Volume 13, Issue 1 (1-2025)
J. Pediatr. Rev 2025, 13(1): 17-28 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Azizi M, Yazdani F, Nikbakht R, Shahhosseini Z. The Biopsychosocial Outcomes of Childlessness or Having One Child on Couple’s Health: A Systematic Review. J. Pediatr. Rev 2025; 13 (1) :17-28
URL: http://jpr.mazums.ac.ir/article-1-657-en.html
URL: http://jpr.mazums.ac.ir/article-1-657-en.html
1- Department of Midwifery, Sexual and Reproductive Health Research Center, Faculty of Nursing and Midwifery, Mazandaran University of Medical Sciences, Sari, Iran.
2- Health Science Research Center, Mazandaran University of Medical Sciences, Sari, Iran.
3- Department of Biostatics and Epidemiology, Faculty of Health, Mazandaran University of Medical Sciences, Sari, Iran.
4- Department of Midwifery, Sexual and Reproductive Health Research Center, Faculty of Nursing and Midwifery, Mazandaran University of Medical Sciences, Sari, Iran. ,zshahhosseini@yahoo.com
2- Health Science Research Center, Mazandaran University of Medical Sciences, Sari, Iran.
3- Department of Biostatics and Epidemiology, Faculty of Health, Mazandaran University of Medical Sciences, Sari, Iran.
4- Department of Midwifery, Sexual and Reproductive Health Research Center, Faculty of Nursing and Midwifery, Mazandaran University of Medical Sciences, Sari, Iran. ,
Full-Text [PDF 593 kb]
(2449 Downloads)
| Abstract (HTML) (2371 Views)
Full-Text: (903 Views)
Introduction
In recent decades, the increase in childlessness or having just one child is one of the significant changes in the demographic structure, especially in developed countries [1]. In this regard, childlessness or having a single child reduces the population in developed and developing countries [2], leading to significant concerns among demographers and policymakers involved in social development [3]. From a general point of view, the increase in childlessness is the result of an individualistic and self-centered society, and this view blames childless women for the rapid population aging and the impending social decline of security systems [4]. The childless rate in Portugal and most Eastern European countries was below 10%. Also, less than 15% of women in France, Belgium, Germany, Norway, Slovakia, Slovenia, and Sweden are childless. In countries such as Austria, Italy, Finland, the Netherlands, and the United Kingdom, childless women reach over 20% [5]. In recent years, Iran has also faced the population change problem in such a way that since the 1960s, the number of births has decreased significantly [6]. There are no accurate statistics on the rate of childlessness in Iran [7]. A study of married people in Iran between the ages of 25 and 54 showed that 12.5% were childless [8]. Another study shows that voluntary childlessness among married women was 8.5% [9].
The literature review shows that reasons for childlessness in couples include involuntary causes (infertility or delayed marriage), voluntary motives (conscious decision not to have children due to social attitudes, greater participation in occupational and social activities, and women’s higher education and lack of traditional attitudes regarding women’s reproductive duties), or death of one or more children [10, 11]. In addition, couples’ disagreements regarding childbearing and time to conceive, or infertility problems caused by postponing fertility, can affect childbearing [1]. In this regard, a study indicates that childlessness caused by the inability to have children has adverse psychological consequences on the reproductive-aged couple’s mental health and requires psychological coping skills [12-14].
Literature review shows that childlessness or having one child affects the individual’s health from various perspectives. From a sociological and economic point of view, childlessness, whether voluntary or involuntary, can positively impact an individual’s health [15, 16]. In contrast, a study in Iran shows that having one child is associated with negative consequences for parents, including physical adverse outcomes such as increasing the risk of breast and ovarian cancer in women; psychological outcomes such as increased stress, anxiety, and depression; and upbringing adverse events, such as increased child-centered family and decreased family cohesion [17]. Some families are unwilling to have more children due to difficulty dealing with the first child, and others due to the new conditions in their lifestyles after childbirth period. Some economic, educational, and welfare problems were other significant factors that led to the couple’s unwillingness to have more children [18, 19].
The biopsychosocial model is an approach to understanding individuals’ mental and physical health status through a multi-systems lens and the influence of biology, psychology, and social environment [20, 21]. Research on childlessness and having one child in families has recently increased [1]. The critical issues in this field include the social consequences of childlessness [22], consequences of childlessness in the labor market [23], and elderly period health and wellbeing [12, 24].
With the introduction of the population youth policy in Iran in recent years, the significant reduction of population growth, and the phenomenon of population aging, it is crucial to identify the consequences of having one child and no children in Iran and worldwide. The literature review shows that despite many studies on the consequences of having one child or no children worldwide, no systematic review has been found in this field. Therefore, this study aimed to assess the biopsychosocial outcomes of childlessness or having one child on couples’ health.
Methods
Study design and protocol registration
This systematic review was conducted according to PRISMA (the preferred reporting items for systematic reviews and meta-analyses) statements in 2020 [25].
Following the PICO (participants, intervention, comparator, outcomes) criteria, the “participants” were childless or with one child couples; the type of “intervention” was not applicable; the “comparator” included couples with more than one child, and the “outcome” was the biopsychosocial outcomes of childlessness or having one child on couple’s health status. According to the PICO components, the research question was formulated: “What are the biopsychosocial outcomes of childlessness or having one child on a couple’s health?”
Before conducting this study, its protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO).
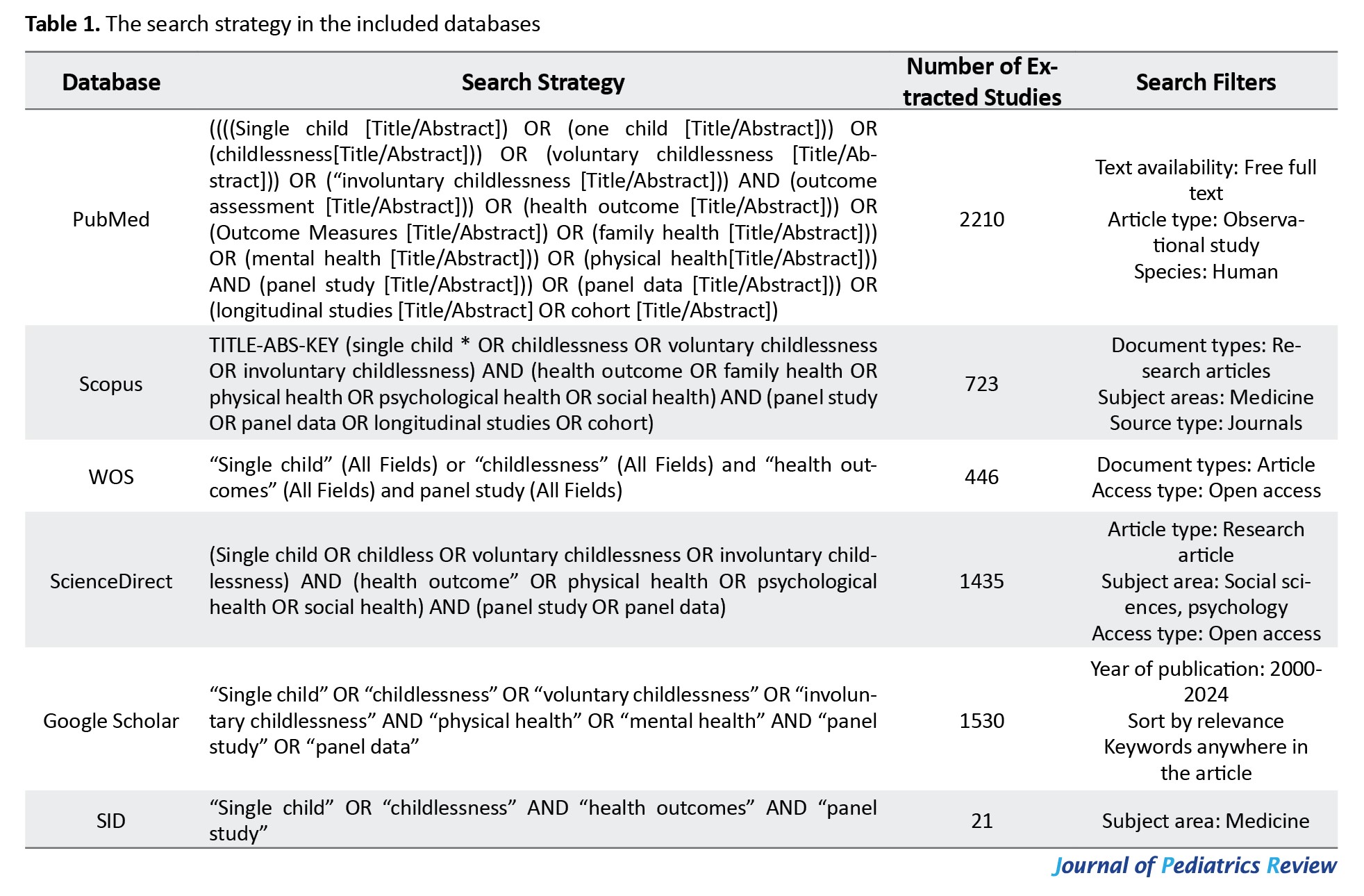
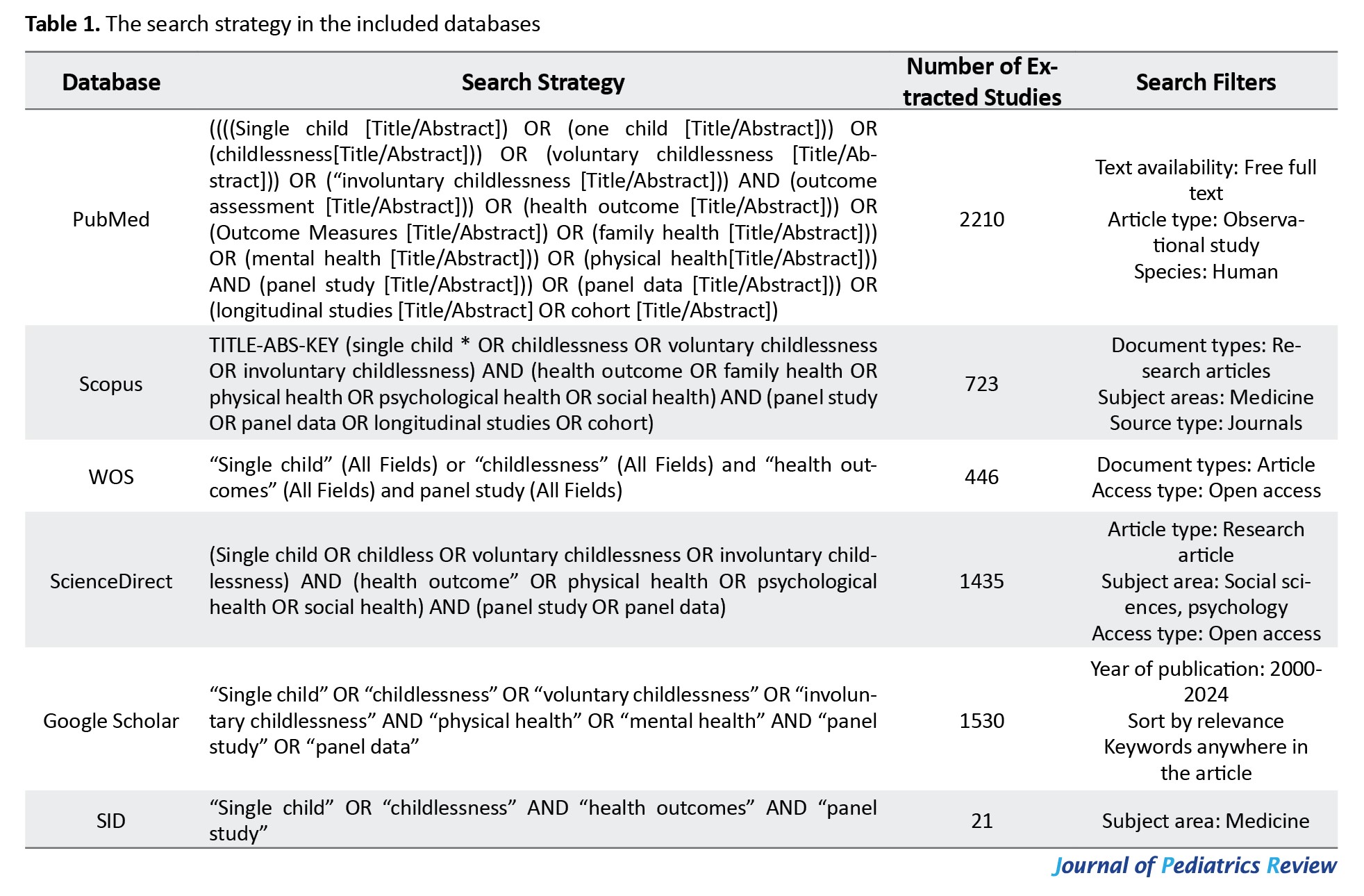
Search strategy and literature search
For this systematic review, authors searched Google Scholar and electronic databases such as PubMed, Scopus, Web of Science, ScienceDirect, and the Iranian database, including the Scientific Information Database (SID). The search was performed by two authors (Fereshteh Yazdani Fereshteh Yazdani & Marzieh Azizi) with no time and language restrictions between March 1, 2024, and April 15, 2024.
To search in the mentioned databases, first, medical subject headings were used to extract search terms as follows: ((One-child [MeSH Terms]) OR (only child [MeSH Terms]) OR (single child [MeSH Terms]) OR (childlessness [MeSH Terms]) OR (voluntary childlessness [MeSH Terms]) OR (involuntary childlessness [MeSH Terms])) AND ((outcome assessment [Title]) OR (health outcome [Title]) OR (outcome measures [Title])) AND ((panel study [MeSH Terms])) OR (cohort study [MeSH Terms]) OR (longitudinal study [MeSH Terms])). The authors searched each database according to the specific guidelines for advanced search provided by each database. In addition, all reference lists of included studies were manually searched to ensure that all additional published articles were identified. The reference manager software EndNote, version 21 was applied to manage the references and eliminate duplicate records.
Inclusion and exclusion criteria
In this systematic review, the inclusion criteria were as follows: The panel, longitudinal, and cohort studies published in scientific journals and assessed the consequences of having one child or childlessness on a couple’s or parent’s health from 1990 to 2024.
In contrast, published thesis or dissertation regarding this study title, studies that have been published in Research Square as preprints, abstracts of conferences indexed in databases, studies with other designs, including case reports, case series and control, letters, narrative, scoping and systematic reviews, randomized controlled trials (RCTs) and studies regarding the childlessness or having a single child with no assessment of its consequences were excluded from this study.
Quality assessment of the included studies
The Newcastle-Ottawa scale (NOS) for the cohort was used to evaluate the methodological quality of the included studies [26]. This scale includes 9 questions in three quality parameters: Selection, comparability, and outcome. Studies with 3 or 4 stars in the selection domain, 1 or 2 stars in the comparability, and 2 or 3 stars in the outcome domain have good quality. Also, if studies acquire two stars in the selection domain, one or two stars in the comparability domain, and two or three stars in the outcome domain, have considered acceptable with fair quality. Poor quality is recognized for studies with 0 or 1 star in the selection domain, 0 stars in the comparability domain, and 0 or 1 star in the outcome domain [27].
Data extraction
The title and abstracts were evaluated for relevance to our review objectives in all included studies. In relevant studies, the full text was carefully read, and if it was consistent with the review’s objectives, the required information was extracted and checked by Zohreh Shahhosseini. Two authors (Fereshteh Yazdani and Marzieh Azizi) assessed each study regarding the eligibility criteria and extracted the required information. The final decision for screening was conducted according to the consultation of the corresponding author (Zohreh Shahhosseini) about any discrepancy in the screening process. The extracted data in tables include the first author, the publication year, the country, the study design, the sample size, the outcomes measure, and the main results of the studies.
Results
Search results
The search results in databases and screening processes are shown in Figure 1. The search resulted in 6365 articles. After excluding duplicate results (n=1105), 5260 articles remained. Afterward, 957 were excluded based on the screening of titles and abstracts. During the full-text review assessment, original articles except for panel, cohort, or longitudinal studies (n=2304), scoping review, narrative review, systematic review, and meta-analysis (n=214), and cohort studies that did not assess the health outcomes of childlessness or having one child (n=1741) were excluded. In addition, the reference lists of searched studies were evaluated, and 13 articles were identified. Among them, 7 articles were excluded due to the lack of assessment of the health outcomes of childlessness or having one child, and 6 were reviewed. Finally, 9 studies were included in this systematic review (Figure 1).
The characteristics of the included studies
From the included studies, 2 studies were conducted in the Netherlands [12, 28]. Also, one study was conducted in China [10], one in Sweden [29], one in Denmark [30], one in Norwegian [31], one in Australia [32], one in the USA [33], and one in Hungary, Austria, Estonia, Netherlands, and Poland [34]. Eight studies were prospective cohort or population-based cohort studies, and one was a panel study. The included studies were published between 2001 and 2022 regarding the publication year.
Main results
The results have been analyzed based on the biopsychosocial perspective. As a result, the present study’s findings led to classifying the results into three main categories: Biological, psychological, and social outcomes (Table 2).


Biological outcomes
Four studies assessed the biological outcomes of having one or no children on a couple’s health [29, 30, 32, 34]. The results of a study conducted by Davis et al., which assessed the effect of parity and mode of birth on the quality of life of couples, show that childless women or those with one child had lower physical health status than women with two or more children. In addition, women with cesarean section(s) also had poorer health quality than women who had vaginal delivery [32]. The multi-countries study conducted by Quashie et al. shows contradictory results, so the results of a survey of Hungarian participants show no significant correlation between childlessness and poor physical health status. In contrast, childlessness in Austria, Estonia, Netherlands, and Poland show better physical health status [34]. Other studies also show the impact of childlessness on the risk of cardiovascular disease and mortality [29], metabolic syndrome, and diabetes in men [30].
Psychological outcomes
Six studies assessed the psychological effect of childlessness or having one child on a couple’s health. The included studies in this field had controversial results.
According to Davis et al.’s study, childless women or those with one child have lower mental health compared to women with two or more children. In addition, having a cesarean section leads to poorer mental health compared to vaginal delivery among women [32]. In Quashie study, there was no significant association between childlessness and poor psychological wellbeing [34]. A European survey by Huijts et al. shows that childlessness is associated with a lowered psychological sense of wellbeing among men, but this association is not significant among women [12]. Consistent with this study, the results of other studies show that women without children have lower satisfaction and self-confidence compared with mothers with children. At the same time, parental status was not related to men’s psychological wellbeing [31]. According to the results of a study in China, childlessness in older adults can cause psychological effects such as less life satisfaction, feelings of more anxiety, and loneliness [10].
In contrast, another study shows that childlessness does not lead to a significantly higher prevalence of loneliness and depression in older adults with any risk factors. In other words, divorced, widowed, and unmarried childless men are significantly lonelier than women of similar status. Also, the prevalence of depression among divorced and widowed childless men was considerably higher than among divorced and widowed women [33].
Social outcomes
The social outcomes of childlessness or having one child were assessed in only one study. Keizer et al. investigated the association between parental status and psychological wellbeing. It shows that childless men are different from fathers with children in terms of participation in society, income level, and life satisfaction [28].
The quality assessment of the studies
Through NOS for cohort studies, the quality of nine studies was investigated. The quality assessment results showed that 3 studies had good methodological quality [29, 30, 32], and 6 had fair quality [10, 12, 28, 31, 33, 34]. The studies’ scores are presented in Table 3.

Discussion
This systematic review investigates the biopsychosocial outcomes of having one child and no children on a couple’s health. Nine studies containing cohort and panel studies were included in the review. The role of voluntary childlessness in explaining this condition is unclear. It is assumed that childlessness in the past was mainly involuntary and caused by late marriage and singleness or infertility due to medical conditions. In contrast, current childlessness is primarily based on a voluntary decision not to conceive [35]. In this regard, childlessness in some societies, especially in the United States, can be the result of couples choosing to postpone childbearing to allow them to pursue other goals in life. Studies showed that these childless years create a space and an opportunity to explore social roles outside the family environment, including education, employment, and leisure [3, 36].
The results of the current study indicate that childlessness can affect people’s biological health. According to the findings of this study, childlessness can increase the chances of developing metabolic diseases and diabetes. The results of a study indicate that male infertility is involved in pathways of diseases, such as cancer, cardiovascular and metabolic disorders. Also, male germ cell gene mutations could lead to or contribute to infertility, metabolic diseases, and diabetes [30]. At the same time, other studies also show that the chances of developing diabetes increase in infertile men [37-40]. Also, our review indicates that childlessness increases the risk of cardiovascular diseases, which was consistent with other studies in infertile people [41-43]. In addition, childlessness raises the death rate compared to couples with children or even adopted children [44-46].
This study also investigated the psychological effects of childlessness on a couple’s health status. In this regard, some of the studies indicated that 80% of infertile people had encountered some psychosexual disorders such as marital and sexual dissatisfaction, impaired personal and interpersonal relationships, decreased sexual desire, and adverse psychiatric disorders [47]. In addition, this study’s findings align with other studies that show that childlessness is related to low mental health and psychological wellbeing [48, 49].
Studies in this area are conflicting, and other studies have shown that from the perspective of biopsychosocial, childless couples had the lowest levels of depression compared to other groups [50]. In addition, unwanted childlessness is not correlated with psychological distress for couples [51]. Contradictions in studies can be due to different cultures related to having children or other situations, such as various recreational facilities and involvement in social activities.
Another finding of this study is the effect of childlessness on social status. Based on the findings of this study, childlessness can affect people’s social participation. According to a survey, childlessness can reduce social activities and communication with family, neighbors, and society [28]. Another study found that those who never had children have smaller networks of older people than parents, partially attributed to a more limited number of relatives [52]. A study found that older people without children, regardless of marital status and gender, are just as likely as those with children to participate in community and voluntary organizations and volunteer work [53]. Consistent with the present study, based on the survey results, fatherhood encourages men to have extensive intergenerational and family interactions [54].
The limitation of this study was the low panel studies regarding childlessness or having one child couples and its effect on their health status. In addition, we could not perform a meta-analysis due to the impossibility of data such as relative risk from included studies. The strength of this study was that it was the first systematic review of cohort and panel studies that addressed the impact of childlessness or having one child on a couple’s health status.
Conclusion
This study assessed the effects of childlessness on a couple’s health using a biopsychosocial approach. The study results indicate that childless couples may have various health problems in biological, psychological, and social aspects, which, in general, negatively affect their quality of life. Due to the considerable decrease in total fertility rate and population growth, the number of childless couples will increase in the future, and these individuals will be at high risk of physical, mental, and social challenges. Therefore, the results of this systematic review can be a good resource for policymakers and health specialists to design and implement cost-effective interventions to improve fertility indicators among the Iranian population. In addition, due to limited information regarding childlessness’s effects on a couple’s health, conducting precise studies with high-quality methodology is proposed in the future.
Ethical Considerations
Compliance with ethical guidelines
This systematic review was conducted according to PRISMA in 2020. Before conducting this study, its protocol was registered in the PROSPERO (Code: CRD42023491821).
Funding
This study was financially supported by Mazandaran University of Medical Sciences, Sari, Iran.
Authors contributions
Conceptualization and supervision: Zohreh Shah Hosseini; Investigation and writing the original draft: Marzieh Azizi and Fereshteh Yazdani; Review and editing: Roya Nikbakht and Marzieh Azizi.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors thank Mazandaran University of Medical Sciences, Sari, Iran for supporting this study.
References
In recent decades, the increase in childlessness or having just one child is one of the significant changes in the demographic structure, especially in developed countries [1]. In this regard, childlessness or having a single child reduces the population in developed and developing countries [2], leading to significant concerns among demographers and policymakers involved in social development [3]. From a general point of view, the increase in childlessness is the result of an individualistic and self-centered society, and this view blames childless women for the rapid population aging and the impending social decline of security systems [4]. The childless rate in Portugal and most Eastern European countries was below 10%. Also, less than 15% of women in France, Belgium, Germany, Norway, Slovakia, Slovenia, and Sweden are childless. In countries such as Austria, Italy, Finland, the Netherlands, and the United Kingdom, childless women reach over 20% [5]. In recent years, Iran has also faced the population change problem in such a way that since the 1960s, the number of births has decreased significantly [6]. There are no accurate statistics on the rate of childlessness in Iran [7]. A study of married people in Iran between the ages of 25 and 54 showed that 12.5% were childless [8]. Another study shows that voluntary childlessness among married women was 8.5% [9].
The literature review shows that reasons for childlessness in couples include involuntary causes (infertility or delayed marriage), voluntary motives (conscious decision not to have children due to social attitudes, greater participation in occupational and social activities, and women’s higher education and lack of traditional attitudes regarding women’s reproductive duties), or death of one or more children [10, 11]. In addition, couples’ disagreements regarding childbearing and time to conceive, or infertility problems caused by postponing fertility, can affect childbearing [1]. In this regard, a study indicates that childlessness caused by the inability to have children has adverse psychological consequences on the reproductive-aged couple’s mental health and requires psychological coping skills [12-14].
Literature review shows that childlessness or having one child affects the individual’s health from various perspectives. From a sociological and economic point of view, childlessness, whether voluntary or involuntary, can positively impact an individual’s health [15, 16]. In contrast, a study in Iran shows that having one child is associated with negative consequences for parents, including physical adverse outcomes such as increasing the risk of breast and ovarian cancer in women; psychological outcomes such as increased stress, anxiety, and depression; and upbringing adverse events, such as increased child-centered family and decreased family cohesion [17]. Some families are unwilling to have more children due to difficulty dealing with the first child, and others due to the new conditions in their lifestyles after childbirth period. Some economic, educational, and welfare problems were other significant factors that led to the couple’s unwillingness to have more children [18, 19].
The biopsychosocial model is an approach to understanding individuals’ mental and physical health status through a multi-systems lens and the influence of biology, psychology, and social environment [20, 21]. Research on childlessness and having one child in families has recently increased [1]. The critical issues in this field include the social consequences of childlessness [22], consequences of childlessness in the labor market [23], and elderly period health and wellbeing [12, 24].
With the introduction of the population youth policy in Iran in recent years, the significant reduction of population growth, and the phenomenon of population aging, it is crucial to identify the consequences of having one child and no children in Iran and worldwide. The literature review shows that despite many studies on the consequences of having one child or no children worldwide, no systematic review has been found in this field. Therefore, this study aimed to assess the biopsychosocial outcomes of childlessness or having one child on couples’ health.
Methods
Study design and protocol registration
This systematic review was conducted according to PRISMA (the preferred reporting items for systematic reviews and meta-analyses) statements in 2020 [25].
Following the PICO (participants, intervention, comparator, outcomes) criteria, the “participants” were childless or with one child couples; the type of “intervention” was not applicable; the “comparator” included couples with more than one child, and the “outcome” was the biopsychosocial outcomes of childlessness or having one child on couple’s health status. According to the PICO components, the research question was formulated: “What are the biopsychosocial outcomes of childlessness or having one child on a couple’s health?”
Before conducting this study, its protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO).
Search strategy and literature search
For this systematic review, authors searched Google Scholar and electronic databases such as PubMed, Scopus, Web of Science, ScienceDirect, and the Iranian database, including the Scientific Information Database (SID). The search was performed by two authors (Fereshteh Yazdani Fereshteh Yazdani & Marzieh Azizi) with no time and language restrictions between March 1, 2024, and April 15, 2024.
To search in the mentioned databases, first, medical subject headings were used to extract search terms as follows: ((One-child [MeSH Terms]) OR (only child [MeSH Terms]) OR (single child [MeSH Terms]) OR (childlessness [MeSH Terms]) OR (voluntary childlessness [MeSH Terms]) OR (involuntary childlessness [MeSH Terms])) AND ((outcome assessment [Title]) OR (health outcome [Title]) OR (outcome measures [Title])) AND ((panel study [MeSH Terms])) OR (cohort study [MeSH Terms]) OR (longitudinal study [MeSH Terms])). The authors searched each database according to the specific guidelines for advanced search provided by each database. In addition, all reference lists of included studies were manually searched to ensure that all additional published articles were identified. The reference manager software EndNote, version 21 was applied to manage the references and eliminate duplicate records.
Inclusion and exclusion criteria
In this systematic review, the inclusion criteria were as follows: The panel, longitudinal, and cohort studies published in scientific journals and assessed the consequences of having one child or childlessness on a couple’s or parent’s health from 1990 to 2024.
In contrast, published thesis or dissertation regarding this study title, studies that have been published in Research Square as preprints, abstracts of conferences indexed in databases, studies with other designs, including case reports, case series and control, letters, narrative, scoping and systematic reviews, randomized controlled trials (RCTs) and studies regarding the childlessness or having a single child with no assessment of its consequences were excluded from this study.
Quality assessment of the included studies
The Newcastle-Ottawa scale (NOS) for the cohort was used to evaluate the methodological quality of the included studies [26]. This scale includes 9 questions in three quality parameters: Selection, comparability, and outcome. Studies with 3 or 4 stars in the selection domain, 1 or 2 stars in the comparability, and 2 or 3 stars in the outcome domain have good quality. Also, if studies acquire two stars in the selection domain, one or two stars in the comparability domain, and two or three stars in the outcome domain, have considered acceptable with fair quality. Poor quality is recognized for studies with 0 or 1 star in the selection domain, 0 stars in the comparability domain, and 0 or 1 star in the outcome domain [27].
Data extraction
The title and abstracts were evaluated for relevance to our review objectives in all included studies. In relevant studies, the full text was carefully read, and if it was consistent with the review’s objectives, the required information was extracted and checked by Zohreh Shahhosseini. Two authors (Fereshteh Yazdani and Marzieh Azizi) assessed each study regarding the eligibility criteria and extracted the required information. The final decision for screening was conducted according to the consultation of the corresponding author (Zohreh Shahhosseini) about any discrepancy in the screening process. The extracted data in tables include the first author, the publication year, the country, the study design, the sample size, the outcomes measure, and the main results of the studies.
Results
Search results
The search results in databases and screening processes are shown in Figure 1. The search resulted in 6365 articles. After excluding duplicate results (n=1105), 5260 articles remained. Afterward, 957 were excluded based on the screening of titles and abstracts. During the full-text review assessment, original articles except for panel, cohort, or longitudinal studies (n=2304), scoping review, narrative review, systematic review, and meta-analysis (n=214), and cohort studies that did not assess the health outcomes of childlessness or having one child (n=1741) were excluded. In addition, the reference lists of searched studies were evaluated, and 13 articles were identified. Among them, 7 articles were excluded due to the lack of assessment of the health outcomes of childlessness or having one child, and 6 were reviewed. Finally, 9 studies were included in this systematic review (Figure 1).
The characteristics of the included studies
From the included studies, 2 studies were conducted in the Netherlands [12, 28]. Also, one study was conducted in China [10], one in Sweden [29], one in Denmark [30], one in Norwegian [31], one in Australia [32], one in the USA [33], and one in Hungary, Austria, Estonia, Netherlands, and Poland [34]. Eight studies were prospective cohort or population-based cohort studies, and one was a panel study. The included studies were published between 2001 and 2022 regarding the publication year.
Main results
The results have been analyzed based on the biopsychosocial perspective. As a result, the present study’s findings led to classifying the results into three main categories: Biological, psychological, and social outcomes (Table 2).


Biological outcomes
Four studies assessed the biological outcomes of having one or no children on a couple’s health [29, 30, 32, 34]. The results of a study conducted by Davis et al., which assessed the effect of parity and mode of birth on the quality of life of couples, show that childless women or those with one child had lower physical health status than women with two or more children. In addition, women with cesarean section(s) also had poorer health quality than women who had vaginal delivery [32]. The multi-countries study conducted by Quashie et al. shows contradictory results, so the results of a survey of Hungarian participants show no significant correlation between childlessness and poor physical health status. In contrast, childlessness in Austria, Estonia, Netherlands, and Poland show better physical health status [34]. Other studies also show the impact of childlessness on the risk of cardiovascular disease and mortality [29], metabolic syndrome, and diabetes in men [30].
Psychological outcomes
Six studies assessed the psychological effect of childlessness or having one child on a couple’s health. The included studies in this field had controversial results.
According to Davis et al.’s study, childless women or those with one child have lower mental health compared to women with two or more children. In addition, having a cesarean section leads to poorer mental health compared to vaginal delivery among women [32]. In Quashie study, there was no significant association between childlessness and poor psychological wellbeing [34]. A European survey by Huijts et al. shows that childlessness is associated with a lowered psychological sense of wellbeing among men, but this association is not significant among women [12]. Consistent with this study, the results of other studies show that women without children have lower satisfaction and self-confidence compared with mothers with children. At the same time, parental status was not related to men’s psychological wellbeing [31]. According to the results of a study in China, childlessness in older adults can cause psychological effects such as less life satisfaction, feelings of more anxiety, and loneliness [10].
In contrast, another study shows that childlessness does not lead to a significantly higher prevalence of loneliness and depression in older adults with any risk factors. In other words, divorced, widowed, and unmarried childless men are significantly lonelier than women of similar status. Also, the prevalence of depression among divorced and widowed childless men was considerably higher than among divorced and widowed women [33].
Social outcomes
The social outcomes of childlessness or having one child were assessed in only one study. Keizer et al. investigated the association between parental status and psychological wellbeing. It shows that childless men are different from fathers with children in terms of participation in society, income level, and life satisfaction [28].
The quality assessment of the studies
Through NOS for cohort studies, the quality of nine studies was investigated. The quality assessment results showed that 3 studies had good methodological quality [29, 30, 32], and 6 had fair quality [10, 12, 28, 31, 33, 34]. The studies’ scores are presented in Table 3.

Discussion
This systematic review investigates the biopsychosocial outcomes of having one child and no children on a couple’s health. Nine studies containing cohort and panel studies were included in the review. The role of voluntary childlessness in explaining this condition is unclear. It is assumed that childlessness in the past was mainly involuntary and caused by late marriage and singleness or infertility due to medical conditions. In contrast, current childlessness is primarily based on a voluntary decision not to conceive [35]. In this regard, childlessness in some societies, especially in the United States, can be the result of couples choosing to postpone childbearing to allow them to pursue other goals in life. Studies showed that these childless years create a space and an opportunity to explore social roles outside the family environment, including education, employment, and leisure [3, 36].
The results of the current study indicate that childlessness can affect people’s biological health. According to the findings of this study, childlessness can increase the chances of developing metabolic diseases and diabetes. The results of a study indicate that male infertility is involved in pathways of diseases, such as cancer, cardiovascular and metabolic disorders. Also, male germ cell gene mutations could lead to or contribute to infertility, metabolic diseases, and diabetes [30]. At the same time, other studies also show that the chances of developing diabetes increase in infertile men [37-40]. Also, our review indicates that childlessness increases the risk of cardiovascular diseases, which was consistent with other studies in infertile people [41-43]. In addition, childlessness raises the death rate compared to couples with children or even adopted children [44-46].
This study also investigated the psychological effects of childlessness on a couple’s health status. In this regard, some of the studies indicated that 80% of infertile people had encountered some psychosexual disorders such as marital and sexual dissatisfaction, impaired personal and interpersonal relationships, decreased sexual desire, and adverse psychiatric disorders [47]. In addition, this study’s findings align with other studies that show that childlessness is related to low mental health and psychological wellbeing [48, 49].
Studies in this area are conflicting, and other studies have shown that from the perspective of biopsychosocial, childless couples had the lowest levels of depression compared to other groups [50]. In addition, unwanted childlessness is not correlated with psychological distress for couples [51]. Contradictions in studies can be due to different cultures related to having children or other situations, such as various recreational facilities and involvement in social activities.
Another finding of this study is the effect of childlessness on social status. Based on the findings of this study, childlessness can affect people’s social participation. According to a survey, childlessness can reduce social activities and communication with family, neighbors, and society [28]. Another study found that those who never had children have smaller networks of older people than parents, partially attributed to a more limited number of relatives [52]. A study found that older people without children, regardless of marital status and gender, are just as likely as those with children to participate in community and voluntary organizations and volunteer work [53]. Consistent with the present study, based on the survey results, fatherhood encourages men to have extensive intergenerational and family interactions [54].
The limitation of this study was the low panel studies regarding childlessness or having one child couples and its effect on their health status. In addition, we could not perform a meta-analysis due to the impossibility of data such as relative risk from included studies. The strength of this study was that it was the first systematic review of cohort and panel studies that addressed the impact of childlessness or having one child on a couple’s health status.
Conclusion
This study assessed the effects of childlessness on a couple’s health using a biopsychosocial approach. The study results indicate that childless couples may have various health problems in biological, psychological, and social aspects, which, in general, negatively affect their quality of life. Due to the considerable decrease in total fertility rate and population growth, the number of childless couples will increase in the future, and these individuals will be at high risk of physical, mental, and social challenges. Therefore, the results of this systematic review can be a good resource for policymakers and health specialists to design and implement cost-effective interventions to improve fertility indicators among the Iranian population. In addition, due to limited information regarding childlessness’s effects on a couple’s health, conducting precise studies with high-quality methodology is proposed in the future.
Ethical Considerations
Compliance with ethical guidelines
This systematic review was conducted according to PRISMA in 2020. Before conducting this study, its protocol was registered in the PROSPERO (Code: CRD42023491821).
Funding
This study was financially supported by Mazandaran University of Medical Sciences, Sari, Iran.
Authors contributions
Conceptualization and supervision: Zohreh Shah Hosseini; Investigation and writing the original draft: Marzieh Azizi and Fereshteh Yazdani; Review and editing: Roya Nikbakht and Marzieh Azizi.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors thank Mazandaran University of Medical Sciences, Sari, Iran for supporting this study.
References
- Tocchioni V. Exploring the childless universe: Profiles of women and men without children in Italy. Demogr Res. 2018; 38:451-70. [DOI:10.4054/DemRes.2018.38.19]
- Rowland DT. Historical trends in childlessness. J Fam Issues. 2007; 28(10):1311-37. [DOI:10.1177/0192513X07303823]
- Okpan SO, Otega O. Socio-cultural consequences of being childless; perspectives across Africa and Europe. Niger J Soc Probl Soc Policy Rev 2021; 1(2). [Link]
- Patel DN. A road without a map: An interpretative phenomenological analysis of intentional childlessness in Indian American women [PhD dissertation]. San Antonio: The University of Texas at; 2023. [Link]
- Miettinen A, Rotkirch A, Szalma I, Donno A, Tanturri ML. Increasing childlessness in Europe: Time trends and country differences. Maastricht: European :union:'s; 2015. [Link]
- Fekri kia R, Pejhan A. [Investigating the demographic and economic characteristics of single-child households in Iran in the 2013 (Persian)]. Soc Res. 2013; 28(7):169-86. [Link]
- Bagi M. Prevalence, reasons and consequences of childlessness in the world and Iran: A systematic review. J Popul Assoc Iran. 2023; 18(35):97-148. [DOI:10.22034/jpai.2023.2004173.1292]
- Foroutan Y, Bijani HR. [Childlessness in Iran: Findings and solutions (Persian)]. J Popul Assoc Iran. 2021; 16(32):177-203. [DOI:10.22034/jpai.2022.535805.1192]
- Nasrabad HBR, Abbasi-Shavazi MJ, Hosseini-Chavoshi M, Karegar-Shoraki MR. Trend and patterns of childlessness in Iran. Paper presented at: The XXVII International Population Conference of the IUSSP. 26-31 August 2013, Busan, Korea. [Link]
- Zhang W, Liu G. Childlessness, psychological wellbeing, and life satisfaction among the elderly in China. J Cross Cult Gerontol. 2007; 22(2):185-203. [DOI:10.1007/s10823-007-9037-3] [PMID]
- Feng Z. Childlessness and vulnerability of older people in China. Age Ageing. 2018; 47(2):275-81. [DOI:10.1093/ageing/afx137] [PMID]
- Huijts T, Kraaykamp G, Subramanian SV. Childlessness and psychological wellbeing in context: A multilevel study on 24 European countries. Eur Sociol Rev. 2013; 29(1):32-47. [DOI:10.1093/esr/jcr037]
- Vikström J, Bladh M, Hammar M, Marcusson J, Wressle E, Sydsjö G. The influences of childlessness on the psychological wellbeing and social network of the oldest old. BMC Geriatr. 2011; 11:78. [DOI:10.1186/1471-2318-11-78] [PMID]
- Bhaskar S. Childlessness, parenthood and psychological wellbeing. Recent Adv Psychol. 2017; 4(2):42-51. [Link]
- Sappleton N. Voluntary and Involuntary Childlessness. In: Nordqvist P, Hudson N, editors. Emerald studies in reproduction, culture and society. Bingley: Emerald Publishing Limited; 2018. [DOI:10.1108/9781787543614]
- Yahyanejad A, Hamzehgardeshi Z, Mousavinasab SN, Azizi M, Shahhosseini Z. The role of social capital on unwillingness toward childbearing in reproductive-aged women. J Nurs Midwifery Sci. 2022; 9(1):73-9. [Link]
- Heravi M, Cheraghi Koutiani E, Herati M. [Analysis of single child injuries for parents with a religious and psychological approach (Persian)]. Q J Islam Stud Soc Inj. 2020; 2(1):163-82. [Link]
- Behmanesh F, Taghizadeh Z, Vedadhir A, Ebadi A, Pourreza A, Abbasi Shavazi M. [Explaining the causes of single child based on women’s views: A qualitative Study (Persian)]. Iran J Epidemiol. 2019; 15(3):279-88. [Link]
- Jun-qing F. The causes and solutions on the problems of child rearing in single-parent family. Proceedings of the 2020 4th International Seminar on Education, Management and Social Sciences (ISEMSS 2020). Dordrecht: Atlantis Press; 2020. [DOI:10.2991/assehr.k.200826.253]
- Card AJ.The biopsychosociotechnical model: a systems-based framework for human-centered health improvement. Health Syst (Basingstoke). 2022; 12(4):387-407. [DOI:10.1080/20476965.2022.2029584] [PMID]
- Bolton D, Gillett G. Biopsychosocial conditions of health and disease. In: The Biopsychosocial Model of Health and Disease. Cham: Palgrave Pivot; 2019. [DOI:10.1007/978-3-030-11899-0_4]
- Beaujouan E, Brzozowska Z, Zeman K. Childlessness trends in twentieth-century Europe: Limited link to growing educational attainment. Vienna: Vienna Institute of Demography Working Papers; 2015. [Link]
- Budig MJ, Misra J, Boeckmann I. The motherhood penalty in cross-national perspective: The importance of work-family policies and cultural attitudes. Soc Polit. 2012; 19(2):163-93. [DOI:10.1093/sp/jxs006]
- Klaus D, Schnettler S. Social networks and support for parents and childless adults in the second half of life: Convergence, divergence, or stability? Adv Life Course Res. 2016; 29:95-105. [DOI:10.1016/j.alcr.2015.12.004]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021; 372:n71. [DOI:10.1136/bmj.n71] [PMID]
- Margulis AV, Pladevall M, Riera-Guardia N, Varas-Lorenzo C, Hazell L, Berkman ND, et al. Quality assessment of observational studies in a drug-safety systematic review, comparison of two tools: The Newcastle-Ottawa scale and the RTI item bank. Clin Epidemiol. 2014; 6:359-68. [DOI:10.2147/CLEP.S66677] [PMID]
- Luchini C, Stubbs B, Solmi M, Veronese N. Assessing the quality of studies in meta-analyses: Advantages and limitations of the Newcastle Ottawa Scale. World J MetaAnal. 2017; 5(4):80-4. [Link]
- Keizer R, Dykstra PA, Poortman AR. Life outcomes of childless men and fathers. Eur Sociol Rev. 2010; 26(1):1-15. [DOI:10.1093/esr/jcn080]
- Elenkov A, Giwercman A, Søgaard Tøttenborg S, Bonde JPE, Glazer CH, Haervig KK, et al. Male childlessness as independent predictor of risk of cardiovascular and all-cause mortality: A population-based cohort study with more than 30 years follow-up. Plos One. 2020; 15(9):e0237422.[DOI:10.1371/journal.pone.0237422] [PMID]
- Bungum AB, Glazer CH, Bonde JP, Nilsson PM, Giwercman A, Søgaard Tøttenborg S. Risk of metabolic disorders in childless men: A population-based cohort study. BMJ Open. 2018; 8(8):e020293. [DOI:10.1136/bmjopen-2017-020293] [PMID]
- Hansen T, Slagsvold B, Moum T. Childlessness and psychological wellbeing in midlife and old age: An examination of parental status effects across a range of outcomes. Soc Indic Res. 2009; 94:343-62. [DOI:10.1007/s11205-008-9426-1]
- Davis DL, Wu C, Brown WJ, Nohr EA. Parity and mode of birth and their relationships with quality of life: A longitudinal study. Plos One. 2022; 17(9):e0273366. [DOI:10.1371/journal.pone.0273366] [PMID]
- Zhang Z, Hayward MD. Childlessness and the psychological wellbeing of older persons. J Gerontol B Psychol Sci Soc Sci. 2001; 56(5):S311-20. [DOI:10.1093/geronb/56.5.S311] [PMID]
- Quashie NT, Arpino B, Antczak R, Mair CA. Childlessness and health among older adults: Variation across five outcomes and 20 countries. J Gerontol B Psychol Sci Soc Sci. 2021; 76(2):348-59. [DOI:10.1093/geronb/gbz153] [PMID]
- Miettinen A. Voluntary or involuntary childlessness? Socio-demographic factors and childlessness intentions among childless Finnish men and women aged 25-44. Finnish Yearb Popul Res. 2010; 45:5–24. [DOI:10.23979/fypr.45051]
- Rybińska A, Morgan SP. Childless expectations and childlessness over the life course. Soc Forces. 2019; 97(4):1571-602. [DOI:10.1093/sf/soy098] [PMID]
- Bener A, Al-Ansari AA, Zirie M, Al-Hamaq AO. Is male fertility associated with type 2 diabetes mellitus? Int Urol Nephrol. 2009; 41(4):777-84. [DOI:10.1007/s11255-009-9565-6] [PMID]
- Ventimiglia E, Capogrosso P, Boeri L, Serino A, Colicchia M, Ippolito S, et al. Infertility as a proxy of general male health: Results of a cross-sectional survey. Fertil Steril. 2015; 104(1):48-55. [DOI:10.1016/j.fertnstert.2015.04.020] [PMID]
- Salonia A, Matloob R, Gallina A, Abdollah F, Saccà A, Briganti A, et al. Are infertile men less healthy than fertile men? Results of a prospective case-control survey. Eur Urol. 2009; 56(6):1025-31. [DOI:10.1016/j.eururo.2009.03.001] [PMID]
- Kasturi SS, Tannir J, Brannigan RE. The metabolic syndrome and male infertility. J Androl. 2008; 29(3):251-9. [DOI:10.2164/jandrol.107.003731] [PMID]
- Chen PC, Chen YJ, Yang CC, Lin TT, Huang CC, Chung CH, et al. Male infertility increases the risk of cardiovascular diseases: A nationwide population-based cohort study in Taiwan. World J Mens Health. 2022; 40(3):490-500. [DOI:10.5534/wjmh.210098] [PMID]
- Farland LV, Wang YX, Gaskins AJ, Rich-Edwards JW, Wang S, Magnus MC, et al. Infertility and risk of cardiovascular disease: A prospective cohort study. J Am Heart Assoc. 2023; 12(5):e027755. [DOI:10.1161/JAHA.122.027755] [PMID]
- Glazer CH, Bonde JP, Eisenberg ML, Giwercman A, Hærvig KK, Rimborg S, et al. Male infertility and risk of nonmalignant chronic diseases: A systematic review of the epidemiological evidence. Semin Reprod Med. 2017; 35(3):282-90. [PMID]
- Agerbo E, Mortensen PB, Munk-Olsen T. Childlessness, parental mortality and psychiatric illness: A natural experiment based on in vitro fertility treatment and adoption. J Epidemiol Community Health. 2013; 67(4):374-6.[DOI:10.1136/jech-2012-201387] [PMID]
- Einiö E, Nisén J, Martikainen P. Number of children and later-life mortality among Finns born 1938-50. Popul Stud (Camb). 2016; 70(2):217-38. [DOI:10.1080/00324728.2016.1195506] [PMID]
- Grundy E, Kravdal Ø. Fertility history and cause-specific mortality: A register-based analysis of complete cohorts of Norwegian women and men. Soc Sci Med. 2010; 70(11):1847-57. [DOI:10.1016/j.socscimed.2010.02.004] [PMID]
- Mohaddesi H, Khalkhali HR, Behrozi-lak T, Rasouli J, Edalat Nemoon R, Ghasemzadeh S. Correlation between marital satisfaction and mental health in infertile couples referred to kosar infertility clinic in urmia: A cross-sectional study. J Obstet Gynecol Cancer Res. 2022;7(4):341-7. [DOI:10.30699/jogcr.7.4.341]
- Chou KL, Chi I. Childlessness and psychological well-being in Chinese older adults. Int J Geriatr Psychiatry. 2004; 19(5):449-57. [DOI:10.1002/gps.1111] [PMID]
- Graham M. Is being childless detrimental to a woman’s health and wellbeing across her life course? Womens Health Issues. 2015; 25(2):176-84. [DOI:10.1016/j.whi.2014.12.002] [PMID]
- Bures RM, Koropeckyj-Cox T, Loree M. Childlessness, parenthood, and depressive symptoms among middle-aged and older adults. J Fam Issues. 2009; 30(5):670-87. [DOI:10.1177/0192513X08331114]
- Maximova K, Quesnel-Vallée A. Mental health consequences of unintended childlessness and unplanned births: Gender differences and life course dynamics. Soc Sci Med. 2009; 68(5):850-7. [DOI:10.1016/j.socscimed.2008.11.012] [PMID]
- Dykstra PA. Off the beaten track: Childlessness and social integration in late life. Res Aging. 2006; 28(6):749-67. [DOI:10.1177/0164027506291745]
- Wenger GC, Dykstra PA, Melkas T, Knipscheer CPM. Social embeddedness and late-life parenthood: Community activity, close ties, and support networks. J Fam Issues. 2007; 28(11):1419-56. [DOI:10.1177/0192513X07303895]
- Knoester C, Eggebeen DJ. The effects of the transition to parenthood and subsequent children on men’s wellbeing and social participation. J Fam Issues. 2006; 27(11):1532-60. [DOI:10.1177/0192513X06290802]
Type of Study: Systematic Review |
Subject:
Pediatrics
Received: 2024/07/25 | Accepted: 2025/01/1 | Published: 2025/01/21
Received: 2024/07/25 | Accepted: 2025/01/1 | Published: 2025/01/21
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |










