Volume 12, Issue 4 (10-2024)
J. Pediatr. Rev 2024, 12(4): 321-328 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Aduramo E, Esan D T, Adesuyi E, Olabode O, Awoniyi E, Oyama B et al . Exploring Developmental Care in Neonatal Jaundice Management: A Case Report with Supporting Literature Synthesis. J. Pediatr. Rev 2024; 12 (4) :321-328
URL: http://jpr.mazums.ac.ir/article-1-678-en.html
URL: http://jpr.mazums.ac.ir/article-1-678-en.html
Esther Aduramo *1 

 , Deborah T. Esan2
, Deborah T. Esan2 

 , Emmanuel Adesuyi3
, Emmanuel Adesuyi3 

 , Opeoluwa Olabode3
, Opeoluwa Olabode3 
 , Elizabeth Awoniyi3
, Elizabeth Awoniyi3 

 , Blessed Oyama3
, Blessed Oyama3 
 , Oluwadamilare Akingbade3
, Oluwadamilare Akingbade3 



 , Deborah T. Esan2
, Deborah T. Esan2 

 , Emmanuel Adesuyi3
, Emmanuel Adesuyi3 

 , Opeoluwa Olabode3
, Opeoluwa Olabode3 
 , Elizabeth Awoniyi3
, Elizabeth Awoniyi3 

 , Blessed Oyama3
, Blessed Oyama3 
 , Oluwadamilare Akingbade3
, Oluwadamilare Akingbade3 

1- Department of Research and Statistics, Institute of Nursing Research, Osogbo, Nigeria. , eniolacrown02@gmail.com
2- Faculty of Nursing, Bowen University, Iwo, Nigeria.
3- Department of Research and Statistics, Institute of Nursing Research, Osogbo, Nigeria.
2- Faculty of Nursing, Bowen University, Iwo, Nigeria.
3- Department of Research and Statistics, Institute of Nursing Research, Osogbo, Nigeria.
Full-Text [PDF 409 kb]
(1851 Downloads)
| Abstract (HTML) (2844 Views)
Full-Text: (1353 Views)
Introduction
Neonatal jaundice or neonatal hyperbilirubinemia is one of the most common medical conditions in newborn babies. All babies have a transient rise in serum bilirubin and about 75% are visibly jaundiced [1]. Jaundice is clinically detectable when the serum bilirubin levels are >85 μmol/L (5 mg/dL) [2].
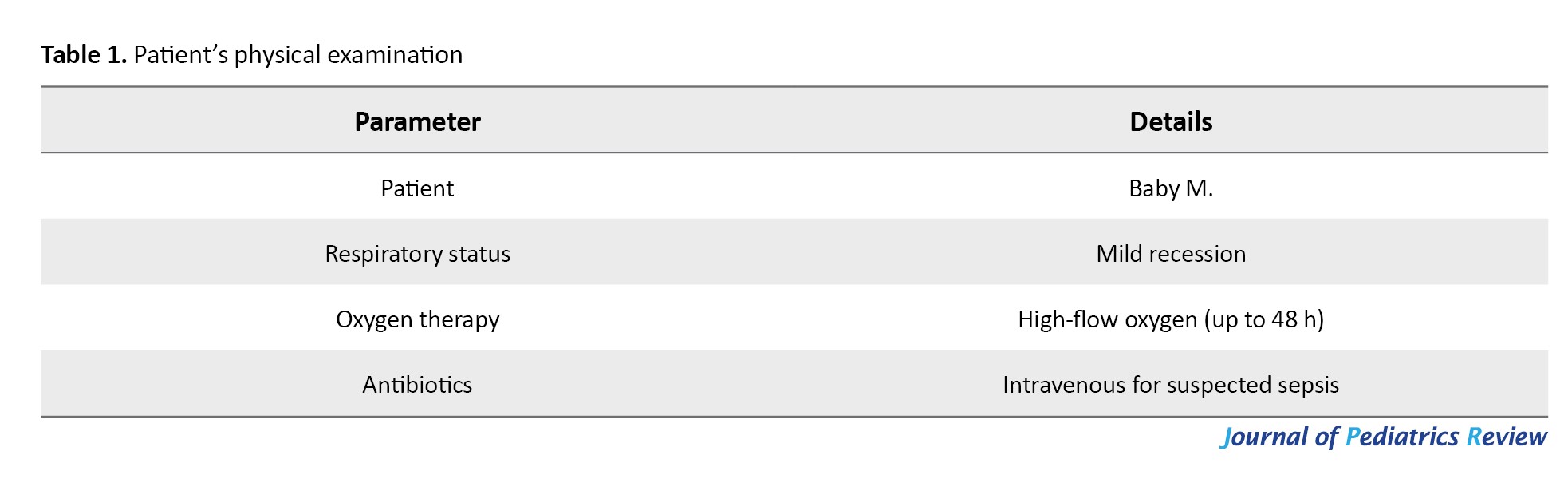
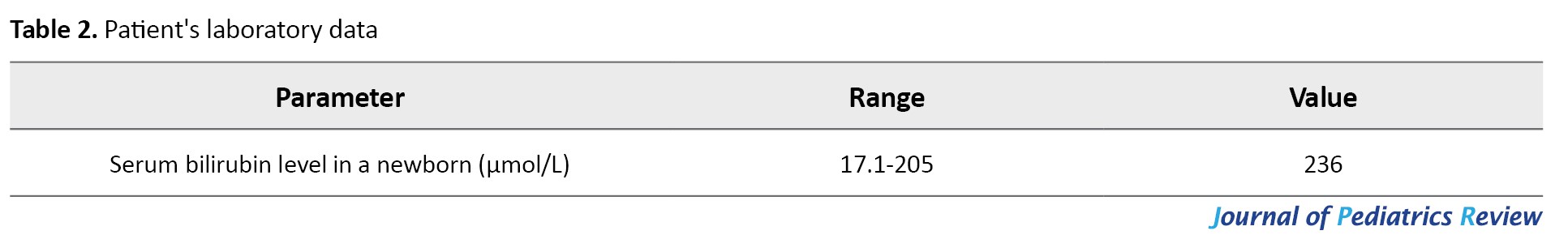
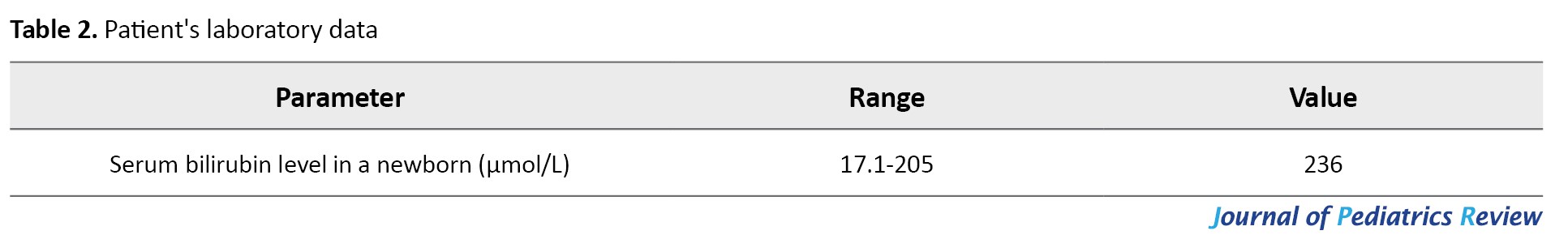
Jaundice refers to a phenomenon that occurs during the first few days of life because of elevated levels of unconjugated bilirubin in the blood [3]. Disruptions in the production and elimination of bilirubin have been identified as the key factors causing neonatal hyperbilirubinemia [4]. The free bilirubin is lipid-soluble and can cross the blood-brain barrier [5]. The incidence of neonatal jaundice was 244.1 per 10000 live births in low-middle-income countries, compared to 3.7 per 10 000 live births in high-income countries [6]. Several factors have been associated with neonatal jaundice. These include infection, rhesus-incompatibility, hypoxia, low birth weight, breastfeeding, hyperbilirubinemia in siblings, glucose-6-phosphate dehydrogenase deficiency, ABO incompatibility, preterm birth and/or the use of oxytocin, polycythemia, and being an infant of a diabetic mother [5, 7, 8]. Tables 1 and 2 present Baby M’s physical examination and laboratory data.
This case report demonstrates how developmental care components can be tailored to manage neonatal jaundice in preterm neonates through a holistic, family-centered, evidence-based approach. Reflecting on current practices encourages healthcare providers to align jaundice management with updated evidence, emphasizing individualized care to enhance outcomes. It also promotes a participatory role for parents, offering educational resources and guidance on practices like feeding and phototherapy. This approach fosters bonding, reduces parental stress, and supports improved neonatal outcomes in a more family-centered neonatal intensive care unit (NICU) environment.
Case Presentation
The subject was a female preterm neonate born at 32+5 weeks of gestation, delivered through cesarean section due to maternal complications, including fibroids, anemia, hypercalcemia, hypomagnesemia, hypokalaemia, and pregnancy-induced hypertension. The subject, “Baby M” was born and cared for at a specialized unit for preterm and critically ill neonates in one of the level 1 hospitals in Kent, United Kingdom. At birth, she required resuscitation with two sets of inflation. Her care was guided by the March 2023 updated version of the National Institute for Health and Care Excellence (NICE), based on the hospital policy.
Upon admission, Baby M presented with prematurity, ventriculomegaly, and bilateral talipes. She exhibited mild respiratory distress, necessitating high-flow oxygen therapy for 48 h, and was started on intravenous antibiotics due to suspected sepsis. On day two, her serum bilirubin level was observed to be 236 μmol/L, exceeding the treatment threshold per the NICE guideline for the management of jaundice. Phototherapy was initiated based on her gestational age and postnatal age.
In the first few days of life, intravenous fluids were administered due to her respiratory difficulties. By day three, she transitioned to her mother’s expressed breast milk because of the importance of breastmilk [2, 9], a preference strongly supported by Baby M’s mother. Comprehensive breastfeeding support was provided, including guidance on positioning during breastfeeding, frequency, maternal nutrition, hygiene, and breast milk storage. Baby M’s mother was also loaned a hospital pump to encourage her to keep expressing breast milk at home during her baby’s hospital stay.
Throughout her care, Baby M’s serum bilirubin levels were regularly monitored while receiving phototherapy adhering strictly to hospital policy and NICE guidelines [9]. Phototherapy was applied with proper positioning and temperature regulation, ensuring Baby M was kept in a thermoneutral environment to minimize energy expenditure [2]. Although parental support during neonatal care was emphasized in the NICE guideline, specific strategies to reduce stress and optimize neurobehavioural development during phototherapy were not explicitly included. However, parents were reassured that nappy changes and feeding could continue during phototherapy to foster parental involvement. This approach aligns with developmental care principles, promoting parental participation potentially improving neonatal outcomes, and reducing hospitalization duration [10]. Baby M was discharged from the unit after two weeks and three days of admission.
Discussion
This case report presents a review of the literature on how developmental care components can be adapted to the management of neonatal jaundice. According to a systematic review of the global estimates of preterm births in 2020, about 13.4 million babies were born prematurely across the globe [11]. Although there have been huge developments in medical sciences, especially neonatology-perinatology, the medical needs and long-term hospitalization of pre-term neonates remain significantly high [12]. Neonatal jaundice is responsible for the highest number of neonatal unit admissions, because about 60% of term and 80% of preterm usually require admission for jaundice, especially in the first week of life [2]. Although neonates with severe hyperbilirubinemia are at risk for bilirubin encephalopathy and kernicterus spectrum disorder [3], the risk of adverse outcomes is higher among preterm compared to term newborn babies [11].
Developmental care approach to jaundice management
Nurses play a crucial role in the care and management of neonatal jaundice, with studies emphasizing the importance of nursing interventions in promoting the recovery of affected newborns [13]. Moreover, the assessment of knowledge and skills of maternity care professionals regarding neonatal hyperbilirubinemia underscores the essential role of healthcare professionals, including nurses, in the timely recognition and management of severe neonatal jaundice [14]. Additionally, the provision of developmental care by nurses in the neonatal unit has been linked to improved quality of care and minimized complications upon discharge [15]. Several studies have highlighted the significance of developmental care in promoting the well-being of preterm infants [16].
Developmental care consists of a range of medical and nursing interventions that are targeted at promoting the comfort of the neonate while minimizing newborn-parental separation by promoting the participation of the parents in the care of their newborn during admission into the neonatal unit [17]. The components of developmental care that will be analyzed in this article include minimizing exposure to pain and stress, minimizing parent-infant separation, skin-to-skin care, and optimizing nutrition [10, 18]. The trend results from these neuroprotective interventions have resulted in improved outcomes for preterm neonates in terms of growth, reduced need for respiratory support, and reduction in the cost of hospitalization and length of stay in the hospital [10, 18, 19]. Developmental care interventions also promote the bonding of the neonates with their parents, improve parental confidence in the provision of care following discharge, and reduce the risks of maternal stress and depression [10] that may result from separation and prolonged hospital stay of the preterm neonate during management for jaundice.
Researchers have emphasized the importance of diagnosing neonatal jaundice promptly to prevent its associated short and long-term sequelae [3]. Visual inspection alone is an unreliable tool for diagnosing jaundice [3]. Consequent to reliance on visual inspection alone, a significant proportion of severe hyperbilirubinemia have been misclassified, and others unnoticed by healthcare providers and or parents [3]. Although blood sample investigations have been confirmed reliable in diagnosing a wide range of abnormalities in pre-term neonates [2], the use of transcutaneous devices has also been reported to facilitate early recognition of neonatal jaundice [20]. Similarly, transcutaneous bilirubin measurement may offer a non-invasive, immediate approach to screening for hyperbilirubinemia among preterm neonates [21]. Preterm neonates, therefore, do not need to be subjected to frequent needle pricks due to the need to carry out investigations regularly.
The need to perform invasive procedures for diagnosis and prompt treatment has made hospitalized neonates the most frequent subjects of painful heel lancing, in the first week/month of their lives [12]. These authors observed that frequent exposure to painful procedures is not only associated with poor pain perception, threshold, and tolerance among such neonates, but they are also at a higher risk for neurobehavioural adverse effects [12]. This can also be associated with worsening clinical status. Accordingly, it is essential to effectively manage and prevent pain among preterm neonates to promote their physical comfort and stabilize their physiological parameters [12]. Pain experience can be alleviated by olfactory and gustatory stimuli from the infant’s mother’s breast milk [22]. The transcutaneous bilirubin measurement can also be explored for assessment during management, to minimize the need for frequent heel prick [3].
Although pain management during heel lancing for bilirubin level assessment among pre-term neonates undergoing phototherapy can be achieved using pharmacological and non-pharmacological approaches, the non-pharmacological approach is preferred due to the side effects of medications [23]. Some of the non-pharmacological approaches that are used for pain management among preterm neonates include oral sucrose, gentle human touch, massage, breastfeeding, white noise and the use of pacifier or non-nutritive sucking [23]. In another randomized control trial that assessed the use of breastmilk for pain relief during newborn screening procedures, researchers concluded that gentle human touch, in combination with the taste and odor of breastmilk, provided relief for neonates during the heel lancing for the screening [24].
Exclusive breastfeeding has been identified as a risk factor for neonatal jaundice among infants with difficulty feeding, emphasizing the need for careful monitoring and support for breastfeeding mothers [25]. Exclusive breastfeeding offers some protection against infants without feeding difficulties [25]. However, breastfed newborns have still been observed to be jaundiced after about one month of life [2]. To offer effective prevention from neonatal jaundice, early and adequate breastfeeding would need to be introduced to the infant [26]. Reports from recent findings have associated the increased levels of bilirubin in breastfed infants with failure to establish breastfeeding [27]. Therefore, improving breastfeeding support and education will likely reduce neonatal jaundice and associated hospital readmissions [28, 29]. Hence, nurses need to provide comprehensive support and education to mothers to ensure proper breastfeeding and to effectively manage neonatal jaundice [30].
Parental participation in the care and feeding of neonates prevents undue separation of the neonates from their parents and the associated feeling of lack of control [9, 14]. Parental participation in care ultimately culminates in effective bonding and improved mental health for the mother [14]. The other benefits of a positive environment include reduced stress for the neonate, optimized neurobehavioural development, and reduced length of stay during hospitalization [14]. In a retrospective study of the effect of continuous and intermittent phototherapy among neonates with hemolytic jaundice, there was no significant difference in the efficiency of phototherapy in the continuous and intermittent groups [5]. Conversely, they recorded a significantly higher occurrence of adverse effects among the continuous phototherapy group than the intermittent phototherapy group [5].
Intermittent phototherapy has been documented to be tolerable and effective among neonates with jaundice; however, there is a lack of evidence to suggest what frequency and length of interruption would affect the effectiveness of the management [9]. Based on the reports from previous studies, the author recommends exploring the effectiveness of intermittent phototherapy to allow more time for cuddles and parental contact with the newborn, as recommended in previous studies [5].
Phototherapy is a major line of treatment for neonatal jaundice because it reduces serum bilirubin levels through photoisomerization, structural isomerization, and photo-oxidation [30]. Phototherapy is considered a safe and well-tolerated therapy for neonatal jaundice [30–32]. It was similarly posited in the prospective observational study that phototherapy helps protect the brain from the effect of unconjugated bilirubin fraction [8]. Neonates with lower gestational age and birthweight require long-term phototherapy, which has consequent adverse effects among these small and vulnerable infants [13]. Parents are often encouraged to participate in nappy changes and feeding of their neonates during phototherapy. Intermittent phototherapy has been documented to be tolerable and effective among neonates with jaundice, but there is a lack of evidence to suggest what frequency and length of interruption would affect the effectiveness of the management [2]. The NICE guideline for managing neonatal jaundice provides information on the importance of continued parental interaction during phototherapy. However, the frequency and length of interruption that would affect the effectiveness of phototherapy were not included [2]. Based on the reports from previous studies, the author recommends exploring the effectiveness of intermittent phototherapy to allow more time for cuddles and parental contact with the newborn [5].
There have been anecdotal reports that the involvement of parents in the management of hospitalized neonates with jaundice has been streamlined to feeding. However, the provision of information on the signs of jaundice during the hospitalization period and involving parents in the management of hospitalized neonates with jaundice goes beyond feeding [2]. Parental support in neonatal care, with information for parents usually including the anticipated period of treatment and reassurance that nappy changes and feeding can usually continue during the period of phototherapy, were also included in the NICE guideline for the management of neonatal jaundice [9]. Maternal knowledge and early care-seeking behavior have been identified as fundamental components of the effective management of neonatal jaundice, highlighting the need for comprehensive education and support for caregivers [24].
The intensity of the phototherapy was not assessed, and therefore, the management length could not be estimated. This contrasts with the guidelines provided by NICE, where the duration of management of jaundice could be estimated based on the type of phototherapy being used, therefore assisting the healthcare providers in providing information to parents on the anticipated duration of therapy [2].
Implication to practice
The benefits of early maternal-infant interactions are overwhelming; thus, there is a need for collaboration to minimize parent-infant separation that is associated with the management of neonates with jaundice [17]. This can be partly achieved by providing continuing education for nurses on family-centered developmental care strategies to facilitate improved outcomes for neonates with jaundice [17]. Moreover, intermittent phototherapy rather than continuous phototherapy should be explored to prevent unnecessary separation and promote bonding between pre-term neonates undergoing phototherapy and their parents. Non-pharmacological measures for pain management, especially during heel lancing for preterm neonates undergoing heel lancing, should be adopted to minimize the neurological consequences associated with the procedure. The overall care and experience of neonatal jaundice can also be improved by welcoming new advancements in pain relief strategies and non-invasive methods of assessment of bilirubin levels.
There is a need to provide information on the signs of jaundice during the antenatal period, and involving parents in the management of hospitalized neonates with jaundice should be supported beyond feeding. There is also a need to identify evidence-based strategies for assessing the intensity of phototherapy to estimate the length of management and provide information to parents on the anticipated duration of therapy. Correspondingly, the authors recommend exploring the effectiveness of intermittent phototherapy and the frequency and length of interruption that would affect the management of neonatal jaundice. Educational resources should be made available to parents during admission. The materials should provide information on “how,” and “to what extent” parents can participate in the care so that nursing and medical care of the neonate with jaundice are not jeopardized [17]. Also, exclusive breastfeeding support and guidance should be provided, acknowledging the individual circumstances and needs of both the mother and neonate [23].
Conclusion
In conclusion, the management of neonatal jaundice requires a multidisciplinary approach, involving developmental care and nursing care. Educating caregivers and healthcare professionals, along with implementing evidence-based management strategies, is essential for improving outcomes and reducing the burden of neonatal jaundice.
Study limitations
The report was limited to a preterm neonate with no other significant medical or surgical condition within the hospital setting. Developmental care focuses on creating a supportive environment tailored to a newborn's sensory, physical, and emotional needs to promote healthy growth, comfort, and bonding with parents. While these interventions are especially emphasized for preterm infants due to the unique challenges of early birth, full-term infants can also benefit from techniques like gentle handling, minimization of stress, and enhanced parental involvement, particularly when they are medically fragile or undergoing intensive treatment.
Ethical Considerations
Compliance with ethical guidelines
The management of Baby M was guided by the ethical principles of the hospital, primarily focusing on the best interests of the neonate, informed consent, parental involvement and adherence to established clinical guidelines. The healthcare team ensured that Baby M's treatment adhered to the NICE guidelines, which are based on evidence-based best practices. These guidelines were followed to provide the most appropriate and effective treatment for neonatal jaundice, minimizing risks while optimizing outcomes.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization: Esther Aduramo; Supervision: Deborah Esan; Methodology: Oluwadamilare Akingbade, Deborah Esan, Emmanuel Adesuyi, and Esther Aduramo; Writing the original draft: Esther Aduramo; Review and editing: Esther Aduramo, Deborah Esan, Oluwadamilare Akingbade, Opeoluwa Olabode, Elizabeth Awoniyi, Blessed Oyama.
Conflicts of interest
The authors declared no conflict of interest.
References
Neonatal jaundice or neonatal hyperbilirubinemia is one of the most common medical conditions in newborn babies. All babies have a transient rise in serum bilirubin and about 75% are visibly jaundiced [1]. Jaundice is clinically detectable when the serum bilirubin levels are >85 μmol/L (5 mg/dL) [2].
Jaundice refers to a phenomenon that occurs during the first few days of life because of elevated levels of unconjugated bilirubin in the blood [3]. Disruptions in the production and elimination of bilirubin have been identified as the key factors causing neonatal hyperbilirubinemia [4]. The free bilirubin is lipid-soluble and can cross the blood-brain barrier [5]. The incidence of neonatal jaundice was 244.1 per 10000 live births in low-middle-income countries, compared to 3.7 per 10 000 live births in high-income countries [6]. Several factors have been associated with neonatal jaundice. These include infection, rhesus-incompatibility, hypoxia, low birth weight, breastfeeding, hyperbilirubinemia in siblings, glucose-6-phosphate dehydrogenase deficiency, ABO incompatibility, preterm birth and/or the use of oxytocin, polycythemia, and being an infant of a diabetic mother [5, 7, 8]. Tables 1 and 2 present Baby M’s physical examination and laboratory data.
This case report demonstrates how developmental care components can be tailored to manage neonatal jaundice in preterm neonates through a holistic, family-centered, evidence-based approach. Reflecting on current practices encourages healthcare providers to align jaundice management with updated evidence, emphasizing individualized care to enhance outcomes. It also promotes a participatory role for parents, offering educational resources and guidance on practices like feeding and phototherapy. This approach fosters bonding, reduces parental stress, and supports improved neonatal outcomes in a more family-centered neonatal intensive care unit (NICU) environment.
Case Presentation
The subject was a female preterm neonate born at 32+5 weeks of gestation, delivered through cesarean section due to maternal complications, including fibroids, anemia, hypercalcemia, hypomagnesemia, hypokalaemia, and pregnancy-induced hypertension. The subject, “Baby M” was born and cared for at a specialized unit for preterm and critically ill neonates in one of the level 1 hospitals in Kent, United Kingdom. At birth, she required resuscitation with two sets of inflation. Her care was guided by the March 2023 updated version of the National Institute for Health and Care Excellence (NICE), based on the hospital policy.
Upon admission, Baby M presented with prematurity, ventriculomegaly, and bilateral talipes. She exhibited mild respiratory distress, necessitating high-flow oxygen therapy for 48 h, and was started on intravenous antibiotics due to suspected sepsis. On day two, her serum bilirubin level was observed to be 236 μmol/L, exceeding the treatment threshold per the NICE guideline for the management of jaundice. Phototherapy was initiated based on her gestational age and postnatal age.
In the first few days of life, intravenous fluids were administered due to her respiratory difficulties. By day three, she transitioned to her mother’s expressed breast milk because of the importance of breastmilk [2, 9], a preference strongly supported by Baby M’s mother. Comprehensive breastfeeding support was provided, including guidance on positioning during breastfeeding, frequency, maternal nutrition, hygiene, and breast milk storage. Baby M’s mother was also loaned a hospital pump to encourage her to keep expressing breast milk at home during her baby’s hospital stay.
Throughout her care, Baby M’s serum bilirubin levels were regularly monitored while receiving phototherapy adhering strictly to hospital policy and NICE guidelines [9]. Phototherapy was applied with proper positioning and temperature regulation, ensuring Baby M was kept in a thermoneutral environment to minimize energy expenditure [2]. Although parental support during neonatal care was emphasized in the NICE guideline, specific strategies to reduce stress and optimize neurobehavioural development during phototherapy were not explicitly included. However, parents were reassured that nappy changes and feeding could continue during phototherapy to foster parental involvement. This approach aligns with developmental care principles, promoting parental participation potentially improving neonatal outcomes, and reducing hospitalization duration [10]. Baby M was discharged from the unit after two weeks and three days of admission.
Discussion
This case report presents a review of the literature on how developmental care components can be adapted to the management of neonatal jaundice. According to a systematic review of the global estimates of preterm births in 2020, about 13.4 million babies were born prematurely across the globe [11]. Although there have been huge developments in medical sciences, especially neonatology-perinatology, the medical needs and long-term hospitalization of pre-term neonates remain significantly high [12]. Neonatal jaundice is responsible for the highest number of neonatal unit admissions, because about 60% of term and 80% of preterm usually require admission for jaundice, especially in the first week of life [2]. Although neonates with severe hyperbilirubinemia are at risk for bilirubin encephalopathy and kernicterus spectrum disorder [3], the risk of adverse outcomes is higher among preterm compared to term newborn babies [11].
Developmental care approach to jaundice management
Nurses play a crucial role in the care and management of neonatal jaundice, with studies emphasizing the importance of nursing interventions in promoting the recovery of affected newborns [13]. Moreover, the assessment of knowledge and skills of maternity care professionals regarding neonatal hyperbilirubinemia underscores the essential role of healthcare professionals, including nurses, in the timely recognition and management of severe neonatal jaundice [14]. Additionally, the provision of developmental care by nurses in the neonatal unit has been linked to improved quality of care and minimized complications upon discharge [15]. Several studies have highlighted the significance of developmental care in promoting the well-being of preterm infants [16].
Developmental care consists of a range of medical and nursing interventions that are targeted at promoting the comfort of the neonate while minimizing newborn-parental separation by promoting the participation of the parents in the care of their newborn during admission into the neonatal unit [17]. The components of developmental care that will be analyzed in this article include minimizing exposure to pain and stress, minimizing parent-infant separation, skin-to-skin care, and optimizing nutrition [10, 18]. The trend results from these neuroprotective interventions have resulted in improved outcomes for preterm neonates in terms of growth, reduced need for respiratory support, and reduction in the cost of hospitalization and length of stay in the hospital [10, 18, 19]. Developmental care interventions also promote the bonding of the neonates with their parents, improve parental confidence in the provision of care following discharge, and reduce the risks of maternal stress and depression [10] that may result from separation and prolonged hospital stay of the preterm neonate during management for jaundice.
Researchers have emphasized the importance of diagnosing neonatal jaundice promptly to prevent its associated short and long-term sequelae [3]. Visual inspection alone is an unreliable tool for diagnosing jaundice [3]. Consequent to reliance on visual inspection alone, a significant proportion of severe hyperbilirubinemia have been misclassified, and others unnoticed by healthcare providers and or parents [3]. Although blood sample investigations have been confirmed reliable in diagnosing a wide range of abnormalities in pre-term neonates [2], the use of transcutaneous devices has also been reported to facilitate early recognition of neonatal jaundice [20]. Similarly, transcutaneous bilirubin measurement may offer a non-invasive, immediate approach to screening for hyperbilirubinemia among preterm neonates [21]. Preterm neonates, therefore, do not need to be subjected to frequent needle pricks due to the need to carry out investigations regularly.
The need to perform invasive procedures for diagnosis and prompt treatment has made hospitalized neonates the most frequent subjects of painful heel lancing, in the first week/month of their lives [12]. These authors observed that frequent exposure to painful procedures is not only associated with poor pain perception, threshold, and tolerance among such neonates, but they are also at a higher risk for neurobehavioural adverse effects [12]. This can also be associated with worsening clinical status. Accordingly, it is essential to effectively manage and prevent pain among preterm neonates to promote their physical comfort and stabilize their physiological parameters [12]. Pain experience can be alleviated by olfactory and gustatory stimuli from the infant’s mother’s breast milk [22]. The transcutaneous bilirubin measurement can also be explored for assessment during management, to minimize the need for frequent heel prick [3].
Although pain management during heel lancing for bilirubin level assessment among pre-term neonates undergoing phototherapy can be achieved using pharmacological and non-pharmacological approaches, the non-pharmacological approach is preferred due to the side effects of medications [23]. Some of the non-pharmacological approaches that are used for pain management among preterm neonates include oral sucrose, gentle human touch, massage, breastfeeding, white noise and the use of pacifier or non-nutritive sucking [23]. In another randomized control trial that assessed the use of breastmilk for pain relief during newborn screening procedures, researchers concluded that gentle human touch, in combination with the taste and odor of breastmilk, provided relief for neonates during the heel lancing for the screening [24].
Exclusive breastfeeding has been identified as a risk factor for neonatal jaundice among infants with difficulty feeding, emphasizing the need for careful monitoring and support for breastfeeding mothers [25]. Exclusive breastfeeding offers some protection against infants without feeding difficulties [25]. However, breastfed newborns have still been observed to be jaundiced after about one month of life [2]. To offer effective prevention from neonatal jaundice, early and adequate breastfeeding would need to be introduced to the infant [26]. Reports from recent findings have associated the increased levels of bilirubin in breastfed infants with failure to establish breastfeeding [27]. Therefore, improving breastfeeding support and education will likely reduce neonatal jaundice and associated hospital readmissions [28, 29]. Hence, nurses need to provide comprehensive support and education to mothers to ensure proper breastfeeding and to effectively manage neonatal jaundice [30].
Parental participation in the care and feeding of neonates prevents undue separation of the neonates from their parents and the associated feeling of lack of control [9, 14]. Parental participation in care ultimately culminates in effective bonding and improved mental health for the mother [14]. The other benefits of a positive environment include reduced stress for the neonate, optimized neurobehavioural development, and reduced length of stay during hospitalization [14]. In a retrospective study of the effect of continuous and intermittent phototherapy among neonates with hemolytic jaundice, there was no significant difference in the efficiency of phototherapy in the continuous and intermittent groups [5]. Conversely, they recorded a significantly higher occurrence of adverse effects among the continuous phototherapy group than the intermittent phototherapy group [5].
Intermittent phototherapy has been documented to be tolerable and effective among neonates with jaundice; however, there is a lack of evidence to suggest what frequency and length of interruption would affect the effectiveness of the management [9]. Based on the reports from previous studies, the author recommends exploring the effectiveness of intermittent phototherapy to allow more time for cuddles and parental contact with the newborn, as recommended in previous studies [5].
Phototherapy is a major line of treatment for neonatal jaundice because it reduces serum bilirubin levels through photoisomerization, structural isomerization, and photo-oxidation [30]. Phototherapy is considered a safe and well-tolerated therapy for neonatal jaundice [30–32]. It was similarly posited in the prospective observational study that phototherapy helps protect the brain from the effect of unconjugated bilirubin fraction [8]. Neonates with lower gestational age and birthweight require long-term phototherapy, which has consequent adverse effects among these small and vulnerable infants [13]. Parents are often encouraged to participate in nappy changes and feeding of their neonates during phototherapy. Intermittent phototherapy has been documented to be tolerable and effective among neonates with jaundice, but there is a lack of evidence to suggest what frequency and length of interruption would affect the effectiveness of the management [2]. The NICE guideline for managing neonatal jaundice provides information on the importance of continued parental interaction during phototherapy. However, the frequency and length of interruption that would affect the effectiveness of phototherapy were not included [2]. Based on the reports from previous studies, the author recommends exploring the effectiveness of intermittent phototherapy to allow more time for cuddles and parental contact with the newborn [5].
There have been anecdotal reports that the involvement of parents in the management of hospitalized neonates with jaundice has been streamlined to feeding. However, the provision of information on the signs of jaundice during the hospitalization period and involving parents in the management of hospitalized neonates with jaundice goes beyond feeding [2]. Parental support in neonatal care, with information for parents usually including the anticipated period of treatment and reassurance that nappy changes and feeding can usually continue during the period of phototherapy, were also included in the NICE guideline for the management of neonatal jaundice [9]. Maternal knowledge and early care-seeking behavior have been identified as fundamental components of the effective management of neonatal jaundice, highlighting the need for comprehensive education and support for caregivers [24].
The intensity of the phototherapy was not assessed, and therefore, the management length could not be estimated. This contrasts with the guidelines provided by NICE, where the duration of management of jaundice could be estimated based on the type of phototherapy being used, therefore assisting the healthcare providers in providing information to parents on the anticipated duration of therapy [2].
Implication to practice
The benefits of early maternal-infant interactions are overwhelming; thus, there is a need for collaboration to minimize parent-infant separation that is associated with the management of neonates with jaundice [17]. This can be partly achieved by providing continuing education for nurses on family-centered developmental care strategies to facilitate improved outcomes for neonates with jaundice [17]. Moreover, intermittent phototherapy rather than continuous phototherapy should be explored to prevent unnecessary separation and promote bonding between pre-term neonates undergoing phototherapy and their parents. Non-pharmacological measures for pain management, especially during heel lancing for preterm neonates undergoing heel lancing, should be adopted to minimize the neurological consequences associated with the procedure. The overall care and experience of neonatal jaundice can also be improved by welcoming new advancements in pain relief strategies and non-invasive methods of assessment of bilirubin levels.
There is a need to provide information on the signs of jaundice during the antenatal period, and involving parents in the management of hospitalized neonates with jaundice should be supported beyond feeding. There is also a need to identify evidence-based strategies for assessing the intensity of phototherapy to estimate the length of management and provide information to parents on the anticipated duration of therapy. Correspondingly, the authors recommend exploring the effectiveness of intermittent phototherapy and the frequency and length of interruption that would affect the management of neonatal jaundice. Educational resources should be made available to parents during admission. The materials should provide information on “how,” and “to what extent” parents can participate in the care so that nursing and medical care of the neonate with jaundice are not jeopardized [17]. Also, exclusive breastfeeding support and guidance should be provided, acknowledging the individual circumstances and needs of both the mother and neonate [23].
Conclusion
In conclusion, the management of neonatal jaundice requires a multidisciplinary approach, involving developmental care and nursing care. Educating caregivers and healthcare professionals, along with implementing evidence-based management strategies, is essential for improving outcomes and reducing the burden of neonatal jaundice.
Study limitations
The report was limited to a preterm neonate with no other significant medical or surgical condition within the hospital setting. Developmental care focuses on creating a supportive environment tailored to a newborn's sensory, physical, and emotional needs to promote healthy growth, comfort, and bonding with parents. While these interventions are especially emphasized for preterm infants due to the unique challenges of early birth, full-term infants can also benefit from techniques like gentle handling, minimization of stress, and enhanced parental involvement, particularly when they are medically fragile or undergoing intensive treatment.
Ethical Considerations
Compliance with ethical guidelines
The management of Baby M was guided by the ethical principles of the hospital, primarily focusing on the best interests of the neonate, informed consent, parental involvement and adherence to established clinical guidelines. The healthcare team ensured that Baby M's treatment adhered to the NICE guidelines, which are based on evidence-based best practices. These guidelines were followed to provide the most appropriate and effective treatment for neonatal jaundice, minimizing risks while optimizing outcomes.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization: Esther Aduramo; Supervision: Deborah Esan; Methodology: Oluwadamilare Akingbade, Deborah Esan, Emmanuel Adesuyi, and Esther Aduramo; Writing the original draft: Esther Aduramo; Review and editing: Esther Aduramo, Deborah Esan, Oluwadamilare Akingbade, Opeoluwa Olabode, Elizabeth Awoniyi, Blessed Oyama.
Conflicts of interest
The authors declared no conflict of interest.
References
- Ministry of Health. Integrated plan for detection and management of neonatal jaundice [Internet]. 2018. [Updated 2025 Jan 2]. Available from: [Link]
- Noureldein M, Hill C, Ali A, Gbenga-Ojo S, Adewuyi M, Fradd V, Surana P. Neonatal jaundice in infants born at 37 weeks: is NICE treating too many? Arch Dis Child Fetal Neonatal Ed, 2023;108(5):547-8. [DOI: 10.1136/archdischild-2022-325075] [PMID]
- Westenberg LEH, van der Geest BAM, Lingsma HF, Nieboer D, Groen H, Vis JY, et al. Better assessment of neonatal jaundice at home (BEAT Jaundice @home): Protocol for a prospective, multicentre diagnostic study. BMJ Open. 2022; 12(11):e061897. [DOI:10.1136/bmjopen-2022-061897] [PMID]
- Hansen TWR, Wong RJ, Stevenson DK. Molecular physiology and pathophysiology of bilirubin handling by the blood, liver, intestine, and brain in the newborn. Physiol Rev. 2020; 100(3):1291-346. [DOI:10.1152/physrev.00004.2019] [PMID]
- Zhou S, Wu X, Ma A, Zhang M, Liu Y. Analysis of therapeutic effect of intermittent and continuous phototherapy on neonatal hemolytic jaundice. Exp Ther Med. 2019; 4007-12. [DOI:10.3892/etm.2019.7432]
- Kinshella MW, Salimu S, Chiwaya B, Chikoti F, Chirambo L, Mwaungulu E, et al. Challenges and recommendations to improve implementation of phototherapy among neonates in Malawian hospitals. BMC Pediatr. 2022; 22(1):367.[DOI:10.1186/s12887-022-03430-y] [PMID]
- Asefa GG, Gebrewahid TG, Nuguse H, Gebremichael MW, Birhane M, Zereabruk K, et al. Determinants of neonatal jaundice among neonates admitted to neonatal intensive care unit in public general hospitals of Central Zone, Tigray, Northern Ethiopia, 2019: A case-control study. Biomed Res Int. 2020; 2020:4743974. [DOI:10.1155/2020/4743974] [PMID]
- Boskabadi H, Molaei MK, Zakerihamidi M. Effect of phototherapy on pro-oxidant/oxidant balance in newborns with jaundice. Biomed Res Ther. 2018; 5(7):2432-9. [Link]
- National Institute for Health and Clinical Excellence (NICE). Jaundice in newborn babies under 28 days clinical guideline. London: NICE: 2023. [Link]
- Byers JF. Components of developmental care and the evidence for their use in NICU. MCN Am J Matern Child Nurs. 2003; 28(3):174-80; quiz 181-2. [DOI:10.1097/00005721-200305000-00007] [PMID]
- Ohuma EO, Moller AB, Bradley E, Chakwera S, Hussain-Alkhateeb L, Lewin A, et al. National, regional, and global estimates of preterm birth in 2020, with trends from 2010: A systematic analysis. Lancet. 2023; 402(10409):1261-71. [DOI:10.1016/S0140-6736(23)00878-4] [PMID]
- Sezer Efe Y, Erdem E, Caner N, Güneş T. The effect of gentle human touch on pain, comfort and physiological parameters in preterm infants during heel lancing. Complement Ther Clin Pract. 2022; 48:101622. [DOI:10.1016/j.ctcp.2022.101622] [PMID]
- Dai J, Xu Y, Yin Q, Chen J, Shi H, Li Y. Effect of systematic holistic nursing combined with the MDT teaching method in the nursing of neonatal jaundice and its impact on the recovery of the newborns' physiological function. J Healthc Eng. 2021; 2021:2013233. [DOI:10.1155/2021/2013233] [PMID]
- van der Geest BAM, Theeuwen IM, Reiss IKM, Steegers EAP, Been JV. Assessing knowledge and skills of maternity care professionals regarding neonatal hyperbilirubinaemia: A nationwide survey. BMC Pregnancy Childbirth. 2021; 21(1):63. [DOI:10.1186/s12884-020-03463-0] [PMID]
- Jalali S, Bagherian B, Mehdipour-Rabori R, Forouzi MA, Roy C, Jamali Z, et al. Assessing virtual education on nurses’ perception and knowledge of developmental care of preterm infants: A quasi-experimental study. BMC Nurs. 2022; 21(1):161. [DOI:10.1186/s12912-022-00939-6] [PMID]
- Symington A, Pinelli J. Developmental care for promoting development and preventing morbidity in preterm infants. Cochrane Database Syst Rev. 2006; 2006(2):CD001814. [DOI:10.1002/14651858.CD001814.pub2] [PMID]
- Soni R, Tscherning C. Family-centred and developmental care on the neonatal unit. Paediatr Child Health. 2021; 31(1):18-23. [DOI:10.1016/j.paed.2020.10.003]
- Cardin AD, Rens LA, Stewart S, Danner-Bowman K, McCarley R, Kopsas R. Neuroprotective Core Measures 1-7: A developmental care journey: Transformations in NICU Design and Caregiving Attitudes. Newborn Infant Nurs Rev. 2015; 15(3):132-41. [DOI:10.1053/j.nainr.2015.06.007]
- Griffiths N, Spence K, Loughran-Fowlds A, Westrup B. Individualised developmental care for babies and parents in the NICU: Evidence-based best practice guideline recommendations. Early Hum Dev. 2019; 139:104840. [DOI:10.1016/j.earlhumdev.2019.104840] [PMID]
- Hulzebos CV, Vitek L, Coda Zabetta CD, Dvořák A, Schenk P, van der Hagen EAE, et al. Screening methods for neonatal hyperbilirubinemia: Benefits, limitations, requirements, and novel developments. Pediatr Res. 2021; 90(2):272-6. [DOI:10.1038/s41390-021-01543-1] [PMID]
- Jegathesan T, Campbell DM, Ray JG, Shah V, Berger H, Hayeems RZ, et al. Transcutaneous versus total serum bilirubin measurements in preterm infants. Neonatology. 2021; 118(4):443-53. [DOI:10.1159/000516648] [PMID]
- Lin CH, Liaw JJ, Chen YT, Yin T, Yang L, Lan HY. Efficacy of breast milk olfactory and gustatory interventions on neonates’ biobehavioral responses to pain during heel prick procedures. Int J Environ Res Public Health. 2022; 19(3):1240. [DOI:10.3390/ijerph19031240] [PMID]
- Seagraves K, Brulte A, Mcneely K, Pritham U. Supporting breastfeeding to reduce newborn readmissions for hyperbilirubinemia. Nurs Womens Health. 2013; 17(6):498-507.[DOI:10.1111/1751-486X.12078] [PMID]
- Salia SM, Afaya A, Wuni A, Ayanore MA, Salia E, Kporvi DD, et al. Knowledge, attitudes and practices regarding neonatal jaundice among caregivers in a tertiary health facility in Ghana. Plos One. 2021; 16(6):e0251846. [DOI:10.1371/journal.pone.0251846] [PMID]
- Scrafford CG, Mullany LC, Katz J, Khatry SK, LeClerq SC, Darmstadt GL, et al. Incidence of and risk factors for neonatal jaundice among newborns in southern Nepal. Trop Med Int Health. 2013; 18(11):1317-28. [DOI:10.1111/tmi.12189] [PMID]
- Siroosbakht S, Aminian AR, Rezakhaniha B. Risk factors of early breastfeeding jaundice: How can gynecologists and nurses be effective in reducing it? J Compr Pediatr. 2020; 11(3).
- Kankaew S, Daramas T, Patoomwan A. View of frequency of breastfeeding, bilirubin levels, and re-admission for jaundice in neonates. Bangk Med J. 2019; 15(2):180-5. [DOI:10.31524/bkkmedj.2019.09.010]
- Jang GJ. Influence of a breastfeeding coaching program on the breastfeeding rates and neonatal morbidity in late preterm infants. Child Health Nurs Res. 2020; 26(3):376-84. [DOI:10.4094/chnr.2020.26.3.376] [PMID]
- Jang GJ, Ko S. Effects of a breastfeeding coaching program on growth and neonatal jaundice in late preterm infants in South Korea. Child Health Nurs Res. 2021; 27(4):377-84. [DOI:10.4094/chnr.2021.27.4.377] [PMID]
- Gothwal S, Singh N, Sitaraman S, Choudhary R, Meena KK, Bairwa GS, et al. Efficacy of transcutaneous bilirubinometry as compared to serum bilirubin in preterm newborn during phototherapy. Eur J Pediatr. 2021; 180(8):2629-36. [DOI:10.1007/s00431-021-04148-2] [PMID]
- Bulut Ö, Dürüyen S. Impacts of phototherapy on DNA damage and total oxidant/ antioxidant status in jaundiced newborns. Turk J Pediatr. 2019; 61(5):697-703. [DOI:10.24953/turkjped.2019.05.008] [PMID]
- Cai A, Qi S, Su Z, Shen H, Yang Y, Cai W, et al. A pilot metabolic profiling study of patients with neonatal jaundice and response to phototherapy. Clin Transl Sci. 2016; 9(4):216-20. [DOI:10.1111/cts.12401] [PMID]
Type of Study: Case Report and Review of Literature |
Subject:
Pediatrics
Received: 2024/02/2 | Accepted: 2024/07/12 | Published: 2024/10/1
Received: 2024/02/2 | Accepted: 2024/07/12 | Published: 2024/10/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |