Volume 13, Issue 3 (7-2025)
J. Pediatr. Rev 2025, 13(3): 257-262 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Heravi N, Hosseini S A, Ghelichi-Ghojogh M, Aghapour S A. Frequency of Autoimmunity in Children With Autism Spectrum Disorders and Their Parents: A Cross-sectional Study. J. Pediatr. Rev 2025; 13 (3) :257-262
URL: http://jpr.mazums.ac.ir/article-1-649-en.html
URL: http://jpr.mazums.ac.ir/article-1-649-en.html
1- Neonatal & Children’s Health Research Center, School of Health, Golestan University of Medical Sciences, Gorgan, Iran.
2- Department of Biostatistics and Epidemiology, School of Health, Golestan University of Medical Sciences, Gorgan, Iran. & Department of Biostatistics and Epidemiology, School of Health, Golestan University of Medical Sciences, Gorgan, Iran.
3- Neonatal & Children’s Health Research Center, School of Health, Golestan University of Medical Sciences, Gorgan, Iran. ,s.a.aghapour@googlemail.com
2- Department of Biostatistics and Epidemiology, School of Health, Golestan University of Medical Sciences, Gorgan, Iran. & Department of Biostatistics and Epidemiology, School of Health, Golestan University of Medical Sciences, Gorgan, Iran.
3- Neonatal & Children’s Health Research Center, School of Health, Golestan University of Medical Sciences, Gorgan, Iran. ,
Full-Text [PDF 433 kb]
(359 Downloads)
| Abstract (HTML) (999 Views)
Full-Text: (168 Views)
Introduction
Autism spectrum disorder (ASD) is a neurobiological condition shaped by genetic, epigenetic, and environmental elements, impacting the growing brain, and marked by impaired social and emotional interaction, difficulties in learning, axiety, epilepsy, language impairments, restrictive actions, and the existence of limited interests and repetitive actions. Reduced size of cells in the hippocampus and limbic system and an elevated number of prefrontal cortex neurons may be related to clinical manifestations. ASD patients also exhibit atypical development of the temporal and frontal lobes and reduced amygdala volume and gray matter in magnetic resonance imaging (MRI) findings [1].
The World Health Organization (WHO) approximates the worldwide occurrence of ASD at 0.76%; nevertheless, this represents merely around 16% of the total children worldwide. The occurrence of ASD is roughly 2.47%, 0.06%, and 0.36% in the USA, Iran, and Asia, respectively [2]. ASD is more predominant in males than in females. Y polysomies are more likely to exhibit autism compared to X chromosome polysomies, indicating the significance of Y chromosome genes in the development of ASD. Girls are less frequently diagnosed than boys, and those who do receive a diagnosis tend to have more intellectual and behavioral disabilities than boys with the diagnosis [3].
ASD is a disorder with a strong genetic basis that causes different phenotypic changes. Each gene mutation leads to different neuropsychiatric disorders. For example, IL1RAPL1, OPHN1, RELN, GluR6, GRIN2A, GRIN2B, CNTNAP2, GABRB3, 5-HTT, and TPH2 are associated with intellectual disability, schizophrenia, childhood absence epilepsy, depression, attention deficit hyperactivity disorder (ADHD), and major depression [4].
Multiple biochemical features are identified as biomarkers that increase the likelihood of ASD. One or more preliminary biomarkers recognized at birth (or earlier) can predict the subsequent emergence of a genuine autistic disorder, such as low serum IGF1, anti-myelin basic protein, increased serotonin, single-nucleotide polymorphism rs1801123, and single-nucleotide polymorphism rs878960 [5].
ASD also has an autoimmune aspect. The initial research suggested the notion that autoimmunity might be a significant cause of ASD, as outlined in a case report that documented a child with a substantial familial background of autoimmune conditions. Also, in recent studies, significant correlations were observed between ASD and additional autoimmune conditions, like celiac disease, hypothyroidism, type 1 diabetes, rheumatoid arthritis, and psoriasis [6].
Therefore, identifying immune mechanisms directly associated with ASD may facilitate the development of preventive measures and potentially lead to the discovery of novel therapeutic agents [7]. No medication has been demonstrated to be effective in addressing the primary symptoms of ASD. Risperidone and aripiprazole are the two drugs that have received approval from the Food and Drug Administration (FDA) for treating children and teenagers with ASD. Both help with irritability and stereotypical behaviors [8]. This study aimed to determine the frequency of autoimmunity in children with ASD and their parents in Gorgan.
Methods
The study with a cross-sectional design was carried out in Gorgan City, located in the northeast of Iran. The records and information related to all autism patients in Golestan Province in 2021 were reviewed, and all eligible patients were identified to be included in the study. Subjects were autistic patients covered by the Welfare Organization of Golestan Province.
This study used diagnostic and statistical manual of mental disorders, fifth edition (DSM-5) criteria as an inclusion criterion for ASD diagnosis, which is detailed below [9]:
A) Ongoing challenges in social communication and social interaction across various environments, including challenges in social-emotional reciprocity, non-verbal communication behaviors, and forming, sustaining, and comprehending relationships.
B) Limited, repetitive patterns of actions, interests, or pursuits.
C) Symptoms must be observable during the early developmental phase.
D) Symptoms lead to notable deterioration in social, work-related, or other crucial aspects of present functioning.
E) These disruptions are not better explained by cognitive impairment.
Informed consent was acquired from participants prior to serum collection. We collected 5 mL of venous blood from children with autism and their parents; from this amount, 2 mL of blood was used for complete blood count (CBC) measurements in tubes containing K2EDTA, and 3 mL of blood was poured into clot tubes for C-reactive protein (CRP) and antinuclear antibody (ANA) measurements. CBC measurements were performed using a Sysmax KX21N cell counter made in Japan. Then, the differential count of white blood cells was done using a light microscope with a 100x lens after preparing a blood smear and performing Giemsa staining.
The clot tube containing 3 mL of venous blood was centrifuged at 4500 rpm after being placed in a Bain-Marie at 37 °C for 15 minutes, and a clot formed in the centrifuge. After centrifugation, the serum was separated from the clot-containing blood cells, transferred into another tube, and stored in a freezer at -20 °C until the experiments were performed. ANA tests were performed using the enzyme linked immunosorbent assay (ELISA) method with the ANA-HEp2 ELISA kit from AESKULISA. Also, CRP tests were performed using the latex agglutination method using a kit made by Padco. Also, 5 mL of venous blood was taken from the parents of the patients whose ANA tests were positive, and all the mentioned tests were performed for them. All tests were conducted in the laboratory of Taleghani Hospital in Gorgan.
Statistical analysis
Mean±SD were used to describe quantitative information, while frequency and relative frequency were used to describe qualitative information. Data were analyzed using STATA software, version 17 software. To represent the quantitative variables, the Mean±SD was employed, while the frequency distribution table was utilized to present the count and percentage of instances for qualitative variables. Qualitative variables were analyzed using the chi-square and Fisher’s exact tests. The Mann-Whitney test was used to compare quantitative variables with qualitative variables due to the non-normality of data distribution. All tests were two-sided, and P<0.05 was considered statistically significant.
Results
Our investigation included a total of 56 individuals. The mean age of children was 10.04±3.99 years, with a range of 1-18 years. Also, the gender distribution of the children included in the study was 43 boys (76.8%) and 13 girls (23.2%). The difference in mean age of male and female patients was not statistically significant (P=0.368).
Based on the cut-off point of the ANA test (10 units/mL), patients were divided into two groups: Those with autoimmune disease (13 individuals; 23.21%) and those without autoimmune disease (43 individuals; 76.79%). ANA values in the two groups were significantly different (P<0.001). The mean ANA values in the autoimmune group were 23.02±6.49 units/mL, while in the non-autoimmune group, they were 4.01±1.66 units/mL (Figure 1).

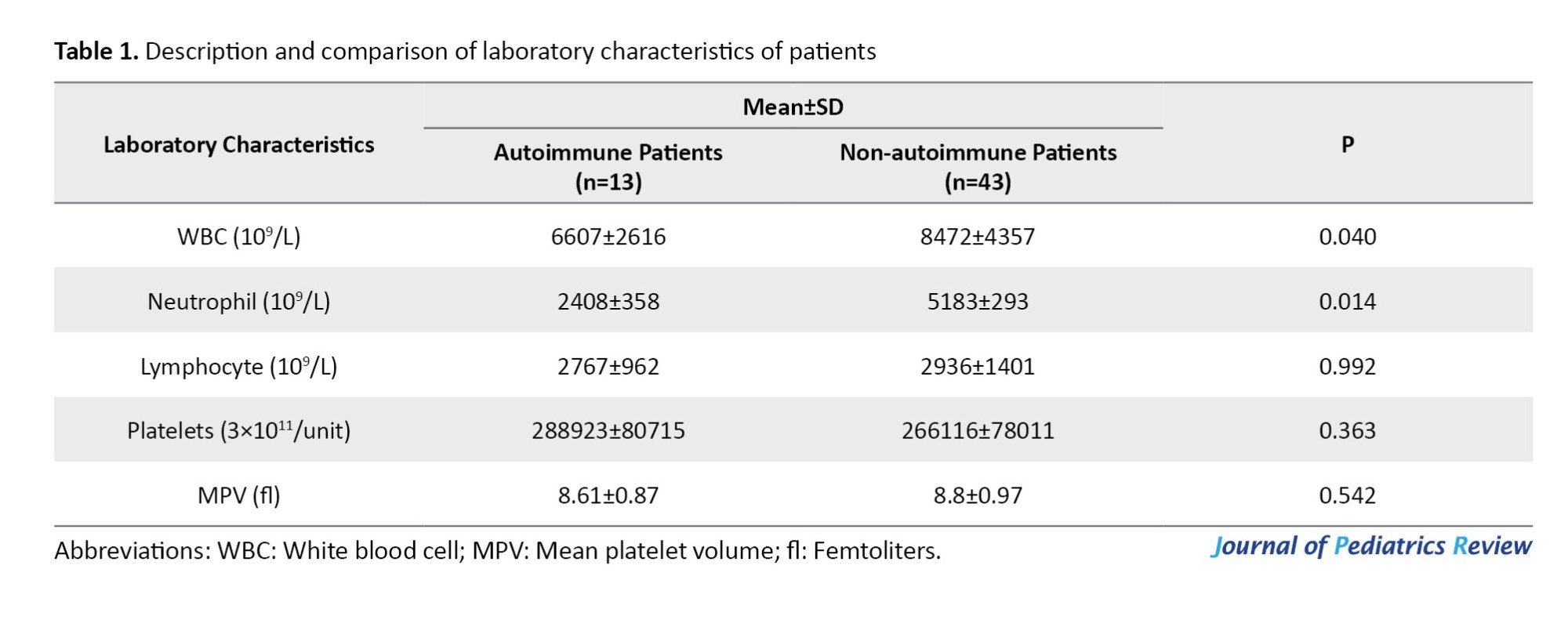
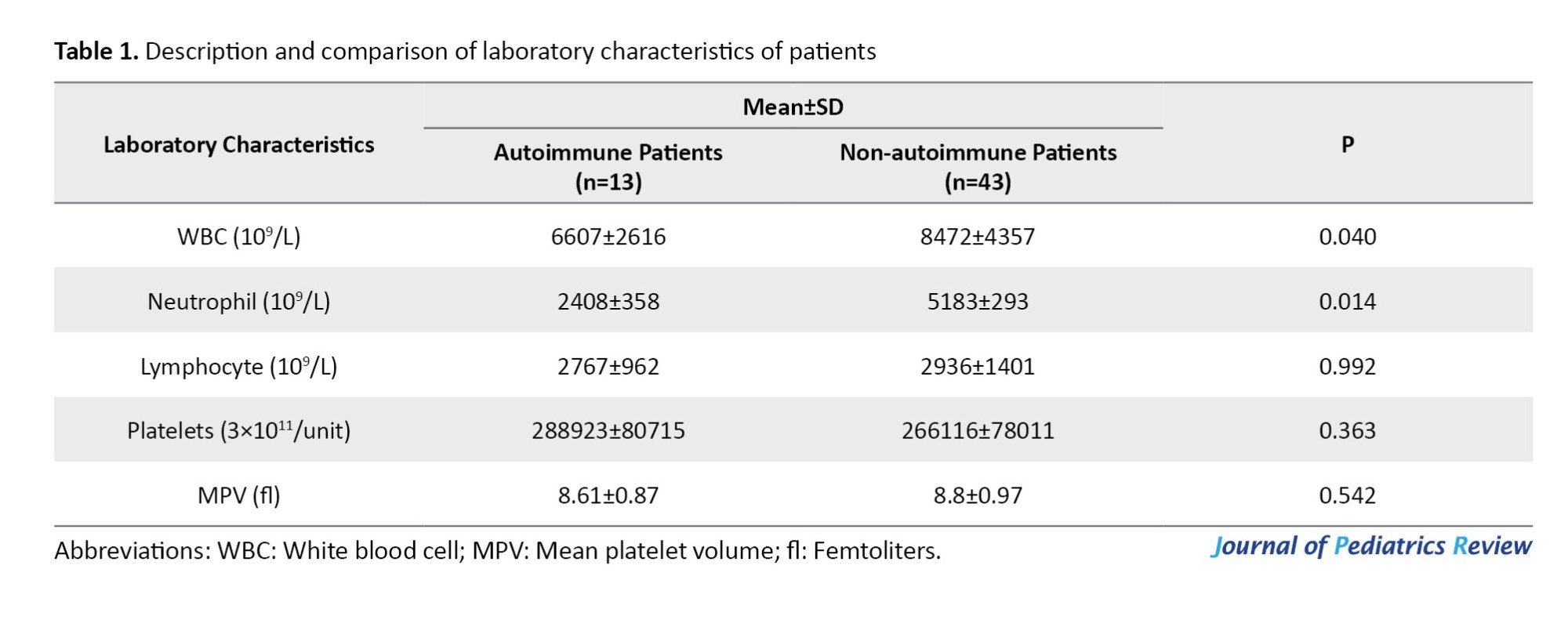
According to Table 1, the number of WBCs (P=0.040) and neutrophils (P=0.014) was significantly lower in the autoimmune group compared to the non-autoimmune group. Also, CRP was positive in 53.8% of patients in the autoimmune group (including 5 cases of +1 and 2 cases of +2), while in the non-autoimmune group, only 8 cases of type +1 were observed, and this difference was statistically significant. Leukocytosis higher than 11000/µL was observed in 7.7% of autoimmune patients (1 out of 13 patients) and 7% of non-autoimmune patients (3 out of 43 patients). Lymphopenia (lymphocytes <3000 for children less than 12 months and lymphocytes <1000 for children older than 12 months) was not observed in any of the studied children in either the autoimmune or non-autoimmune groups.
None of the fathers of autistic patients with autoimmunity were positive for CRP and ANA tests, while 15.4% of mothers (2 mothers) were positive for CRP and ANA tests. However, the two groups of fathers and mothers of autistic children with autoimmunity did not show a significant difference in terms of positive cases for CRP and ANA. The differences in the results of ANA, white blood cells, neutrophils, lymphocytes, platelets, and mean platelet volume were not significant between the two groups of fathers and mothers of children with autism (Table 2).

Discussion
ASD is a neurodevelopmental condition marked by deficits in social, cognitive, and behavioral aspects. Clinical signs of ASD involve challenges in social communication and interaction, sensory irregularities, repetitive actions, and different degrees of intellectual disability [10].
Maternal immune dysfunction might be the foundation for the behavioral irregularities seen in a portion of children impacted by the disorder [6]. Autoimmune disorders encompass a broad range of diseases that occur due to autoantibodies, which are produced as a result of excessive stimulation of the immune system exacerbated by insufficient activation of T and B cells [11].
In the present study, the number of WBCs (mean difference=-1864, P=0.040) and neutrophils (mean difference=-1603, P=0.014) in the group of autoimmune patients was significantly lower than in the non-autoimmune group. CRP was also positive in 53.8% of the autoimmune patients and 18.6% of non-autoimmune patients (P=0.013). None of the fathers of autistic patients with autoimmunity tested positive for CRP and anti-nuclear antibody tests, while 15.4% of mothers (2 mothers) were positive for both tests. The relationship between CBC and ASD remains unclear in different articles. Kulaksizoglu et al. [12] assessed CBC information in children with ASD, intending to investigate connections between ASD and inflammation. They found that neutrophil count and neutrophil/lymphocyte ratio (NLR) values were considerably elevated in ASD patients, which is in contrast to our findings. Also, Tural Hesapcioglu et al. evaluated CBC parameters in ASD patients in 2017, and showed significantly higher monocyte values and lower lymphocyte to monocyte ratio (LMR) [13]. Gazestani et al., identified a preserved dysregulated gene network through the examination of leukocyte transcriptomic data from toddlers aged 1 to 4 years with ASD, which can disrupt WBC genes [14].
The processes that result in the generation of anti-nucleosome-specific autoantibodies (ANA) in certain autoimmune disorders remain unclear; however, it has been noted that increased rates of apoptosis result in autoantibody formation. Additionally, nucleosomes may provoke the generation of interleukin-6 and activate lymphoproliferation and IgG production by splenic B cells. In a study, serum concentrations of anti-nucleosome-specific antibodies were elevated in certain autistic children, with significant concentrations observed in 46.7% of children with autism spectrum disorder. They also showed that the level of specific anti-nucleosome antibodies in autistic children from families with known autoimmune problems is significantly higher than in autistic children from healthy families [11].
In the present study, it was shown that nearly a quarter of autistic children had high levels of antinuclear antibodies in their serum. The level of specific anti-nucleosome antibodies in autistic children from families with known autoimmune problems is significantly higher than autistic children from healthy families, which is associated with an increased likelihood of ADHD in children [15].
Lee et al. showed that both parental autoimmune disorders were linked to a heightened probability of ADHD in youngsters. Nonetheless, solely paternal autoimmune disorders were linked to the risk of ASD in children [16]. In the present study, an increase in antinuclear antibodies was observed in only 15.4% of the mothers of children with ASD who had elevated ANA levels, and the ANA level was not increased in any of the fathers of these children. Consequently, the results of the current research are inconsistent with the findings of Lee et al.’s study. Regarding this observed disparity, it should be noted that the present study considered an increase in ANA levels above the normal range as an indicator of an autoimmune disorder. In contrast, the study by Lee et al. focused on specific cases of autoimmune diseases under follow-up in the parents of children with ASD.
Conclusion
There is a link between ASD and autoimmune disorders. However, additional studies are required with a broader group of patients to establish whether these antibodies contribute to the onset of autoimmunity in a specific subset of autistic children. Further investigations should be conducted to explore disease pathogenesis, and new therapeutic approaches such as gene therapy and immunotherapy could be very helpful. Given that the role of autoimmunity in autism is being discussed, utilizing diagnostic facilities for autoimmune patients and related treatments may also be effective in improving the symptoms of ASD.
Limitation
The difficulty of identifying patients with ASD in the community complicates coordination with the blood sampling process. There is a lack of studies on the level of cytokines in individuals and families of patients with autism spectrum disorder, as well as a lack of information about other necessary diagnostic procedures for autism spectrum patients (such as neuroimaging and cytokine testing).
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Golestan University of Medical Sciences, Gorgan, Iran (Code: IR.GOUMS.REC.1400.129).
Funding
This study was extracted from the PhD dissertation of Nasser Heravi, approved by the School of Medicine, Golestan University of Medical Sciences, Gorgan, Iran. This study was financially supported by Golestan University of Medical Sciences, Gorgan, Iran (Grant No.: 111416).
Authors contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results, and manuscript drafting. Each author approved the submission of the final version of the manuscript.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors are very grateful to all hospital authorities for their permission to conduct this study and for their various forms of cooperation.
References
Autism spectrum disorder (ASD) is a neurobiological condition shaped by genetic, epigenetic, and environmental elements, impacting the growing brain, and marked by impaired social and emotional interaction, difficulties in learning, axiety, epilepsy, language impairments, restrictive actions, and the existence of limited interests and repetitive actions. Reduced size of cells in the hippocampus and limbic system and an elevated number of prefrontal cortex neurons may be related to clinical manifestations. ASD patients also exhibit atypical development of the temporal and frontal lobes and reduced amygdala volume and gray matter in magnetic resonance imaging (MRI) findings [1].
The World Health Organization (WHO) approximates the worldwide occurrence of ASD at 0.76%; nevertheless, this represents merely around 16% of the total children worldwide. The occurrence of ASD is roughly 2.47%, 0.06%, and 0.36% in the USA, Iran, and Asia, respectively [2]. ASD is more predominant in males than in females. Y polysomies are more likely to exhibit autism compared to X chromosome polysomies, indicating the significance of Y chromosome genes in the development of ASD. Girls are less frequently diagnosed than boys, and those who do receive a diagnosis tend to have more intellectual and behavioral disabilities than boys with the diagnosis [3].
ASD is a disorder with a strong genetic basis that causes different phenotypic changes. Each gene mutation leads to different neuropsychiatric disorders. For example, IL1RAPL1, OPHN1, RELN, GluR6, GRIN2A, GRIN2B, CNTNAP2, GABRB3, 5-HTT, and TPH2 are associated with intellectual disability, schizophrenia, childhood absence epilepsy, depression, attention deficit hyperactivity disorder (ADHD), and major depression [4].
Multiple biochemical features are identified as biomarkers that increase the likelihood of ASD. One or more preliminary biomarkers recognized at birth (or earlier) can predict the subsequent emergence of a genuine autistic disorder, such as low serum IGF1, anti-myelin basic protein, increased serotonin, single-nucleotide polymorphism rs1801123, and single-nucleotide polymorphism rs878960 [5].
ASD also has an autoimmune aspect. The initial research suggested the notion that autoimmunity might be a significant cause of ASD, as outlined in a case report that documented a child with a substantial familial background of autoimmune conditions. Also, in recent studies, significant correlations were observed between ASD and additional autoimmune conditions, like celiac disease, hypothyroidism, type 1 diabetes, rheumatoid arthritis, and psoriasis [6].
Therefore, identifying immune mechanisms directly associated with ASD may facilitate the development of preventive measures and potentially lead to the discovery of novel therapeutic agents [7]. No medication has been demonstrated to be effective in addressing the primary symptoms of ASD. Risperidone and aripiprazole are the two drugs that have received approval from the Food and Drug Administration (FDA) for treating children and teenagers with ASD. Both help with irritability and stereotypical behaviors [8]. This study aimed to determine the frequency of autoimmunity in children with ASD and their parents in Gorgan.
Methods
The study with a cross-sectional design was carried out in Gorgan City, located in the northeast of Iran. The records and information related to all autism patients in Golestan Province in 2021 were reviewed, and all eligible patients were identified to be included in the study. Subjects were autistic patients covered by the Welfare Organization of Golestan Province.
This study used diagnostic and statistical manual of mental disorders, fifth edition (DSM-5) criteria as an inclusion criterion for ASD diagnosis, which is detailed below [9]:
A) Ongoing challenges in social communication and social interaction across various environments, including challenges in social-emotional reciprocity, non-verbal communication behaviors, and forming, sustaining, and comprehending relationships.
B) Limited, repetitive patterns of actions, interests, or pursuits.
C) Symptoms must be observable during the early developmental phase.
D) Symptoms lead to notable deterioration in social, work-related, or other crucial aspects of present functioning.
E) These disruptions are not better explained by cognitive impairment.
Informed consent was acquired from participants prior to serum collection. We collected 5 mL of venous blood from children with autism and their parents; from this amount, 2 mL of blood was used for complete blood count (CBC) measurements in tubes containing K2EDTA, and 3 mL of blood was poured into clot tubes for C-reactive protein (CRP) and antinuclear antibody (ANA) measurements. CBC measurements were performed using a Sysmax KX21N cell counter made in Japan. Then, the differential count of white blood cells was done using a light microscope with a 100x lens after preparing a blood smear and performing Giemsa staining.
The clot tube containing 3 mL of venous blood was centrifuged at 4500 rpm after being placed in a Bain-Marie at 37 °C for 15 minutes, and a clot formed in the centrifuge. After centrifugation, the serum was separated from the clot-containing blood cells, transferred into another tube, and stored in a freezer at -20 °C until the experiments were performed. ANA tests were performed using the enzyme linked immunosorbent assay (ELISA) method with the ANA-HEp2 ELISA kit from AESKULISA. Also, CRP tests were performed using the latex agglutination method using a kit made by Padco. Also, 5 mL of venous blood was taken from the parents of the patients whose ANA tests were positive, and all the mentioned tests were performed for them. All tests were conducted in the laboratory of Taleghani Hospital in Gorgan.
Statistical analysis
Mean±SD were used to describe quantitative information, while frequency and relative frequency were used to describe qualitative information. Data were analyzed using STATA software, version 17 software. To represent the quantitative variables, the Mean±SD was employed, while the frequency distribution table was utilized to present the count and percentage of instances for qualitative variables. Qualitative variables were analyzed using the chi-square and Fisher’s exact tests. The Mann-Whitney test was used to compare quantitative variables with qualitative variables due to the non-normality of data distribution. All tests were two-sided, and P<0.05 was considered statistically significant.
Results
Our investigation included a total of 56 individuals. The mean age of children was 10.04±3.99 years, with a range of 1-18 years. Also, the gender distribution of the children included in the study was 43 boys (76.8%) and 13 girls (23.2%). The difference in mean age of male and female patients was not statistically significant (P=0.368).
Based on the cut-off point of the ANA test (10 units/mL), patients were divided into two groups: Those with autoimmune disease (13 individuals; 23.21%) and those without autoimmune disease (43 individuals; 76.79%). ANA values in the two groups were significantly different (P<0.001). The mean ANA values in the autoimmune group were 23.02±6.49 units/mL, while in the non-autoimmune group, they were 4.01±1.66 units/mL (Figure 1).

According to Table 1, the number of WBCs (P=0.040) and neutrophils (P=0.014) was significantly lower in the autoimmune group compared to the non-autoimmune group. Also, CRP was positive in 53.8% of patients in the autoimmune group (including 5 cases of +1 and 2 cases of +2), while in the non-autoimmune group, only 8 cases of type +1 were observed, and this difference was statistically significant. Leukocytosis higher than 11000/µL was observed in 7.7% of autoimmune patients (1 out of 13 patients) and 7% of non-autoimmune patients (3 out of 43 patients). Lymphopenia (lymphocytes <3000 for children less than 12 months and lymphocytes <1000 for children older than 12 months) was not observed in any of the studied children in either the autoimmune or non-autoimmune groups.
None of the fathers of autistic patients with autoimmunity were positive for CRP and ANA tests, while 15.4% of mothers (2 mothers) were positive for CRP and ANA tests. However, the two groups of fathers and mothers of autistic children with autoimmunity did not show a significant difference in terms of positive cases for CRP and ANA. The differences in the results of ANA, white blood cells, neutrophils, lymphocytes, platelets, and mean platelet volume were not significant between the two groups of fathers and mothers of children with autism (Table 2).

Discussion
ASD is a neurodevelopmental condition marked by deficits in social, cognitive, and behavioral aspects. Clinical signs of ASD involve challenges in social communication and interaction, sensory irregularities, repetitive actions, and different degrees of intellectual disability [10].
Maternal immune dysfunction might be the foundation for the behavioral irregularities seen in a portion of children impacted by the disorder [6]. Autoimmune disorders encompass a broad range of diseases that occur due to autoantibodies, which are produced as a result of excessive stimulation of the immune system exacerbated by insufficient activation of T and B cells [11].
In the present study, the number of WBCs (mean difference=-1864, P=0.040) and neutrophils (mean difference=-1603, P=0.014) in the group of autoimmune patients was significantly lower than in the non-autoimmune group. CRP was also positive in 53.8% of the autoimmune patients and 18.6% of non-autoimmune patients (P=0.013). None of the fathers of autistic patients with autoimmunity tested positive for CRP and anti-nuclear antibody tests, while 15.4% of mothers (2 mothers) were positive for both tests. The relationship between CBC and ASD remains unclear in different articles. Kulaksizoglu et al. [12] assessed CBC information in children with ASD, intending to investigate connections between ASD and inflammation. They found that neutrophil count and neutrophil/lymphocyte ratio (NLR) values were considerably elevated in ASD patients, which is in contrast to our findings. Also, Tural Hesapcioglu et al. evaluated CBC parameters in ASD patients in 2017, and showed significantly higher monocyte values and lower lymphocyte to monocyte ratio (LMR) [13]. Gazestani et al., identified a preserved dysregulated gene network through the examination of leukocyte transcriptomic data from toddlers aged 1 to 4 years with ASD, which can disrupt WBC genes [14].
The processes that result in the generation of anti-nucleosome-specific autoantibodies (ANA) in certain autoimmune disorders remain unclear; however, it has been noted that increased rates of apoptosis result in autoantibody formation. Additionally, nucleosomes may provoke the generation of interleukin-6 and activate lymphoproliferation and IgG production by splenic B cells. In a study, serum concentrations of anti-nucleosome-specific antibodies were elevated in certain autistic children, with significant concentrations observed in 46.7% of children with autism spectrum disorder. They also showed that the level of specific anti-nucleosome antibodies in autistic children from families with known autoimmune problems is significantly higher than in autistic children from healthy families [11].
In the present study, it was shown that nearly a quarter of autistic children had high levels of antinuclear antibodies in their serum. The level of specific anti-nucleosome antibodies in autistic children from families with known autoimmune problems is significantly higher than autistic children from healthy families, which is associated with an increased likelihood of ADHD in children [15].
Lee et al. showed that both parental autoimmune disorders were linked to a heightened probability of ADHD in youngsters. Nonetheless, solely paternal autoimmune disorders were linked to the risk of ASD in children [16]. In the present study, an increase in antinuclear antibodies was observed in only 15.4% of the mothers of children with ASD who had elevated ANA levels, and the ANA level was not increased in any of the fathers of these children. Consequently, the results of the current research are inconsistent with the findings of Lee et al.’s study. Regarding this observed disparity, it should be noted that the present study considered an increase in ANA levels above the normal range as an indicator of an autoimmune disorder. In contrast, the study by Lee et al. focused on specific cases of autoimmune diseases under follow-up in the parents of children with ASD.
Conclusion
There is a link between ASD and autoimmune disorders. However, additional studies are required with a broader group of patients to establish whether these antibodies contribute to the onset of autoimmunity in a specific subset of autistic children. Further investigations should be conducted to explore disease pathogenesis, and new therapeutic approaches such as gene therapy and immunotherapy could be very helpful. Given that the role of autoimmunity in autism is being discussed, utilizing diagnostic facilities for autoimmune patients and related treatments may also be effective in improving the symptoms of ASD.
Limitation
The difficulty of identifying patients with ASD in the community complicates coordination with the blood sampling process. There is a lack of studies on the level of cytokines in individuals and families of patients with autism spectrum disorder, as well as a lack of information about other necessary diagnostic procedures for autism spectrum patients (such as neuroimaging and cytokine testing).
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Golestan University of Medical Sciences, Gorgan, Iran (Code: IR.GOUMS.REC.1400.129).
Funding
This study was extracted from the PhD dissertation of Nasser Heravi, approved by the School of Medicine, Golestan University of Medical Sciences, Gorgan, Iran. This study was financially supported by Golestan University of Medical Sciences, Gorgan, Iran (Grant No.: 111416).
Authors contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results, and manuscript drafting. Each author approved the submission of the final version of the manuscript.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors are very grateful to all hospital authorities for their permission to conduct this study and for their various forms of cooperation.
References
- Mukherjee SB. Autism spectrum disorders-Diagnosis and management. Indian J Pediatr. 2017; 84(4):307-14. [DOI:10.1007/s12098-016-2272-2] [PMID]
- Baxter AJ, Brugha TS, Erskine HE, Scheurer RW, Vos T, Scott JG. The epidemiology and global burden of autism spectrum disorders. Psychol Med. 2015; 45(3):601-13. [DOI:10.1017/S003329171400172X] [PMID]
- Tartaglia NR, Wilson R, Miller JS, Rafalko J, Cordeiro L, Davis S, et al. Autism spectrum disorder in males with sex chromosome aneuploidy: XXY/Klinefelter syndrome, XYY, and XXYY. J Dev Behav Pediatr. 2017; 38(3):197-207. [DOI:10.1097/DBP.0000000000000429] [PMID] [PMCID]
- Won H, Mah W, Kim E. Autism spectrum disorder causes, mechanisms, and treatments: Focus on neuronal synapses. Front Mol Neurosci. 2013; 6:19. [DOI:10.3389/fnmol.2013.00019] [PMID] [PMCID]
- Steinman G, Mankuta D. Molecular biology of autism's etiology - An alternative mechanism. Med Hypotheses. 2019; 130:109272. [DOI:10.1016/j.mehy.2019.109272] [PMID]
- Edmiston E, Ashwood P, Van de Water J. Autoimmunity, autoantibodies, and autism spectrum disorder. Biol Psychiatry. 2017; 81(5):383-90. [DOI:10.1016/j.biopsych.2016.08.031] [PMID] [PMCID]
- Marchezan J. Editorial: Autism spectrum disorder and autoimmune diseases: A pathway in common? J Am Acad Child Adolesc Psychiatry. 2019; 58(5):481-3. [DOI:10.1016/j.jaac.2019.03.014] [PMID]
- Goel R, Hong JS, Findling RL, Ji NY. An update on pharmacotherapy of autism spectrum disorder in children and adolescents. Int Rev Psychiatry. 2018; 30(1):78-95. [DOI:10.1080/09540261.2018.1458706] [PMID]
- Constantino JN, Charman T. Diagnosis of autism spectrum disorder: Reconciling the syndrome, its diverse origins, and variation in expression. Lancet Neurol. 2016; 15(3):279-91. [DOI:10.1016/S1474-4422(15)00151-9] [PMID]
- Lord C, Brugha TS, Charman T, Cusack J, Dumas G, Frazier T, et al. Autism spectrum disorder. Nat Rev Dis Primers. 2020; 6(1):5. [DOI:10.1038/s41572-019-0138-4] [PMID] [PMCID]
- Lee KH, Ahn BS, Cha D, Jang WW, Choi E, Park S, et al. Understanding the immunopathogenesis of autoimmune diseases by animal studies using gene modulation: A comprehensive review. Autoimmun Rev. 2020; 19(3):102469. [DOI:10.1016/j.autrev.2020.102469] [PMID]
- Kulaksizoglu S, Koparan C. High neutrophil to lymphocyte ratio and low mean platelet volume level in autism spectrum disorders. Ann Med Res. 2019; 26(10):2382-5. [DOI:10.5455/annalsmedres.2019.09.550]
- Tural Hesapcioglu S, Kasak M, Cıtak Kurt AN, Ceylan MF. High monocyte level and low lymphocyte to monocyte ratio in autism spectrum disorders. Int J Dev Disabil. 2017; 65(2):73-81. [DOI:10.1080/20473869.2017.1371369] [PMID] [PMCID]
- Gazestani VH, Pramparo T, Nalabolu S, Kellman BP, Murray S, Lopez L, et al. A perturbed gene network containing PI3K-AKT, RAS-ERK and WNT-β-catenin pathways in leukocytes is linked to ASD genetics and symptom severity. Nat Neurosci. 2019; 22(10):1624-34. [DOI:10.1038/s41593-019-0489-x] [PMID] [PMCID]
- AL-Ayadhi LY, Mostafa GA. Serum antinucleosome-specific antibody as a marker of autoimmunity in children with autism. J Neuroinflammation. 2014; 11:69. [DOI:10.1186/1742-2094-11-69] [PMID] [PMCID]
- Lee H, Hsu JW, Tsai SJ, Huang KL, Bai YM, Su TP, et al. Risk of attention deficit hyperactivity and autism spectrum disorders among the children of parents with autoimmune diseases: A nationwide birth cohort study. Eur Child Adolesc Psychiatry. 2023; 32(2):283-91. [DOI:10.1007/s00787-021-01860-0] [PMID]
Type of Study: Original Article |
Subject:
Clinical Psychology
Received: 2024/06/26 | Accepted: 2024/07/13 | Published: 2025/07/19
Received: 2024/06/26 | Accepted: 2024/07/13 | Published: 2025/07/19
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









