Volume 13, Issue 1 (1-2025)
J. Pediatr. Rev 2025, 13(1): 41-48 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ezoddin N, Sobhanian P, Mousavi S A, Reisi N. Management of Gastric Trichobezoar in Children: A Case Report and Literature Review. J. Pediatr. Rev 2025; 13 (1) :41-48
URL: http://jpr.mazums.ac.ir/article-1-697-en.html
URL: http://jpr.mazums.ac.ir/article-1-697-en.html
1- Pediatric Infectious Diseases Research Center, Communicable Diseases Institute, Mazandaran University of Medical Sciences, Sari, Iran.
2- Pediatric Infectious Diseases Research Center, Communicable Diseases Institute, Mazandaran University of Medical Sciences, Sari, Iran. & Student Research Committee, Faculty of Medicine, Mazandaran University of Medical Sciences, Sari, Iran. ,Drpooriasobhanian@outlook.com
3- Pediatric Infectious Diseases Research Center, Communicable Diseases Institute, Mazandaran University of Medical Sciences, Sari, Iran. & Student Research Committee, Faculty of Medicine, Mazandaran University of Medical Sciences, Sari, Iran.
2- Pediatric Infectious Diseases Research Center, Communicable Diseases Institute, Mazandaran University of Medical Sciences, Sari, Iran. & Student Research Committee, Faculty of Medicine, Mazandaran University of Medical Sciences, Sari, Iran. ,
3- Pediatric Infectious Diseases Research Center, Communicable Diseases Institute, Mazandaran University of Medical Sciences, Sari, Iran. & Student Research Committee, Faculty of Medicine, Mazandaran University of Medical Sciences, Sari, Iran.
Full-Text [PDF 670 kb]
(624 Downloads)
| Abstract (HTML) (1241 Views)
Full-Text: (638 Views)
Introduction
Trichobezoars, which are hairballs formed from ingested hair, represent a unique and often overlooked clinical entity, particularly in pediatric populations [1, 2]. These gastrointestinal obstructions are commonly associated with trichotillomania, a psychiatric disorder characterized by the compulsive pulling out of one’s hair, often accompanied by trichophagia or the ingestion of hair [3]. The prevalence of trichobezoar is notably higher in young females, [4] with studies indicating that they can lead to significant gastrointestinal complications if left untreated, including obstruction, perforation [4, 5], and even life-threatening conditions such as Rapunzel syndrome, where a long tail of hair extends into the intestines [6].
The clinical presentation of trichobezoars can be diverse, often mimicking other gastrointestinal disorders. Common symptoms include abdominal pain, nausea, vomiting, and changes in bowel habits. In some cases, patients may present with more severe complications, such as bowel obstruction or jaundice due to biliary obstruction caused by large trichobezoars [5, 6, 7, 8]. A literature review reveals that managing trichobezoars typically involves a combination of surgical intervention and psychiatric support [9]. Diagnostic modalities such as abdominal ultrasound, computed tomography (CT), and endoscopy are crucial for accurately identifying trichobezoars, allowing for timely surgical intervention when necessary [10, 11]. In addressing the psychological aspects of trichotillomania and trichophagia, it is essential to recognize the interplay between psychiatric disorders and gastrointestinal manifestations. Therefore, the management of trichobezoars must extend beyond surgical intervention to include comprehensive psychiatric care [12-14].
In this case report, we present the clinical management of a 12-year-old child with untreated trichotillomania who developed a trichobezoar, describing the gastrointestinal signs and symptoms, diagnostic methods employed, surgical interventions, and the multifaceted treatment approach. In addition, we will review the published literature to provide an up-to-date review of trichobezoar management in children.
Case Presentation
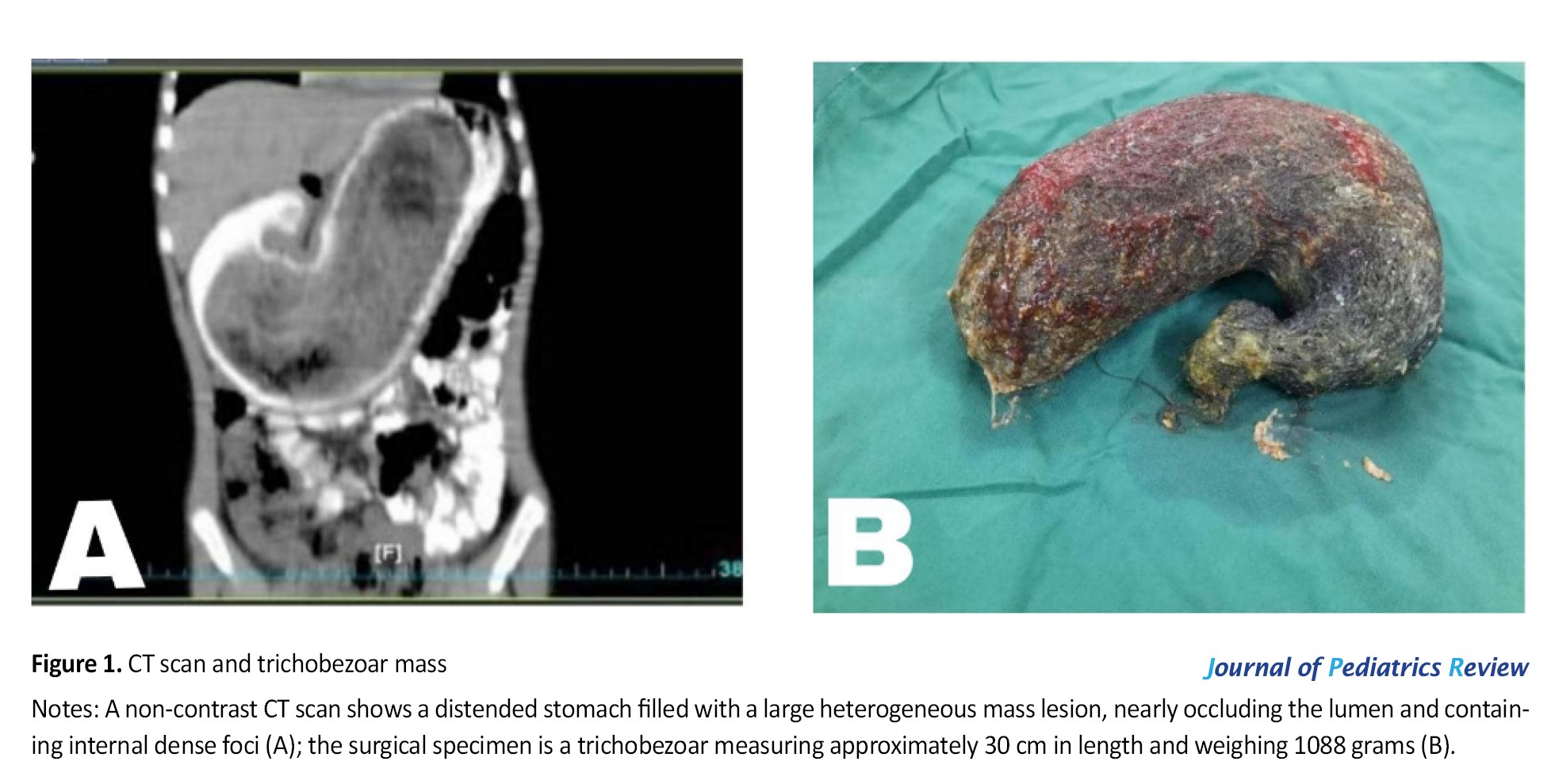
A 12-year-old girl was brought to the Emergency Department of Bou-Ali Sina Hospital in Sari City, Mazandaran Province, Iran, with persistent nausea, vomiting, and abdominal pain that had intensified over the past 20 days. The vomiting was non-bilious and non-bloody, primarily occurring in the mornings. The abdominal pain worsened with solid foods, was not positional, did not radiate, and had no relation to bowel movements. The patient’s history included dietary changes, significant weight loss of about 5 kg over the past month, melena, anorexia, dysphagia, odynophagia, and fever. There was no personal or family history of peptic ulcers, dyspnea, diarrhea, or constipation. However, the family history revealed a grandfather with gastric cancer and a father with obsessive behaviors. Vital signs were stable (temperature: 37 °C, blood pressure: 90/60 mm Hg, heart rate: 100 bpm, respiratory rate: 22 breaths/min), and the patient appeared generally healthy despite her symptoms. Notably, she had been pulling and eating her hair for 4 years. Physical examination revealed normal bowel sounds and a tender, non-mobile mass measuring 13×22 cm from the upper to lower abdomen. Dullness on percussion in the upper abdomen suggested a large mass in the anatomical area of the stomach. Hepatomegaly or splenomegaly was absent. The patient exhibited patchy hair loss on her scalp with varying lengths distributed across normal-appearing skin. Laboratory tests showed normal white blood cell counts and hemoglobin levels. However, elevated urea (28 mg/dL), lactate dehydrogenase (370 u/L), alkaline phosphatase (483 u/L), and an elevated erythrocyte sedimentation rate (27 mm/h) indicated possible underlying gastrointestinal pathology. Imaging studies prior to surgery revealed no pathological lesions on chest x-ray. An abdominal ultrasound showed a mass with echogenic margins measuring 109 mm in the upper abdomen, possibly indicating a space-occupying lesion such as a bezoar. An erect abdominal x-ray demonstrated a heterogeneous shadow under the gastric air bubble. Non-contrast CT imaging revealed a distended stomach containing a sizeable heterogeneous mass lesion, almost filling the lumen with internal dense foci (Figure 1). Management involved laparotomy and removal of an abdominal trichobezoar under general anesthesia. A midline incision revealed an enlarged stomach with thickened walls. A longitudinal incision allowed for the removal of the trichobezoar measuring approximately 30 cm in length and weighing 1088 g—a mass entirely composed of hair (Figure 1). Pathology confirmed an intragastric mass (trichobezoar) measuring 2×13×5.4 cm. A psychiatric consultation indicated that the patient had been suffering from trichotillomania for 4 years without treatment. Considering these findings and her history, a diagnosis of trichobezoar was established. After discharge, she was referred for continued psychiatric treatment to address her underlying condition.
Discussion
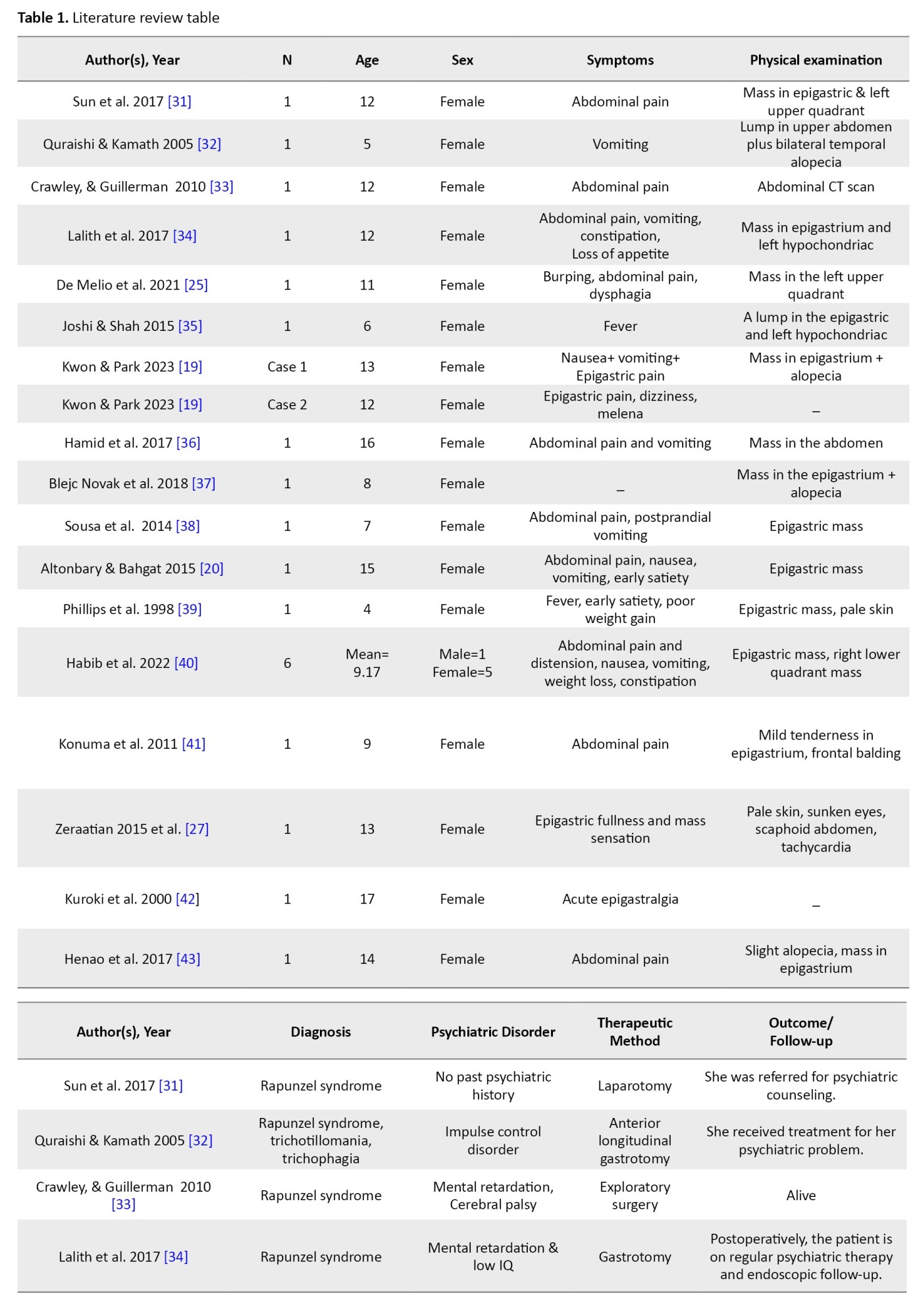
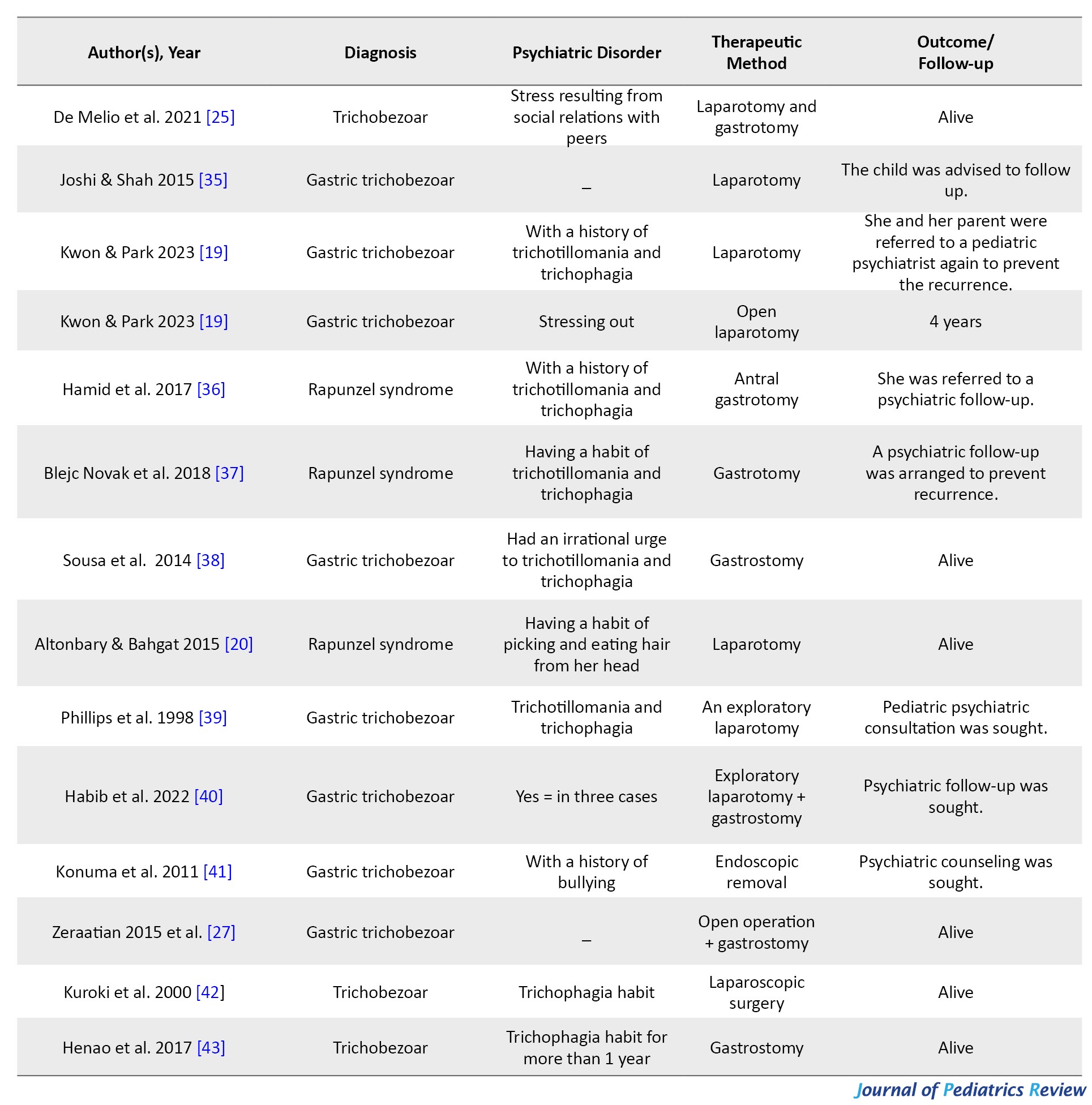
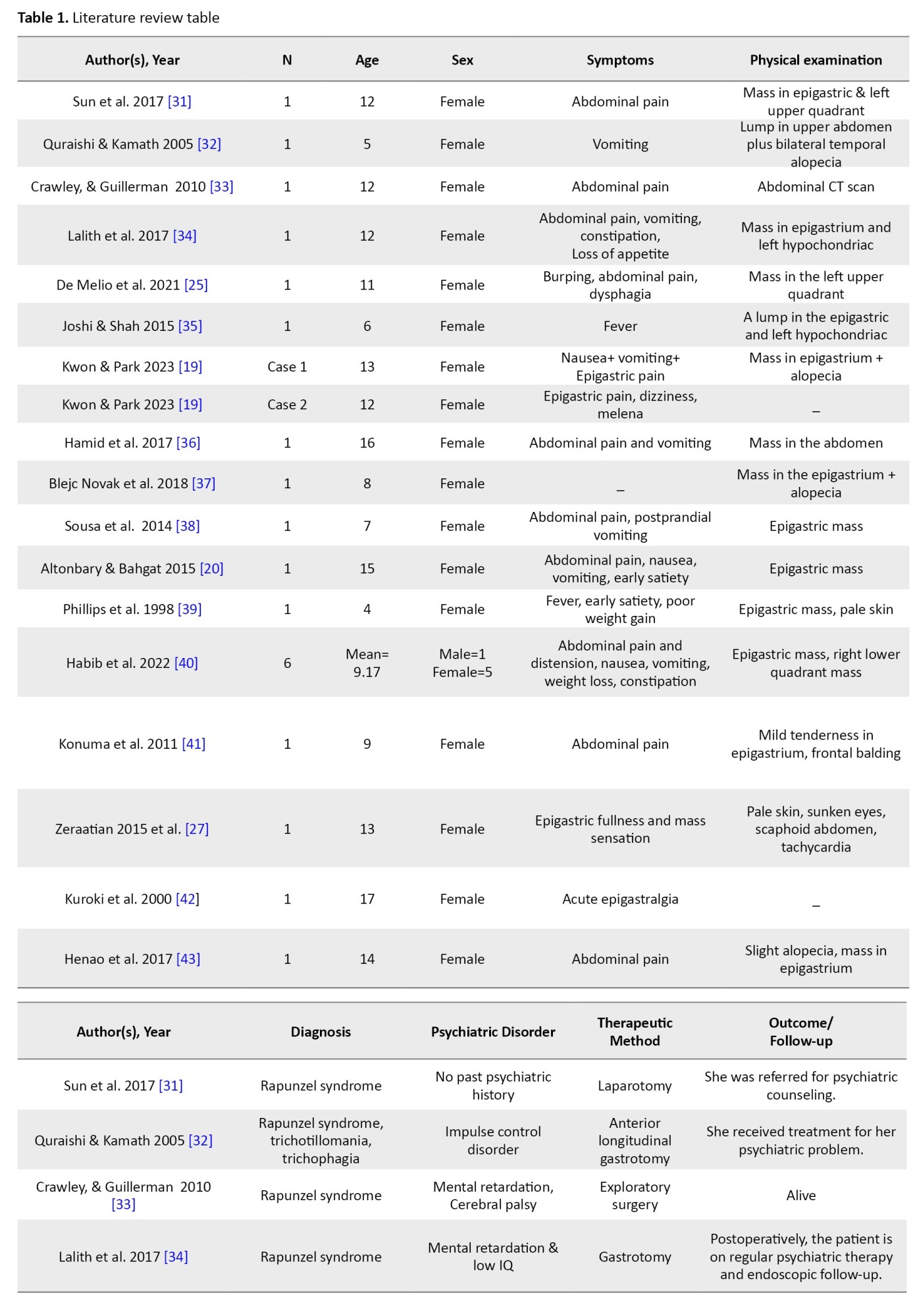
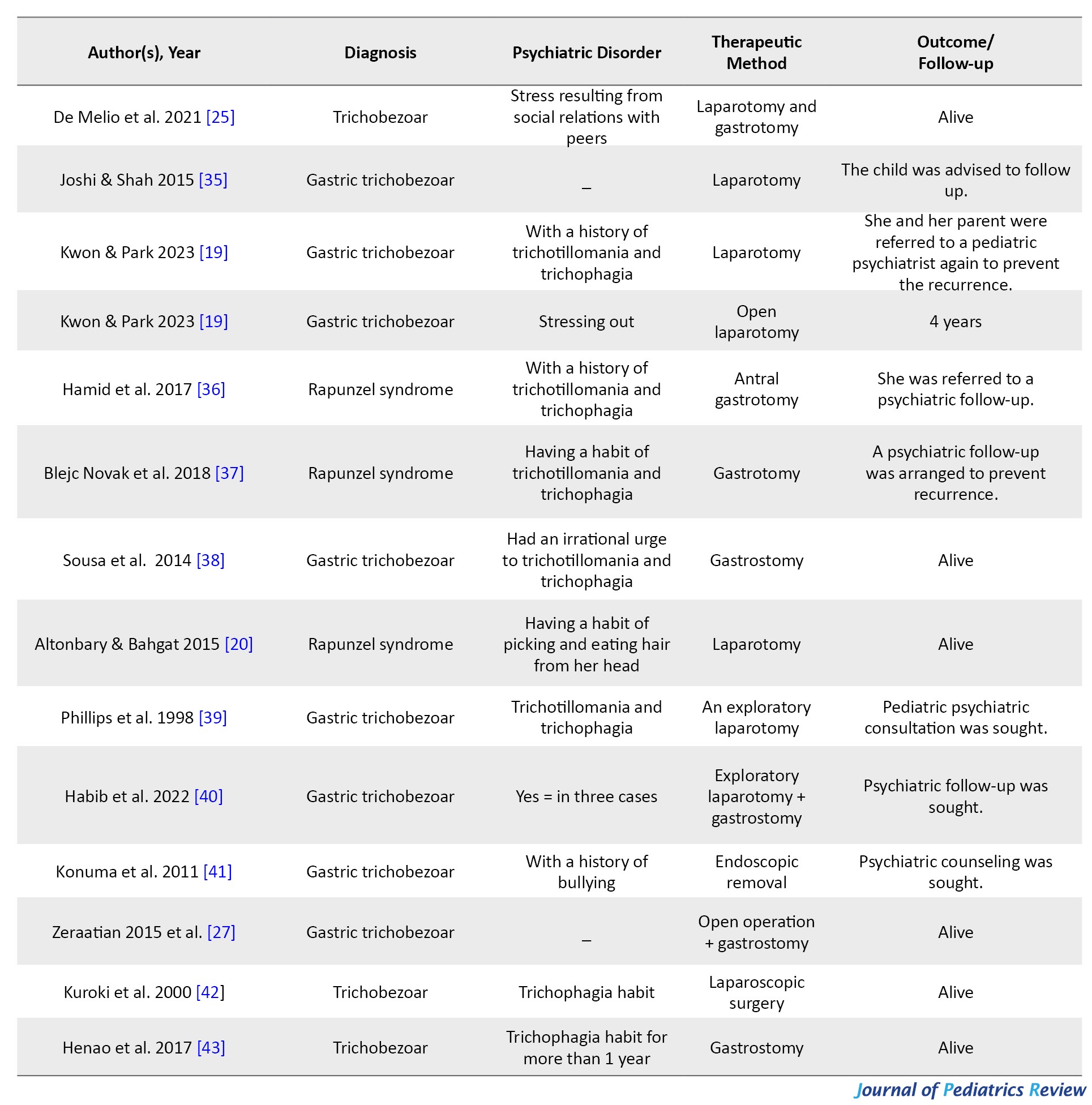
This case report focuses on the clinical management of a 12-year-old child with untreated trichotillomania who developed a trichobezoar, highlighting the gastrointestinal symptoms, diagnostic techniques, and comprehensive treatment strategies employed. Additionally, we performed an extensive literature review using PubMed and Google Scholar without a time limit, utilizing MeSH terms such as “trichobezoar,” “bezoar,” and “pediatrics,” along with AND and OR operators. Our review included articles documenting cases of trichobezoar in children to enhance our understanding of its management (Table 1).
Bezoars are a concretion and accumulation of indigested or foreign materials in the gastrointestinal tract, and they are usually classified into phytobezoar, pharmacobezoar, trichobezoar, and lactobezoar [6, 10, 15, 16]. The accumulation and impaction of indigested hairs, food, and mucus in the stomach is called gastric trichobezoar and mostly affects females between 13 and 20 years of age [17-19]. In this disease, the swallowed hair remains in the stomach fold due to escaping peristaltic propulsion, and it assumes the shape of the stomach [6]. When the tail of the trichobezoar extends into the small intestine (duodenum, jejunum, and ileum) or to the colon, it is called Rapunzel syndrome [6, 20].
In this disease, patients usually have previous psychiatric diseases such as trichotillomania (hair pulling) and trichophagia (hair eating), and they might be with mental retardation and psychological problems [19, 21, 22]. Trichotillomania is a psychosomatic disorder in which the irresistible urge to pull out one’s hair causes significant hair loss and functional impairment. In this disorder, the patient feels calm and safe by pulling their hair from the head and other body parts. This condition is a habit disorder in children and has a better prognosis than trichotillomania in adults [23, 24]. Besides the patient’s hair, wigs, doll’s hair, and blankets are the other sources of trichobezoar hair [19].
The symptoms of trichobezoar range from none to severe, depending on the degree of obstruction [22, 25]. The complications include asymptomatic or chronic recurrent abdominal pain, nausea, vomiting, loss of appetite, and weight loss. Gastric perfusion is rare in this disease, but erosive gastritis, esophagitis, and ulcerations that lead to bleeding and/or perfusion are also trichobezoar complications [26, 27]. During the physical examination, a lump may be palpated in the epigastrium, and alopecia may be present [28].
Ultrasound, plain film, upper gastrointestinal tract endoscopy, and CT scan are diagnostic methods for trichobezoar. CT scan is a more accessible evaluation method, but the final diagnosis and gold standard is upper gastrointestinal endoscopy due to the direct view of trichobezoar [19, 28, 29].
In general, managing and treating trichobezoar includes removing the mass and dealing with the underlying psychiatric and physical causes to prevent the recurrence [6]. Trichobezoar can be treated by laparoscopy, laparotomy, or endoscopy. Endoscopic removal can only be effective for small trichobezoars, and repeated treatment attempts can lead to esophageal perforation, esophagitis, or pressure ulcers [22]. According to the study conducted by Gorter et al., the success rate of endoscopic treatment is 5%, laparoscopy is 75%, and laparotomy with a 100% success rate in trichobezoar treatment is the preferred treatment option for patients [9]. Follow-up and psychiatric treatment of patients is necessary to prevent and decrease recurrence [30].
Ethical Considerations
Compliance with ethical guidelines
Permission was obtained from the child’s parents to publish the current case report and any associated photographs. This article adheres to all relevant ethical principles. The patient and her parents have provided written informed consent for disseminating this manuscript and collecting images.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
References
Trichobezoars, which are hairballs formed from ingested hair, represent a unique and often overlooked clinical entity, particularly in pediatric populations [1, 2]. These gastrointestinal obstructions are commonly associated with trichotillomania, a psychiatric disorder characterized by the compulsive pulling out of one’s hair, often accompanied by trichophagia or the ingestion of hair [3]. The prevalence of trichobezoar is notably higher in young females, [4] with studies indicating that they can lead to significant gastrointestinal complications if left untreated, including obstruction, perforation [4, 5], and even life-threatening conditions such as Rapunzel syndrome, where a long tail of hair extends into the intestines [6].
The clinical presentation of trichobezoars can be diverse, often mimicking other gastrointestinal disorders. Common symptoms include abdominal pain, nausea, vomiting, and changes in bowel habits. In some cases, patients may present with more severe complications, such as bowel obstruction or jaundice due to biliary obstruction caused by large trichobezoars [5, 6, 7, 8]. A literature review reveals that managing trichobezoars typically involves a combination of surgical intervention and psychiatric support [9]. Diagnostic modalities such as abdominal ultrasound, computed tomography (CT), and endoscopy are crucial for accurately identifying trichobezoars, allowing for timely surgical intervention when necessary [10, 11]. In addressing the psychological aspects of trichotillomania and trichophagia, it is essential to recognize the interplay between psychiatric disorders and gastrointestinal manifestations. Therefore, the management of trichobezoars must extend beyond surgical intervention to include comprehensive psychiatric care [12-14].
In this case report, we present the clinical management of a 12-year-old child with untreated trichotillomania who developed a trichobezoar, describing the gastrointestinal signs and symptoms, diagnostic methods employed, surgical interventions, and the multifaceted treatment approach. In addition, we will review the published literature to provide an up-to-date review of trichobezoar management in children.
Case Presentation
A 12-year-old girl was brought to the Emergency Department of Bou-Ali Sina Hospital in Sari City, Mazandaran Province, Iran, with persistent nausea, vomiting, and abdominal pain that had intensified over the past 20 days. The vomiting was non-bilious and non-bloody, primarily occurring in the mornings. The abdominal pain worsened with solid foods, was not positional, did not radiate, and had no relation to bowel movements. The patient’s history included dietary changes, significant weight loss of about 5 kg over the past month, melena, anorexia, dysphagia, odynophagia, and fever. There was no personal or family history of peptic ulcers, dyspnea, diarrhea, or constipation. However, the family history revealed a grandfather with gastric cancer and a father with obsessive behaviors. Vital signs were stable (temperature: 37 °C, blood pressure: 90/60 mm Hg, heart rate: 100 bpm, respiratory rate: 22 breaths/min), and the patient appeared generally healthy despite her symptoms. Notably, she had been pulling and eating her hair for 4 years. Physical examination revealed normal bowel sounds and a tender, non-mobile mass measuring 13×22 cm from the upper to lower abdomen. Dullness on percussion in the upper abdomen suggested a large mass in the anatomical area of the stomach. Hepatomegaly or splenomegaly was absent. The patient exhibited patchy hair loss on her scalp with varying lengths distributed across normal-appearing skin. Laboratory tests showed normal white blood cell counts and hemoglobin levels. However, elevated urea (28 mg/dL), lactate dehydrogenase (370 u/L), alkaline phosphatase (483 u/L), and an elevated erythrocyte sedimentation rate (27 mm/h) indicated possible underlying gastrointestinal pathology. Imaging studies prior to surgery revealed no pathological lesions on chest x-ray. An abdominal ultrasound showed a mass with echogenic margins measuring 109 mm in the upper abdomen, possibly indicating a space-occupying lesion such as a bezoar. An erect abdominal x-ray demonstrated a heterogeneous shadow under the gastric air bubble. Non-contrast CT imaging revealed a distended stomach containing a sizeable heterogeneous mass lesion, almost filling the lumen with internal dense foci (Figure 1). Management involved laparotomy and removal of an abdominal trichobezoar under general anesthesia. A midline incision revealed an enlarged stomach with thickened walls. A longitudinal incision allowed for the removal of the trichobezoar measuring approximately 30 cm in length and weighing 1088 g—a mass entirely composed of hair (Figure 1). Pathology confirmed an intragastric mass (trichobezoar) measuring 2×13×5.4 cm. A psychiatric consultation indicated that the patient had been suffering from trichotillomania for 4 years without treatment. Considering these findings and her history, a diagnosis of trichobezoar was established. After discharge, she was referred for continued psychiatric treatment to address her underlying condition.
Discussion
This case report focuses on the clinical management of a 12-year-old child with untreated trichotillomania who developed a trichobezoar, highlighting the gastrointestinal symptoms, diagnostic techniques, and comprehensive treatment strategies employed. Additionally, we performed an extensive literature review using PubMed and Google Scholar without a time limit, utilizing MeSH terms such as “trichobezoar,” “bezoar,” and “pediatrics,” along with AND and OR operators. Our review included articles documenting cases of trichobezoar in children to enhance our understanding of its management (Table 1).
Bezoars are a concretion and accumulation of indigested or foreign materials in the gastrointestinal tract, and they are usually classified into phytobezoar, pharmacobezoar, trichobezoar, and lactobezoar [6, 10, 15, 16]. The accumulation and impaction of indigested hairs, food, and mucus in the stomach is called gastric trichobezoar and mostly affects females between 13 and 20 years of age [17-19]. In this disease, the swallowed hair remains in the stomach fold due to escaping peristaltic propulsion, and it assumes the shape of the stomach [6]. When the tail of the trichobezoar extends into the small intestine (duodenum, jejunum, and ileum) or to the colon, it is called Rapunzel syndrome [6, 20].
In this disease, patients usually have previous psychiatric diseases such as trichotillomania (hair pulling) and trichophagia (hair eating), and they might be with mental retardation and psychological problems [19, 21, 22]. Trichotillomania is a psychosomatic disorder in which the irresistible urge to pull out one’s hair causes significant hair loss and functional impairment. In this disorder, the patient feels calm and safe by pulling their hair from the head and other body parts. This condition is a habit disorder in children and has a better prognosis than trichotillomania in adults [23, 24]. Besides the patient’s hair, wigs, doll’s hair, and blankets are the other sources of trichobezoar hair [19].
The symptoms of trichobezoar range from none to severe, depending on the degree of obstruction [22, 25]. The complications include asymptomatic or chronic recurrent abdominal pain, nausea, vomiting, loss of appetite, and weight loss. Gastric perfusion is rare in this disease, but erosive gastritis, esophagitis, and ulcerations that lead to bleeding and/or perfusion are also trichobezoar complications [26, 27]. During the physical examination, a lump may be palpated in the epigastrium, and alopecia may be present [28].
Ultrasound, plain film, upper gastrointestinal tract endoscopy, and CT scan are diagnostic methods for trichobezoar. CT scan is a more accessible evaluation method, but the final diagnosis and gold standard is upper gastrointestinal endoscopy due to the direct view of trichobezoar [19, 28, 29].
In general, managing and treating trichobezoar includes removing the mass and dealing with the underlying psychiatric and physical causes to prevent the recurrence [6]. Trichobezoar can be treated by laparoscopy, laparotomy, or endoscopy. Endoscopic removal can only be effective for small trichobezoars, and repeated treatment attempts can lead to esophageal perforation, esophagitis, or pressure ulcers [22]. According to the study conducted by Gorter et al., the success rate of endoscopic treatment is 5%, laparoscopy is 75%, and laparotomy with a 100% success rate in trichobezoar treatment is the preferred treatment option for patients [9]. Follow-up and psychiatric treatment of patients is necessary to prevent and decrease recurrence [30].
Ethical Considerations
Compliance with ethical guidelines
Permission was obtained from the child’s parents to publish the current case report and any associated photographs. This article adheres to all relevant ethical principles. The patient and her parents have provided written informed consent for disseminating this manuscript and collecting images.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
References
- Liang Y, Huang L, Wang D, Liu T, Li X, Wang W, et al. Rapunzel syndrome in children: A retrospective review of ten cases combined with literature review in a tertiary referral center. Pediatr Surg Int. 2024; 40(1):121. [DOI:10.1007/s00383-024-05705-0] [PMID]
- Vaughan ED Jr, Sawyers JL, Scott HW Jr. The rapunzel syndrome. An unusual complication of intestinal bezoar. Surgery. 1968; 63(2):339-43. [PMID]
- Snorrason I, Ricketts EJ, Stein AT, Björgvinsson T. Trichophagia and trichobezoar in trichotillomania: A narrative mini-review with clinical recommendations. J Obsessive-Compuls Relat Disord. 2021; 31:100680. [DOI:10.1016/j.jocrd.2021.100680]
- Snorrason I, Ricketts EJ, Stein AT, Thamrin H, Lee SJ, Goldberg H, et al. Sex Differences in Age at Onset and Presentation of Trichotillomania and Trichobezoar: A 120-year systematic review of cases. Child Psychiatry Hum Dev. 2022; 53(1):165-71. [DOI:10.1007/s10578-020-01117-y] [PMID]
- Mirza MB, Talat N, Saleem M. Gastrointestinal trichobezoar: An experience with 17 cases. J Pediatr Surg. 2020; 55(11):2504-9. [DOI:10.1016/j.jpedsurg.2020.04.020] [PMID]
- Gonuguntla V, Joshi DD. Rapunzel syndrome: A comprehensive review of an unusual case of trichobezoar. Clin Med Res. 2009; 7(3):99-102. [DOI:10.3121/cmr.2009.822] [PMID]
- Paschos KA, Chatzigeorgiadis A. Surgical and endoscopic treatment of a double phytobezoar causing ileus and jaundice: A case report. Iran J Med Sci. 2019; 44(1):70-3. [PMID]
- Verma A, Sharma S, Tyagi G, Singh S. Huge trichobezoar causing obstructive jaundice. BMJ Case Rep. 2014; 2014:bcr2013201667. [DOI:10.1136/bcr-2013-201667] [PMID]
- Gorter RR, Kneepkens CM, Mattens EC, Aronson DC, Heij HA. Management of trichobezoar: Case report and literature review. Pediatr Surg Int. 2010; 26(5):457-63. [DOI:10.1007/s00383-010-2570-0] [PMID]
- Paschos KA, Chatzigeorgiadis A. Pathophysiological and clinical aspects of the diagnosis and treatment of bezoars. Ann Gastroenterol. 2019; 32(3):1-9. [DOI:10.20524/aog.2019.0370]
- Taylor JE, Clegg D. Foreign bodies and bowel obstructions. In: Victorovich Garbuzenko D, editor. Intestinal Obstructions. London: IntechOpen; 2020. [Link]
- Farhat LC, Olfson E, Nasir M, Levine JLS, Li F, Miguel EC,et al. Pharmacological and behavioral treatment for trichotillomania: An updated systematic review with meta-analysis. Depress Anxiety. 2020; 37(8):715-27. [DOI:10.1002/da.23028] [PMID]
- Sabra MAA, Kalaldeh MA, Alnaeem MM, Zyoud AH. The efficacy of using psychotherapy interventions to minimize symptoms of trichotillomania and trichophagia: A scoping review. J Contemp Psychother. 2024; 54(2):143-54. [DOI:10.1007/s10879-023-09604-8]
- Slikboer R, Nedeljkovic M, Bowe SJ, Moulding R. A systematic review and meta-analysis of behaviourally based psychological interventions and pharmacological interventions for trichotillomania. Clin Psychol. 2017; 21(1):20-32. [DOI:10.1111/cp.12074]
- Andrus CH, Ponsky JL. Bezoars: Classification, pathophysiology, and treatment. Am J Gastroenterol. 1988; 83(5):476-8.[Link]
- Espinoza González R. [Gastrointestinal bezoars (Spanish)]. Rev Med Chil. 2016; 144(8):1073-7. [PMID]
- Ahmed MM, Tahir KS, Gubari MIM, Rasul RHK, Rashid MJ, Abdul Aziz JM. Large trichobezoar associated with misdiagnosis, a rare case report with a brief literature review. Int J Surg Case Rep. 2021; 88:106551. [DOI:10.1016/j.ijscr.2021.106551] [PMID]
- Huaco Aranguri AA, Orduña Carpio RA, Ortiz Castro C, Delgado Gonzales M, Haito Chávez Y. [Gastric trichobezoar: Case report and literature review (Spanish)]. Rev Gastroenterol Peru. 2022; 42(3):193-8. [DOI:10.47892/rgp.2022.423.1343]
- Kwon HJ, Park J. Treatment of large gastric trichobezoar in children: Two case reports and literature review. Medicine (Baltimore). 2023; 102(16):e33589. [DOI:10.1097/MD.0000000000033589] [PMID]
- Altonbary AY, Bahgat MH. Rapunzel syndrome. J Transl Int Med. 2015; 3(2):79-81. [DOI:10.1515/jtim-2015-0008] [PMID]
- Harrabi F, Ammar H, Ben Latifa M, Gupta R, Ben Ali A. Gastric trichobezoar causing gastrointestinal bleeding: A case report. Cureus. 2022; 14(10):e30282. [DOI:10.7759/cureus.30282]
- Al-Osail EM, Zakary NY, Abdelhadi Y. Best management modality of trichobezoar: A case report. Int J Surg Case Rep. 2018; 53:458-60. [DOI:10.1016/j.ijscr.2018.11.030] [PMID]
- Sehgal VN, Srivastava G.Trichotillomania +/- trichobezoar: Revisited. J Eur Acad Dermatol Venereol. 2006; 20(8):911-5. [DOI:10.1111/j.1468-3083.2006.01590.x] [PMID]
- Grant JE, Chamberlain SR. Trichotillomania. Am J Psychiatry. 2016; 173(9):868-74. [DOI:10.1176/appi.ajp.2016.15111432] [PMID]
- De Melio J, Debrouwere T, Herman M. Trichobezoar. J Belg Soc Radiol. 2021; 105(1):31. [DOI:10.5334/jbsr.2478] [PMID]
- Daoud R, Tlili A, Fendri S, Akrout A, Trigui A, Boujelbene S. Gastric trichobezoar: An uncommon cause of epigastric pain: A case report. Clin Case Rep. 2022; 10(4):e05653. [DOI:10.1002/ccr3.5653] [PMID]
- Zeraatian S, Ameri S, Tabesh H, Kamalzadeh N. Uncommon presentation of gastric trichobezoar: A case report. Iran J Public Health. 2015; 44(7):1008-11. [PMID]
- Sanneerappa PB, Hayes HM, Daly E, na Moodley V. Trichobezoar: A diagnosis which is hard to swallow and harder to digest. BMJ Case Rep. 2014; 2014:bcr2013201569. [DOI:10.1136/bcr-2013-201569] [PMID]
- Nettikadan A, Ravi MJ, Shivaprasad M. Recurrent rapunzel syndrome - A rare tale of a hairy tail. Int J Surg Case Rep. 2018; 45:83-6. [DOI:10.1016/j.ijscr.2018.03.017] [PMID]
- Haggui B, Hidouri S, Ksia A, Oumaya M, Mosbahi S, Messaoud M, et al. Management of trichobezoar: About 6 cases. Afr J Paediatr Surg. 2022; 19(2):102-4. [DOI:10.4103/ajps.AJPS_110_20] [PMID]
- Sun ZN, Hu DL, Chen ZM. Trichobezoar and rapunzel syndrome. World J Pediatr. 2017; 13(1):91. [DOI:10.1007/s12519-016-0055-5] [PMID]
- Quraishi AH, Kamath BS. Rapunzel syndrome. Gastrointest Endosc. 2005; 62(4):611. [DOI:10.1016/S0016-5107(05)01579-8] [PMID]
- Crawley AJ, Guillerman RP. Rapunzel syndrome. Pediatr Radiol. 2010; 40(Suppl 1):S100. [DOI:10.1007/s00247-010-1864-7] [PMID]
- Lalith S, Gopalakrishnan KL, Ilangovan G, Jayajothi A. Rapunzel Syndrome. J Clin Diagn Res. 2017; 11(9):TD01-2. [DOI:10.7860/JCDR/2017/28593.10594] [PMID]
- Joshi N, Shah R. Gastric trichobezoar in a 6-year old girl. APSP J Case Rep. 2015; 6(1):8. [PMID]
- Hamid M, Chaoui Y, Mountasser M, Sabbah F, Raiss M, Hrora A, et al. Giant gastric trichobezoar in a young female with Rapunzel syndrome: Case report. Pan Afr Med J. 2017; 27:252. [DOI:10.11604/pamj.2017.27.252.9110] [PMID]
- Blejc Novak A, Zupančič Ž, Plut D, Gvardijančič D, Homan M. Rapunzel syndrome: A rare form of trichobezoar in the stomach with some extension into the small intestine. Acta Dermatovenerol Alp Pannonica Adriat. 2018; 27(3):155-7. [DOI:10.15570/actaapa.2018.32] [PMID]
- Sousa MC, Alves N, Herédia V. Gastric trichobezoar in a pediatric patient. Acta Med Port. 2014; 27(5):665.[DOI:10.20344/amp.4904] [PMID]
- Phillips MR, Zaheer S, Drugas GT. Gastric trichobezoar: Case report and literature review. Mayo Clin Proc. 1998; 73(7):653-6. [PMID]
- Habib M, Amjad MB, Abbas M, Chaudhary MA. Gastric Trichobezoars in paediatric population- A series of six cases and literature review. Ann Med Surg (Lond). 2022; 84:104906. [DOI:10.1016/j.amsu.2022.104906] [PMID]
- Konuma H, Fu K, Morimoto T, Shimizu T, Izumi Y, Shiyanagi S, et al. Endoscopic retrieval of a gastric trichobezoar. World J Gastrointest Endosc. 2011; 3(1):20-2. [DOI:10.4253/wjge.v3.i1.20] [PMID]
- Kuroki Y, Otagiri Sh, Sakamoto T, Tsukada K, Tanaka M. Case report of trichobezoar causing gastric perforation. Digestive Endosc 2000; 12(2):181-5. [DOI:10.1046/j.1443-1661.2000.00023.x]
- Henao AM, Medina MC, Reyes F, Uriza LF. [Gastric trichobezoar: Presentation of a case (Spanish)]. Rev. Colomb. Radiol. [online journal]. 2017;28(3):4486-91. [Link]
Type of Study: Case Report and Review of Literature |
Subject:
Pediatric Gastroenterology
Received: 2024/11/9 | Accepted: 2024/12/14 | Published: 2025/01/21
Received: 2024/11/9 | Accepted: 2024/12/14 | Published: 2025/01/21
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |