothers, in the field of obesity prevention behaviors in children. Hopefully, this study will lead to a better role for primary care doctors and improve their performance quality.
Methods
This cross-sectional study was conducted on 240 children aged 4-6 years living in Behbahan City, Iran, in 2016. A random multi-stage sampling method was used in this study. In the first stage, out of 20 kindergartens in Behbahan, 4 were randomly selected. Then, 60 children aged 4-6 years were randomly selected from each kindergarten. The sample size was calculated with 90% test power and 5% Type I error. The selected 240 children had no health problems according to the children’s health records in the kindergartens. The mothers of the children completed the questionnaires after obtaining their informed consent. Data collection tools consisted of a demographic form and a questionnaire based on social cognitive theory constructs derived from the childhood health program measurement instrument designed by Adam Knowlden et al. [25]. The questionnaire based on social cognitive theory (constructs (environment, outcome expectation, emotional coping, self-control, and self-efficacy) consisted of 4 obesity-prevention behaviors in children, with 64 questions scored on a 5-point Likert-type scale from 0 to 4. This questionnaire was approved by 10 panel members specialized in health education and promotion, yielding a content validity ratio of 0.81 and a content validity index of 0.94. The validity of constructs was also assessed by factor analysis, in which the reagents selected to measure each concept had a desirable and significant factor load. To measure the reliability of the questionnaire in a preliminary study, the Cronbach α coefficient was calculated by interviewing 30 mothers. The internal correlation for each social cognitive theory construct was higher than 0.7. The data analysis was performed using the Friedman test by SPSS software, version 23.
Results
Of 240 participating children, 133(55.4%) were boys and 107(44.6%) were girls. The Mean±SD age of children was 5.13±0.68 years.
Prioritizing the constructs of social-cognitive theory related to physical activity behavior
Prioritizing the constructs of social cognitive theory related to physical activity behavior the value of Friedman test (χ2=288.485) is significant at the error level of <0.01. It should be noted that, with a confidence interval of 0.99, there was a significant difference between the effect of constructs on the behavior of physical activity. According to the results, the average effect of the “outcome expectation” construct was 4.38, which showed the highest effect (Table 1).
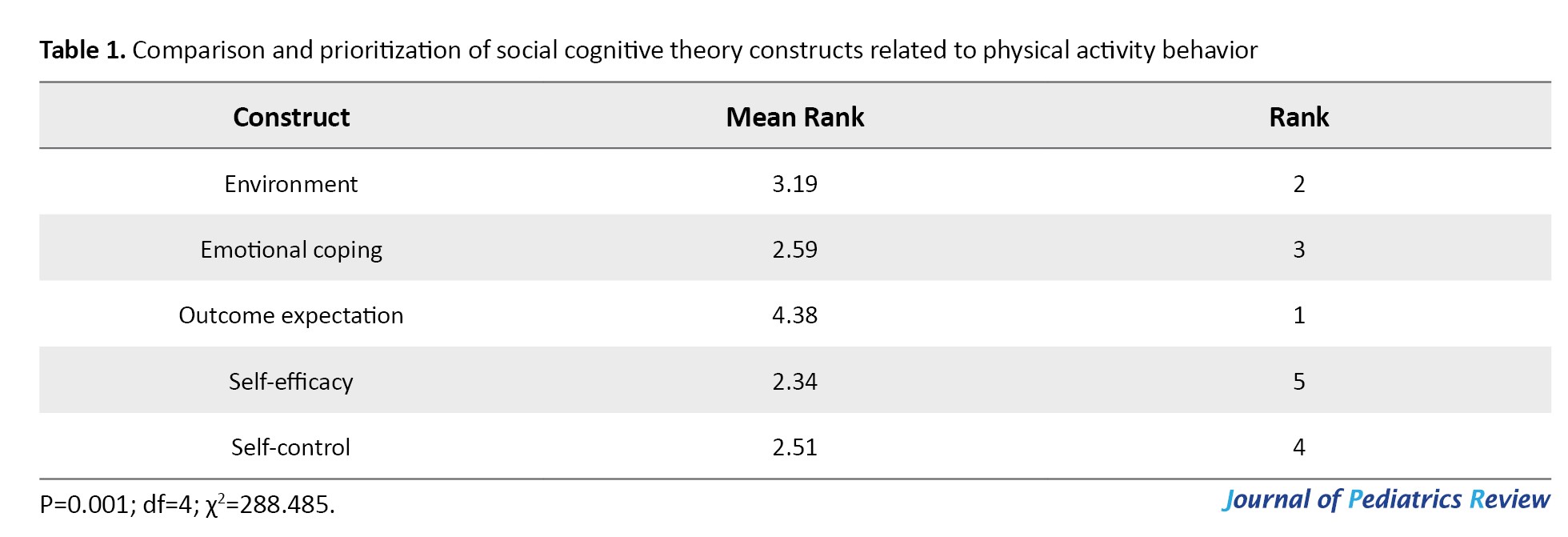
Also, the average effect of “self-efficacy” construct was 2.34, which showed the lowest effect among the factors affecting physical activity behavior (Table 2).
Environment emotional coping outcome expectation self-efficacy
Prioritizing the constructs of social-cognitive theory related to eating fruit and vegetable behavior
Prioritizing the constructs of social cognitive theory related to eating fruit and vegetables considering the value of the Friedman test (χ2=511.232), which is significant at the error level of <0.01, it should be said that, with the confidence interval of 0.99, there was a significant difference between the effect of constructs on fruit and vegetable eating behavior. According to the results obtained from Table 2, the average effect of the “outcome expectation “construct was 4.39, which showed the highest effect among the factors affecting fruit and vegetable eating behavior. Also, the average “self-efficacy” construct effect was 1.91, which showed the lowest effect among the factors affecting fruit and vegetable eating behavior (Table 2).
Prioritizing the constructs of social cognitive theory related to consumption of sugar-free drinks
Given the value of the Friedman test (χ2=246.460), which is significant at the error level of <0.01, it should be noted that, with the confidence interval of 0.99, there was a significant difference between the effect of constructs on the behavior of consuming sugar-free drinks. According to the results, the average effect of the “outcome expectation” construct was 4.25, which showed the highest effect among the factors affecting the behavior of consuming sugar-free drinks (Table 3).

Also, the average effect of the “self-efficacy” construct was 2.46, which showed the lowest effect among the factors affecting the behavior of consuming sugar-free drinks (Table 3).
Prioritizing the constructs of social cognitive theory related to screen behavior
Considering the value of the Friedman test (χ2=316.137), which is significant at the error level of less than 0.01, it should be noted that, with a confidence interval of 0.99, there was a significant difference between the effect of constructs of screening behavior. According to the results obtained from Table 4, the average effect of the “outcome expectation” construct was 4.19, which showed the highest effect among the factors affecting screen behavior.
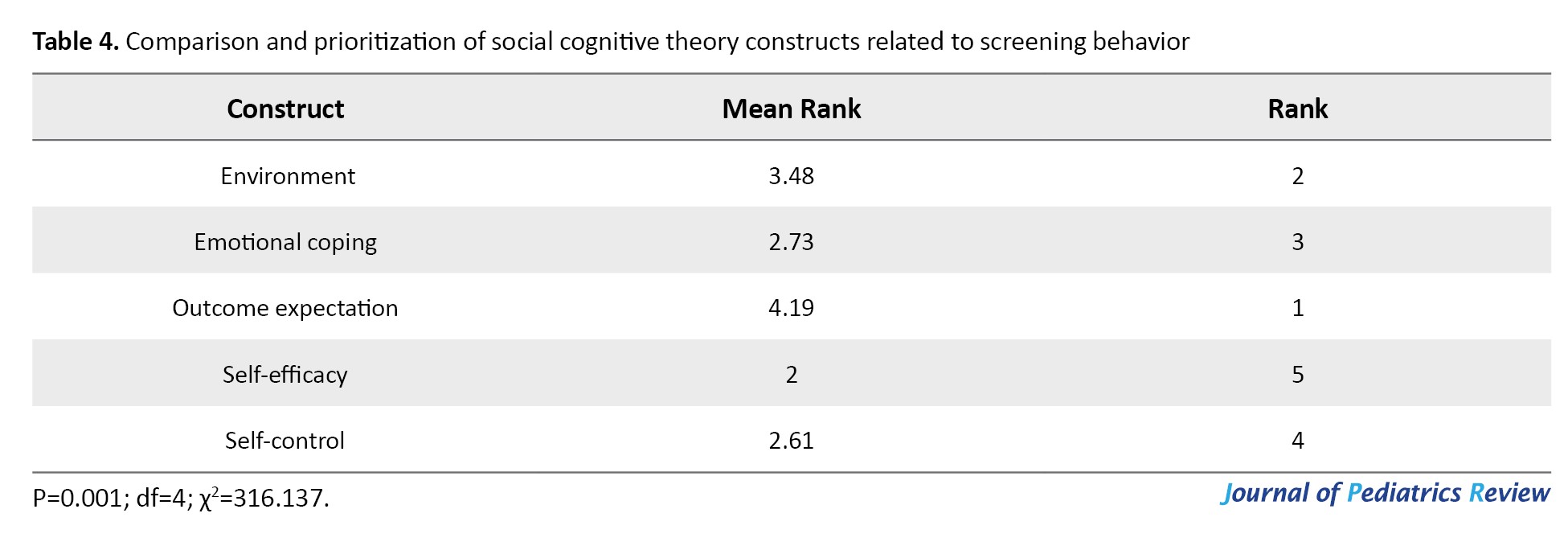
Also, the average effect of the “self-efficacy” construct was 2, which showed the lowest effect among the factors affecting screen behavior (Table 4).
Discussion
Due to the increasing prevalence of childhood obesity, its prevention is desirable. According to studies, cognitive social theory constructs effectively prevent obesity behaviors [20, 21, 26-30]. So far, no study has prioritized the constructs of cognitive social theory that affect obesity-prevention behaviors in children aged 4-6 years. For health policymakers and planners, prioritizing the constructs is important because it provides the structure and guidance for designing proper interventions. Moreover, the extension and design of intervention without prioritizing influential factors leads to its failure. Ignoring need assessment leads to interventions’ failure because decisions about interventions’ design are directly related to critical factors. It is clear that special attention needs to be paid to identifying the factors that influence obesity prevention to avoid the consequences and costs of improper preventive interventions. The present study was conducted to answer this question: “What is the ranking and importance of social cognitive theory constructs that affect the prevention of childhood obesity from the mothers’ point of view?”
Knowing this ranking can be a practical step toward successfully implementing relevant interventions. Unsuccessful implementation of interventions is an issue that threatens the effectiveness of interventions. On the other hand, making rational and wise decisions guarantees the long-term effectiveness of interventions. Health managers should make correct decisions about obesity factors and prioritize their decisions about obesity-prevention interventions because knowing the key variables will help them better manage these variables to improve children’s health. Knowledge of these key factors will increase the predictability of decisions made by healthcare managers and policymakers. Given the limitations of financial resources in health systems, especially in developing countries, it is necessary to identify the most important constructs that affect obesity prevention behaviors. The present study was conducted for this purpose, and we hope it will help planners determine the best strategies.
According to the results of the present study, from the mothers’ point of view, the most important construct of social cognitive theory that affects all 4 obesity-prevention behaviors in 4-6 years old children was the “outcome expectation” construct. This finding confirms that mothers, to promote obesity prevention behaviors in their children, viewed awareness of the desired consequences of their children’s involvement in these behaviors as an important factor. Therefore, to increase obesity-prevention behaviors in 4-6 years old children through the framework of social cognitive theory, adjusting the “outcome expectation” construct is the priority. By motivating mothers to understand the positive consequences of their children’s obesity-prevention behaviors and creating higher-level expectations in them, mothers are more likely to take action to manage their children’s obesity-related behaviors [31]. This finding is consistent with the results of Knowlden et al. [25] and Zolghadr [32] studies.
This study showed that from the mothers’ point of view, in all 4 obesity prevention behaviors in children aged 4-6 years, the environment construct had the second priority. In other words, mothers consider the physical condition surrounding their children very important in preventing obesity. Therefore, to promote obesity-prevention behaviors in 4-6 years old children through the framework of social-cognitive theory, the second priority is modification of the environment construct. Consequently, mothers can develop obesity-prevention behaviors in their children by creating opportunities to overcome obstacles in real-life conditions and creating learning experiences to motivate them to continue their obesity-prevention behaviors. These findings are consistent with the results of a study by Knowlden et al. [25].
Our study showed that from the mothers’ perspective, to increase the behaviors of physical activity and consumption of fruits and vegetables and reduce screening behavior in children, the constructs of “emotional coping” and “goal adjustment” have the third and fourth priority, respectively. However, to increase the behavior of consuming sugar-free drinks in children, the construct of “goal adjustment” has the third priority, and “emotional coping” is the fourth priority. Therefore, to improve the behaviors of physical activity and consumption of fruits and vegetables and reduce screening behavior in children aged 4-6 years through the framework of social cognitive theory, the construct of “emotional coping” has the third priority. In other words, mothers consider it more important for their children to manage and control the emotional and physiological states associated with performing these behaviors than to set goals and create programs to facilitate them. However, the behavior of consuming sugar-free drinks is quite the opposite. Therefore, maternal-centered interventions for preventing obesity in children aged 4-6 years must include techniques for managing children’s emotional and physiological states and skills to regulate goals, monitor progress, and reinforce behavior.
According to the present study, from the mothers’ point of view, the construct of “self-efficacy,” which is the confidence in the ability to follow the behaviors that prevent obesity in children, had the lowest priority. In other words, mothers, to facilitate the prevention of obesity in their children, consider other constructs to be of higher priority than the construct of “self-efficacy.”
It is suggested that primary care providers and family doctors educate the family, especially mothers, in the field of obesity-prevention behaviors in children based on the findings of this research.
The present study is very limitless and noticeable in many ways. This study was conducted in a small geographical area and on a relatively small number of mothers. So, the results of this study can be tested by surveying mothers in different geographical areas, and the results can be assessed. In this study, fathers could not participate, so it is suggested that they participate in other studies. The subject of the present study has a high potential for follow-up and development in future research.
Conclusion
Ignoring the issues of obesity policies and interventions is associated with an increase in the prevalence of obesity, which is at the forefront of prevention programs in terms of relevance and related complications. Reversing the rise of childhood obesity requires the development and evaluation of intervention programs. Policymakers and planners across the country play an important role in combating obesity because of their ability to create policies and programs that affect obesity prevention behaviors. When clarifying a problem, it is important to pay close attention to the indicators, measurements, and other necessary frameworks to make sure that decisions about what is being focused on as a specific problem are made consciously. This study identified and evaluated the most important factors influencing the prevention of obesity in children aged 4-6 years and showed that from the mothers’ point of view, the construct of “outcome expectation” has the highest priority among the constructs of obesity-prevention behaviors in 4-6 years old children. It is hoped that by using the results of this evaluation, we will see the implementation of effective and efficient interventions and, consequently, a reduction in the prevalence of obesity in children aged 4-6 years.
Ethical Considerations
Compliance with ethical guidelines
The Research and Ethics Committee of Tehran University of Medical Sciences, Tehran, Iran approved the study protocol (Code: IR.TUMS.REC.1394.1557).
Funding
The Vice-Chancellor for Research and Technology of Tehran University of Medical Sciences, Tehran, Iran provided the financial resources for this research (Grant No.: 240/1869).
Authors contributions
Conceptualization and study design: Elham Nejadsadeghi; Data analysis and interpretation: Victoria Momenabadi; Statistical analysis: Maryam Zahmatkeshan.Writing the original draft: Maryam Seraji; Review and editing: Elham Nejadsadeghi.
Conflicts of interest
There is no conflict of interest to be declared.
Acknowledgements
The authors would like to express my sincere gratitude to the mothers and children who participated in this study and helped them in this research.
References
- Di Cesare M, Sorić M, Bovet P, Miranda JJ, Bhutta Z, Stevens GA, et al. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019; 17(1):212. [DOI:10.1186/s12916-019-1449-8] [PMID]
- Djalalinia S, Kelishadi R, Qorbani M, Peykari N, Kasaeian A, Nasli-Esfahani E, et al. A systematic review on the prevalence of overweight and obesity, in Iranian children and adolescents. Iran J Pediatr. 2016; 26(3):e2599. [DOI:10.5812/ijp.2599] [PMID]
- Agha-Alinejad H, Farzad B, Salari M, Kamjoo S, Harbaugh BL, Peeri M. Prevalence of overweight and obesity among Iranian preschoolers: Interrelationship with physical fitness. J Res Med Sci. 2015; 20(4):334-41. [PMID]
- Mansori K, Khateri S, Moradi Y, Khazaei Z, Mirzaei H, Hanis SM, t al. Prevalence of obesity and overweight in Iranian children aged less than 5 years: A systematic review and meta-analysis. Korean J Pediatr. 2019; 62(6):206-12. [DOI:10.3345/kjp.2018.07255] [PMID]
- Nemati M, Mikaeili N, Hadi Z. Prevalence of Obesity in Iranian Children: A systematic review study and meta -analysis. Caspian J Pediatrs. 2022; 8(2):748 -59. [Link]
- Akbari H, Mohammadi M. The prevalence of obesity in Iranian children: A systematic review and meta-analysis. J Pediatr Rev. 2022; 10(2):93-102. [DOI:10.32598/jpr.10.2.875.2]
- Sarokhani D, Sarokhani M, Hasanpour Dehkordi A, Ghanei Gheshlagh R, Fakhri M. Prevalence of obesity and overweight in Iranian students: A systematic review and meta-analysis. J Pediatr Endocrinol Metab. 2020; 33(4):453-68. [DOI:10.1515/jpem-2019-0474] [PMID]
- Hajian-Tilaki K, Heidari B. Childhood obesity, overweight, socio-demographic and life style determinants among preschool children in Babol, Northern Iran. Iran J Public Health. 2013; 42(11):1283-91. [PMID]
- Nejadsadeghi E, Sadeghi R, Shojaeizadeh D, Yekaninejad MS, Djazayeri A, Majlesi F. Influence of lifestyle factors on Body Mass Index in preschoolers in Behbahan city, southwest Iran, 2016. Electron Physician. 2018; 10(4):6725-32. [DOI:10.19082/6725] [PMID]
- Hosseini Z. [Evaluation of Body Mass Index among childern of primary school in Behbahan city (Persian)]. Fam Health. 2010; 1(1):1-11. [Link]
- Smith JD, Fu E, Kobayashi MA. Prevention and management of childhood obesity and its psychological and health comorbidities. Annu Rev Clin Psychol. 2020; 16:351-78. [DOI:10.1146/annurev-clinpsy-100219-060201] [PMID]
- Santos AF, Martins MC, Fernandes C, Bost KK, Veríssimo M. Relation between attachment and obesity in preschool years: A systematic review of the literature. Nutrients. 2021; 13(10):3572. [DOI:10.3390/nu13103572] [PMID]
- Tung JY, Ho FK, Tung KT, Wong RS, Wong WH, Chow BC, et al. Does obesity persist from childhood to adolescence? A 4-year prospective cohort study of chinese students in Hong Kong. BMC Pediatr. 2021; 21(1):60. [DOI:10.1186/s12887-021-02504-7] [PMID]
- Kim M, Kim Y, Go Y, Lee S, Na M, Lee Y, et al. Multidimensional cognitive behavioral therapy for obesity applied by psychologists using a digital platform: Open-label randomized controlled trial. JMIR Mhealth Uhealth. 2020; 8(4):e14817. [DOI:10.2196/14817] [PMID]
- Knowlden A, Sharma M. A feasibility and efficacy randomized controlled trial of an online preventative program for childhood obesity: Protocol for the EMPOWER intervention. JMIR Res Protoc. 2012; 1(1):e5. [DOI:10.2196/resprot.2141] [PMID]
- Reis WP, Ghamsary M, Galustian C, Galust H, Herring P, Gaio J, et al. Childhood Obesity: Is the built environment more important than the food environment? Clin Med Insights Pediatr. 2020; 14:1179556520932123. [DOI:10.1177/1179556520932123] [PMID]
- Ayala GX, Monge-Rojas R, King AC, Hunter R, Berge JM. The social environment and childhood obesity: Implications for research and practice in the United States and countries in Latin America. Obes Rev. 2021; 22 Suppl 3(Suppl 3):e13246. [DOI:10.1111/obr.13246] [PMID]
- Mahmood L, Flores-Barrantes P, Moreno LA, Manios Y, Gonzalez-Gil EM. The influence of parental dietary behaviors and practices on children’s eating habits. Nutrients. 2021; 13(4):1138. [DOI:10.3390/nu13041138] [PMID]
- Doggui R, Gallant F, Bélanger M. Parental control and support for physical activity predict adolescents’ moderate to vigorous physical activity over five years. Int J Behav Nutr Phys Act. 2021; 18(1):43. [DOI:10.1186/s12966-021-01107-w] [PMID]
- Salimi N, Karimi-Shahanjarini A, Hazavehei SMM, Roshanaei G. The effect of education on increase breakfast consumption among female students based on social cognitive theory (SCT). Health Scope. 2018; 7(4):e61758. [DOI:10.5812/jhealthscope.61758]
- Mirkarimi SK, Ozoni Doji R, Honarvar M, Aref LF. [Correlation between physical activities, consumption of fruits and vegetables and using social cognitive theory constructs in obese or overweight women referring to health centers in Gorgan (Persian)]. Jorjani Biomed J. 2017; 5(1):52-42. [Link]
- Adhikari C, Puri A, Thapa D, Thapa R, Magar S, Sunil GC. Application of social cognitive theory in obesity prevention: A rapid review. J Health Allied Sci. 2018; 7(1):53-62. [DOI:10.37107/jhas.23]
- Bagherniya M, Taghipour A, Sharma M, Sahebkar A, Contento IR, Keshavarz SA, et al. Obesity intervention programs among adolescents using social cognitive theory: A systematic literature review. Health Educ Res. 2018; 33(1):26-39. [DOI:10.1093/her/cyx079] [PMID]
- Herrera-Sánchez IM, León-Pérez JM, León-Rubio JM. Steps to ensure a successful implementation of occupational health and safety interventions at an organizational level. Front Psychol. 2017; 8:2135. [DOI:10.3389/fpsyg.2017.02135] [PMID]
- Knowlden AP. Feasibility and efficacy of the enabling mothers to prevent pediatric obesity through web-based education and reciprocal determinism (EMPOWER) randomized control trial. Ohio: University of Cincinnati; 2013. [Link]
- Nasirzadeh M, Abdolkarimi M, Asadollahi Z, Hashemian M. Investigating factors effect on fruit and vegetable consumption: Applying social cognitive theory. J Community Health Res. 2020. [DOI:10.18502/jchr.v9i3.4259]
- Sharifi M, Karimi-Shahanjarini A, Bashirian S, Moghimbeigi A. [The effect of an educational intervention on the consumption of healthy snacks in children 1-5 years old (Persian)]. Hayat J. 2017; 22(4):381-93. [Link]
- Alexander DS, Cao C, Alfonso ML. Examining whether the social cognitive theory concepts predict childhood obesity prevention outcome expectations. Int Q Community Health Educ. 2021; 41(2):143-51.[DOI:10.1177/0272684X20915383] [PMID]
- Nyström CD, Sandin S, Henriksson P, Henriksson H, Trolle-Lagerros Y, Larsson C, et al. Mobile-based intervention intended to stop obesity in preschool- aged children: The MINISTOP randomized controlled trial. Am J Clin Nutr. 2017; 105(6):1327-35. [DOI:10.3945/ajcn.116.150995] [PMID]
- Anton S, Das SK, McLaren C, Roberts SB. Application of social cognitive theory in weight management: Time for a biological component? Obesity (Silver Spring). 2021; 29(12):1982-6. [DOI:10.1002/oby.23257] [PMID]
- Sharma M. Theoretical foundations of health education and health promotion. Massachusetts: Jones & Bartlett Learning; 2022. [Link]
- Zolghadr R, Shojaeizadeh D, Sadeghi R, Majlesi F, Yekaninejad MS, Nejadsadeghi E. Effective factors of the healthy nutritional behavior based on the application of social cognitive theory among 13-15-year-old students. Int J Pediatr. 2019; 7(3):9115-23. [DOI:10.22038/ijp.2017.26462.2269]
Type of Study: Original Article |
Subject:
Pediatrics
Received: 2024/04/28 | Accepted: 2025/02/1 | Published: 2025/01/21
Received: 2024/04/28 | Accepted: 2025/02/1 | Published: 2025/01/21
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









