Volume 12, Issue 4 (10-2024)
J. Pediatr. Rev 2024, 12(4): 301-310 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kalat H L, Mohammadi M H, Sorouri S, Kharazmi H A, Ramazanian Bafghi Z, Ghazanfarpour M et al . Investigating the Effect of Olfactory Stimulation in Preterm Infants: A Review Study. J. Pediatr. Rev 2024; 12 (4) :301-310
URL: http://jpr.mazums.ac.ir/article-1-651-en.html
URL: http://jpr.mazums.ac.ir/article-1-651-en.html
Hashem Lashgari Kalat *1 

 , Mohammad Hasan Mohammadi2
, Mohammad Hasan Mohammadi2 

 , Shahabaddin Sorouri3
, Shahabaddin Sorouri3 

 , Hossein Ali Kharazmi4
, Hossein Ali Kharazmi4 

 , Zahra Ramazanian Bafghi5
, Zahra Ramazanian Bafghi5 

 , Masumeh Ghazanfarpour6
, Masumeh Ghazanfarpour6 

 , Najmeh Soltani Nejad7
, Najmeh Soltani Nejad7 




 , Mohammad Hasan Mohammadi2
, Mohammad Hasan Mohammadi2 

 , Shahabaddin Sorouri3
, Shahabaddin Sorouri3 

 , Hossein Ali Kharazmi4
, Hossein Ali Kharazmi4 

 , Zahra Ramazanian Bafghi5
, Zahra Ramazanian Bafghi5 

 , Masumeh Ghazanfarpour6
, Masumeh Ghazanfarpour6 

 , Najmeh Soltani Nejad7
, Najmeh Soltani Nejad7 


1- Department of Pediatrics, Clinical Research Development Center of Children’s Hospital, Hormozgan University of Medical Science, Bandar Abbas, Iran. , ghazanfarpour@yahoo.com
2- Department of Pediatrics, Faculty of Medicine, Zabol University of Medical Sciences, Zabol, Iran.
3- Lung Diseases Research Center, Faculty of Medicine, Mashhad University of Medical Science, Mashhad, Iran.
4- Department of Pediatrics, Clinical Research Development Center of Children’s Hospital, Hormozgan University of Medical Science, Bandar Abbas, Iran.
5- Student Research Committee, Razi Faculty of Nursing and Midwifery, Kerman University of Medical Sciences, Kerman, Iran.
6- Reproductive and Family Health Research Center, Kerman University of Medical Sciences, Kerman, Iran.
7- Department of Pediatrics, Afzalipour Faculty of Medicine, Kerman University of Medical Sciences, Kerman, Iran.
2- Department of Pediatrics, Faculty of Medicine, Zabol University of Medical Sciences, Zabol, Iran.
3- Lung Diseases Research Center, Faculty of Medicine, Mashhad University of Medical Science, Mashhad, Iran.
4- Department of Pediatrics, Clinical Research Development Center of Children’s Hospital, Hormozgan University of Medical Science, Bandar Abbas, Iran.
5- Student Research Committee, Razi Faculty of Nursing and Midwifery, Kerman University of Medical Sciences, Kerman, Iran.
6- Reproductive and Family Health Research Center, Kerman University of Medical Sciences, Kerman, Iran.
7- Department of Pediatrics, Afzalipour Faculty of Medicine, Kerman University of Medical Sciences, Kerman, Iran.
Full-Text [PDF 445 kb]
(744 Downloads)
| Abstract (HTML) (1723 Views)
Full-Text: (771 Views)
Introduction
Premature birth, described as under 37 weeks of gestation, increases the likelihood of fatality and morbidity due to respiratory immaturity and ineffectual oral feeding performance [1]. In the neonatal intensive care unit, premature infants are frequently exposed to painful procedures during the first days [1, 2]. Also, infants are exposed to several negative olfactory stimuli including strong perfumes or scented aftershave, alcohol, cleaning chemicals, alcohol-based hand rubs, and oral remedies. These odors must be curtailed with a positive stimulus, such as breastfeeding-related substances as well as materials with parental smell utilized as a counterbalance [3]. The olfactory and gustatory receptors develop by the eighth week of gestation and become functional by the 24th and 17th weeks, respectively [4]. According to several studies, olfactory stimulation could alleviate pain and neonatal crying during painful procedures by releasing fragrances and other familiar aromas, such as the mother’s milk and amniotic odor [5], can mark a sooner transition from the feeding tube to efficient oral feeding [6], mediates the apnea.
Besides respiratory problems, the lack of or inefficient oral feeding performance is a major problem facing premature newborns [6]. Researchers and clinicians need to be cognizant of procedures and positive olfactory stimuli mediating major problems and more adaptable premature infants to the neonatal intensive care unit and hospital environments. Accordingly, it is essential to undertake a comprehensive review of the effect of aromatherapy on apnea, the transition from tube feeding (gavage) to oral feeding, pain, growth, and duration of hospital stay.
Methods
The major English databases, such as PubMed, Embase, Scopus, Cochrane Library and Web of Science, were systematically reviewed without any time restrictions up to April 12, 2022. The search keywords were as follows: ([Preterm infant*] OR [premature infant*] OR [preterm newborn] OR [premature newborn] OR [premature neonate*] OR [preterm neonate*] OR [premature baby] OR [preterm baby] OR (prematurity]) AND ([aromatherapy] OR [olfactometer] OR [olfactory stimulation] OR [aroma] OR [odor]).
All the clinical trials assessed the effect of the aroma on variables, such as apnea, the transition from tube feeding (gavage) to oral feeding, pain, growth, and duration of hospital stay.
Inclusion and exclusion criteria
All clinical trials that investigated the effect of the aroma on variables such as apnea, transition time to oral feeding, pain, growth, and duration of hospital stay in preterm infants were included in the study. Preterm infants were considered birth less than 37 weeks of gestational age. Only interventions that used olfactory sense were included in the study. Non-English articles, letters to the editor, reviews, non-human studies and multi-sensorial intervention studies were excluded. Two researchers independently evaluated study eligibility. Disagreements were resolved by consensus, which required the reviewers to discuss the reasoning for their decisions.
Data extraction
Data extraction was done independently by two of the authors using pre-piloted forms. The accuracy of the data was subsequently adjudicated by a third reviewer. The Table 1 list the considered parameters, including the first author, the year of publication, the location and type of study, gestational age and infant weight at birth.
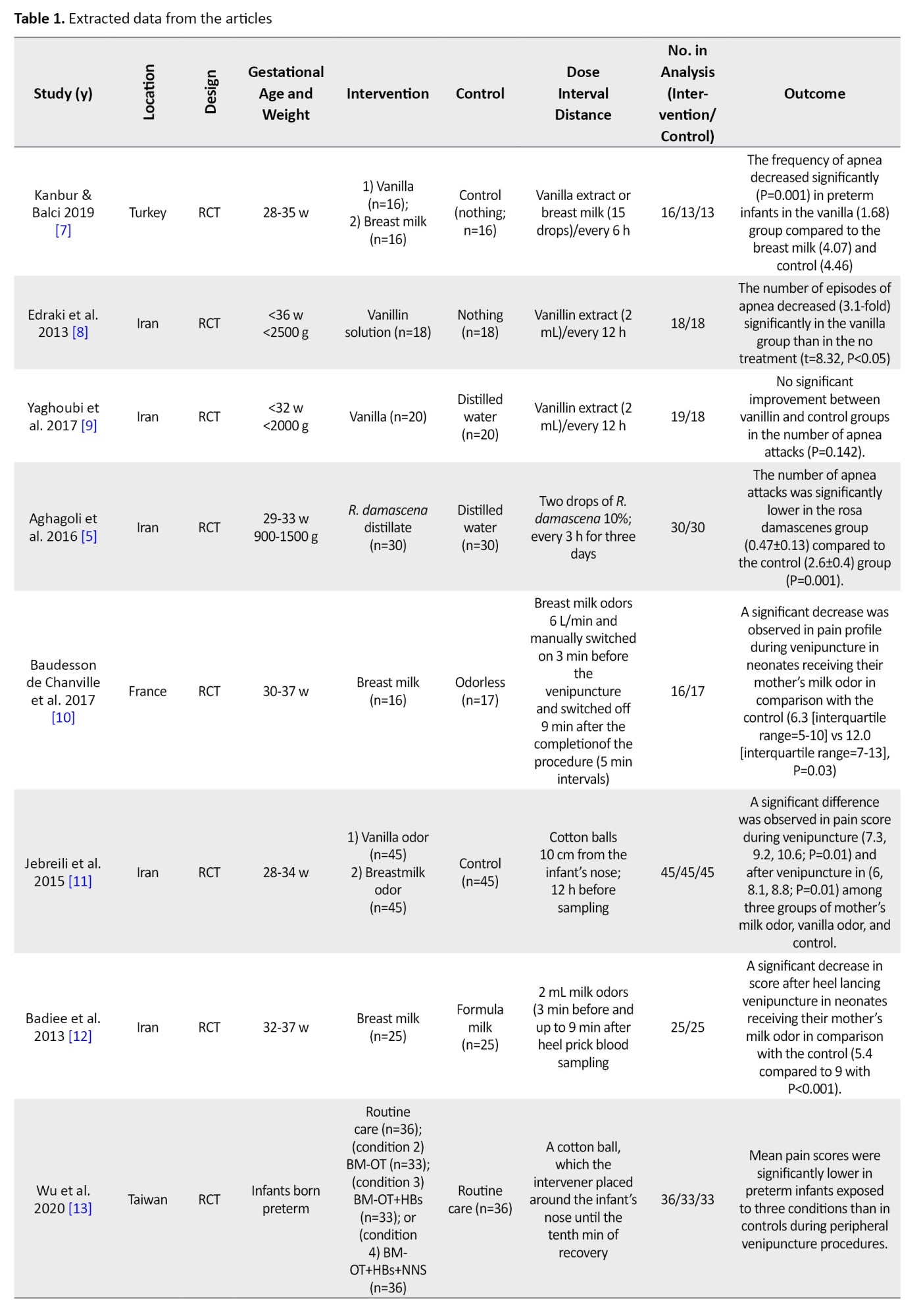

Other characteristics of subjects were Apgar score, hemoglobin, stability or instability of neonate, intervention and control groups, aroma dose, intervention intervals, aroma distance from the infant’s nose, and outcomes.
Quality assessment
The Jaded scale is a validated scale and was used to assess the risk of bias in the study. The quality of studies was evaluated according to the Jaded scale. It consisted of 8 items, as shown in Table 2.
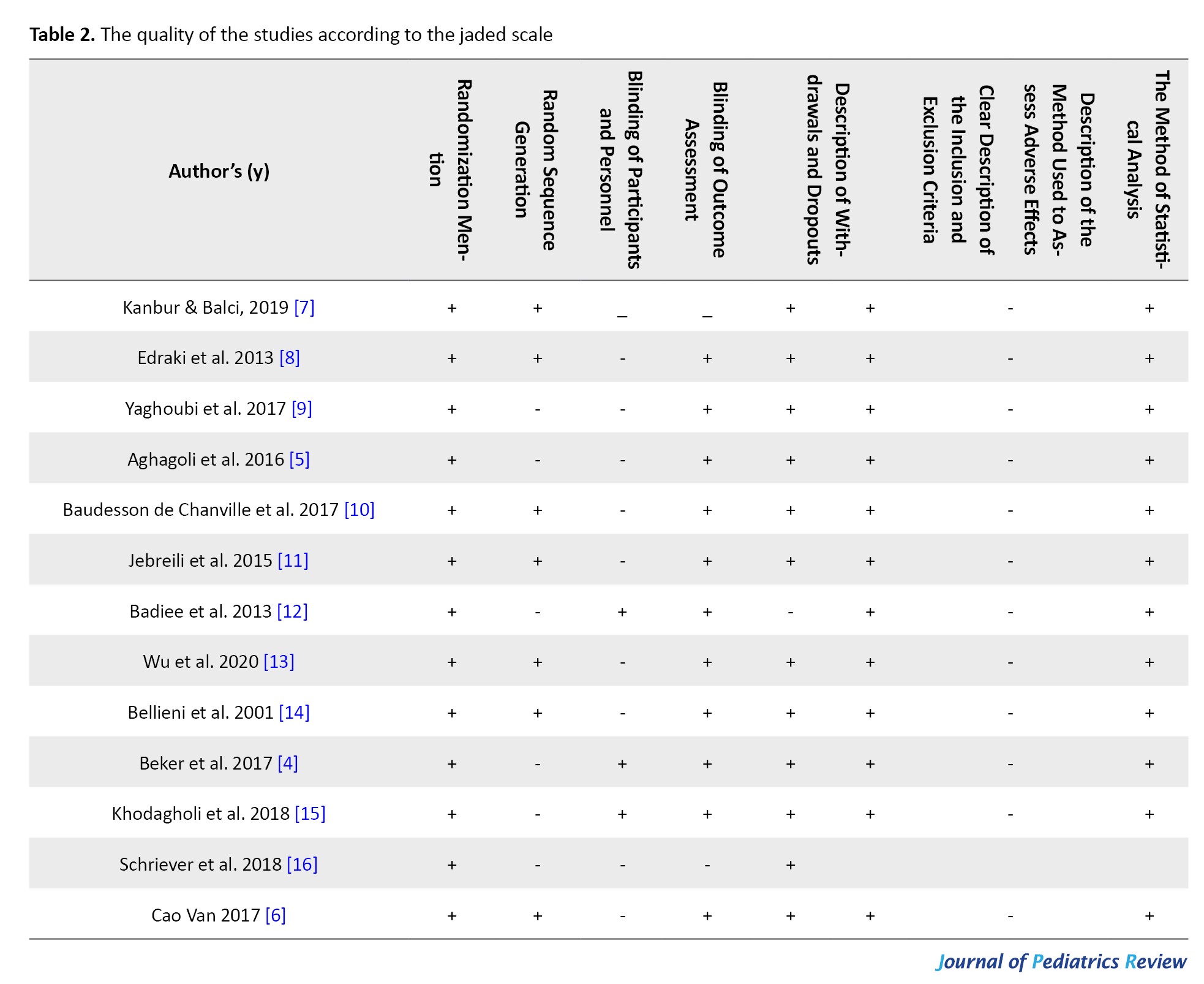
The methodological quality of the studies was assessed independently by the two authors. Disagreements between the assessors were subsequently adjudicated by a third reviewer (Table 2).
Results
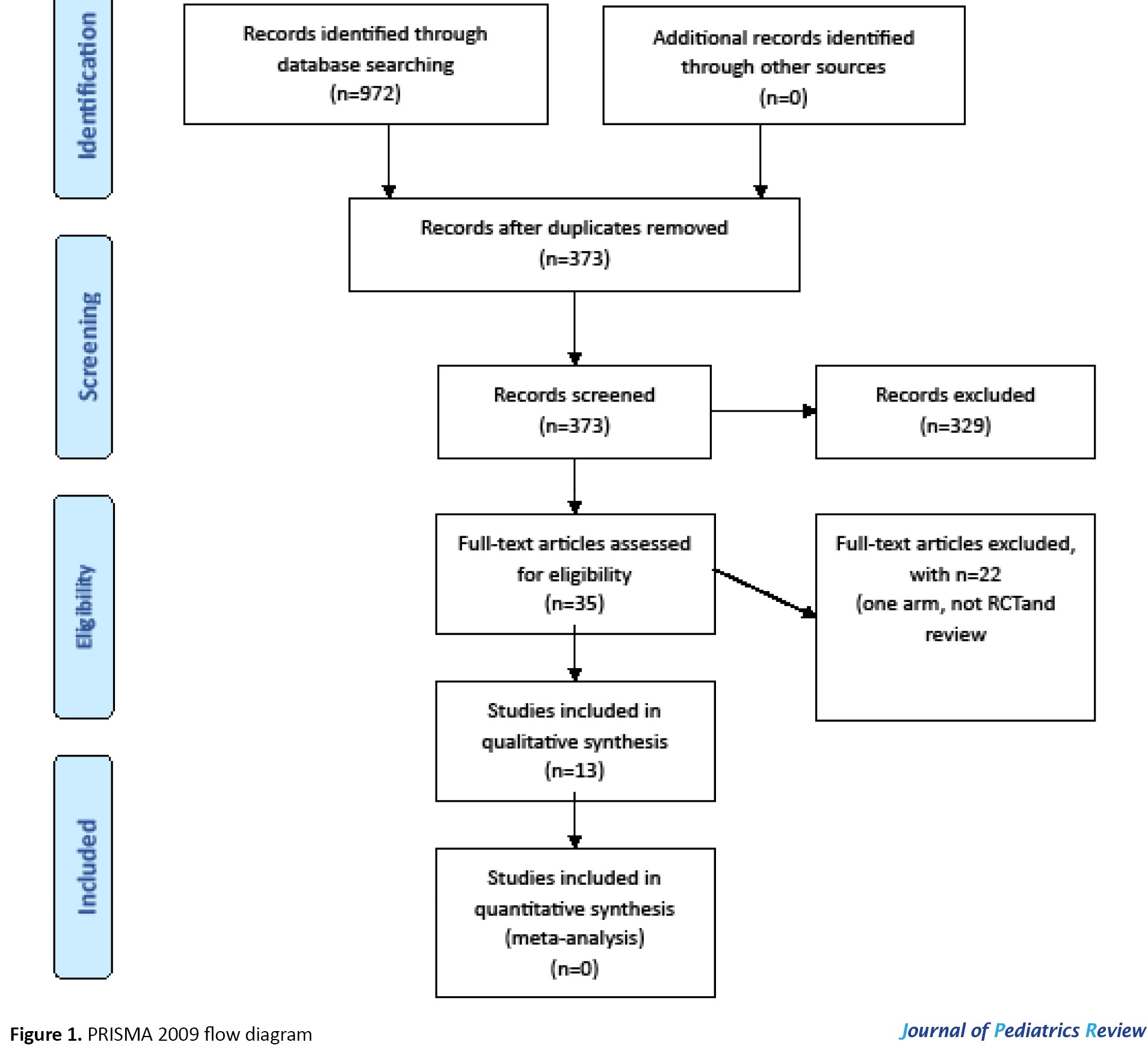
A total of 927 titles were retrieved from a main database search. In addition, none of the trials were identified by hand-searched of the bibliographies of relevant articles. After removing duplicates, 347 trials remained of which 312 studies that were excluded because they did not meet the inclusion criteria based on title and abstract. The full text of the remaining 35 studies was reviewed, and another 22 studies were excluded because they did not meet the inclusion criteria. Finally, 13 studies were included in the review (Figure 1).
The effect of aromatherapy on apnea
Studies assessed the effect of aromatherapy with vanilla, breast milk, and Rosa damascenes on apnea. Two studies assessed the effect of aromatherapy with vanilla on apnea. The frequency of apnea decreased significantly in preterm infants in the vanilla group than in the breast milk and control [7] and no treatment (P<0.05) [8]. In contrast in Yaghoubi et al.’s study, the number of apnea attacks did not change after treatment with Vanilla control (P=0.142) [9]. In the study by Aghagoli et al. (2016) the number of apnea attacks was significantly lower in the Rosa damascenes group than control (distilled water) (P<0.05) [5].
The effect of aromatherapy on painful procedures
Three studies showed a significant decrease in premature infant pain profile score after heel lancing during venipuncture and after venipuncture in neonates receiving their mother’s milk odor in comparison with the control [10-12].
According to Wu et al. (2020) mean pain scores were significantly lower in preterm infants exposed to breast milk odor (n=36) or heartbeat sounds (HBs) + BM odor (n=33) or BM odor + non-nutritive sucking (NNS) + HBs (n=36) compared to the controls (routine care; n=36) during peripheral venipuncture procedures [13]. One study assessed the effect of sensorial saturation (SS) on painful procedures preterm infants were randomized into five different procedures: control, 10% oral glucose plus sucking, SS, oral water, and 10% oral glucose. SS is a multisensorial stimulation consisting of delicate tactile, vestibular, gustative, olfactory, auditory, and visual stimuli. SS has a greater analgesic effect on heel prick in preterm infants in comparison with control and sucking + oral glucose groups (P<0.001) [14].
Aromatherapy on transition from tube feeding (gavage) to oral feeding
Two studies assessed the effect of breast milk odor and one study assessed the effect of vanilla odor or rose on transition from tube feeding to oral feeding. In Beker et al.’s study, preterm infants were exposed to either the smell or taste of milk before each feed reached full enteral feeds at a shorter time (13.5 days) than no exposure group (15.5 days); however, the difference between the two groups was non-significant (P=0.1) [4]. In Khodagholi et al., study, milk odor in combination with NNS compared to alone NNS decreased transition feeding time to oral feeding (P=0.07) [15]. In Schriever et al.’s study, infants preterm exposed to the vanilla odor than the control group indicated a faster transition from tube feeding to oral feeding but, the difference was not significant between rose odor and control [16].
Aromatherapy on hospital discharge
In Cao Van et al.’s study [6], the length of hospitalization was shorter in infants stimulated with anise or cinnamon (group A) than odorless stimulation (control group). However, it was non-significant (P=0.12). In Khodagholi et al, milk odor in combination with NNS compared to NNS alone decreased hospital discharge time(P=0.07) [15].
Discussion
According to this review, olfactory stimulation by some pleasant odors was effective on painful procedures and apnea attacks in preterm infants. Meanwhile, hospital discharge time and transition time from tube feeding to oral feeding were shorter. However, the results were insignificant.
This review found that there are controversial results about the aromatherapy effect of pleasant odor vanillin on apnea attacks in preterm infants [8]. Rosa damascenes odor had a therapeutic effect on apnea attacks [23], but not other odors [5]. Recently, two systematic reviews reported consistent results with significant effects on apnea attacks in preterm infants. The first systematic review with three studies has shown that aromatherapy is effective in treating apnea in preterm infants. However, due to the small sample size and low number of studies included in their systematic review, the authors reiterated that their findings should be interpreted with caution [17]. The second systematic review and meta-analysis showed that the treatment with aromatherapy can significantly decrease apnea attacks compared to the control in the preterm infant [18]. According to our research aromatherapy with vanillin has a preventing [9] and therapeutic effect [7] on apneas episodes in preterm infants. In addition, regarding the multidimensional effect of vanillin, first, it may run through the nasal mucosa and enroll in the brain through the bloodstream. Second, the vanillin can improve orbitofrontal blood flow. Third, vanillin helps the newborns deal with the stress [8]. Fourth, vanillin probably has pharmacological properties; therefore, it can directly and indirectly affect the respiratory centers. In a study, the number of apnea attacks was significantly lower in the R. damascenes group compared to the control (distilled water; P<0.05) [5]. The extract of R. damascena stimulates axons and dendrites in the nervous system [19]. Moreover, the hydro-alcoholic extract of R. damascenes has a dilatory effect on respiratory airways [5, 20].
According to our review, BM and the vanillin odor were effective in preterm infants’ venipuncture [3, 4, 13] that is consistent with previous systematic reviews addressing the effect of pleasant odor on painful procedures. A systematic review showed aromatherapy with lavender could decrease painful procedures in infants and children [21]. A meta-analysis with eight randomized controlled trials involving 453 participants conducted by Zhang in 2018 showed that BM odor significantly decreased pain scores in newborns with large effect sizes for painful procedures [22]. Another systematic review was published by Norouziasl et al. and concluded that aromatherapy with the mother’s milk, vanilla and the mother’s odor could lessen painful procedures and improve physiological parameters [23].
According to a study, aromatherapy with anise or cinnamon led to a sudden transition from the feeding tube to effectual oral feeding in premature infants [6]. Moreover, cinnamon contains expressive anti-allergic, anti-ulcerogenic, antipyretic, anesthetic, and analgesic characteristics. It also has medicinal applications due to its strong aromatic, sweet, and warm odor or food additives [24]. The anise essential oil boosts the production of BM, expedites milk secretion, and acts as a diuretic substance. The anise seeds consist of anethole, which is a debilitated estrogenic agent. Given its role as a dopamine receptor antagonist, it could be activated by prolactin secretion increment [25].
However, published clinical studies reported controversial results about this effect, According to our study, infants exposed to milk odor transitioned from tube feeding to oral feeding 2-10 days earlier. However, the results were insignificant. The results of a systematic review of two studies revealed that exposure to the smell and taste of milk with gastric or nasogastric tube feedings had no clear effect on the time to reach full sucking feeds and full tube feeding [26]. Findings of a meta-analysis with 8 studies revealed that in comparison to the control group, infants preterm exposed to either pleasant odors or BM odor transitioned from tube feeding to oral feeding earlier [27]. Smell and taste play a significant role in improving digestion and absorption of food. Therefore, providing some milk for the infant to smell and taste via an orogastric or nasogastric tube can potentially bolster their ability to tolerate greater volumes of milk quickly.
The results of our review of three studies concluded there was no evidence of a clear effect of exposure to pleasant odors such as anise cinnamon or milk odor on hospital discharge time and weight at discharge in preterm infants. Inconsistent with our results, a systematic review of two studies revealed exposure to the smell and taste of milk with an orogastric or nasogastric tube may decrease the length of hospitalization in preterm infants [26].
Conclusion
Olfactory stimulation by some pleasant odors can help improve apnea attacks in preterm infants. Olfactory stimulation by milk odor is a safe, non-invasive and family-friendly intervention in improving painful procedures in preterm infants. The results were not conclusive although it was found that infants preterm exposed to pleasant odors had a shorter transition time from tube feeding to oral feeding and discharge earlier in the day.
Limitations and suggestions for future studies
This study faced some limitations of this study. First of all, the studies included in our systematic review had a small sample size. Second, only one kind of apnea, i.e. the idiopathic apnea of prematurity, has been studied in newborns. Hence, it is required to conduct further investigation to verify the effectiveness of this non-pharmacological method in various types of apnea. Despite randomization, the gender distribution was not balanced. Hence, it was obvious that male gender exhibited a higher disadvantage in premature infants. A review of literature male and female infants respond differentially to environmental stimuli, with different growth and neurodevelopmental trajectories. No study included in our review assessed sexually dimorphic response to aromatherapy on painful producers. Future studies should be conducted as systematic reviews with meta-analyses on this topic to address the gaps in knowledge identified from the results of this review.
Ethical Considerations
Compliance with ethical guidelines
This article is a meta-analysis with no human or animal sample.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization, project administration, and funding acquisition: Masumeh Ghazanfarpour, Mohammad Hasan Mohammadi, and Hashem Lashgari Kalat; Methodology: Zahra Ramazanian Bafghi, Shahabaddin Sorouri, Hossein Ali Kharazmi, Najmeh Soltani Nejad, Mohammad Hasan Mohammadi and Hashem Lashgari Kalat; Software: Hashem Lashgari Kalat, Masumeh Ghazanfarpour and Shahabaddin Sorouri; Validation and supervision: Shahabaddin Sorouri, Hossein Ali Kharazmi, Hashem Lashgari Kalat and Mohammad Hasan Mohammadi; Formal analysis: Zahra Ramazanian Bafghi, Najmeh Soltani Nejad and Masumeh Ghazanfarpour; Investigation: Hashem Lashgari Kalat, Masumeh Ghazanfarpour and Mohammad Hasan Mohammadi; Resources: Shahabaddin Sorouri, Hossein Ali Kharazmi, Najmeh Soltani Nejad and Hashem Lashgari Kalat; Data curation: Shahabaddin Sorouri, Hossein Ali Kharazmi, Mohammad Hasan Mohammadi and Hashem Lashgari Kalat; Writing the original draft: Hashem Lashgari Kalat, Shahabaddin Sorouri, Hossein Ali Kharazmi and Mohammad Hasan Mohammadi; Review and editing: All authors.
Conflicts of interest
The authors declared no conflict of interest.
Premature birth, described as under 37 weeks of gestation, increases the likelihood of fatality and morbidity due to respiratory immaturity and ineffectual oral feeding performance [1]. In the neonatal intensive care unit, premature infants are frequently exposed to painful procedures during the first days [1, 2]. Also, infants are exposed to several negative olfactory stimuli including strong perfumes or scented aftershave, alcohol, cleaning chemicals, alcohol-based hand rubs, and oral remedies. These odors must be curtailed with a positive stimulus, such as breastfeeding-related substances as well as materials with parental smell utilized as a counterbalance [3]. The olfactory and gustatory receptors develop by the eighth week of gestation and become functional by the 24th and 17th weeks, respectively [4]. According to several studies, olfactory stimulation could alleviate pain and neonatal crying during painful procedures by releasing fragrances and other familiar aromas, such as the mother’s milk and amniotic odor [5], can mark a sooner transition from the feeding tube to efficient oral feeding [6], mediates the apnea.
Besides respiratory problems, the lack of or inefficient oral feeding performance is a major problem facing premature newborns [6]. Researchers and clinicians need to be cognizant of procedures and positive olfactory stimuli mediating major problems and more adaptable premature infants to the neonatal intensive care unit and hospital environments. Accordingly, it is essential to undertake a comprehensive review of the effect of aromatherapy on apnea, the transition from tube feeding (gavage) to oral feeding, pain, growth, and duration of hospital stay.
Methods
The major English databases, such as PubMed, Embase, Scopus, Cochrane Library and Web of Science, were systematically reviewed without any time restrictions up to April 12, 2022. The search keywords were as follows: ([Preterm infant*] OR [premature infant*] OR [preterm newborn] OR [premature newborn] OR [premature neonate*] OR [preterm neonate*] OR [premature baby] OR [preterm baby] OR (prematurity]) AND ([aromatherapy] OR [olfactometer] OR [olfactory stimulation] OR [aroma] OR [odor]).
All the clinical trials assessed the effect of the aroma on variables, such as apnea, the transition from tube feeding (gavage) to oral feeding, pain, growth, and duration of hospital stay.
Inclusion and exclusion criteria
All clinical trials that investigated the effect of the aroma on variables such as apnea, transition time to oral feeding, pain, growth, and duration of hospital stay in preterm infants were included in the study. Preterm infants were considered birth less than 37 weeks of gestational age. Only interventions that used olfactory sense were included in the study. Non-English articles, letters to the editor, reviews, non-human studies and multi-sensorial intervention studies were excluded. Two researchers independently evaluated study eligibility. Disagreements were resolved by consensus, which required the reviewers to discuss the reasoning for their decisions.
Data extraction
Data extraction was done independently by two of the authors using pre-piloted forms. The accuracy of the data was subsequently adjudicated by a third reviewer. The Table 1 list the considered parameters, including the first author, the year of publication, the location and type of study, gestational age and infant weight at birth.
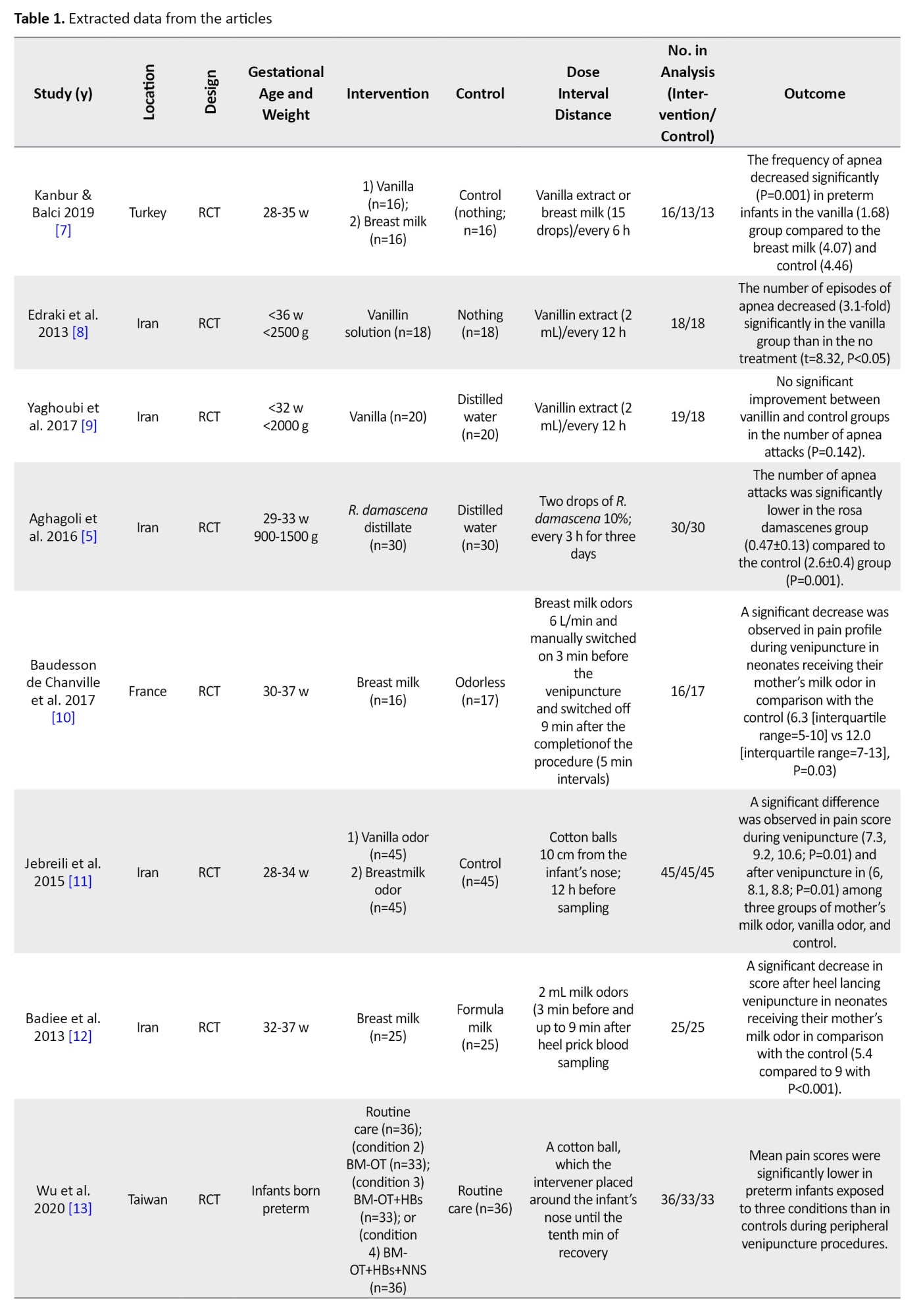

Other characteristics of subjects were Apgar score, hemoglobin, stability or instability of neonate, intervention and control groups, aroma dose, intervention intervals, aroma distance from the infant’s nose, and outcomes.
Quality assessment
The Jaded scale is a validated scale and was used to assess the risk of bias in the study. The quality of studies was evaluated according to the Jaded scale. It consisted of 8 items, as shown in Table 2.
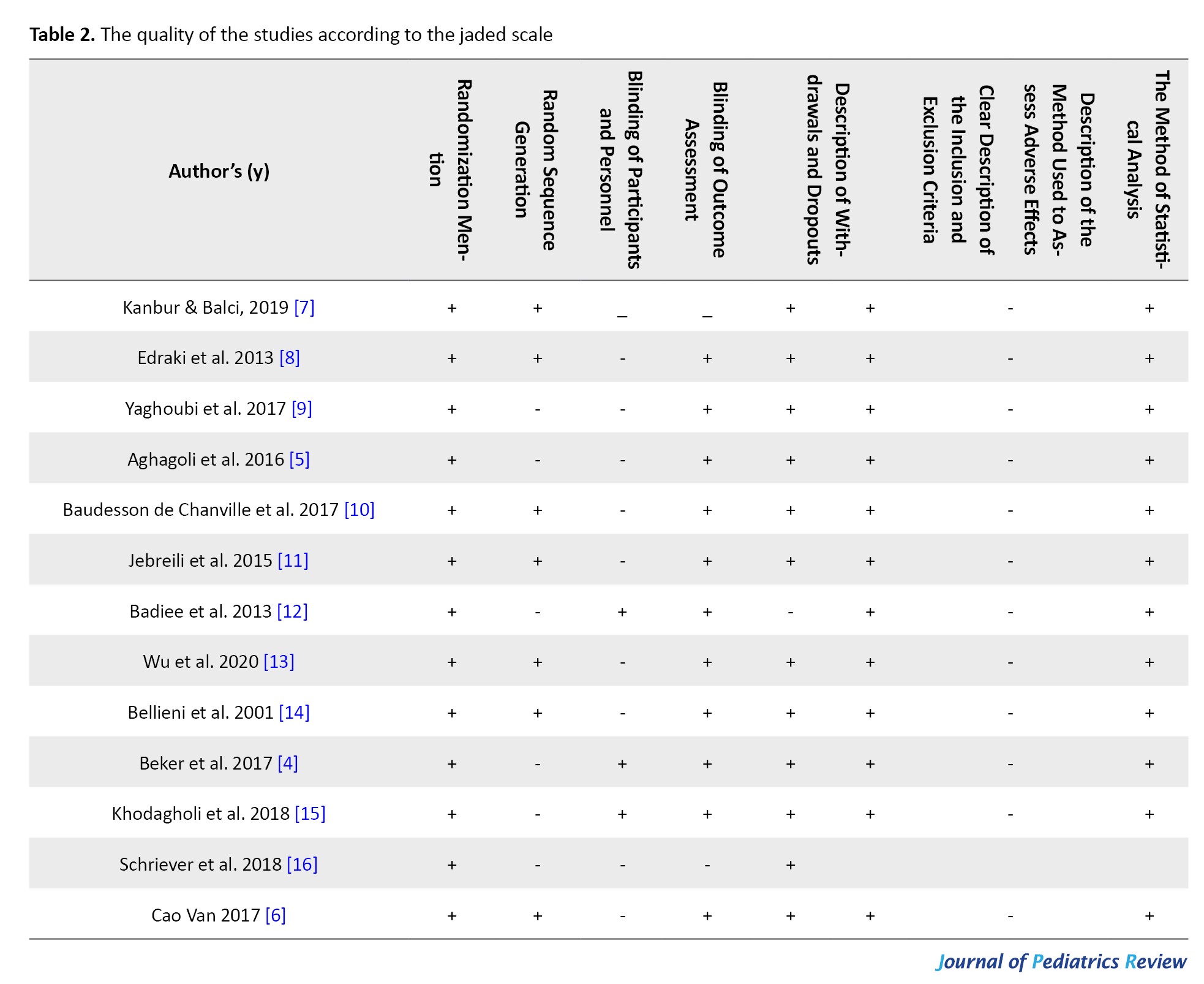
The methodological quality of the studies was assessed independently by the two authors. Disagreements between the assessors were subsequently adjudicated by a third reviewer (Table 2).
Results
A total of 927 titles were retrieved from a main database search. In addition, none of the trials were identified by hand-searched of the bibliographies of relevant articles. After removing duplicates, 347 trials remained of which 312 studies that were excluded because they did not meet the inclusion criteria based on title and abstract. The full text of the remaining 35 studies was reviewed, and another 22 studies were excluded because they did not meet the inclusion criteria. Finally, 13 studies were included in the review (Figure 1).
The effect of aromatherapy on apnea
Studies assessed the effect of aromatherapy with vanilla, breast milk, and Rosa damascenes on apnea. Two studies assessed the effect of aromatherapy with vanilla on apnea. The frequency of apnea decreased significantly in preterm infants in the vanilla group than in the breast milk and control [7] and no treatment (P<0.05) [8]. In contrast in Yaghoubi et al.’s study, the number of apnea attacks did not change after treatment with Vanilla control (P=0.142) [9]. In the study by Aghagoli et al. (2016) the number of apnea attacks was significantly lower in the Rosa damascenes group than control (distilled water) (P<0.05) [5].
The effect of aromatherapy on painful procedures
Three studies showed a significant decrease in premature infant pain profile score after heel lancing during venipuncture and after venipuncture in neonates receiving their mother’s milk odor in comparison with the control [10-12].
According to Wu et al. (2020) mean pain scores were significantly lower in preterm infants exposed to breast milk odor (n=36) or heartbeat sounds (HBs) + BM odor (n=33) or BM odor + non-nutritive sucking (NNS) + HBs (n=36) compared to the controls (routine care; n=36) during peripheral venipuncture procedures [13]. One study assessed the effect of sensorial saturation (SS) on painful procedures preterm infants were randomized into five different procedures: control, 10% oral glucose plus sucking, SS, oral water, and 10% oral glucose. SS is a multisensorial stimulation consisting of delicate tactile, vestibular, gustative, olfactory, auditory, and visual stimuli. SS has a greater analgesic effect on heel prick in preterm infants in comparison with control and sucking + oral glucose groups (P<0.001) [14].
Aromatherapy on transition from tube feeding (gavage) to oral feeding
Two studies assessed the effect of breast milk odor and one study assessed the effect of vanilla odor or rose on transition from tube feeding to oral feeding. In Beker et al.’s study, preterm infants were exposed to either the smell or taste of milk before each feed reached full enteral feeds at a shorter time (13.5 days) than no exposure group (15.5 days); however, the difference between the two groups was non-significant (P=0.1) [4]. In Khodagholi et al., study, milk odor in combination with NNS compared to alone NNS decreased transition feeding time to oral feeding (P=0.07) [15]. In Schriever et al.’s study, infants preterm exposed to the vanilla odor than the control group indicated a faster transition from tube feeding to oral feeding but, the difference was not significant between rose odor and control [16].
Aromatherapy on hospital discharge
In Cao Van et al.’s study [6], the length of hospitalization was shorter in infants stimulated with anise or cinnamon (group A) than odorless stimulation (control group). However, it was non-significant (P=0.12). In Khodagholi et al, milk odor in combination with NNS compared to NNS alone decreased hospital discharge time(P=0.07) [15].
Discussion
According to this review, olfactory stimulation by some pleasant odors was effective on painful procedures and apnea attacks in preterm infants. Meanwhile, hospital discharge time and transition time from tube feeding to oral feeding were shorter. However, the results were insignificant.
This review found that there are controversial results about the aromatherapy effect of pleasant odor vanillin on apnea attacks in preterm infants [8]. Rosa damascenes odor had a therapeutic effect on apnea attacks [23], but not other odors [5]. Recently, two systematic reviews reported consistent results with significant effects on apnea attacks in preterm infants. The first systematic review with three studies has shown that aromatherapy is effective in treating apnea in preterm infants. However, due to the small sample size and low number of studies included in their systematic review, the authors reiterated that their findings should be interpreted with caution [17]. The second systematic review and meta-analysis showed that the treatment with aromatherapy can significantly decrease apnea attacks compared to the control in the preterm infant [18]. According to our research aromatherapy with vanillin has a preventing [9] and therapeutic effect [7] on apneas episodes in preterm infants. In addition, regarding the multidimensional effect of vanillin, first, it may run through the nasal mucosa and enroll in the brain through the bloodstream. Second, the vanillin can improve orbitofrontal blood flow. Third, vanillin helps the newborns deal with the stress [8]. Fourth, vanillin probably has pharmacological properties; therefore, it can directly and indirectly affect the respiratory centers. In a study, the number of apnea attacks was significantly lower in the R. damascenes group compared to the control (distilled water; P<0.05) [5]. The extract of R. damascena stimulates axons and dendrites in the nervous system [19]. Moreover, the hydro-alcoholic extract of R. damascenes has a dilatory effect on respiratory airways [5, 20].
According to our review, BM and the vanillin odor were effective in preterm infants’ venipuncture [3, 4, 13] that is consistent with previous systematic reviews addressing the effect of pleasant odor on painful procedures. A systematic review showed aromatherapy with lavender could decrease painful procedures in infants and children [21]. A meta-analysis with eight randomized controlled trials involving 453 participants conducted by Zhang in 2018 showed that BM odor significantly decreased pain scores in newborns with large effect sizes for painful procedures [22]. Another systematic review was published by Norouziasl et al. and concluded that aromatherapy with the mother’s milk, vanilla and the mother’s odor could lessen painful procedures and improve physiological parameters [23].
According to a study, aromatherapy with anise or cinnamon led to a sudden transition from the feeding tube to effectual oral feeding in premature infants [6]. Moreover, cinnamon contains expressive anti-allergic, anti-ulcerogenic, antipyretic, anesthetic, and analgesic characteristics. It also has medicinal applications due to its strong aromatic, sweet, and warm odor or food additives [24]. The anise essential oil boosts the production of BM, expedites milk secretion, and acts as a diuretic substance. The anise seeds consist of anethole, which is a debilitated estrogenic agent. Given its role as a dopamine receptor antagonist, it could be activated by prolactin secretion increment [25].
However, published clinical studies reported controversial results about this effect, According to our study, infants exposed to milk odor transitioned from tube feeding to oral feeding 2-10 days earlier. However, the results were insignificant. The results of a systematic review of two studies revealed that exposure to the smell and taste of milk with gastric or nasogastric tube feedings had no clear effect on the time to reach full sucking feeds and full tube feeding [26]. Findings of a meta-analysis with 8 studies revealed that in comparison to the control group, infants preterm exposed to either pleasant odors or BM odor transitioned from tube feeding to oral feeding earlier [27]. Smell and taste play a significant role in improving digestion and absorption of food. Therefore, providing some milk for the infant to smell and taste via an orogastric or nasogastric tube can potentially bolster their ability to tolerate greater volumes of milk quickly.
The results of our review of three studies concluded there was no evidence of a clear effect of exposure to pleasant odors such as anise cinnamon or milk odor on hospital discharge time and weight at discharge in preterm infants. Inconsistent with our results, a systematic review of two studies revealed exposure to the smell and taste of milk with an orogastric or nasogastric tube may decrease the length of hospitalization in preterm infants [26].
Conclusion
Olfactory stimulation by some pleasant odors can help improve apnea attacks in preterm infants. Olfactory stimulation by milk odor is a safe, non-invasive and family-friendly intervention in improving painful procedures in preterm infants. The results were not conclusive although it was found that infants preterm exposed to pleasant odors had a shorter transition time from tube feeding to oral feeding and discharge earlier in the day.
Limitations and suggestions for future studies
This study faced some limitations of this study. First of all, the studies included in our systematic review had a small sample size. Second, only one kind of apnea, i.e. the idiopathic apnea of prematurity, has been studied in newborns. Hence, it is required to conduct further investigation to verify the effectiveness of this non-pharmacological method in various types of apnea. Despite randomization, the gender distribution was not balanced. Hence, it was obvious that male gender exhibited a higher disadvantage in premature infants. A review of literature male and female infants respond differentially to environmental stimuli, with different growth and neurodevelopmental trajectories. No study included in our review assessed sexually dimorphic response to aromatherapy on painful producers. Future studies should be conducted as systematic reviews with meta-analyses on this topic to address the gaps in knowledge identified from the results of this review.
Ethical Considerations
Compliance with ethical guidelines
This article is a meta-analysis with no human or animal sample.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization, project administration, and funding acquisition: Masumeh Ghazanfarpour, Mohammad Hasan Mohammadi, and Hashem Lashgari Kalat; Methodology: Zahra Ramazanian Bafghi, Shahabaddin Sorouri, Hossein Ali Kharazmi, Najmeh Soltani Nejad, Mohammad Hasan Mohammadi and Hashem Lashgari Kalat; Software: Hashem Lashgari Kalat, Masumeh Ghazanfarpour and Shahabaddin Sorouri; Validation and supervision: Shahabaddin Sorouri, Hossein Ali Kharazmi, Hashem Lashgari Kalat and Mohammad Hasan Mohammadi; Formal analysis: Zahra Ramazanian Bafghi, Najmeh Soltani Nejad and Masumeh Ghazanfarpour; Investigation: Hashem Lashgari Kalat, Masumeh Ghazanfarpour and Mohammad Hasan Mohammadi; Resources: Shahabaddin Sorouri, Hossein Ali Kharazmi, Najmeh Soltani Nejad and Hashem Lashgari Kalat; Data curation: Shahabaddin Sorouri, Hossein Ali Kharazmi, Mohammad Hasan Mohammadi and Hashem Lashgari Kalat; Writing the original draft: Hashem Lashgari Kalat, Shahabaddin Sorouri, Hossein Ali Kharazmi and Mohammad Hasan Mohammadi; Review and editing: All authors.
Conflicts of interest
The authors declared no conflict of interest.
References
- Neshat H, Jebreili M, Seyyedrasouli A, Ghojazade M, Hosseini MB, Hamishehkar H. Effects of breast milk and vanilla odors on premature neonate’s heart rate and blood oxygen saturation during and after venipuncture. Pediatr Neonatol. 2016; 57(3):225-31. [DOI:10.1016/j.pedneo.2015.09.004] [PMID]
- Craig KD, Whitfield MF, Grunau RVE, Linton J, Hadjistavropoulos HD. Pain in the preterm neonate: Behavioural and physiological indices. Pain. 1993; 52(3):287-99. [DOI:10.1016/0304-3959(93)90162-I] [PMID]
- Küçük Alemdar D, Kardaş Özdemir F. Effects of having preterm infants smell amniotic fluid, mother's milk, and mother's odor during heel stick procedure on pain, physiological parameters, and crying duration. Breastfeed Med. 2017; 12:297-304. [DOI:10.1089/bfm.2017.0006] [PMID]
- Beker F, Opie G, Noble E, Jiang Y, Bloomfield FH. Smell and taste to improve nutrition in very preterm infants: A randomized controlled pilot trial. Neonatology. 111(3):260-6. [DOI:10.1159/000450883] [PMID]
- Aghagoli S, Salimi A, Salimi M, Ghazavi Z, Marofi M, Mohammadbeigi A. Aromatherapy with rosa damascenes in apnea, bradycardia and Spo2 of preterm infants; a randomized clinical trial. Int J Pediatr. 2016; 4(6):1911-8. [Link]
- Cao Van H, Guinand N, Damis E, Mansbach AL, Poncet A, Hummel T, et al. Olfactory stimulation may promote oral feeding in immature newborn: A randomized controlled trial. Eur Arch Otorhinolaryngol. 2018; 275(1):125-9. [DOI:10.1007/s00405-017-4796-0] [PMID]
- Kanbur BN, Balci S. Impact of the odors of vanilla extract and breast milk on the frequency of apnea in preterm neonates. Jpn J Nurs Sci. 2020; 17(1):e12271. [DOI:10.1111/jjns.12271] [PMID]
- Edraki M, Pourpulad H, Kargar M, Pishva N, Zare N, Montaseri H. Olfactory stimulation by vanillin prevents apnea in premature newborn infants. Iran J Pediatr. 2013; 23(3):261-8. [PMID]
- Yaghoubi S, Salmani N, Dehghani K, DavoodiZadehJolgeh H. Investigating effect of olfactory stimulation by vanilla on the rate of apnea attacks in neonates with apnea of prematurity: A randomized clinical trial. Int J Pediatr. 2017; 5(12):6221-9. [Link]
- Baudesson de Chanville A, Brevaut-Malaty V, Garbi A, Tosello B, Baumstarck K, Gire C. Analgesic effect of maternal human milk odor on premature neonates: A randomized controlled trial. J Hum Lact. 2017; 33(2):300-8. [DOI:10.1177/0890334417693225] [PMID]
- Jebreili M, Neshat H, Seyyedrasouli A, Ghojazade M, Hosseini MB, Hamishehkar H. Comparison of breastmilk odor and vanilla odor on mitigating premature infants’ response to pain during and after venipuncture. Breastfeed Med. 2015; 10(7):362-5. [DOI:10.1089/bfm.2015.0060] [PMID]
- Badiee Z, Asghari M, Mohammadizadeh M. The calming effect of maternal breast milk odor on premature infants. Pediatr Neonatol. 2013;5 4(5):322-5. [DOI:10.1016/j.pedneo.2013.04.004] [PMID]
- Wu Y, Zhang C, Liu H, Duan C, Li C, Fan J, et al. Perinatal depressive and anxiety symptoms of pregnant women along with COVID-19 outbreak in China. Am J Obstet Gynecol. 2020; 223(2):240.e1-240.e9. [PMID]
- Bellieni CV, Buonocore G, Nenci A, Franci N, Cordelli DM, Bagnoli F. Sensorial saturation: An effective analgesic tool for heel-prick in preterm infants: A prospective randomized trial. Biol Neonate. 2001; 80(1):15-8. [DOI:10.1159/000047113] [PMID]
- Khodagholi Z, Zarifian T, Soleimani F, Khoshnood Shariati M, Bakhshi E. The effect of non-nutritive sucking and maternal milk odor on the independent oral feeding in preterm infants. Iran J Child Neurol. 2018; 12(4):55-64. [PMID]
- Schriever VA, Gellrich J, Rochor N, Croy I, Cao-Van H, Rüdiger M, et al. Sniffin’away the feeding tube: The influence of olfactory stimulation on oral food intake in newborns and premature infants. Chem Senses. 2018; 43(7):469-74.[DOI:10.1093/chemse/bjy034] [PMID]
- Ataei Nakhaei A, Javid A, Marefat M, Chaichy Z, Alshahrestani A, Nazarpour P. Is aromatherapy effective for apnea in preterm infants? A systematic review. Int J Pediatr. 2019; 7(7):9741-7. [DOI:10.22038/ijp.2019.40056.3402]
- Rustaee S, Rezapour-Nasrabad R, Ghazanfarpour M, Piri S, Moosavi Moqaddam SF, Behdarvandi A, et al. The effects of aroma on apnea attacks and oxygen saturation among preterm infants: A systematic review and meta-analysis. Galen Med J. 2023; 12:e2846. [DOI:10.31661/gmj.v12i.2846] [PMID]
- Gambari R. Predictive analyses of biological effects of natural products: From plant extracts to biomolecular laboratory and computer modeling. Evid Based Complement Alternat Med. 2011; 2011:383290. [DOI:10.1093/ecam/nep096] [PMID]
- Kowalski J, Samojedny A, Paul M, Pietsz G, Wilczok T. Effect of apigenin, kaempferol and resveratrol on the expression of interleukin-1beta and tumor necrosis factor-alpha genes in J774. 2 macrophages. Pharmacol Rep. 2005; 57(3):390-4. [PMID]
- Sezavar M, Ahmadi R, Shojaei H, Jafari M, Hashemi I, Attaei Nakhaie AR, et al. The effect of lavender oil for relief painful producer in children and infants: A systematic review. J Pediatr Perspect. 2020; 8(4):11177-85. [Link]
- Zhang S, Su F, Li J, Chen W. The analgesic effects of maternal milk odor on newborns: A meta-analysis. Breastfeed Med. 2018; 13(5):327-34. [DOI:10.1089/bfm.2017.0226] [PMID]
- Norouziasl S, Ataei Nakhaei A, Kalani-moghaddam F, Dehghani N, Ahmadinezhad F. The effects of different strategies on the painful procedure management, and the physiological parameters in preterm infants: A systematic review. Int J Pediatr. 2020; 8(5):11251-9. [Link]
- Wang R, Wang R, Yang B. Extraction of essential oils from five cinnamon leaves and identification of their volatile compound compositions. Innovative Food Sci Emerg Technol. 2009; 10(2):289-92. [DOI:10.1016/j.ifset.2008.12.002]
- Wang GY, Yang C, Yang Z, Yang W, Jiang S, Zhang G, et al. Effects of dietary star anise (I llicium verum H ook f) supplementation during gestation and lactation on the performance of lactating multiparous sows and nursing piglets. Anim Sci J. 2015; 86(4):401-7. [DOI:10.1111/asj.12300] [PMID]
- Muelbert M, Lin L, Bloomfield FH, Harding JE. Exposure to the smell and taste of milk to accelerate feeding in preterm infants. Cochrane Database Syst Rev. 2019; 7(7):CD013038.[DOI:10.1002/14651858.CD013038.pub2] [PMID]
- Jalaly E, Ghazanfarpour M, Afiat Milad M, Abdi F, Soleimany S, Saadat S. The effects of breast milk and other pleasant odors on the transition from gavage to oral feeding in preterm infants: A systematic review and meta-analysis. J Pediatr Revi. 2024; 12(1):5-14. [DOI: 10.32598/jpr.12.1.283.7]
Type of Study: Review Article |
Subject:
Pediatrics
Received: 2024/06/17 | Accepted: 2024/09/18 | Published: 2024/10/1
Received: 2024/06/17 | Accepted: 2024/09/18 | Published: 2024/10/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |