Volume 13, Issue 3 (7-2025)
J. Pediatr. Rev 2025, 13(3): 169-182 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Zakariaee S S, Naderi N, Kazemi-Arpanahi H. Diagnostic Reference Levels for Pediatric CT Examinations Based on Patient Size: A Meta-analysis. J. Pediatr. Rev 2025; 13 (3) :169-182
URL: http://jpr.mazums.ac.ir/article-1-684-en.html
URL: http://jpr.mazums.ac.ir/article-1-684-en.html
1- Department of Medical Physics, Faculty of Paramedical Sciences, Ilam University of Medical Sciences, Ilam, Iran. , salman_zakariaee@yahoo.com
2- Department of Midwifery, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran.
3- Department of Health Information Technology, Faculty of Paramedical Sciences, Abadan University of Medical Sciences, Abadan, Iran.
2- Department of Midwifery, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam, Iran.
3- Department of Health Information Technology, Faculty of Paramedical Sciences, Abadan University of Medical Sciences, Abadan, Iran.
Full-Text [PDF 3143 kb]
(814 Downloads)
| Abstract (HTML) (1044 Views)
Full-Text: (465 Views)
Introduction
Computed tomography (CT) is one of the most common diagnostic methods used in clinics. Studies have estimated that more than 62 million CTs are performed annually in the U.S., and at least 6.45% of them are related to pediatric imaging [1, 2]. A dramatic increase in pediatric CT examinations was reported over the past several decades [3].
Radiation protection holds particular importance for imaging examinations that involve high radiation doses, such as CT scans [4, 5]. Children exhibit higher radiosensitivity than adults due to the increased radiosensitivity of their developing organs and tissues. After radiation exposure during the CT examinations, there is a longer life expectancy for children than adults, leading to higher lifetime risks of developing radiation-induced malignancies [6, 7]. Consequently, radiation-induced diseases may occur with several times greater risk for children than for adults in an identical CT examination. For pediatric CT imaging, it is essential to keep the radiation dose as low as reasonably practicable without compromising the quality of the diagnostic images [8-11]. The International Commission on Radiological Protection (ICRP) introduced diagnostic reference levels (DRLs) criteria in 1996 to meet this need [3, 12-14]. Based on this recommended index, it could be determined whether the scanning protocols of CT examinations have been adequately optimized [15]. Volumetric CT dose index (CTDIvol), dose length product (DLP), and size-specific dose estimates (SSDE) are the dosimetric quantities recommended for DRL establishment [11, 16].
The importance of establishing DRLs for pediatric imaging was emphasized in European guidelines on DRLs for pediatrics (radiation protection No. 185), and the first establishment of DRLs for pediatric CT was reported in 2000 [12, 15]. Since then, DRLs for pediatric CT examinations have been announced by different countries and associations. The reported values were considerably different based on the study location, even for the same CT scanner. These differences may be the result of several factors, including the type of CT scanner and its characteristics, CT examination protocol, patient’s body size, etc. [1, 17, 18].
The major problem in comparing the established DRLs is the wide range of patient sizes, even within the same age group, which results in a considerable variation in radiation doses announced for institutions and countries [4, 19]. ICRP 135 and European guidelines on DRLs for pediatric imaging recommended the establishment of age‑ and size‑specific DRLs to deal with this problem [20]. The results of pioneering studies have shown that patient sizes do not correlate with age bands, and patient size has been suggested as the more preferred index to design scanning protocols and radiation dose management in medical imaging centers [3, 19]. The size and material compositions of the scanning area are the main factors to determine absorbed dose magnitudes during a radiological examination. Hence, it is recommended in international guidelines that patient size must be considered the primary criterion for establishing the DRLs. During the transition period, age may serve as an additional index [21].
There are a few limited review studies on the establishment of DRLs for pediatric CT examinations, which mainly describe age-specific DRLs [20, 22-28]. To our knowledge, a dedicated systematic review and meta-analysis study has not yet been performed for the assessment of size‑specific DRLs of pediatric CT examinations. The objective of the current study was to explore the literature on existing size‑specific DRLs and determine radiation dose metrics (CTDIvol, DLP, and SSDE) for five patient sizes in pediatric CT examinations.
Methods
Protocol of the systematic review and meta-analysis
The systematic review and meta-analysis were conducted according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) checklist [29].
Information sources and search strategies
A systematic literature search was carried out using Web of Science, PubMed, Embase, Scopus databases, and the Google Scholar search engine. The following MeSH and non-MeSH terms were used for literature searching: (“diagnostic reference level”* OR “DRL”*) AND (CT OR “computed tomography” OR “x-ray CT scan” OR “x-ray CAT scan” OR “CT scan” OR “CAT scan”).
The systematic literature search was conducted without the beginning date restriction until May 2024. Case reports, editorials, commentaries, and opinions were not included in the meta-analysis.
Eligibility criteria
Studies were pre-included if they reported the establishment of DRLs for pediatric CT examinations based on patient size. A child was defined as a human being from birth to the age of 18 [30]. Hence, as the inclusion criterion, this limit was applied to the age of the study participants, and publications investigating only DRLs for pediatric CT examinations were included. The exclusion criteria were as follows: 1) Studies that reported DRL values for imaging modalities other than CT. 2) The age of participants for whom DRL values were reported exceeded the age limit defined for a child. 3) Studies that did not provide sufficient data to calculate the Mean±SD for radiation dose metrics. However, no limitation was applied to the studied part of the body, the size of participants, the publication language, and the sex of the study participants.
Study selection and data collection process
The first author of the selected reports, publication date, study location, sizes of the study participants, sample size, radiation dose metrics (CTDIvol, DLP, and SSDE) for five patient sizes in pediatric CT, DRLs, and other related information were extracted from the studies. For studies that reported radiation dose metrics as median and first quartile (Q1) to third quartile (Q3) range, the Mean±SD values were extracted using the Equations 1 and 2:
1. Mean=(Median+Q1+Q3)/3
2. SD=(Q3-Q1)/1.35
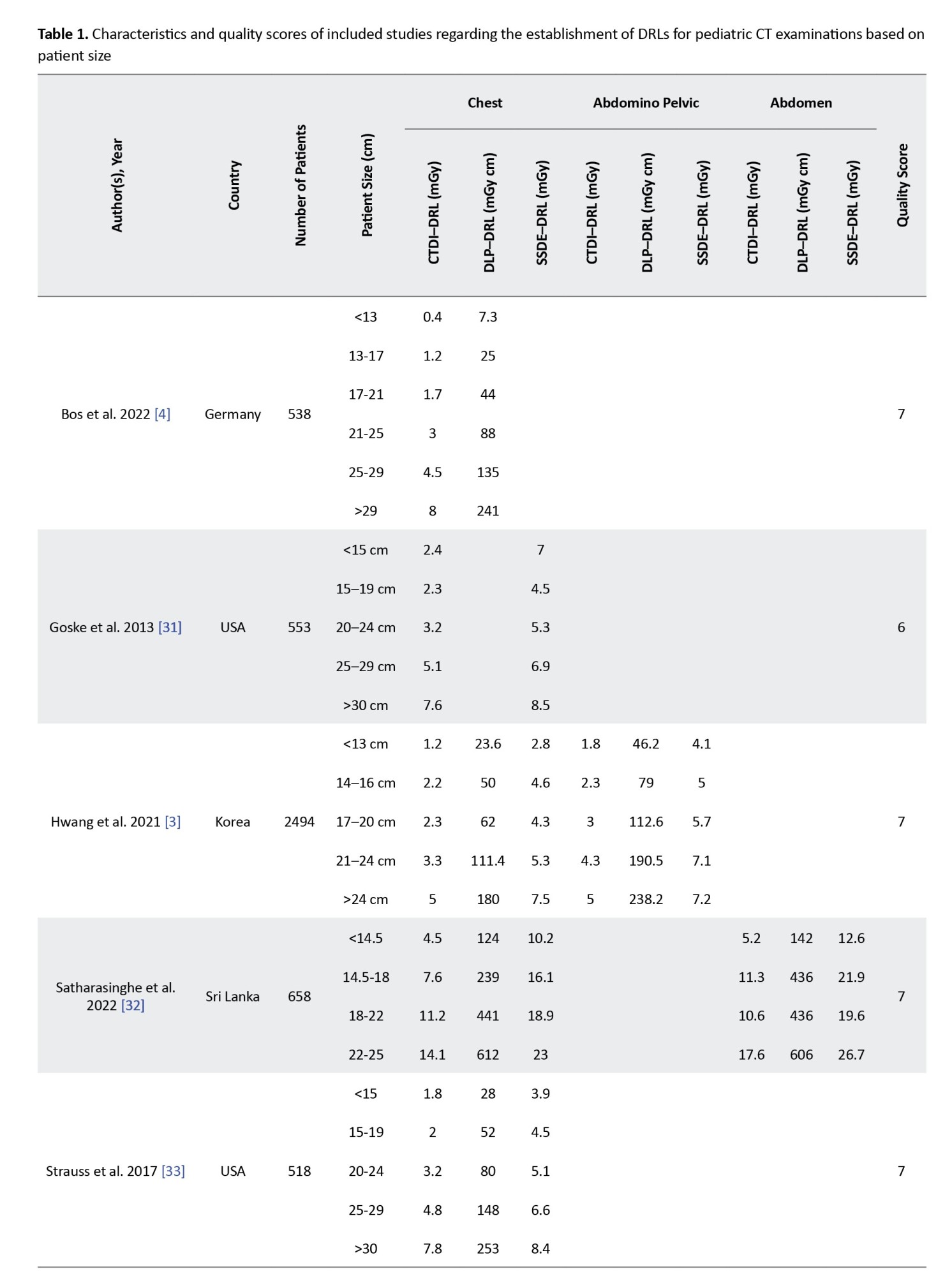
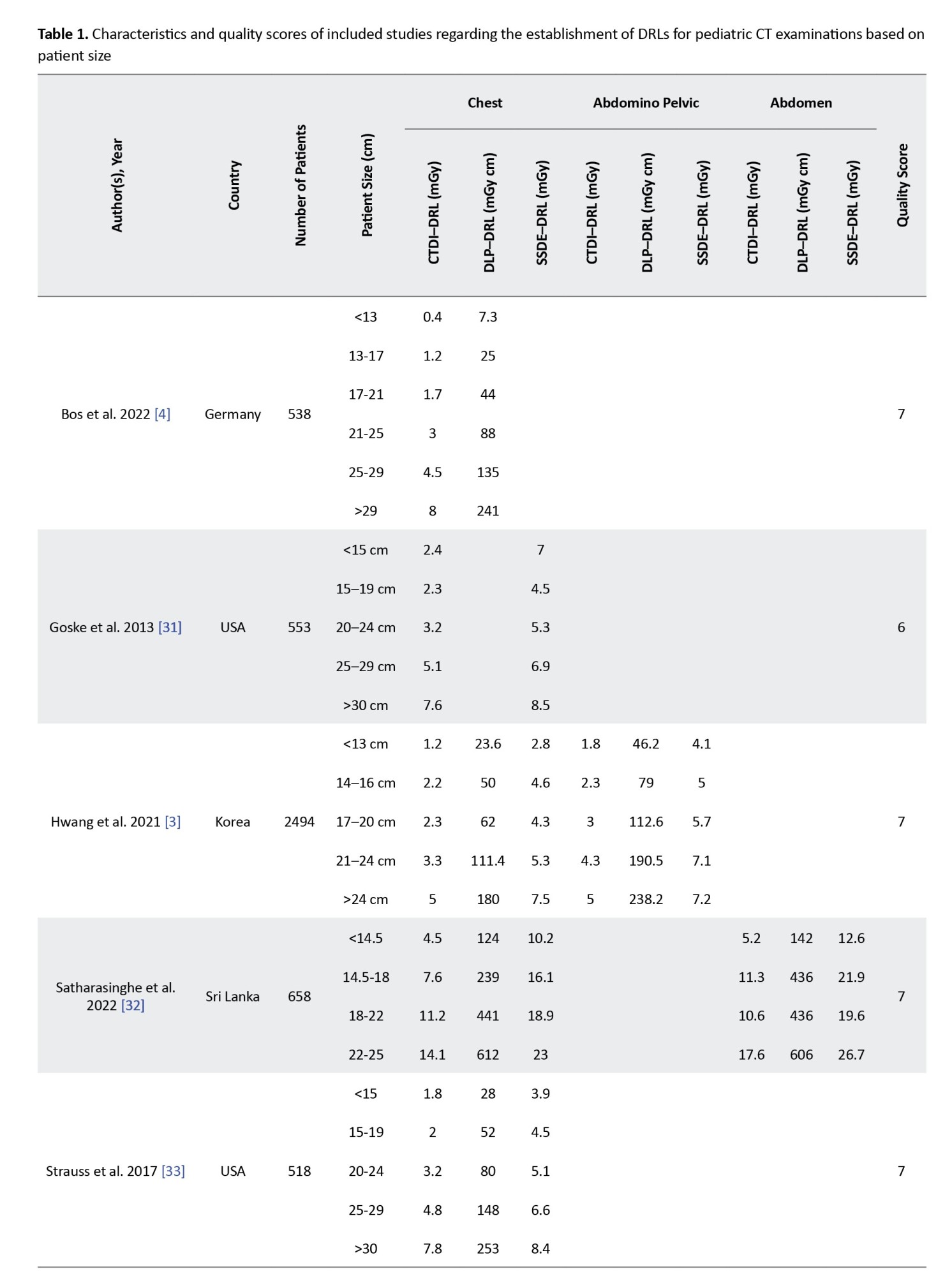
The main data extracted are presented in Table 1.
Quality assessment of the studies
The quality and risk of bias of the studies were evaluated using the Newcastle-Ottawa scale (NOS). The risk of bias for each study was assessed based on three aspects, including the selection of the exposed populations, comparability, and outcome measurements. The maximum score for a study is 7.
Summary measures and synthesis of results
STATA software, version 16.0, was used for data analysis. In this study, the Mean±SD of radiation dose metrics reported for each patient size group were used to determine the overall effect size. Cochran’s Q test and the inconsistency index (I2) test were used to evaluate heterogeneity between studies.
The possible sources of between-study heterogeneity were assessed through subgroup analysis, where the study location was evaluated as the moderator variable. Publication bias among studies was evaluated through visual inspection of the generated funnel plots. Publication bias refers to the condition where a study has a low probability of being published when its results are negative, non-significant, or have small effects.
Results
Study selection
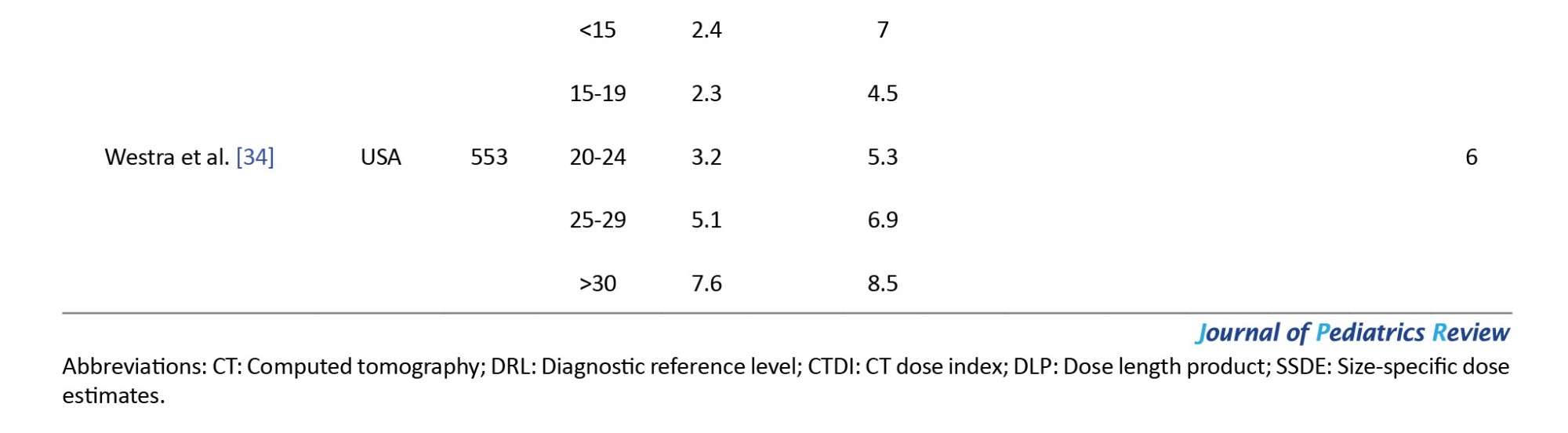
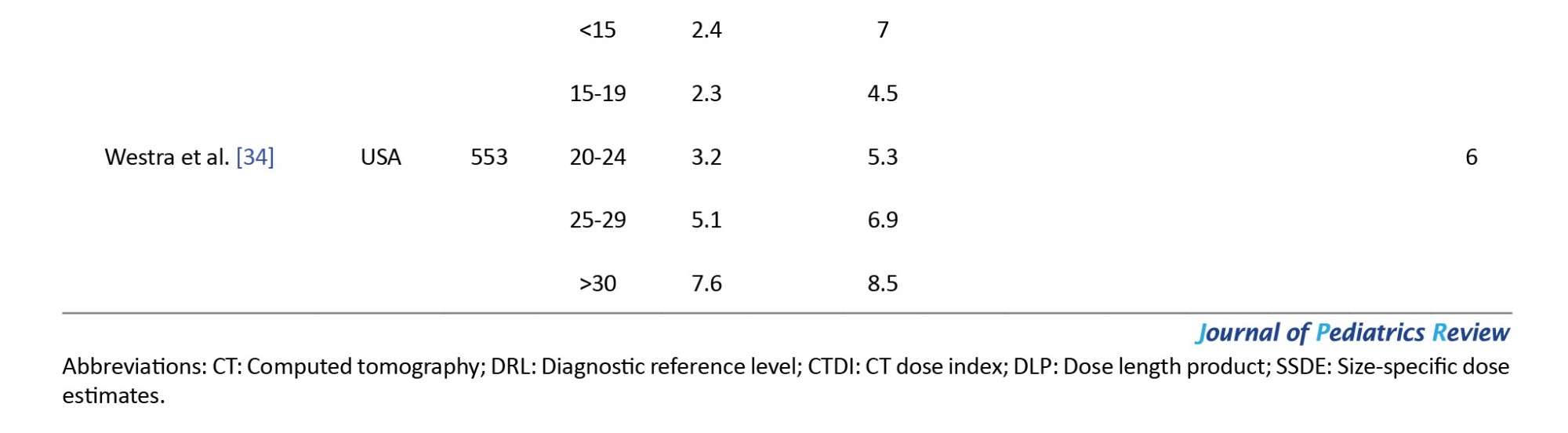
A total of 1,521 articles were identified through the initial search. Seven hundred sixty-four duplicate articles were removed, and 291 papers were screened based on their titles and abstracts. The full texts of 60 studies were evaluated after removing irrelevant studies. The reports that did not have sufficient data to calculate the Mean±SD for radiation dose metrics were excluded. Finally, six reports regarding the establishment of DRLs for pediatric CT examinations were included in the meta-analytical processes based on the inclusion criteria (Figure 1).
Characteristics and quality of the included studies
The characteristics of the included studies regarding the establishment of DRLs for pediatric CT examinations based on patient size are detailed in Table 1. The table presents the first author, publication date, study location, sizes of the study participants, DRLs, and the sample sizes of the studies reporting DRLs for pediatric patients undergoing chest, abdominopelvic, and abdomen CT examinations. The quality scores of the included articles are listed in the last column. All six included articles were rated as high quality (four articles had a score of 7, and two articles had a score of 6). Thus, the quality of the studies was not the source of heterogeneity among the studies. This study retrieved a total of 4761 patients undergoing pediatric CT examinations. Modern CT scanners are equipped with tube current modulation (TCM) that alters the x-ray tube current as a function of patient attenuation at a given region of interest. TCM yields significant reductions in patient doses while maintaining image noise. Therefore, the dose surveys for establishing DRLs in pediatric CT examinations are recommended to be performed in the patient grouping based on their effective diameters or water equivalent diameters [3]. The meta-analysis was performed for studies describing the establishment of DRLs for pediatric CT examinations based on the effective diameter (cm) or water equivalent diameter (cm) of the patients. For abdominopelvic and abdomen CT examinations, there were not enough studies to perform a meta-analysis test (n<3). Hence, the radiation dose metrics (CTDIvol, DLP, and SSDE) were only analyzed for pediatric chest CT. The extracted data for five groups of effective diameters, including <15 cm, 15–19 cm, 20–24 cm, 25–29 cm, and ≥30 cm, were entered into the analysis. Two articles written by Goske et al. [31] and Westra et al. [34] reported data from the same registry and had identical values. Therefore, only one of them was included in the analysis.
Risk of bias within the studies
For all radiation dose metrics (CTDIvol, DLP, and SSDE) in five groups of effective diameters, the significance value obtained from the χ2 test of heterogeneity was <0.001. Moreover, the I2 values for all studies ranged from 94.3% to 100%. Therefore, the random-effects model of the meta-analysis was used for the studies.
Synthesis of the results
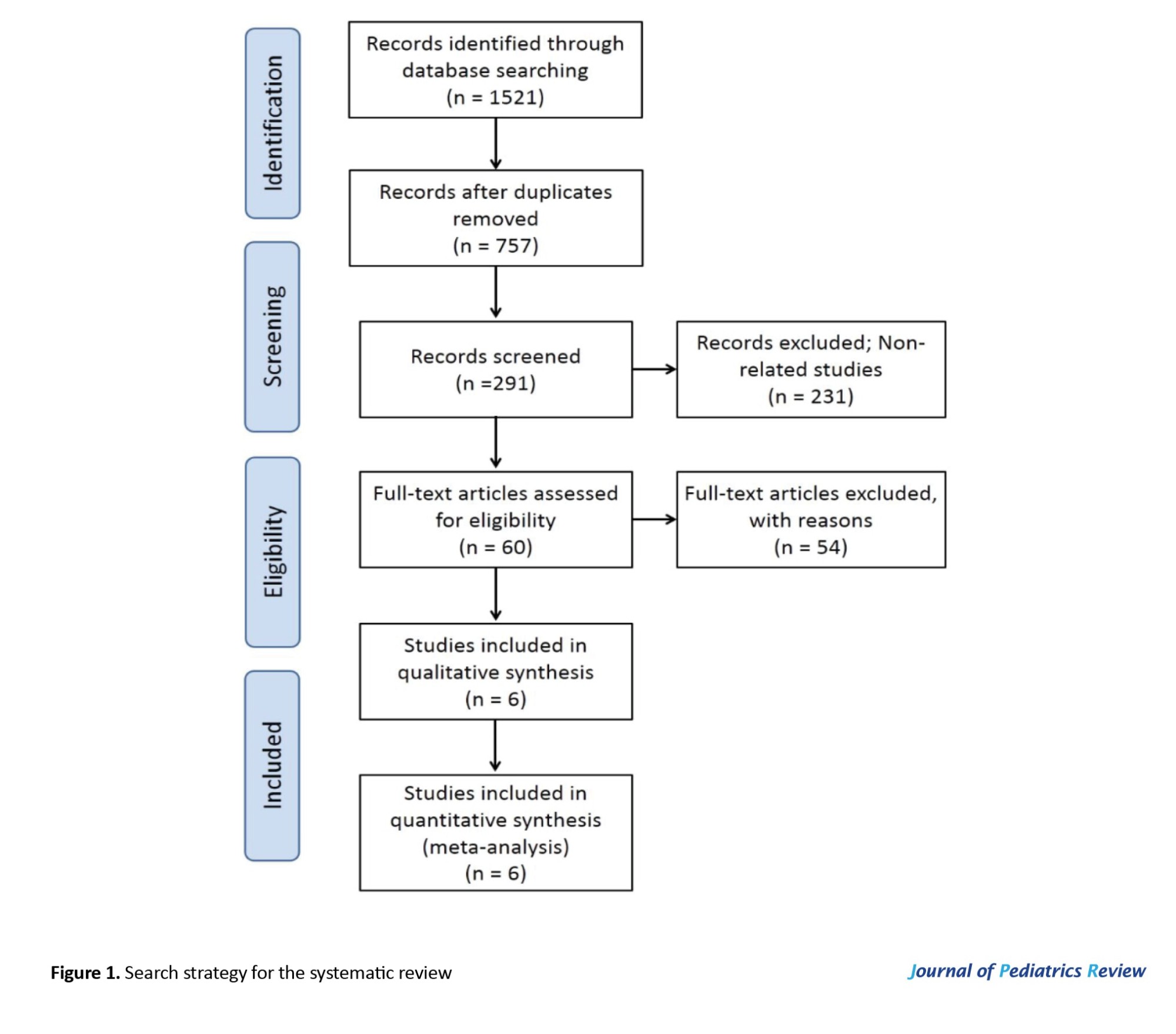
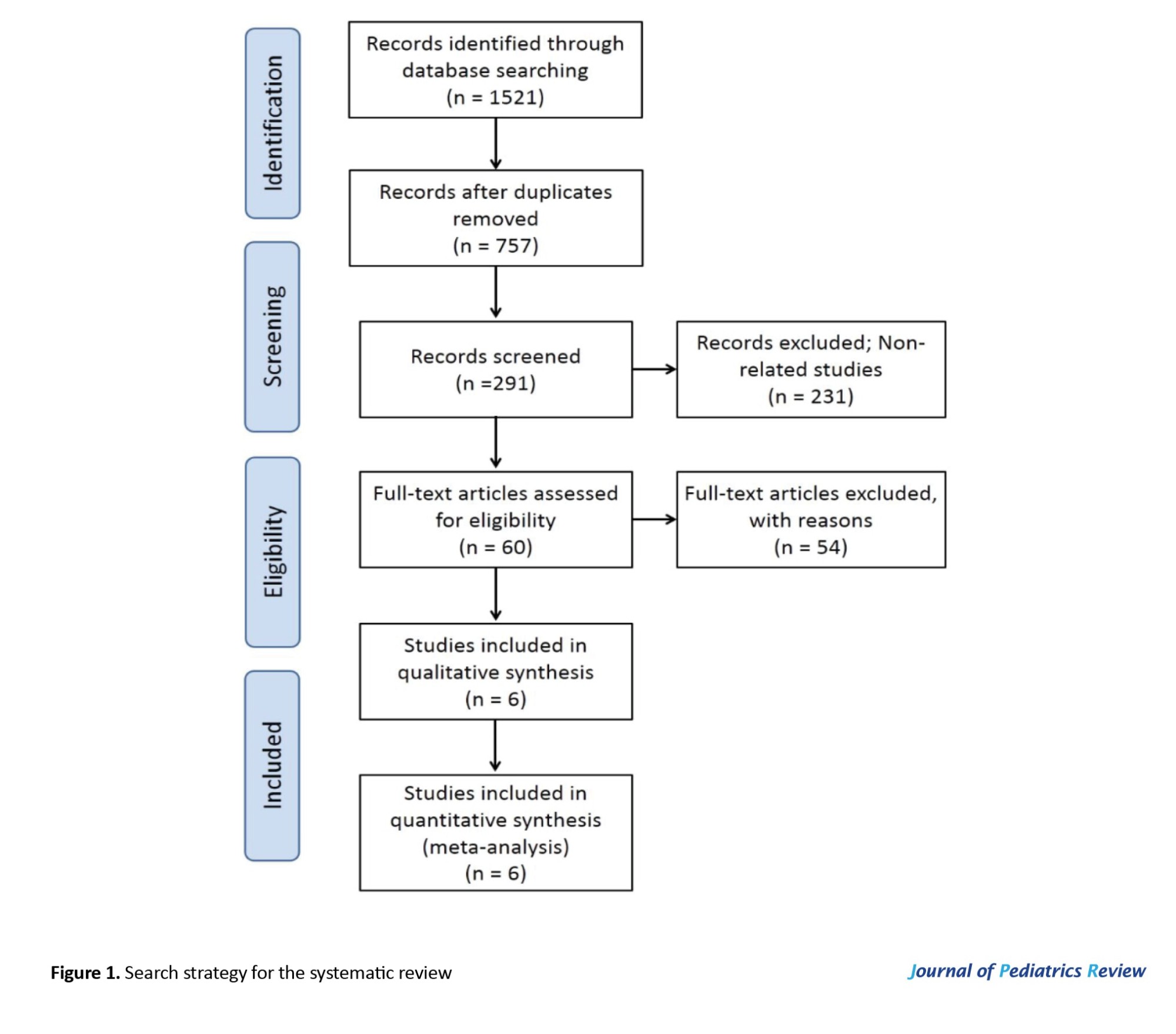
The forest plots for radiation dose metrics (CTDIvol, DLP, and SSDE) are presented in Figures 2, 3 and 4, respectively.
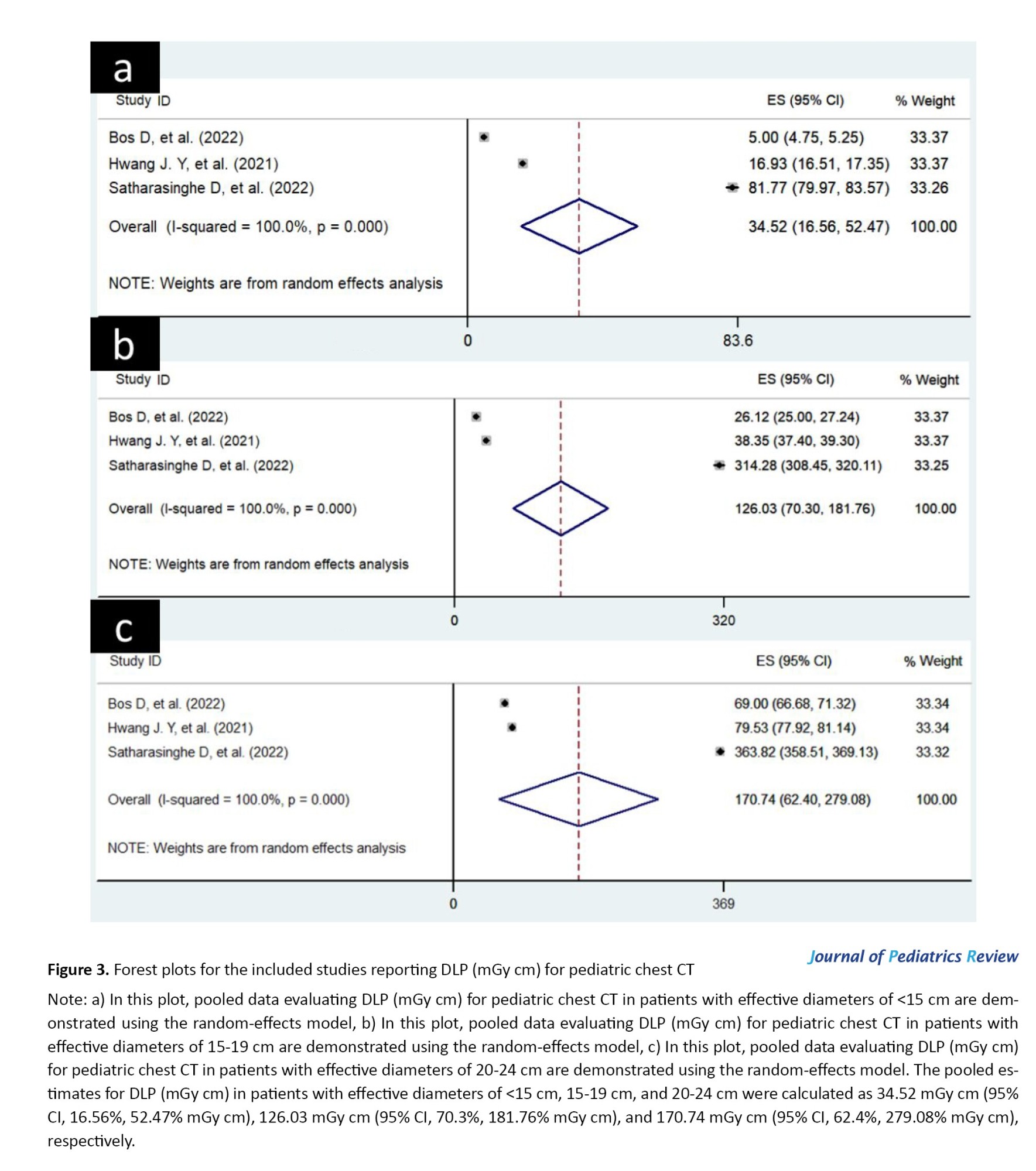
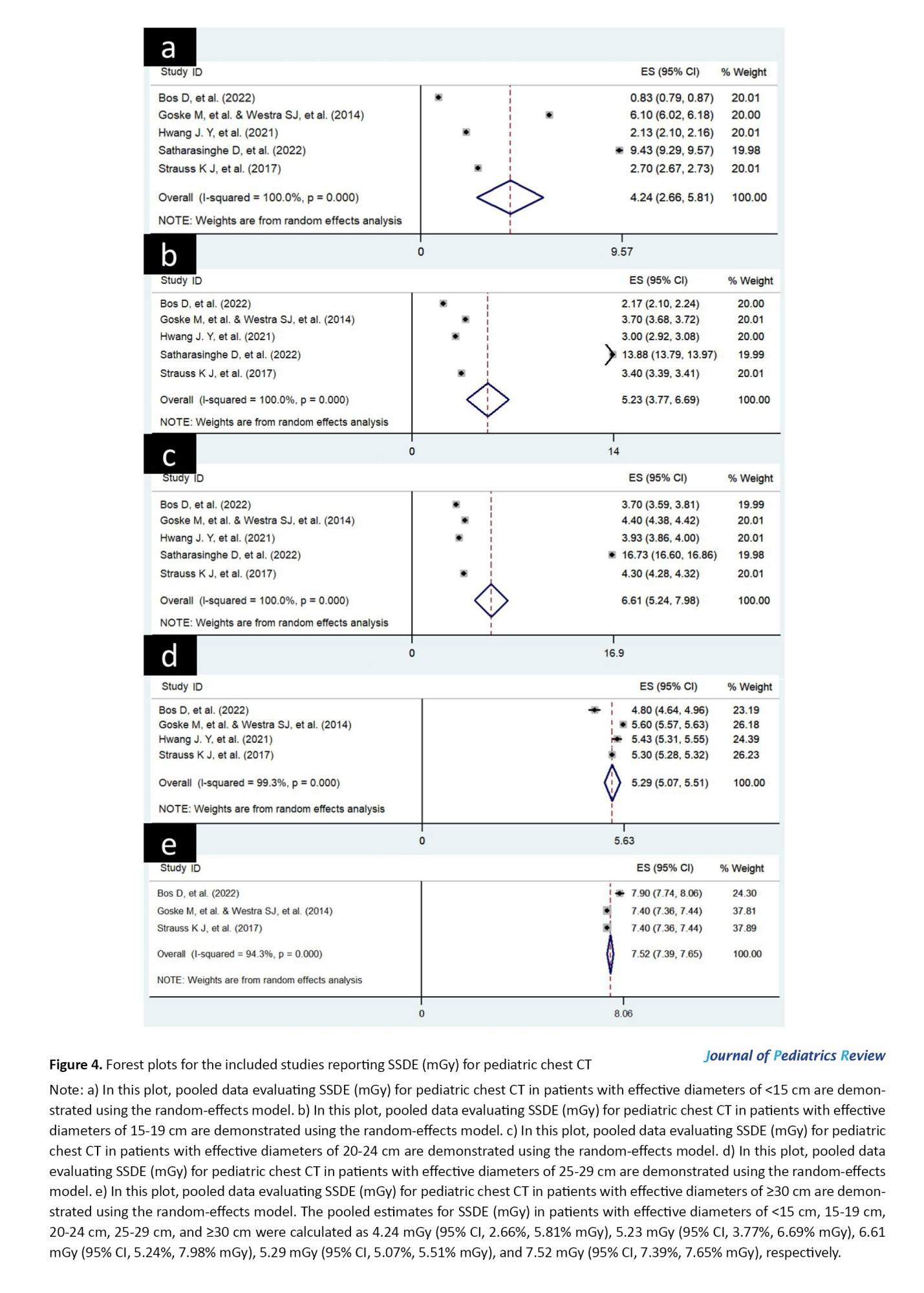
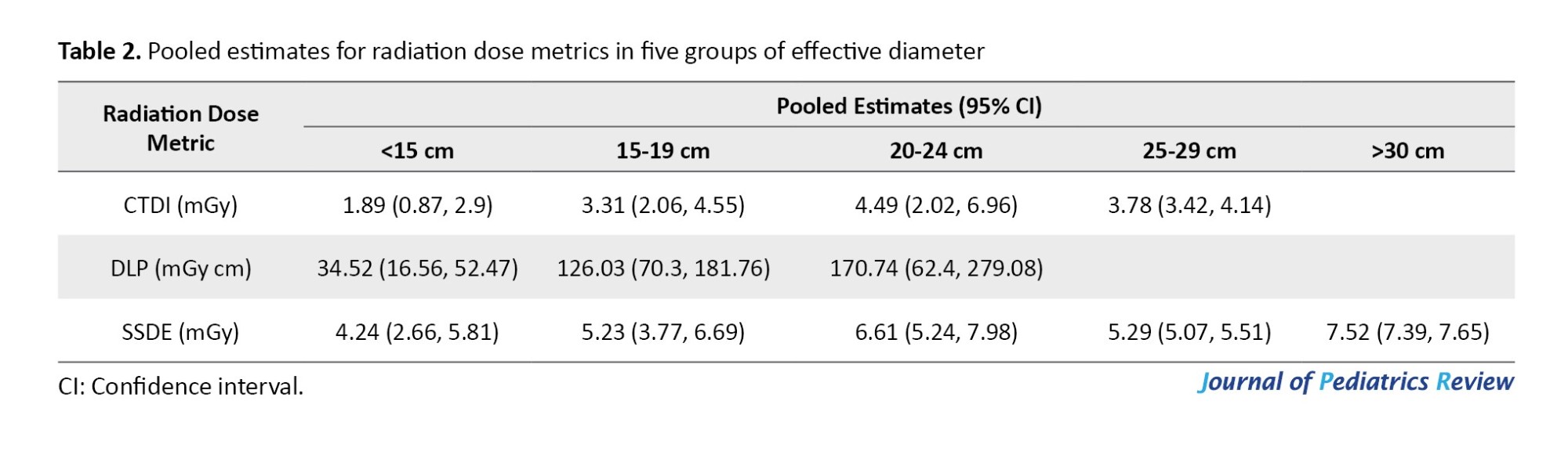
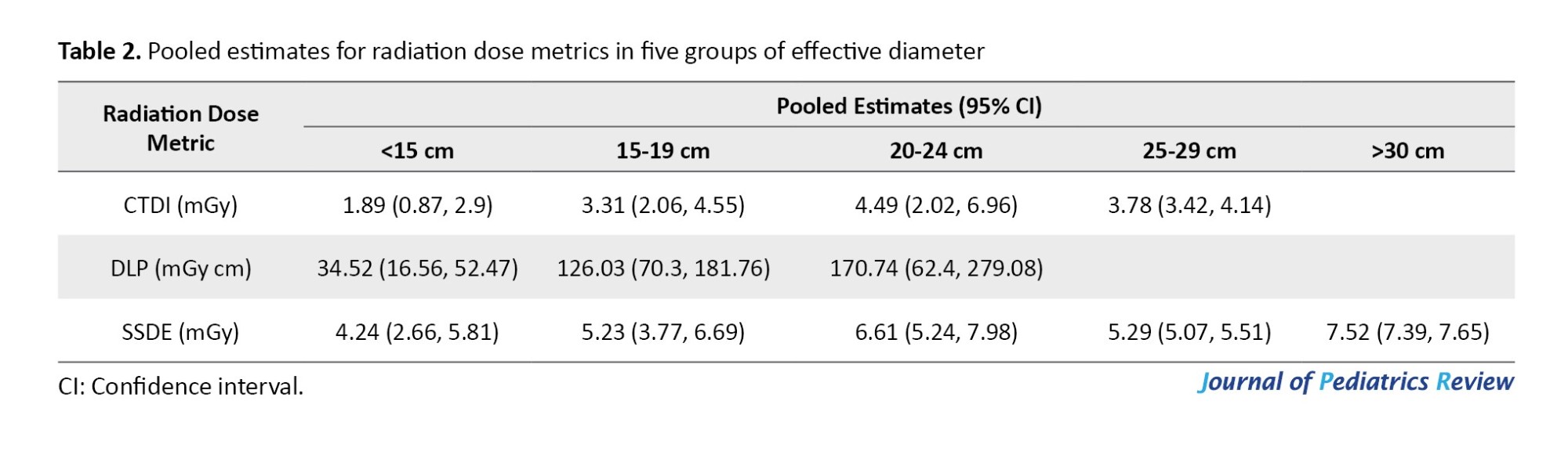
In these representations, the mean effect sizes (with 95% CI) of studies and the overall effect sizes (with 95% CI) for five groups of effective diameters are presented in separate subfigures. The pooled estimates for all radiation dose metrics in five groups of effective diameters are listed in Table 2.
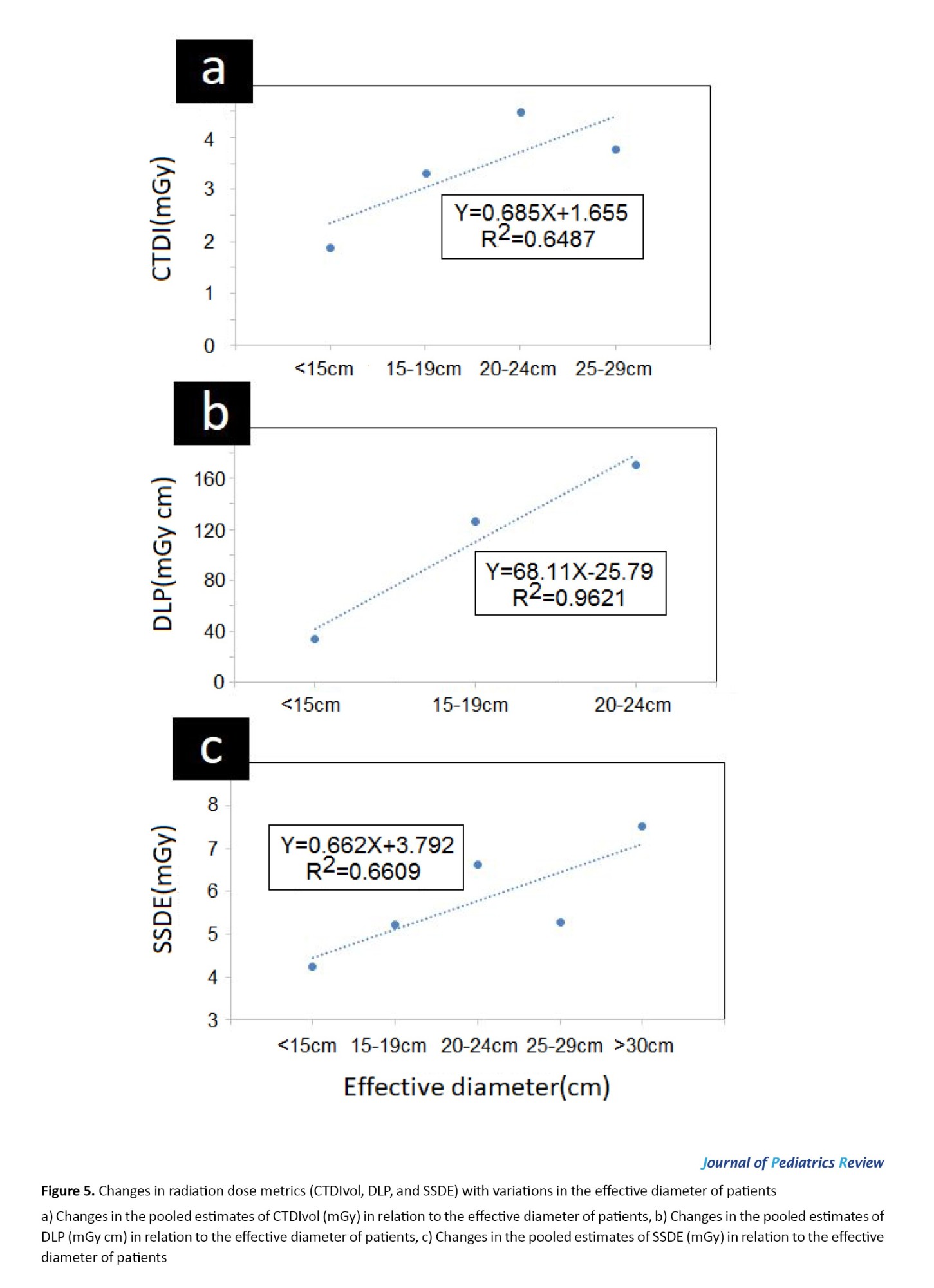
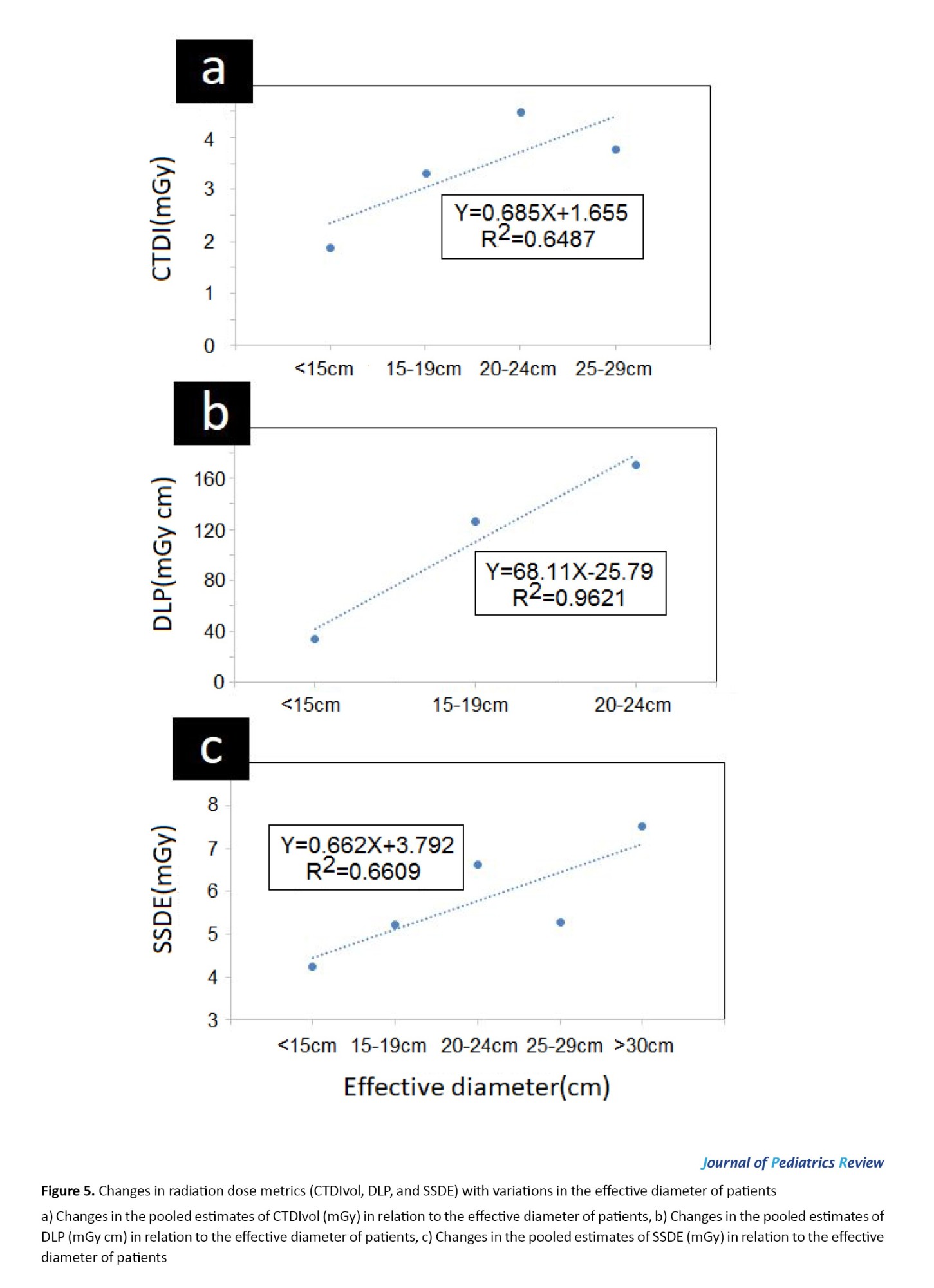
For the five effective diameters of patients, the pooled estimates for CTDIvol, DLP, and SSDE metrics are plotted separately in Figure 5. In this plot, changes in radiation dose metrics were evaluated in relation to changes in the effective diameter of patients.
Risk of bias across studies
For evaluating publication bias among studies, Begg’s funnel plots for radiation dose metrics (CTDIvol, DLP, and SSDE) were visually inspected (analyses are not presented here). For each radiation dose metric, Begg’s funnel plots related to five groups of effective diameters were investigated in separate subfigures. The shapes of Begg’s funnel plots were considered to be moderately asymmetrical, which demonstrates the publication bias in the reports.
Discussion
Red bone marrow, breast tissue, and thyroid glands are some of the most radiosensitive organs that may be irradiated in chest CT examinations. Due to the increasing potential of radiation-induced damage during pediatric CT, protocol optimization is crucial for children’s imaging [4]. Establishing DRL is an effective method for monitoring radiation doses and reducing excessive radiation levels in medical imaging [17, 33, 35]. DRL data are used as a quality measure for local centers and provide the performance comparison between a medical imaging center with other institutions [10].
In the current study, we explored the literature on existing size‑specific DRLs and determined radiation dose metrics (CTDIvol, DLP, and SSDE) for five patient sizes in the pediatric chest CT examinations. Although there are original articles describing the establishment of DRLs for different institutions, no meta-analysis has been carried out on this subject. To the best of our knowledge, this report is the first meta-analysis exploring the literature on existing size‑specific DRLs to determine radiation dose metrics for five patient sizes in pediatric chest CT examinations.
There are a few limited review studies on the establishment of DRLs for pediatric CT examinations [20, 22-28]. In the study by Kadavigere et al. [20], the reported DRLs and methods used to determine these DRLs for pediatric CT examinations were reviewed. Their systematic review was performed in accordance with the PRISMA checklist, and a total of 501 articles were retrieved from Cochrane Library, Scopus, CINAHL, PubMed/Medline, and Web of Science databases. In the comparison of DRLs between studies, conflicting results were listed for the DRLs of head and chest CT examinations. Some of the DRL values were within the recommended ranges, and others were higher than the limits. This study merely reported the DRL values without any analysis.
A similar study reviewed the magnitudes of DRL variation and the factors influencing these variations [23]. The evaluation of the results of 52 articles indicated that the variation of PDRLs for a specified brain examination in a similar age group could reach a factor of 2-fold. Their results showed that the size of the scanning area is one of the main factors attributable to DRL variations.
These studies did not present pooled estimates for DRLs. The reviews mainly described the different techniques proposed to define DRLs, the DRLs reported, the scanning protocols, and the methods used to classify patients. In our study, in addition to evaluating the DRLs of pediatric CT examinations for five patient sizes in different countries, we also present the pooled estimates of these DRLs worldwide.
Our primary analysis on a total number of 4761 patients undergoing pediatric chest CT found that the weighted pooled estimates for CTDIvol (mGy) in patients with effective diameters of <15 cm, 15-19 cm, 20-24 cm, and 25-29 cm were 1.89 mGy (95% CI, 0.87%, 2.9% mGy), 3.31 mGy (95% CI, 2.06%, 4.55% mGy), 4.49 mGy (95% CI, 2.02%, 6.96% mGy), and 3.78 mGy (95% CI, 3.42%, 4.14% mGy), respectively. The pooled estimates for DLP (mGy cm) in patients with effective diameters of <15 cm, 15-19 cm, and 20-24 cm were 34.52 mGy cm (95% CI, 16.56%, 52.47% mGy cm), 126.03 mGy cm (95% CI, 70.3%, 181.76% mGy cm), and 170.74 mGy cm (95% CI, 62.4%, 279.08% mGy cm), respectively. The pooled estimates for SSDE (mGy) in patients with effective diameters of <15 cm, 15-19 cm, 20-24 cm, 25-29 cm, and ≥30 cm were 4.24 mGy (95% CI, 2.66%, 5.81% mGy), 5.23 mGy (95% CI, 3.77%, 6.69% mGy), 6.61 mGy (95% CI, 5.24%, 7.98% mGy), 5.29 mGy (95% CI, 5.07%, 5.51% mGy), and 7.52 mGy (95% CI, 7.39%, 7.65% mGy), respectively. These pooled estimates were generally higher than those recommended by the European Commission (radiation protection No. 185) [4, 36], which indicates that the protocol settings for pediatric chest CT scans are not fully optimized. These findings imply the need for reviewing and optimizing pediatric chest CT protocols.
As shown in Figure 5, the pooled estimates for the radiation dose metrics were increased by increasing the effective diameters of the patients. The absorbed dose is the amount of energy deposited by x-ray photons in the bodies of patients undergoing scans. Hence, radiation dose metrics may increase by increasing the effective diameters of the patients. The effect of tissue volume on the absorbed dose magnitudes confirms the results presented in Figure 5.
The reported radiation dose metrics (CTDIvol, DLP, and SSDE) were categorized and subgrouped according to study locations. For all radiation dose metrics (CTDIvol, DLP, and SSDE), there were significant subgroup effects for the study location (P<0.001). It means that the study location significantly modifies radiation dose metrics reported for pediatric chest CT examinations. The wide variation of DRIs reported for different countries can be mainly due to different scanning parameters used in medical imaging institutions (including kVp, mA, scanning time, pitch factor, slice thickness, etc.) [1]. There is no standardized acquisition protocol [10], and scanning parameters influenced the patients’ doses. On the other hand, image processing technology is constantly being improved to reduce patient doses and enhance the quality of images [10]. These factors also lead to expanding the range of radiation dose magnitudes even for a specific CT procedure. Therefore, establishing DRL and comparing achieved data with those of other institutions must be considered a permanent moving target to keep patients’ doses within the permitted limits.
Patient dose surveys are periodically performed to evaluate whether the patient’s doses are acceptable compared to the recommended and reported DRLs [10]. These comparisons are complicated when patient characteristics are not similarly documented [20]. Institutions stratify their patients by different categories [10], which makes the comparison of DRL data difficult. Thus, a worldwide consensus is needed for harmonization in the classification of patients. This study recommends the establishment of a standard size set for data registration that considerably facilitates the comparison of DRLs across local and international levels.
Conclusion
Radiation protection is of great importance for pediatric CT examinations because children have a higher radiosensitivity and longer life expectancy than adults. For imaging departments, the radiation exposure to children and the optimization status of scanning protocols can be assessed based on the recommended DRL indices. In this study, literature on existing size‑specific DRLs was reviewed to determine radiation dose metrics for five patient sizes in pediatric chest CT examinations. The results indicated that the pooled estimates for radiation dose metrics of pediatric chest CT examinations were generally higher than the recommended limits. Therefore, the pediatric chest CT protocols must be reviewed and optimized worldwide.
Limitations
This study attempted to highlight the necessity for optimizing scanning protocols and improving DRLs of pediatric CT examinations in order to adhere to specified radiation protection limits. Although a comprehensive systematic review was performed following PRISMA guidelines, we could not evaluate DRLs for abdominopelvic and abdomen CT examinations due to the lack of sufficient studies to perform a meta-analysis (n<3). In addition to the need to assess the DRLs for abdominopelvic and abdomen CT examinations, due to worldwide concerns about the radiation dose to children during CT imaging and the notable rise in studies on this topic, updating this meta-analysis is essential in the near future.
Ethical Considerations
Compliance with ethical guidelines
All experimental protocols were approved by the ethical committee of Abadan University of Medical Sciences (Code: IR.ABADANUMS.REC.1402.119). All research processes were performed in accordance with the relevant guidelines and regulations of the ethical committee of Abadan University of Medical Sciences, Abadan, Iran.
Funding
This study was supported by the research project, Funded by Abadan University of Medical Sciences, Abadan, Iran (Grant No.: 1402U-1713).
Authors contributions
Conceptualization, methodology, formal analysis, data curation, and resources: Seyed Salman Zakariaee, and Hadi Kazemi-Arpanahi; Data collection and writing: Seyed Salman Zakariaee, Negar Naderi, and Hadi Kazemi-Arpanahi.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to acknowledge the role of the Research Deputy of the Abadan University of Medical Sciences, Abadan, Iran, for financially supporting this project.
References
Computed tomography (CT) is one of the most common diagnostic methods used in clinics. Studies have estimated that more than 62 million CTs are performed annually in the U.S., and at least 6.45% of them are related to pediatric imaging [1, 2]. A dramatic increase in pediatric CT examinations was reported over the past several decades [3].
Radiation protection holds particular importance for imaging examinations that involve high radiation doses, such as CT scans [4, 5]. Children exhibit higher radiosensitivity than adults due to the increased radiosensitivity of their developing organs and tissues. After radiation exposure during the CT examinations, there is a longer life expectancy for children than adults, leading to higher lifetime risks of developing radiation-induced malignancies [6, 7]. Consequently, radiation-induced diseases may occur with several times greater risk for children than for adults in an identical CT examination. For pediatric CT imaging, it is essential to keep the radiation dose as low as reasonably practicable without compromising the quality of the diagnostic images [8-11]. The International Commission on Radiological Protection (ICRP) introduced diagnostic reference levels (DRLs) criteria in 1996 to meet this need [3, 12-14]. Based on this recommended index, it could be determined whether the scanning protocols of CT examinations have been adequately optimized [15]. Volumetric CT dose index (CTDIvol), dose length product (DLP), and size-specific dose estimates (SSDE) are the dosimetric quantities recommended for DRL establishment [11, 16].
The importance of establishing DRLs for pediatric imaging was emphasized in European guidelines on DRLs for pediatrics (radiation protection No. 185), and the first establishment of DRLs for pediatric CT was reported in 2000 [12, 15]. Since then, DRLs for pediatric CT examinations have been announced by different countries and associations. The reported values were considerably different based on the study location, even for the same CT scanner. These differences may be the result of several factors, including the type of CT scanner and its characteristics, CT examination protocol, patient’s body size, etc. [1, 17, 18].
The major problem in comparing the established DRLs is the wide range of patient sizes, even within the same age group, which results in a considerable variation in radiation doses announced for institutions and countries [4, 19]. ICRP 135 and European guidelines on DRLs for pediatric imaging recommended the establishment of age‑ and size‑specific DRLs to deal with this problem [20]. The results of pioneering studies have shown that patient sizes do not correlate with age bands, and patient size has been suggested as the more preferred index to design scanning protocols and radiation dose management in medical imaging centers [3, 19]. The size and material compositions of the scanning area are the main factors to determine absorbed dose magnitudes during a radiological examination. Hence, it is recommended in international guidelines that patient size must be considered the primary criterion for establishing the DRLs. During the transition period, age may serve as an additional index [21].
There are a few limited review studies on the establishment of DRLs for pediatric CT examinations, which mainly describe age-specific DRLs [20, 22-28]. To our knowledge, a dedicated systematic review and meta-analysis study has not yet been performed for the assessment of size‑specific DRLs of pediatric CT examinations. The objective of the current study was to explore the literature on existing size‑specific DRLs and determine radiation dose metrics (CTDIvol, DLP, and SSDE) for five patient sizes in pediatric CT examinations.
Methods
Protocol of the systematic review and meta-analysis
The systematic review and meta-analysis were conducted according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) checklist [29].
Information sources and search strategies
A systematic literature search was carried out using Web of Science, PubMed, Embase, Scopus databases, and the Google Scholar search engine. The following MeSH and non-MeSH terms were used for literature searching: (“diagnostic reference level”* OR “DRL”*) AND (CT OR “computed tomography” OR “x-ray CT scan” OR “x-ray CAT scan” OR “CT scan” OR “CAT scan”).
The systematic literature search was conducted without the beginning date restriction until May 2024. Case reports, editorials, commentaries, and opinions were not included in the meta-analysis.
Eligibility criteria
Studies were pre-included if they reported the establishment of DRLs for pediatric CT examinations based on patient size. A child was defined as a human being from birth to the age of 18 [30]. Hence, as the inclusion criterion, this limit was applied to the age of the study participants, and publications investigating only DRLs for pediatric CT examinations were included. The exclusion criteria were as follows: 1) Studies that reported DRL values for imaging modalities other than CT. 2) The age of participants for whom DRL values were reported exceeded the age limit defined for a child. 3) Studies that did not provide sufficient data to calculate the Mean±SD for radiation dose metrics. However, no limitation was applied to the studied part of the body, the size of participants, the publication language, and the sex of the study participants.
Study selection and data collection process
The first author of the selected reports, publication date, study location, sizes of the study participants, sample size, radiation dose metrics (CTDIvol, DLP, and SSDE) for five patient sizes in pediatric CT, DRLs, and other related information were extracted from the studies. For studies that reported radiation dose metrics as median and first quartile (Q1) to third quartile (Q3) range, the Mean±SD values were extracted using the Equations 1 and 2:
1. Mean=(Median+Q1+Q3)/3
2. SD=(Q3-Q1)/1.35
The main data extracted are presented in Table 1.
Quality assessment of the studies
The quality and risk of bias of the studies were evaluated using the Newcastle-Ottawa scale (NOS). The risk of bias for each study was assessed based on three aspects, including the selection of the exposed populations, comparability, and outcome measurements. The maximum score for a study is 7.
Summary measures and synthesis of results
STATA software, version 16.0, was used for data analysis. In this study, the Mean±SD of radiation dose metrics reported for each patient size group were used to determine the overall effect size. Cochran’s Q test and the inconsistency index (I2) test were used to evaluate heterogeneity between studies.
The possible sources of between-study heterogeneity were assessed through subgroup analysis, where the study location was evaluated as the moderator variable. Publication bias among studies was evaluated through visual inspection of the generated funnel plots. Publication bias refers to the condition where a study has a low probability of being published when its results are negative, non-significant, or have small effects.
Results
Study selection
A total of 1,521 articles were identified through the initial search. Seven hundred sixty-four duplicate articles were removed, and 291 papers were screened based on their titles and abstracts. The full texts of 60 studies were evaluated after removing irrelevant studies. The reports that did not have sufficient data to calculate the Mean±SD for radiation dose metrics were excluded. Finally, six reports regarding the establishment of DRLs for pediatric CT examinations were included in the meta-analytical processes based on the inclusion criteria (Figure 1).
Characteristics and quality of the included studies
The characteristics of the included studies regarding the establishment of DRLs for pediatric CT examinations based on patient size are detailed in Table 1. The table presents the first author, publication date, study location, sizes of the study participants, DRLs, and the sample sizes of the studies reporting DRLs for pediatric patients undergoing chest, abdominopelvic, and abdomen CT examinations. The quality scores of the included articles are listed in the last column. All six included articles were rated as high quality (four articles had a score of 7, and two articles had a score of 6). Thus, the quality of the studies was not the source of heterogeneity among the studies. This study retrieved a total of 4761 patients undergoing pediatric CT examinations. Modern CT scanners are equipped with tube current modulation (TCM) that alters the x-ray tube current as a function of patient attenuation at a given region of interest. TCM yields significant reductions in patient doses while maintaining image noise. Therefore, the dose surveys for establishing DRLs in pediatric CT examinations are recommended to be performed in the patient grouping based on their effective diameters or water equivalent diameters [3]. The meta-analysis was performed for studies describing the establishment of DRLs for pediatric CT examinations based on the effective diameter (cm) or water equivalent diameter (cm) of the patients. For abdominopelvic and abdomen CT examinations, there were not enough studies to perform a meta-analysis test (n<3). Hence, the radiation dose metrics (CTDIvol, DLP, and SSDE) were only analyzed for pediatric chest CT. The extracted data for five groups of effective diameters, including <15 cm, 15–19 cm, 20–24 cm, 25–29 cm, and ≥30 cm, were entered into the analysis. Two articles written by Goske et al. [31] and Westra et al. [34] reported data from the same registry and had identical values. Therefore, only one of them was included in the analysis.
Risk of bias within the studies
For all radiation dose metrics (CTDIvol, DLP, and SSDE) in five groups of effective diameters, the significance value obtained from the χ2 test of heterogeneity was <0.001. Moreover, the I2 values for all studies ranged from 94.3% to 100%. Therefore, the random-effects model of the meta-analysis was used for the studies.
Synthesis of the results
The forest plots for radiation dose metrics (CTDIvol, DLP, and SSDE) are presented in Figures 2, 3 and 4, respectively.
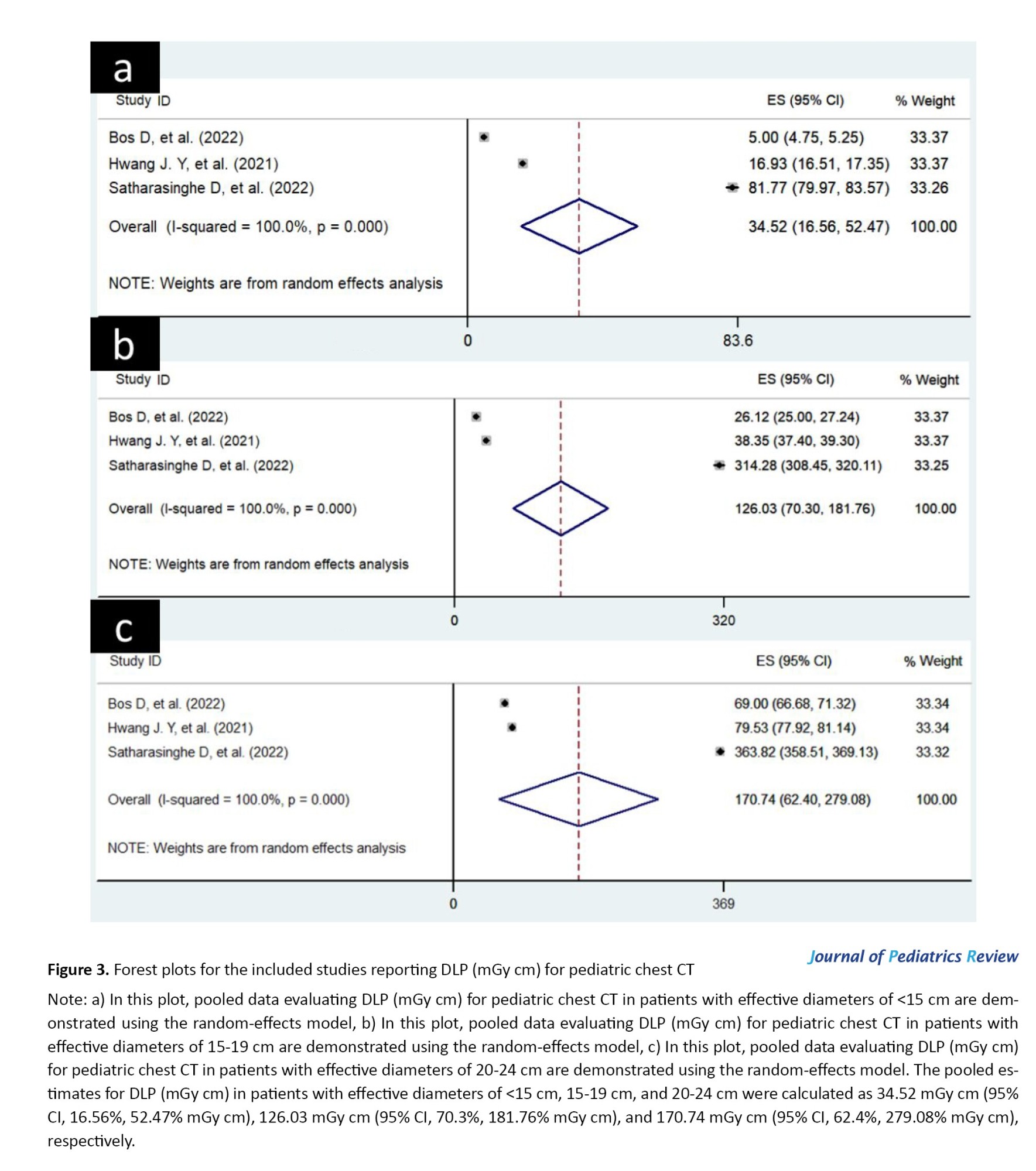
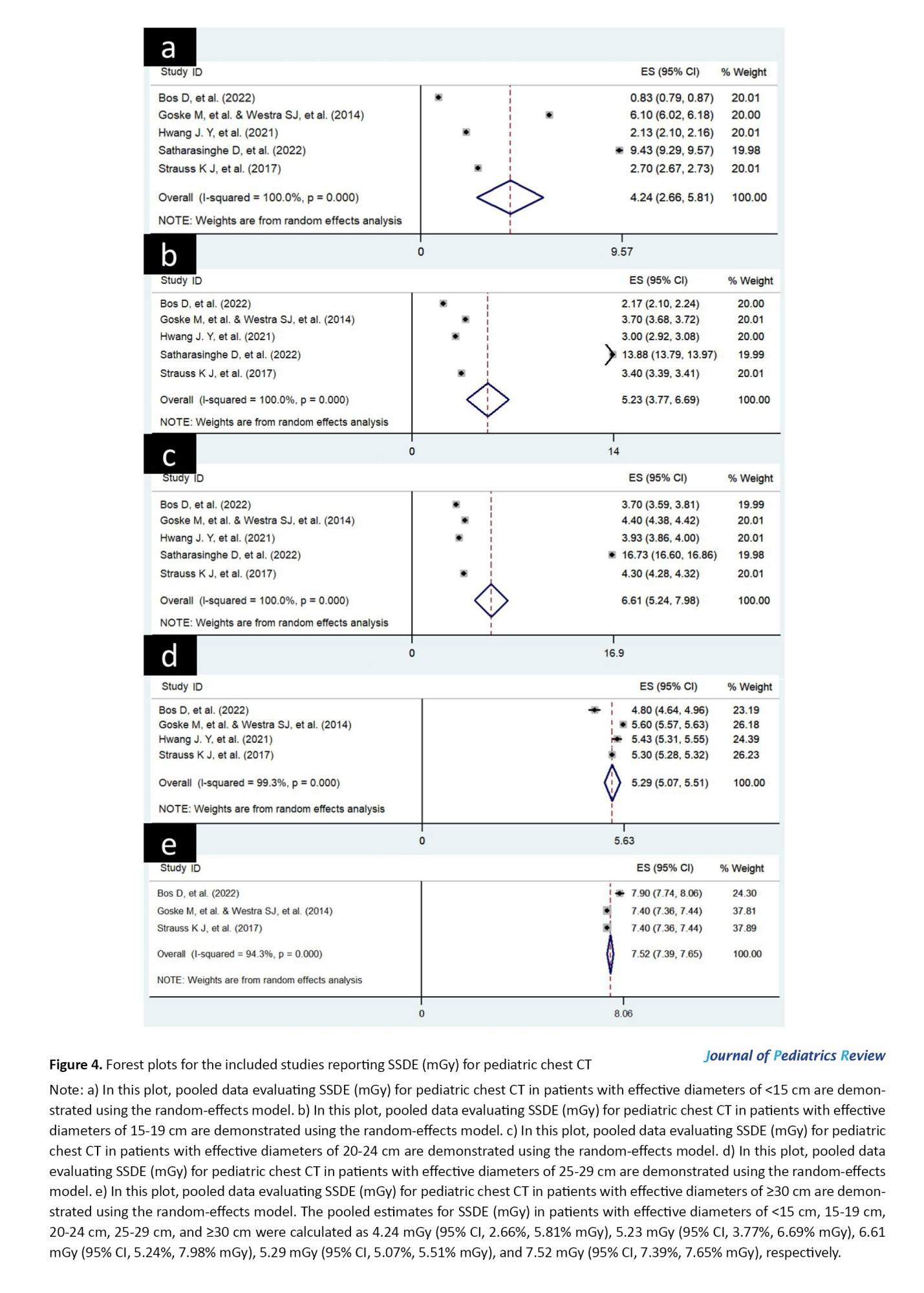
In these representations, the mean effect sizes (with 95% CI) of studies and the overall effect sizes (with 95% CI) for five groups of effective diameters are presented in separate subfigures. The pooled estimates for all radiation dose metrics in five groups of effective diameters are listed in Table 2.
For the five effective diameters of patients, the pooled estimates for CTDIvol, DLP, and SSDE metrics are plotted separately in Figure 5. In this plot, changes in radiation dose metrics were evaluated in relation to changes in the effective diameter of patients.
Risk of bias across studies
For evaluating publication bias among studies, Begg’s funnel plots for radiation dose metrics (CTDIvol, DLP, and SSDE) were visually inspected (analyses are not presented here). For each radiation dose metric, Begg’s funnel plots related to five groups of effective diameters were investigated in separate subfigures. The shapes of Begg’s funnel plots were considered to be moderately asymmetrical, which demonstrates the publication bias in the reports.
Discussion
Red bone marrow, breast tissue, and thyroid glands are some of the most radiosensitive organs that may be irradiated in chest CT examinations. Due to the increasing potential of radiation-induced damage during pediatric CT, protocol optimization is crucial for children’s imaging [4]. Establishing DRL is an effective method for monitoring radiation doses and reducing excessive radiation levels in medical imaging [17, 33, 35]. DRL data are used as a quality measure for local centers and provide the performance comparison between a medical imaging center with other institutions [10].
In the current study, we explored the literature on existing size‑specific DRLs and determined radiation dose metrics (CTDIvol, DLP, and SSDE) for five patient sizes in the pediatric chest CT examinations. Although there are original articles describing the establishment of DRLs for different institutions, no meta-analysis has been carried out on this subject. To the best of our knowledge, this report is the first meta-analysis exploring the literature on existing size‑specific DRLs to determine radiation dose metrics for five patient sizes in pediatric chest CT examinations.
There are a few limited review studies on the establishment of DRLs for pediatric CT examinations [20, 22-28]. In the study by Kadavigere et al. [20], the reported DRLs and methods used to determine these DRLs for pediatric CT examinations were reviewed. Their systematic review was performed in accordance with the PRISMA checklist, and a total of 501 articles were retrieved from Cochrane Library, Scopus, CINAHL, PubMed/Medline, and Web of Science databases. In the comparison of DRLs between studies, conflicting results were listed for the DRLs of head and chest CT examinations. Some of the DRL values were within the recommended ranges, and others were higher than the limits. This study merely reported the DRL values without any analysis.
A similar study reviewed the magnitudes of DRL variation and the factors influencing these variations [23]. The evaluation of the results of 52 articles indicated that the variation of PDRLs for a specified brain examination in a similar age group could reach a factor of 2-fold. Their results showed that the size of the scanning area is one of the main factors attributable to DRL variations.
These studies did not present pooled estimates for DRLs. The reviews mainly described the different techniques proposed to define DRLs, the DRLs reported, the scanning protocols, and the methods used to classify patients. In our study, in addition to evaluating the DRLs of pediatric CT examinations for five patient sizes in different countries, we also present the pooled estimates of these DRLs worldwide.
Our primary analysis on a total number of 4761 patients undergoing pediatric chest CT found that the weighted pooled estimates for CTDIvol (mGy) in patients with effective diameters of <15 cm, 15-19 cm, 20-24 cm, and 25-29 cm were 1.89 mGy (95% CI, 0.87%, 2.9% mGy), 3.31 mGy (95% CI, 2.06%, 4.55% mGy), 4.49 mGy (95% CI, 2.02%, 6.96% mGy), and 3.78 mGy (95% CI, 3.42%, 4.14% mGy), respectively. The pooled estimates for DLP (mGy cm) in patients with effective diameters of <15 cm, 15-19 cm, and 20-24 cm were 34.52 mGy cm (95% CI, 16.56%, 52.47% mGy cm), 126.03 mGy cm (95% CI, 70.3%, 181.76% mGy cm), and 170.74 mGy cm (95% CI, 62.4%, 279.08% mGy cm), respectively. The pooled estimates for SSDE (mGy) in patients with effective diameters of <15 cm, 15-19 cm, 20-24 cm, 25-29 cm, and ≥30 cm were 4.24 mGy (95% CI, 2.66%, 5.81% mGy), 5.23 mGy (95% CI, 3.77%, 6.69% mGy), 6.61 mGy (95% CI, 5.24%, 7.98% mGy), 5.29 mGy (95% CI, 5.07%, 5.51% mGy), and 7.52 mGy (95% CI, 7.39%, 7.65% mGy), respectively. These pooled estimates were generally higher than those recommended by the European Commission (radiation protection No. 185) [4, 36], which indicates that the protocol settings for pediatric chest CT scans are not fully optimized. These findings imply the need for reviewing and optimizing pediatric chest CT protocols.
As shown in Figure 5, the pooled estimates for the radiation dose metrics were increased by increasing the effective diameters of the patients. The absorbed dose is the amount of energy deposited by x-ray photons in the bodies of patients undergoing scans. Hence, radiation dose metrics may increase by increasing the effective diameters of the patients. The effect of tissue volume on the absorbed dose magnitudes confirms the results presented in Figure 5.
The reported radiation dose metrics (CTDIvol, DLP, and SSDE) were categorized and subgrouped according to study locations. For all radiation dose metrics (CTDIvol, DLP, and SSDE), there were significant subgroup effects for the study location (P<0.001). It means that the study location significantly modifies radiation dose metrics reported for pediatric chest CT examinations. The wide variation of DRIs reported for different countries can be mainly due to different scanning parameters used in medical imaging institutions (including kVp, mA, scanning time, pitch factor, slice thickness, etc.) [1]. There is no standardized acquisition protocol [10], and scanning parameters influenced the patients’ doses. On the other hand, image processing technology is constantly being improved to reduce patient doses and enhance the quality of images [10]. These factors also lead to expanding the range of radiation dose magnitudes even for a specific CT procedure. Therefore, establishing DRL and comparing achieved data with those of other institutions must be considered a permanent moving target to keep patients’ doses within the permitted limits.
Patient dose surveys are periodically performed to evaluate whether the patient’s doses are acceptable compared to the recommended and reported DRLs [10]. These comparisons are complicated when patient characteristics are not similarly documented [20]. Institutions stratify their patients by different categories [10], which makes the comparison of DRL data difficult. Thus, a worldwide consensus is needed for harmonization in the classification of patients. This study recommends the establishment of a standard size set for data registration that considerably facilitates the comparison of DRLs across local and international levels.
Conclusion
Radiation protection is of great importance for pediatric CT examinations because children have a higher radiosensitivity and longer life expectancy than adults. For imaging departments, the radiation exposure to children and the optimization status of scanning protocols can be assessed based on the recommended DRL indices. In this study, literature on existing size‑specific DRLs was reviewed to determine radiation dose metrics for five patient sizes in pediatric chest CT examinations. The results indicated that the pooled estimates for radiation dose metrics of pediatric chest CT examinations were generally higher than the recommended limits. Therefore, the pediatric chest CT protocols must be reviewed and optimized worldwide.
Limitations
This study attempted to highlight the necessity for optimizing scanning protocols and improving DRLs of pediatric CT examinations in order to adhere to specified radiation protection limits. Although a comprehensive systematic review was performed following PRISMA guidelines, we could not evaluate DRLs for abdominopelvic and abdomen CT examinations due to the lack of sufficient studies to perform a meta-analysis (n<3). In addition to the need to assess the DRLs for abdominopelvic and abdomen CT examinations, due to worldwide concerns about the radiation dose to children during CT imaging and the notable rise in studies on this topic, updating this meta-analysis is essential in the near future.
Ethical Considerations
Compliance with ethical guidelines
All experimental protocols were approved by the ethical committee of Abadan University of Medical Sciences (Code: IR.ABADANUMS.REC.1402.119). All research processes were performed in accordance with the relevant guidelines and regulations of the ethical committee of Abadan University of Medical Sciences, Abadan, Iran.
Funding
This study was supported by the research project, Funded by Abadan University of Medical Sciences, Abadan, Iran (Grant No.: 1402U-1713).
Authors contributions
Conceptualization, methodology, formal analysis, data curation, and resources: Seyed Salman Zakariaee, and Hadi Kazemi-Arpanahi; Data collection and writing: Seyed Salman Zakariaee, Negar Naderi, and Hadi Kazemi-Arpanahi.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to acknowledge the role of the Research Deputy of the Abadan University of Medical Sciences, Abadan, Iran, for financially supporting this project.
References
- Afzalipour R, Abdollahi H, Hajializadeh MS, Jafari S, Mahdavi SR. [Estimation of diagnostic reference levels for children computed tomography: A study in Tehran, Iran (Persian)]. Int J Radiat Res. 2019; 17(3):407-13. [Link]
- Bouaoun A, Omrane LB, Mogaadi M, Khomsi WD, Zidi A, Hammou A. Pediatric head CT exposure doses in Tunisia: A Pilot study towards the establishment of national diagnostic reference levels. Radiat Prot Dosim. 2018; 182(2):241-51. [DOI:10.1093/rpd/ncy055] [PMID]
- Hwang JY, Choi YH, Yoon HM, Ryu YJ, Shin HJ, Kim HG, et al. Establishment of local diagnostic reference levels of pediatric abdominopelvic and chest CT examinations based on the body weight and size in Korea. Korean J Radiol. 2021; 22(7):1172-84. [DOI:10.3348/kjr.2020.0890] [PMID] [PMCID]
- Bos D, Zensen S, Opitz MK, Haubold J, Nassenstein K, Kinner S, et al. Diagnostic reference levels for chest computed tomography in children as a function of patient size. Pediatr Radiol. 2022; 52(8):1446-55. [DOI:10.1007/s00247-022-05340-8] [PMID] [PMCID]
- Zira DJ, Yahaya TH, Umar M, Chukwuemeka N, Sidi M, Emmanuel R, et al. Clinical indication-based diagnostic reference levels for paediatric head computed tomography examinations in Kano Metropolis, northwestern Nigeria. Radiography. 2021; 27(2):617-21. [DOI:10.1016/j.radi.2020.11.021]
- United Nations Scientific Committee on the Effects of Atomic Radiation. Sources, effects and risks of ionizing radiation, united nations scientific committee on the effects of atomic radiation (UNSCEAR) 2013 report, volume II: Scientific Annex B-Effects of radiation exposure of children. Vienna: United Nations Scientific Committee on the Effects of Atomic Radiation; 2013. [Link]
- Kutanzi KR, Lumen A, Koturbash I, Miousse IR. Pediatric exposures to ionizing radiation: Carcinogenic considerations. Int J Environ Res Public health. 2016; 13(11):1-14. [DOI:10.3390/ijerph13111057] [PMID] [PMCID]
- Ploussi A, Syrgiamiotis V, Makri T, Hatzigiorgi C, Efstathopoulos EP. Local diagnostic reference levels in pediatric CT examinations: A survey at the largest children’s hospital in Greece. Br J Radiol. 2020; 93(1116):1-6. [DOI:10.1259/bjr.20190358] [PMID] [PMCID]
- Ashworth E, Woods L, Cook JV. Diagnostic reference levels in paediatric fluoroscopy: How does a secondary referral centre compare with 2018 European guidelines? Br J Radiol. 2021; 94(1123):1-5. [DOI:10.1259/bjr.20201269] [PMID] [PMCID]
- Bibbo G, Brown S, Linke R. Diagnostic reference levels of paediatric computed tomography examinations performed at a dedicated Australian paediatric hospital. J Med Imaging Radiat Oncol. 2016; 60(4):475-84. [DOI:10.1111/1754-9485.12488]
- Tahmasebzadeh A, Paydar R, Kermanshahi MS, Maziar A, Rezaei M, Reiazi R. Pediatric regional DRL assessment in common CT examinations for medical exposure optimization in Tehran, Iran. Radiat Prot Dosim. 2020; 192(3):341-9. [DOI:10.1093/rpd/ncaa192] [PMID]
- Benmessaoud M, Dadouch A, Talbi M, Tahiri M, El-Ouardi Y. Diagnostic reference levels for paediatric head computed tomography in Morocco: A nationwide survey. Radiat Prot Dosim. 2020; 191(4):400-8. [DOI:10.1093/raddos/ncaa170] [PMID]
- Célier D, Roch P, Etard C, Ducou Le Pointe H, Brisse HJ. Multicentre survey on patient dose in paediatric imaging and proposal for updated diagnostic reference levels for France. Part 1: Computed tomography. Eur Radiol. 2020; 30(2):1156-65. [DOI:10.1007/s00330-019-06405-3] [PMID]
- Kanal KM, Butler PF, Chatfield MB, Wells J, Samei E, Simanowith M, et al. U.S. diagnostic reference levels and achievable doses for 10 pediatric CT examinations. Radiology. 2022; 302(1):164-74. [DOI:10.1148/radiol.2021219027] [PMID]
- Kim JS, Lee SK, Kim SK, Yoo SM, Kim JM, Yoon SW. National diagnostic reference levels and achievable doses for 13 adult ct protocols and a paediatric head ct protocol: National survey of Korean hospitals. Radiat Prot Dosimetry. 2019; 187(2):220-9. [DOI:10.1093/rpd/ncz156] [PMID]
- Imai R, Miyazaki O, Horiuchi T, Kurosawa H, Nosaka S. Local diagnostic reference level based on size-specific dose estimates: Assessment of pediatric abdominal/pelvic computed tomography at a Japanese national children’s hospital. Pediatr Radiol. 2015; 45(3):345-53. [DOI:10.1007/s00247-014-3189-4] [PMID]
- Kim MC, Chang KH, Hwang JH, Nam YC, Han DK, Yoon J. Radiation dose for pediatric and young adult CT: A survey to establish age-based reference levels of 2015-2016 in Korea. Radiat Prot Dosim. 2017; 175(2):228-37. [DOI:10.1093/rpd/ncw289] [PMID]
- Mohammadbeigi A, Khoshgard K, Haghparast A, Eivazi MT. Local DRLs for paediatric CT examinations based on size-specific dose estimates in Kermanshah, Iran. Radiat Prot Dosim. 2019; 186(4):496-506. [DOI:10.1093/rpd/ncz056] [PMID]
- Järvinen H, Seuri R, Kortesniemi M, Lajunen A, Hallinen E, Savikurki-Heikkilä P, et al. Indication-based national diagnostic reference levels for paediatric CT: A newapproach with proposed values. Radiat Prot Dosim. 2015; 165(1-4):86-90. [DOI:10.1093/rpd/ncv044] [PMID]
- Kadavigere R, Sukumar S, Pendem S. Diagnostic reference levels for computed tomography examinations in pediatric population-a systematic review. J Cancer Res Ther. 2021; 17(4):845-52. [DOI:10.4103/jcrt.JCRT_945_20] [PMID]
- Hwang J, Yoon HM, Hwang JY, Choi YH, Lee YY, Lee SM, et al. Establishment of local diagnostic reference levels for pediatric neck CT at Nine University Hospitals in South Korea. Korean J Radiol. 2025; 26(1):65-74. [DOI:10.3348/kjr.2024.0689] [PMID] [PMCID]
- Aljuaid LM, Althobaiti SF, Althobaiti AA, Alsufyani AH, Alotaibi MH, Elkhader BA, et al. Age-specific DRLs for pediatric brain CT: A review for exploring the practices in Saudi Arabia. Appl Radiat Isot. 2025; 217:111664. [DOI:10.1016/j.apradiso.2025.111664] [PMID]
- Garba I, Engel-Hills P. Paediatric diagnostic reference levels for common computed tomography procedures: A systematic review. Radiography. 2025; 31(1):27-35. [DOI:10.1016/j.radi.2024.09.058] [PMID]
- Triantopoulou S, Hernàndez AC, Tsapaki V. A literature review of paediatric diagnostic reference levels in diagnostic and interventional radiology and cardiology. Hell J Radiol. 2020; 5(4):24-44. [Link]
- Abanomy A. Computed tomography diagnostic reference levels for routine pediatric examinations in Saudi Arabia: A systematic review. Cureus. 2024; 16(10):1-8. [DOI:10.7759/cureus.71072] [PMID] [PMCID]
- Khafaji M, Albahiti S. Diagnostic reference levels in pediatric cardiac CT imaging: A literature review. Int J Biomed. 2023; 13(4):207-12. [DOI:10.21103/Article13(4)_RA2]
- Gyan E, Subaar C, Edusei G, Antwi Nyarko L. Paediatric computed tomography diagnostic reference levels in Africa: A systematic review. J Med Radiat Sci. 2025; 72(1):139-47. [DOI:10.1002/jmrs.824] [PMID] [PMCID]
- Satharasinghe D, Jeyasugiththan J, Wanninayake W, Pallewatte A. Paediatric diagnostic reference levels in computed tomography: A systematic review. J Radiol Prot. 2021; 41(1):1-27. [DOI:10.1088/1361-6498/abd840] [PMID]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann Intern Med. 2009; 151(4):65-94. [DOI:10.7326/0003-4819-151-4-200908180-00136] [PMID]
- Lansdown G, Vaghri Z. Article 1: Definition of a Child. In: Vaghri Z, Zermatten J, Lansdown G, Ruggiero R. Monitoring State compliance with the UN convention on the rights of the child children’s well-being: Indicators and research. Cham: Springer; 2022. [Link]
- Goske MJ, Strauss KJ, Coombs LP, Mandel KE, Towbin AJ, Larson DB, et al. Diagnostic reference ranges for pediatric abdominal CT. Radiology. 2013; 268(1):208-18. [DOI:10.1148/radiol.13120730] [PMID]
- Satharasinghe D, Jeyasugiththan J, Wanninayake WMNMB, Pallewatte AS, Samarasinghe RANKK. Patient size as a parameter for determining diagnostic reference levels for paediatric computed tomography (CT) procedures. Phys Med. 2022; 102:55-65. [DOI:10.1016/j.ejmp.2022.09.004] [PMID]
- Strauss KJ, Goske MJ, Towbin AJ, Sengupta D, Callahan MJ, Darge K, et al. Pediatric chest CT diagnostic reference ranges: Development and application. Radiology. 2017; 284(1):219-27. [DOI:10.1148/radiol.2017161530] [PMID]
- Westra S.J. GMJ, Chatfield M., Strauss K., Callahan M., Darge K., Frush D.P., Podberesky D., Towbin A., Prince J. Radiology quality improvement registry of ct scans in children (QUIRCC): Diagnostic reference levels for pediatric chest ct. Pediatr Radiol 2014; 44 (SUPPL. 2): S313. [DOI:10.1007/s00247-014-2968-2]
- Rawashdeh M, Abdelrahman M, Zaitoun M, Saade C, Alewaidat H, McEntee MF. Diagnostic reference levels for paediatric CT in Jordan. J Radiol Prot. 2019; 39(4):1060-73. [DOI:10.1088/1361-6498/ab3ee2] [PMID]
- Bosmans H, Damilakis J, Ducou le Pointe H, Foley SJ. Radiation protection No. 185 - European guidelines on diagnostic reference levels for paediatric imaging. Luxembourg: Publications Office of the European; 2018. [Link]
Type of Study: Meta-analysis Review |
Subject:
Radiology
Received: 2024/09/28 | Accepted: 2025/07/12 | Published: 2025/07/19
Received: 2024/09/28 | Accepted: 2025/07/12 | Published: 2025/07/19
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









