Volume 13, Issue 2 (4-2025)
J. Pediatr. Rev 2025, 13(2): 139-144 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mahjoub Khatibani S P, Rabiei S, Kousha M, Vejdani J, Maleki A, Maleki D. Examining Oral Health and Habits in Children With Attention Deficit Hyperactivity Disorder: A Cross-sectional Study. J. Pediatr. Rev 2025; 13 (2) :139-144
URL: http://jpr.mazums.ac.ir/article-1-634-en.html
URL: http://jpr.mazums.ac.ir/article-1-634-en.html
Seyedeh Porousha Mahjoub Khatibani1 

 , Shaghayegh Rabiei2
, Shaghayegh Rabiei2 

 , Maryam Kousha3
, Maryam Kousha3 

 , Javaneh Vejdani1
, Javaneh Vejdani1 

 , Arayeh Maleki4
, Arayeh Maleki4 

 , Dina Maleki *5
, Dina Maleki *5 




 , Shaghayegh Rabiei2
, Shaghayegh Rabiei2 

 , Maryam Kousha3
, Maryam Kousha3 

 , Javaneh Vejdani1
, Javaneh Vejdani1 

 , Arayeh Maleki4
, Arayeh Maleki4 

 , Dina Maleki *5
, Dina Maleki *5 


1- Department of Pediatric Dentistry, Dental Sciences Research Center, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
2- Dental Sciences Research Center, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Psychiatry, Shafa Hospital, Guilan University of Medical Sciences, Rasht, Iran.
4- Tehran University of Medical Sciences, Tehran, Iran.
5- Dental Sciences Research Center, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran. ,dinamaleki74@gmail.com
2- Dental Sciences Research Center, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Psychiatry, Shafa Hospital, Guilan University of Medical Sciences, Rasht, Iran.
4- Tehran University of Medical Sciences, Tehran, Iran.
5- Dental Sciences Research Center, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran. ,
Keywords: Attention deficit hyperactivity disorder (ADHD), Bruxism, Permanent dentition, Dental caries, Oral health
Full-Text [PDF 376 kb]
(793 Downloads)
| Abstract (HTML) (1519 Views)
Full-Text: (351 Views)
Introduction
Attention deficit hyperactivity disorder (ADHD) is one of the most common psychiatric disorders in children [1, 2]. The number of children with ADHD has continuously increased over the past 20 years; accordingly, 4% to 9% of children in the United States, 10% to 12% in Iran, and 8% to 12% worldwide are diagnosed with ADHD [3-6]. According to the American Dental Association (ADA), the prevalence of ADHD in children was reported to be 6% to 11%.5-6 ADHD diagnosis in boys is 3 to 6 times higher compared to girls [2, 7].
ADHD children are not capable of performing some daily activities, such as brushing their teeth. Thus, poor oral hygiene is common in these children [7, 8]. They are also more likely to develop unhealthy habits leading to dental caries; i.e., using drugs, tobacco, and alcohol, and eating meals more frequently due to binge eating [1, 9, 10]. Decay-missed-filled teeth (DMFT) index is one of the best epidemiological indices to indicate oral hygiene [3, 11]. Drugs suppressing ADHD symptoms, for instance, methylphenidate and dextroamphetamine, may cause gingival overgrowth, xerostomia, and bruxism [12, 13]. Involuntary grinding or clenching in sleep is called bruxism, which is a multifactorial condition [7, 10, 13]. Studies claim that occlusal interferences and the abnormal anatomy of the temporomandibular joint, along with psychological factors, such as stress, anxiety, and individual features like ADHD, lead to bruxism [13-17].
Grooms et al [17] found there to be more primary carious lesions in children with ADHD compared to the control group. Broadbent et al [18] stated that ADHD is a risk factor for high dental caries among children aged 11 to 13 years, whereas Blomqvist et al. [19] claimed that the relation between ADHD and increased dental caries is not significant.
Due to the divergent results of the previous studies and the absence of similar ones in Iranian populations, the present study was conducted to discuss the oral health condition and habits of children with ADHD.
Methods
This analytic cross-sectional study was carried out in the Pediatric Department of the Dental Faculty of Guilan University of Medical Sciences from 2021 to 2024. This study evaluated the oral health and oral habits of 36 children diagnosed with ADHD and 36 children without ADHD (control group). The ADHD of children was diagnosed by one of the authors, who is a psychiatrist. Children 12 to 14 years old who had lost all of their primary teeth were included in the study. Patients who had any other medical conditions, consumed medicine for ADHD, and were undergoing orthodontic treatment were excluded. Written consent was obtained from the parents. The study is reported according to the strengthening the reporting of observational studies in epidemiology guidelines.
To determine the sample size for the two groups of test and control, the following formula was used, considering a statistical power of 80%, an error rate of 0.05, standard deviations equal to 9.2 and 33.5, and d=16.3. The sample size was calculated at 35.61 minimum, which was rounded up to 36 for both groups [3].
The DMFT and the gingival bleeding index (GBI) were measured in both groups. To measure the DMFT, dental surfaces, pits, and grooves were explored; any tooth with unsupported enamel and softened enamel around a lesion or treated with the provisional filling was declared as decayed. To make a careful diagnosis of proximal caries, two bitewing radiographs were obtained from each patient with their parents’ consent using the Minray/ Soredex/ Finland radiography device on a 70 kVp/ 7 mA/ 0.2 s setting. The extracted teeth were counted as “missing,” and the restored teeth as “filled.”
To determine the periodontal condition, the GBI index was measured using the Michigan O, marking William’s probe at 6 points (i.e. mesial, middle, distal portions in both buccal and lingual sides) around each tooth. The bleeding status of each point was recorded, and ultimately, the number of bleeding points was divided by the total number of assessed points, and the percentage was then calculated.
Parents filled out the questionnaires regarding the information about their education level and the oral habits and oral health of the child.
The first five questions were about the oral habits of the children. The questions asked that if their children had experienced nail-biting, thumb-sucking, teeth-grinding, placing foreign objects between teeth, or any trauma to the head, face, or neck area. The answers were “yes” or “no.”
Questions 6 to 8 focused on the children’s oral health. They asked: “Does your child brush their teeth at night?”, “Does your child brush their teeth in the morning?”, and “Does your child use dental floss?”. Each question had two possible answers: “Yes” or “No.”
To analyze the data, the SPSS software, version 16 (SPSS Inc., Chicago, IL, USA) was used, and the independent t-test, the analysis of variance, the Fisher test, and linear regression test were applied at the significance level of 0.05.
Results
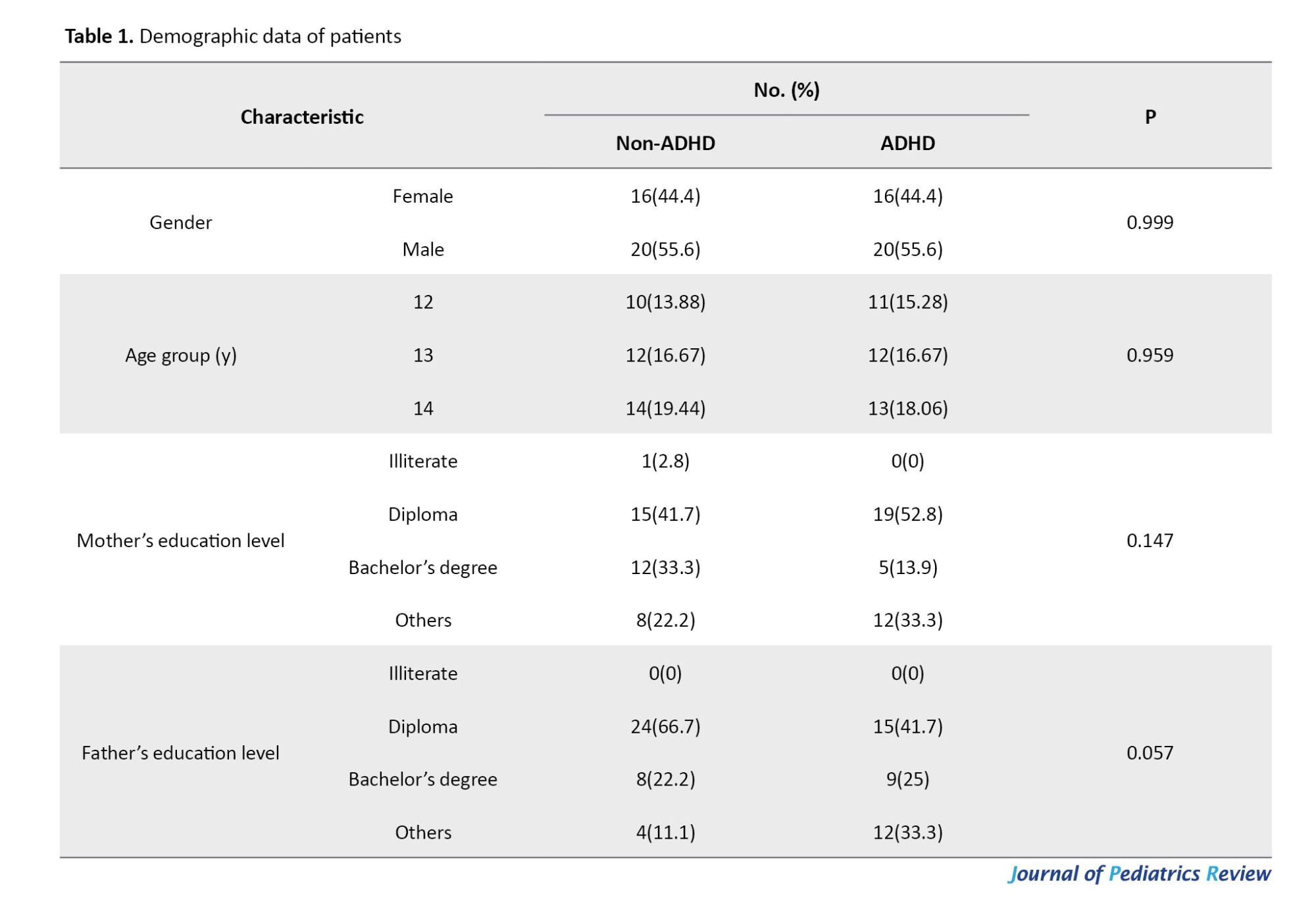
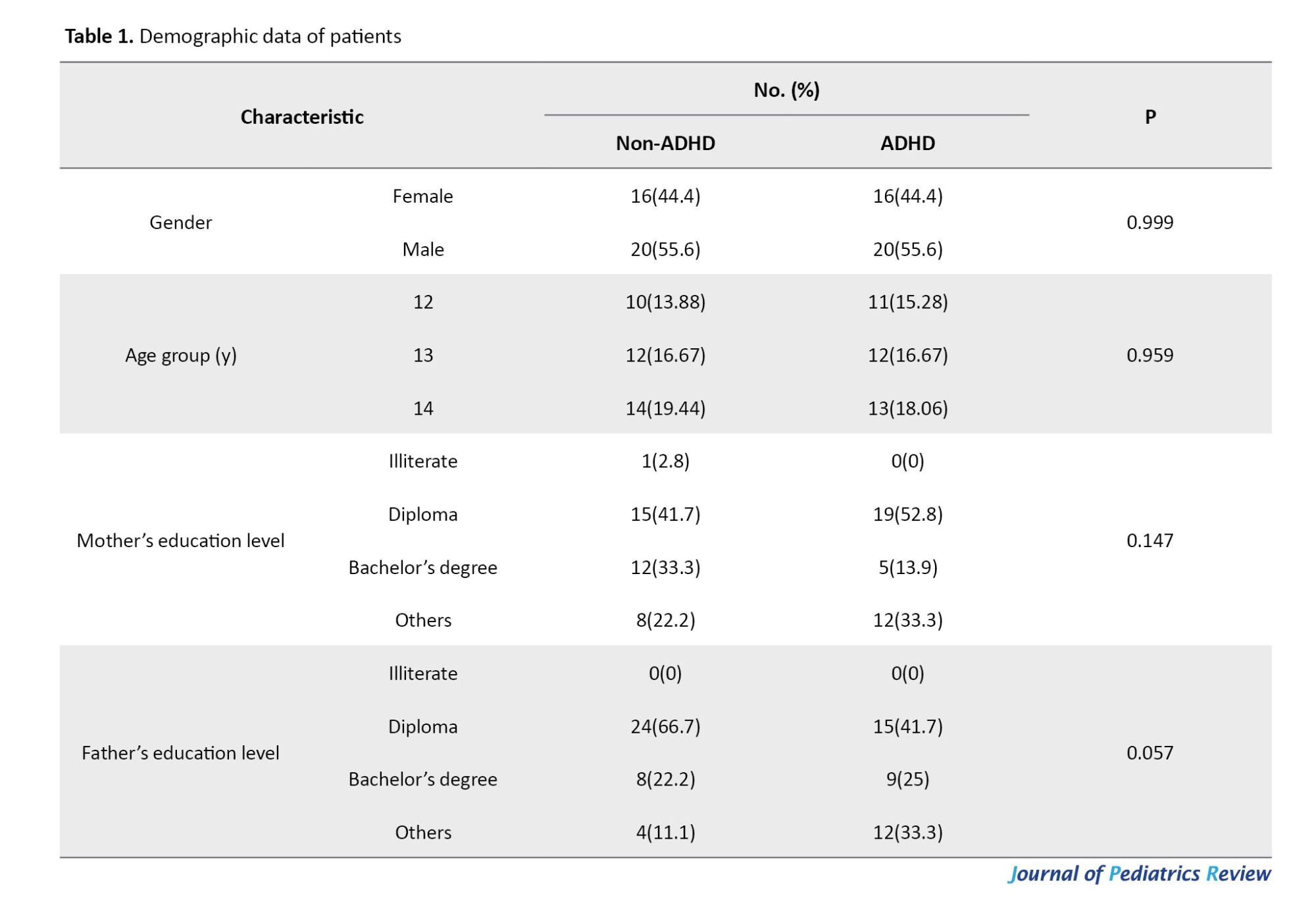
In the current study, 72 children (40 boys and 32 girls) aged 12-14 years were selected and allocated into two groups of 36, then examined and assessed. The distribution data regarding gender, age, mothers’ education level, and fathers’ education level are presented in Table 1. The distribution of patients according to gender, age, mothers’ and fathers’ education level was not significantly different (P=0.999, P=0.959, P=0.057, and P=0.147, respectively).
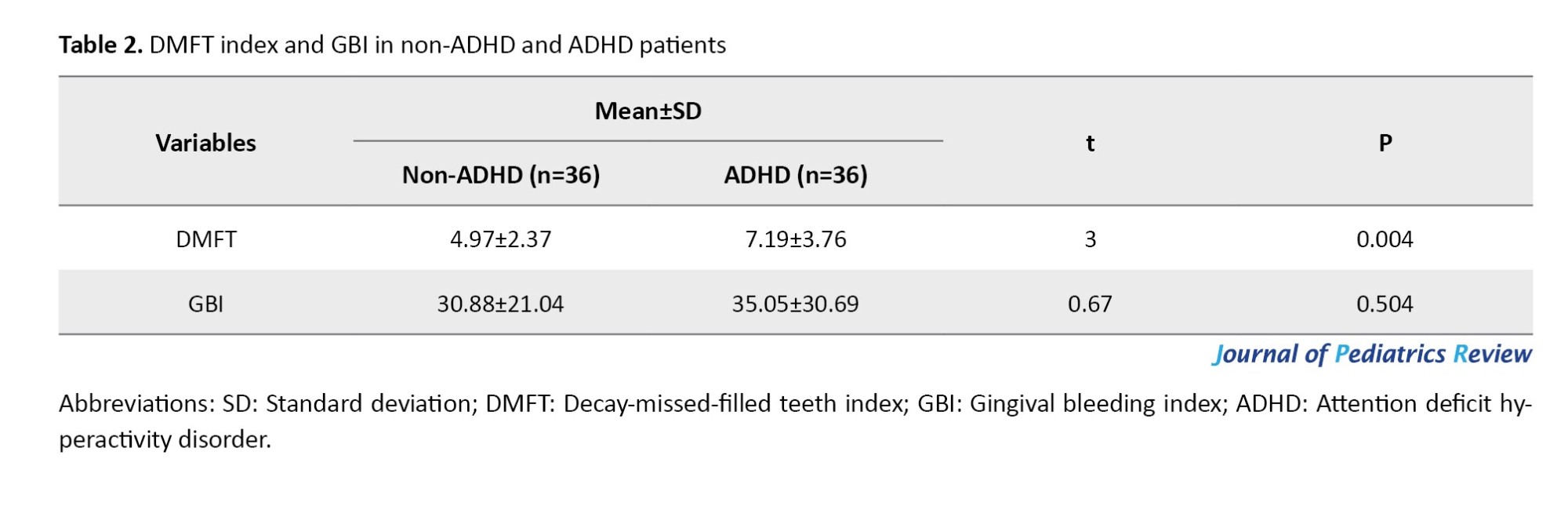
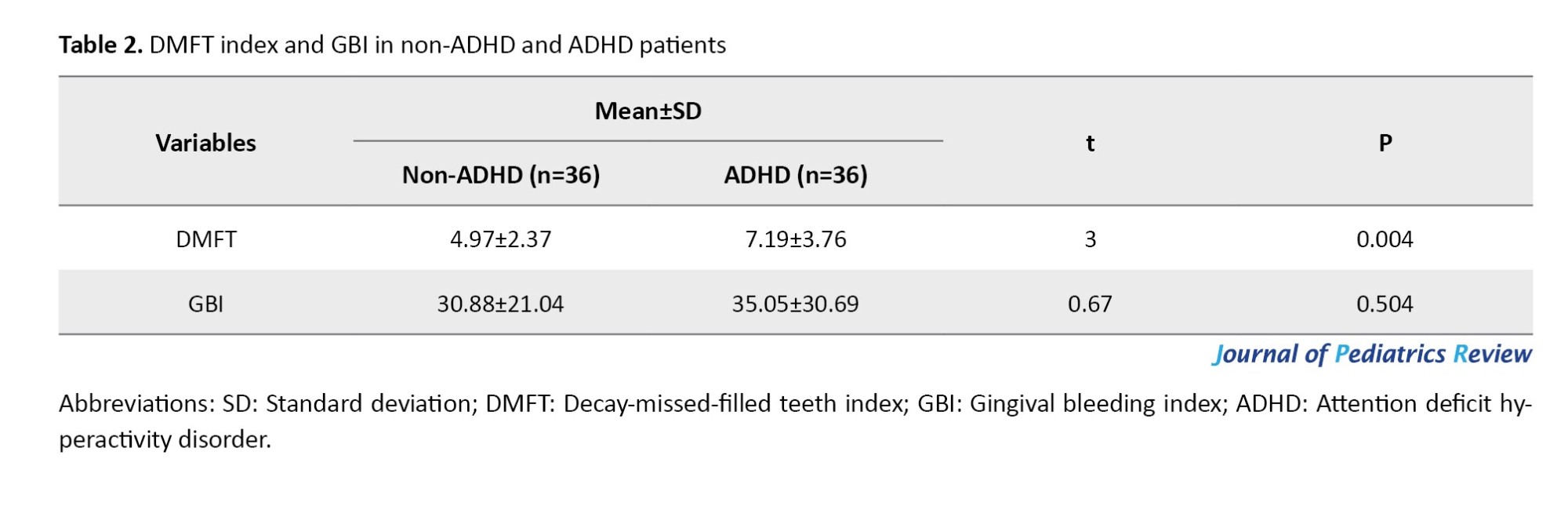
Using the independent t-test, DMFT and GBI were compared in the two groups (Table 2). Accordingly, DMFT was significantly higher in the ADHD group than non-ADHD group (P=0.004). GBI was not significantly different between the two study groups (P=0.504).
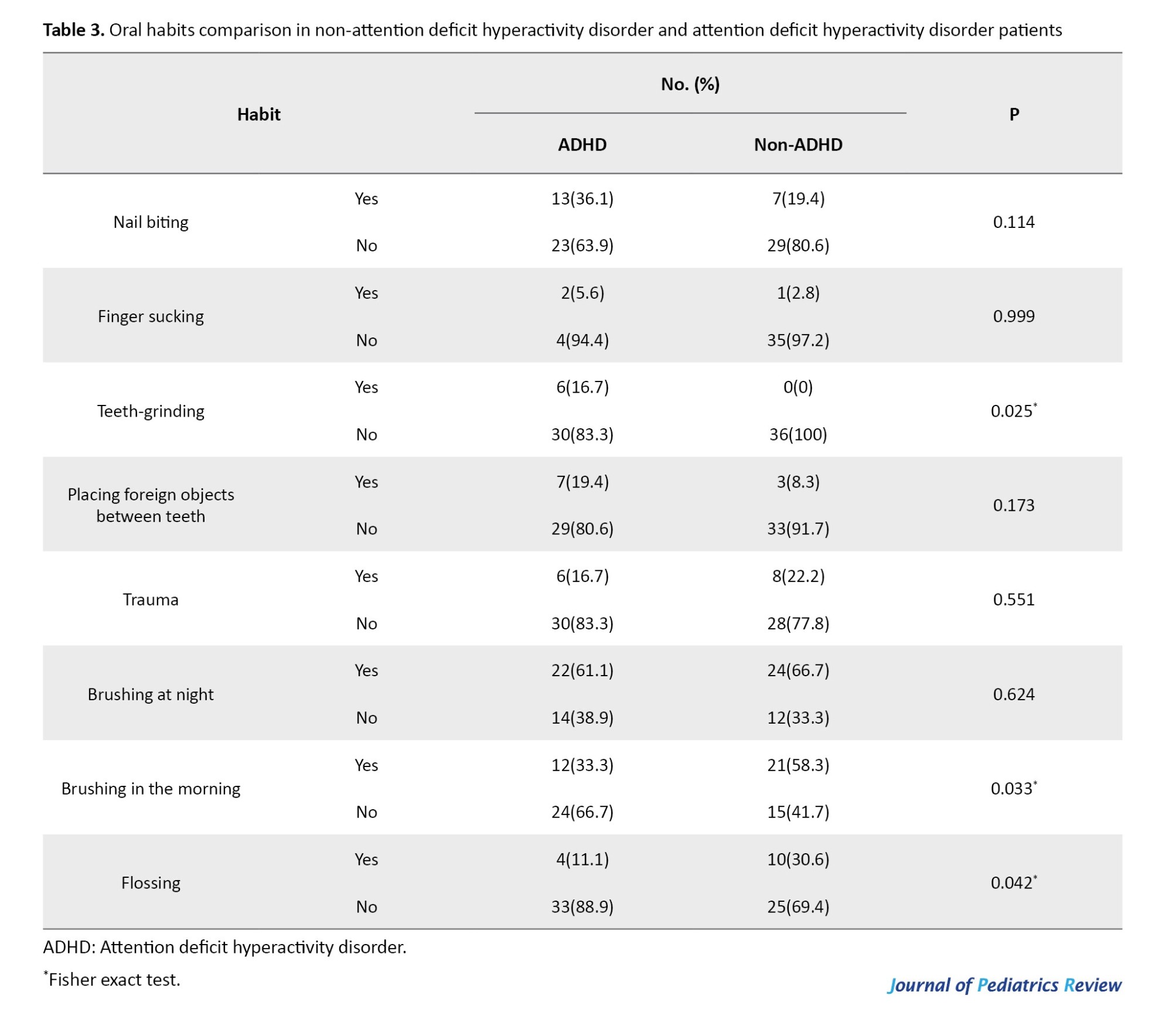
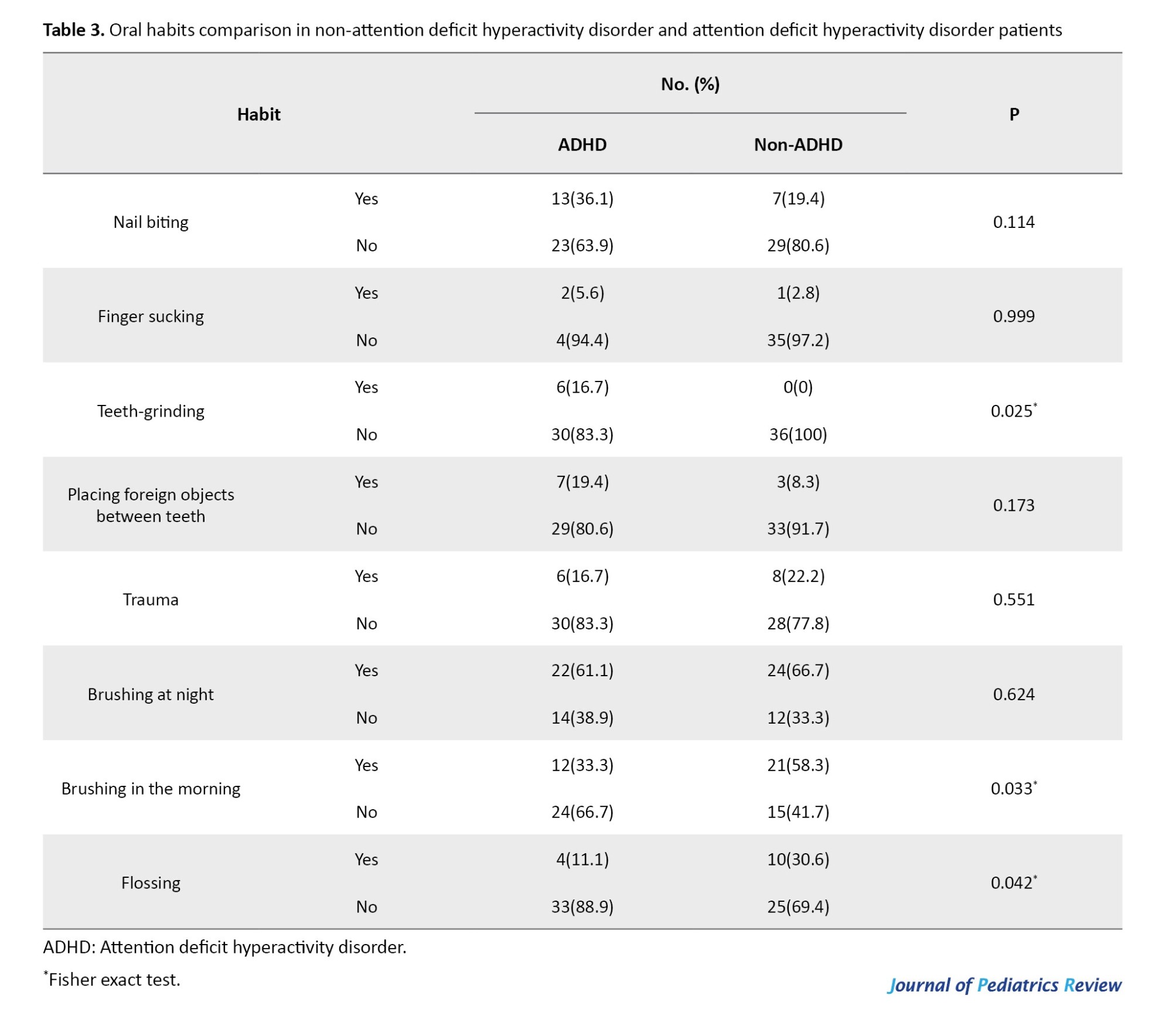
To analyze the data from the questionnaire about oral habits, the Fisher exact test was applied. According to Table 3, tooth grinding, brushing in the morning, and flossing were significantly different between the groups (P=0.025, P=0.033, P=0.042, respectively).
Discussion
Children and teenagers diagnosed with ADHD cannot focus on their daily activities, such as brushing their teeth, and lack integrity, therefore, they have poor oral hygiene [5]. Other factors, for example, being more prone to use alcohol, tobacco, and drugs, [6, 7] ineffective brushing, and snacking frequently, are definite determinants for the development of dental caries in these patients [9, 10]. Moreover, as children and teenagers grow older, their responsibilities increase and parental supervision decreases, so ADHD is exacerbated, which may majorly affect the future dental needs of the patients [3]. The present study investigated the DMFT and GBI indices through clinical and radiographical examination and assessed bruxism using a questionnaire. The results showed that DMFT was higher in ADHD patients.
Similarly, in a study by Broadbent et al [18], it was indicated that the DMFT index in children with ADHD was higher and ADHD was a factor for tooth decay in the age range of 11 to 13 years old. Additionally, the consumption of drugs and sweet beverages to compensate for xerostomia was considered an important factor for tooth decay [18, 20]. Grooms et al. [17] and Kohlboeck et al. [21] also reached similar findings.
However, Blomqvist et al. [1] found conflicting results. In 2006, a total of 25 children with ADHD and 58 healthy 11-year-olds were studied, and due to unhealthy diets, ineffective brushing, and lack of focus, DMFS was significantly higher in the test group. However, in another study in 2007, a test and control group of 13-year-old children, including 21 and 79 subjects respectively, were investigated, and despite their poor hygiene, the DMFS index was not statistically significant [19].
Accordingly, to inspect the relationship between ADHD and oral hygiene in permanent dentition, Chau et al. [22] conducted a study and reported no significant difference between the ADHD and control groups. As for the mean GBI index, despite it being higher in the test group, the existing mean difference was not statistically significant; this is consistent with the findings of the study carried out by Kohlboeck et al. [21] Chau et al. [22] stated that the gingivitis in ADHD patients was higher than the control group; however, in the case of periodontal disease, the differences were not significant.
As the results demonstrated, bruxism was significantly higher in the test group, and the results of studies carried out by Mota-Veloso et al. [23] and Chau et al. [22] were consistent with the current study’s findings. It is suggested that future studies be conducted with more subjects and older age groups. Also, it is suggested to compare the oral health and oral habits of ADHD children who are consuming medicine and are not consuming medicine. One of the limitations of this study was not considering the diet of children.
Conclusion
Children diagnosed with ADHD had poor oral hygiene and increased dental caries compared to the non-ADHD children. DMFT index and bruxism were significantly higher, and although the GBI index difference in the two groups was not statistically significant, it was indeed higher in ADHD patients. With regular dentist appointments, prevention, education, and proper brushing, children’s oral and dental problems will decrease. As a result, regular appointments and proper health education for this group of children should be in the dentist’s schedule.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1398.244).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflicts of interest
The authors declared no conflict of interest.
References
Attention deficit hyperactivity disorder (ADHD) is one of the most common psychiatric disorders in children [1, 2]. The number of children with ADHD has continuously increased over the past 20 years; accordingly, 4% to 9% of children in the United States, 10% to 12% in Iran, and 8% to 12% worldwide are diagnosed with ADHD [3-6]. According to the American Dental Association (ADA), the prevalence of ADHD in children was reported to be 6% to 11%.5-6 ADHD diagnosis in boys is 3 to 6 times higher compared to girls [2, 7].
ADHD children are not capable of performing some daily activities, such as brushing their teeth. Thus, poor oral hygiene is common in these children [7, 8]. They are also more likely to develop unhealthy habits leading to dental caries; i.e., using drugs, tobacco, and alcohol, and eating meals more frequently due to binge eating [1, 9, 10]. Decay-missed-filled teeth (DMFT) index is one of the best epidemiological indices to indicate oral hygiene [3, 11]. Drugs suppressing ADHD symptoms, for instance, methylphenidate and dextroamphetamine, may cause gingival overgrowth, xerostomia, and bruxism [12, 13]. Involuntary grinding or clenching in sleep is called bruxism, which is a multifactorial condition [7, 10, 13]. Studies claim that occlusal interferences and the abnormal anatomy of the temporomandibular joint, along with psychological factors, such as stress, anxiety, and individual features like ADHD, lead to bruxism [13-17].
Grooms et al [17] found there to be more primary carious lesions in children with ADHD compared to the control group. Broadbent et al [18] stated that ADHD is a risk factor for high dental caries among children aged 11 to 13 years, whereas Blomqvist et al. [19] claimed that the relation between ADHD and increased dental caries is not significant.
Due to the divergent results of the previous studies and the absence of similar ones in Iranian populations, the present study was conducted to discuss the oral health condition and habits of children with ADHD.
Methods
This analytic cross-sectional study was carried out in the Pediatric Department of the Dental Faculty of Guilan University of Medical Sciences from 2021 to 2024. This study evaluated the oral health and oral habits of 36 children diagnosed with ADHD and 36 children without ADHD (control group). The ADHD of children was diagnosed by one of the authors, who is a psychiatrist. Children 12 to 14 years old who had lost all of their primary teeth were included in the study. Patients who had any other medical conditions, consumed medicine for ADHD, and were undergoing orthodontic treatment were excluded. Written consent was obtained from the parents. The study is reported according to the strengthening the reporting of observational studies in epidemiology guidelines.
To determine the sample size for the two groups of test and control, the following formula was used, considering a statistical power of 80%, an error rate of 0.05, standard deviations equal to 9.2 and 33.5, and d=16.3. The sample size was calculated at 35.61 minimum, which was rounded up to 36 for both groups [3].
The DMFT and the gingival bleeding index (GBI) were measured in both groups. To measure the DMFT, dental surfaces, pits, and grooves were explored; any tooth with unsupported enamel and softened enamel around a lesion or treated with the provisional filling was declared as decayed. To make a careful diagnosis of proximal caries, two bitewing radiographs were obtained from each patient with their parents’ consent using the Minray/ Soredex/ Finland radiography device on a 70 kVp/ 7 mA/ 0.2 s setting. The extracted teeth were counted as “missing,” and the restored teeth as “filled.”
To determine the periodontal condition, the GBI index was measured using the Michigan O, marking William’s probe at 6 points (i.e. mesial, middle, distal portions in both buccal and lingual sides) around each tooth. The bleeding status of each point was recorded, and ultimately, the number of bleeding points was divided by the total number of assessed points, and the percentage was then calculated.
Parents filled out the questionnaires regarding the information about their education level and the oral habits and oral health of the child.
The first five questions were about the oral habits of the children. The questions asked that if their children had experienced nail-biting, thumb-sucking, teeth-grinding, placing foreign objects between teeth, or any trauma to the head, face, or neck area. The answers were “yes” or “no.”
Questions 6 to 8 focused on the children’s oral health. They asked: “Does your child brush their teeth at night?”, “Does your child brush their teeth in the morning?”, and “Does your child use dental floss?”. Each question had two possible answers: “Yes” or “No.”
To analyze the data, the SPSS software, version 16 (SPSS Inc., Chicago, IL, USA) was used, and the independent t-test, the analysis of variance, the Fisher test, and linear regression test were applied at the significance level of 0.05.
Results
In the current study, 72 children (40 boys and 32 girls) aged 12-14 years were selected and allocated into two groups of 36, then examined and assessed. The distribution data regarding gender, age, mothers’ education level, and fathers’ education level are presented in Table 1. The distribution of patients according to gender, age, mothers’ and fathers’ education level was not significantly different (P=0.999, P=0.959, P=0.057, and P=0.147, respectively).
Using the independent t-test, DMFT and GBI were compared in the two groups (Table 2). Accordingly, DMFT was significantly higher in the ADHD group than non-ADHD group (P=0.004). GBI was not significantly different between the two study groups (P=0.504).
To analyze the data from the questionnaire about oral habits, the Fisher exact test was applied. According to Table 3, tooth grinding, brushing in the morning, and flossing were significantly different between the groups (P=0.025, P=0.033, P=0.042, respectively).
Discussion
Children and teenagers diagnosed with ADHD cannot focus on their daily activities, such as brushing their teeth, and lack integrity, therefore, they have poor oral hygiene [5]. Other factors, for example, being more prone to use alcohol, tobacco, and drugs, [6, 7] ineffective brushing, and snacking frequently, are definite determinants for the development of dental caries in these patients [9, 10]. Moreover, as children and teenagers grow older, their responsibilities increase and parental supervision decreases, so ADHD is exacerbated, which may majorly affect the future dental needs of the patients [3]. The present study investigated the DMFT and GBI indices through clinical and radiographical examination and assessed bruxism using a questionnaire. The results showed that DMFT was higher in ADHD patients.
Similarly, in a study by Broadbent et al [18], it was indicated that the DMFT index in children with ADHD was higher and ADHD was a factor for tooth decay in the age range of 11 to 13 years old. Additionally, the consumption of drugs and sweet beverages to compensate for xerostomia was considered an important factor for tooth decay [18, 20]. Grooms et al. [17] and Kohlboeck et al. [21] also reached similar findings.
However, Blomqvist et al. [1] found conflicting results. In 2006, a total of 25 children with ADHD and 58 healthy 11-year-olds were studied, and due to unhealthy diets, ineffective brushing, and lack of focus, DMFS was significantly higher in the test group. However, in another study in 2007, a test and control group of 13-year-old children, including 21 and 79 subjects respectively, were investigated, and despite their poor hygiene, the DMFS index was not statistically significant [19].
Accordingly, to inspect the relationship between ADHD and oral hygiene in permanent dentition, Chau et al. [22] conducted a study and reported no significant difference between the ADHD and control groups. As for the mean GBI index, despite it being higher in the test group, the existing mean difference was not statistically significant; this is consistent with the findings of the study carried out by Kohlboeck et al. [21] Chau et al. [22] stated that the gingivitis in ADHD patients was higher than the control group; however, in the case of periodontal disease, the differences were not significant.
As the results demonstrated, bruxism was significantly higher in the test group, and the results of studies carried out by Mota-Veloso et al. [23] and Chau et al. [22] were consistent with the current study’s findings. It is suggested that future studies be conducted with more subjects and older age groups. Also, it is suggested to compare the oral health and oral habits of ADHD children who are consuming medicine and are not consuming medicine. One of the limitations of this study was not considering the diet of children.
Conclusion
Children diagnosed with ADHD had poor oral hygiene and increased dental caries compared to the non-ADHD children. DMFT index and bruxism were significantly higher, and although the GBI index difference in the two groups was not statistically significant, it was indeed higher in ADHD patients. With regular dentist appointments, prevention, education, and proper brushing, children’s oral and dental problems will decrease. As a result, regular appointments and proper health education for this group of children should be in the dentist’s schedule.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1398.244).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflicts of interest
The authors declared no conflict of interest.
References
- Blomqvist M, Holmberg K, Fernell E, Ek U, Dahllöf G. Oral health, dental anxiety, and behavior management problems in children with attention deficit hyperactivity disorder. Eur J Oral Sci. 2006; 114(5):385-90. [DOI:10.1111/j.1600-0722.2006.00393.x] [PMID]
- Suzuki T, Wada K, Nakazato M, Ohtani T, Yamazaki M, Ikeda S. Associations between Adult Attention-Deficit/Hyperactivity Disorder (ADHD) traits and sociodemographic characteristics in Japanese Workers. Neuropsychiatr Dis Treat. 2023; 19:759-73. [DOI:10.2147/NDT.S398478] [PMID]
- Heshmatpour F, Abdikhani MS. Ce-Ag-ZnO/Fe3O4 nanocomposites: A novel magnetically separable photocatalyst for highly efficient photodegradation of contaminants. Physica B Condens Matter. 2019; 570:312-9. [DOI:10.1016/j.physb.2019.06.005]
- Manoharan S, Krishnamoorthy K. Dental caries and children with Attention Deficit Hyperactivity Disorder (ADHD)-A review. J Pharm Sci Res. 2016; 8(7):613-5. [Link]
- Chandra P, Anandakrishna L, Ray P. Caries experience and oral hygiene status of children suffering from attention deficit hyperactivity disorder. J Clin Pediatr Dent. 2009; 34(1):25-9. [DOI:10.17796/jcpd.34.1.n170271832662v44] [PMID]
- Friedlander AH, Yagiela JA, Mahler ME, Rubin R. The pathophysiology, medical management, and dental implications of adult attention-deficit/hyperactivity disorder. J Am Dent Assoc. 2007; 138(4):475-82; quiz 535, 537. [DOI:10.14219/jada.archive.2007.0199] [PMID]
- Cortese S, Isnard P, Frelut ML, Michel G, Quantin L, Guedeney A, et al. Association between symptoms of attention-deficit/hyperactivity disorder and bulimic behaviors in a clinical sample of severely obese adolescents. Int J Obes. 2007; 31(2):340-6. [DOI:10.1038/sj.ijo.0803400] [PMID]
- Holbrook WP, Árnadóttir IB, Takazoe I, Birkhed D, Frostell G. Longitudinal study of caries, cariogenic bacteria and diet in children just before and after starting school. Eur J Oral Sci. 1995; 103(1):42-5. [DOI:10.1111/j.1600-0722.1995.tb00009.x] [PMID]
- No Author. Report of workshop aimed at defining guidelines for caries clinical trials: Superiority and equivalency claims for anticaries dentifrices. Council on Dental Therapeutics. J Am Dent Assoc. 1988; 117(5):663-5. [DOI:10.14219/jada.archive.1988.0048] [PMID]
- Sciberras E, Efron D, Gerner B, Davey M, Mensah F, Oberklaid F, et al. Study protocol: The sleeping sound with attention-deficit/hyperactivity disorder project. BMC Pediatr. 2010; 10:101. [DOI:10.1186/1471-2431-10-101] [PMID]
- Vejdani J, Janeshin A, Gholinia F, Alinejad Roudsari F, Maleki D. The prevalence of malocclusion and dental caries in 11-to 14-year-old children in Roudsar, Iran. J Dentomaxillofacial Radiol Pathol Surg. 2019; 8(4):7-12. [Link]
- Malekzadeh M, Maleki D, Zohary M. Effect of adjunctive low-level laser therapy on gingival graft: A Review of the Literature. J Dentomaxillofacial Radiol Pathol Surg. 2022; 11(1):7-13. [Link]
- Manfredini D, Restrepo C, Diaz-Serrano K, Winocur E, Lobbezoo F. Prevalence of sleep bruxism in children: A systematic review of the literature. J Oral Rehabil. 2013; 40(8):631-42. [DOI:10.1111/joor.12069] [PMID]
- Malekzadeh M, Nosrati M, Maleki D. Assessment of dental student’knowledge of tooth wear: Diagnosis, prevalence and treatment: A Randomized Questionnaire-based Cross-sectional Study. J Dentomaxillofacial. 2018; 7(3):123-8. [Link]
- Serra-Negra JM, Ramos-Jorge ML, Flores-Mendoza CE, Paiva SM, Pordeus IA. Influence of psychosocial factors on the development of sleep bruxism among children. Int J Paediatr Dent. 2009; 19(5):309-17. [DOI:10.1111/j.1365-263X.2009.00973.x] [PMID]
- Chervin RD, Archbold KH, Dillon JE, Panahi P, Pituch KJ, Dahl RE, et al. Inattention, hyperactivity, and symptoms of sleep-disordered breathing. Pediatrics. 2002; 109(3):449-56. [DOI:10.1542/peds.109.3.449] [PMID]
- Grooms MT, Keels MA, Roberts MW, McIver FT. Caries experience associated with attention-deficit/hyperactivity disorder. J Clin Pediatr Dent. 2005; 30(1):3-7. [PMID]
- Broadbent JM, Ayers KM, Thomson WM. Is attention-deficit hyperactivity disorder a risk factor for dental caries? A case-control study. Caries Res. 2004; 38(1):29-33. [DOI:10.1159/000073917] [PMID]
- Blomqvist M, Holmberg K, Fernell E, Ek U, Dahllöf G. Dental caries and oral health behavior in children with attention deficit hyperactivity disorder. Eur J Oral Sci. 2007; 115(3):186-91. [DOI:10.1111/j.1600-0722.2007.00451.x] [PMID]
- Shooshtary MH, Chimeh N, Najafi M, Mohamadi MR, Yousefi-Nouraie R, Rahimi-Mvaghar A. The prevalence of Attention Deficit Hyperactivity Disorder in Iran: A systematic review. Iran J Psychiatry. 2010; 5(3):88-92. [PMID]
- Kohlboeck G, Heitmueller D, Neumann C, Tiesler C, Heinrich J, Heinrich-Weltzien R, et al. Is there a relationship between hyperactivity/inattention symptoms and poor oral health? Results from the GINIplus and LISAplus study. Clin Oral Investig. 2013; 17(5):1329-38. [DOI:10.1007/s00784-012-0829-7] [PMID]
- Chau YC, Lai KY, McGrath CP, Yiu CK. Oral health of children with attention deficit hyperactivity disorder. Eur J Oral Sci. 2017; 125(1):49-54. [PMID]
- Mota-Veloso I, Celeste RK, Fonseca CP, Soares MEC, Marques LS, Ramos-Jorge ML, et al. Effects of attention deficit hyperactivity disorder signs and socio-economic status on sleep bruxism and tooth wear among schoolchildren: Structural equation modelling approach. Int J Paediatr Dent. 2017 ; 27(6):523-31. [PMID]
Type of Study: Original Article |
Subject:
Dentistry
Received: 2025/01/12 | Accepted: 2025/03/10 | Published: 2025/04/1
Received: 2025/01/12 | Accepted: 2025/03/10 | Published: 2025/04/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |