Volume 13, Issue 1 (1-2025)
J. Pediatr. Rev 2025, 13(1): 87-94 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Pournasiri Z, Mirmohammadkhani M, Pourpashang P. Validity of the Ultrasonography Findings for Screening Vesicoureteral Reflux in Children With Urinary Tract Infection. J. Pediatr. Rev 2025; 13 (1) :87-94
URL: http://jpr.mazums.ac.ir/article-1-710-en.html
URL: http://jpr.mazums.ac.ir/article-1-710-en.html
1- Pediatric Nephrology Research Center, Research Institute for Children’s Health, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Social Determinants of Health Research Center, Semnan University of Medical Sciences, Semnan, Iran.
3- Department of Pediatric Nephrology, School of Medicine, Bahrami Hospital, Tehran University of Medical Sciences, Tehran, Iran. & Pediatric Chronic Kidney Disease Research Center, Gene, Cell & Tissue Research Institute, Tehran University of Medical Sciences, Tehran, Iran. ,paaniz.p@gmail.com
2- Social Determinants of Health Research Center, Semnan University of Medical Sciences, Semnan, Iran.
3- Department of Pediatric Nephrology, School of Medicine, Bahrami Hospital, Tehran University of Medical Sciences, Tehran, Iran. & Pediatric Chronic Kidney Disease Research Center, Gene, Cell & Tissue Research Institute, Tehran University of Medical Sciences, Tehran, Iran. ,
Keywords: Sensitivity, Specificity, Voiding cystourethrography (VCUG), Vesicoureteral reflux, Ultrasound
Full-Text [PDF 384 kb]
(832 Downloads)
| Abstract (HTML) (1830 Views)
Full-Text: (555 Views)
Introduction
Urinary tract infection (UTI) is one of the most common bacterial infections in children. UTI usually occurs when bacteria migrate up the ureter into the urethra. Infection may occur anywhere from the urethra to the renal parenchyma [1]. Vesicoureteral reflux (VUR) is the retrograde urine flow from the bladder into the upper urinary tract, usually occurring during voiding [2]. VUR is associated with frequent UTIs, scarring of the renal cortex, and permanent kidney damage, especially in children. It is the most common neonatal urologic abnormality, occurring in approximately 1% of infants and up to 15% of children born with prenatal hydronephrosis [3, 4].
VUR is often discovered during the initial evaluation of UTI. However, the prevalence of VUR in children with UTI varies among different races and groups. VUR prevalence is 10% to 51.4% of children with the first UTI episode, with the lowest prevalence in black children [5, 6, 7].
VUR has some complications. Studies have shown that at the time of diagnosis, 30% to 54% of children with VUR have renal parenchymal scarring [5, 8]. High-grade VUR and recurrent pyelonephritis are considered the most important risk factors for renal scarring in children. In addition, gender differences in the development of renal parenchymal damage have been reported, with severe bilateral VUR being more common in boys. Girls are usually first diagnosed at an older age, and their VUR is often less severe, but girls are more prone to the occurrence of recurrent UTIs [9, 10].
The gold standard diagnostic procedure for assessing VUR in children is voiding cystourethrography (VCUG). This exam provides accurate anatomic imaging, detects bladder diverticula, identifies ureteral duplication, demonstrates the extent of bladder wall trabeculation, and facilitates VUR grading. However, performing VCUG in infants and young children requires specialized knowledge to minimize psychological and physical damage and reduce radiation exposure [11-13].
Radionuclide cystography (RNC) is an alternative, sensitive method that lacks spatial resolution. Many efforts have been made to use ultrasonography (US) to diagnose VUR and eliminate radiation exposure. Kidney US is recommended for initial and follow-up evaluations to evaluate kidney anatomy, cortical thickness, presence of hydronephrosis, and any structural abnormalities. Unfortunately, US lacks high sensitivity or specificity for diagnosing high-grade VUR. So far, limited studies have evaluated the sensitivity of US for diagnosing VUR. Therefore, this study evaluated the US findings in children with UTIs with and without VUR.
Methods
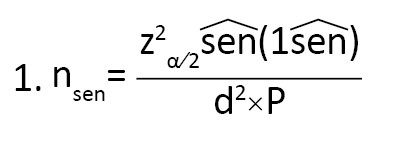
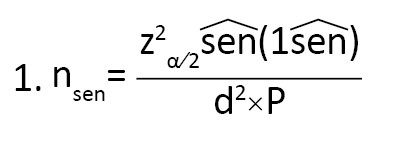
Data on 183 children with UTI in Loghman Hakim and Mofid hospitals, Tehran City, Iran, in 2024 was examined in this cross-sectional study. They had a US with or without VUR based on VCUG or RNC. The urine sample was taken midstream from children younger than 18 diagnosed with UTI. In the non-toilet-trained children, the urine sample was first collected using a urinary bag. If the urine sample was positive, the sample was retaken (as sterile) by a urinary catheter or suprapubic method. The selection of samples in this study was carried out using a convenience sampling approach. The samples were recruited from patients who underwent medical examination in the two above-mentioned hospitals for one year, from the beginning of October 2023 to the end of September 2024. All eligible samples were enrolled in the study according to the inclusion criteria. The exclusion criteria were failure to perform the VCUG or RNC due to lack of indication or parental consent to perform the procedures. Given the available scientific evidence that US has a sensitivity of at least 60% in diagnosing VUR (P=0.6), and with the hypothesis that US as a good method may have an acceptable level of diagnostic value in terms of sensitivity (i.e. a of 80%), the minimum sample size required for this study was estimated to be 160 people using the Equation 1 with α=0.05 and d=0.1 (d=0.08):
In examining urine culture results in the midstream sample, the growth of more than 50000 colonies of an organism, one colony in the suprapubic sample, or more than 1000 colonies in the urine culture catheter sample was considered positive. The US of the kidneys, urinary tract, and bladder was performed for all children with a UTI. Also, VCUG or RNC was performed for the patients if there was an indication. According to the guidelines, the indications include children under 2 years or 2-3 years of age who have febrile UTI, especially if it is recurrent or accompanied by US abnormalities or fetal anomalies. Patients who are involved with overactive bladder or have recurrent UTI or their urine cultures are reported to contain atypical microbes [14].
Statistical analysis
In this study, frequency distribution statistics were used to describe qualitative variables, and Mean±SD and range (minimum and maximum values) were used to report and describe the age, the only numerical variable. Sensitivity and specificity were calculated to investigate the US diagnostic value in determining VUR. Kappa statistic was used to examine the agreement between the two methods. Cohen suggested the kappa result be interpreted as follows: Values ≤0 are interpreted as no agreement; 0.01–0.20 as none to slight; 0.21–0.40 as fair; 0.41– 0.60 as moderate; 0.61–0.80 as substantial; and 0.81–1.00 as almost perfect agreement. The chi-square test was used to compare proportions. SPSS software, version 20 was used for analyses, and P<0.05 were considered significant in all statistical tests.
Results
In this study, 183 children were assessed. Their Mean±SD age was 6.98±4.07 years (minimum 1 year and maximum 17 years); 119(65%) were girls, and 64(35%) were boys. Table 1 presents the findings of the right and left urinary tract anatomy, based on the US, separated by gender and side.
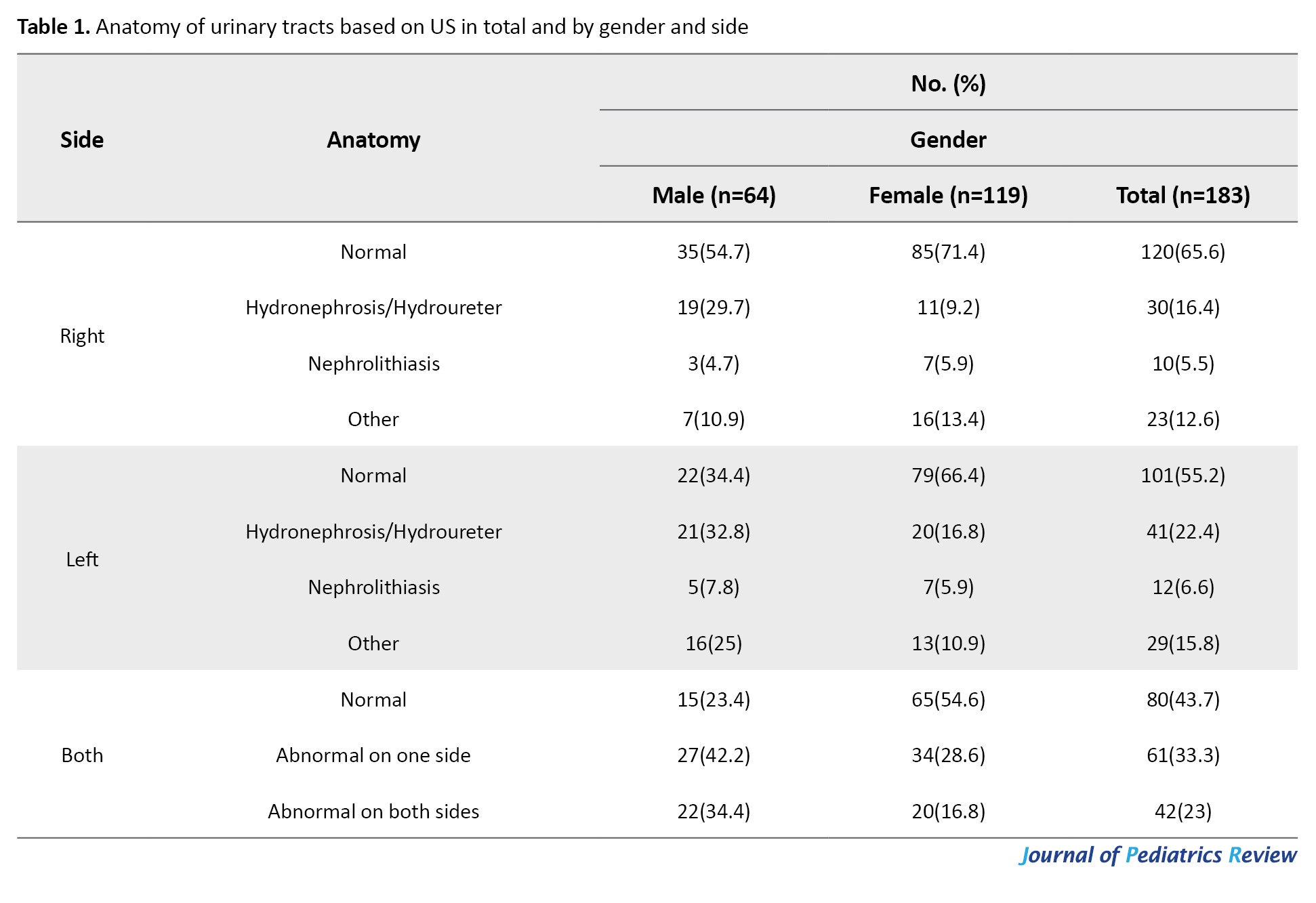
As seen in Table 1, out of the total 183 eligible children examined by US, 80(43.7%) were reported as normal, 63(34.4%), and 82(44.8%) were reported to have abnormalities in their right and left urinary systems, respectively. Also, 42 children (23%) had abnormalities in both sides.
VUR was assessed in 112 children (61.2%) using VCUG and 63(34.4%) using RNC, and both methods were used for only 8 children. In 8 patients who used both methods, the results of the two methods were in complete agreement in 6 patients, and there was a difference in results in only 2 patients, which, in the final analysis of the results, VCUG results were considered. Table 2 shows the status of VUR based on analysis of initial (first) VCUG/RNC results of urinary tracts by gender and side.
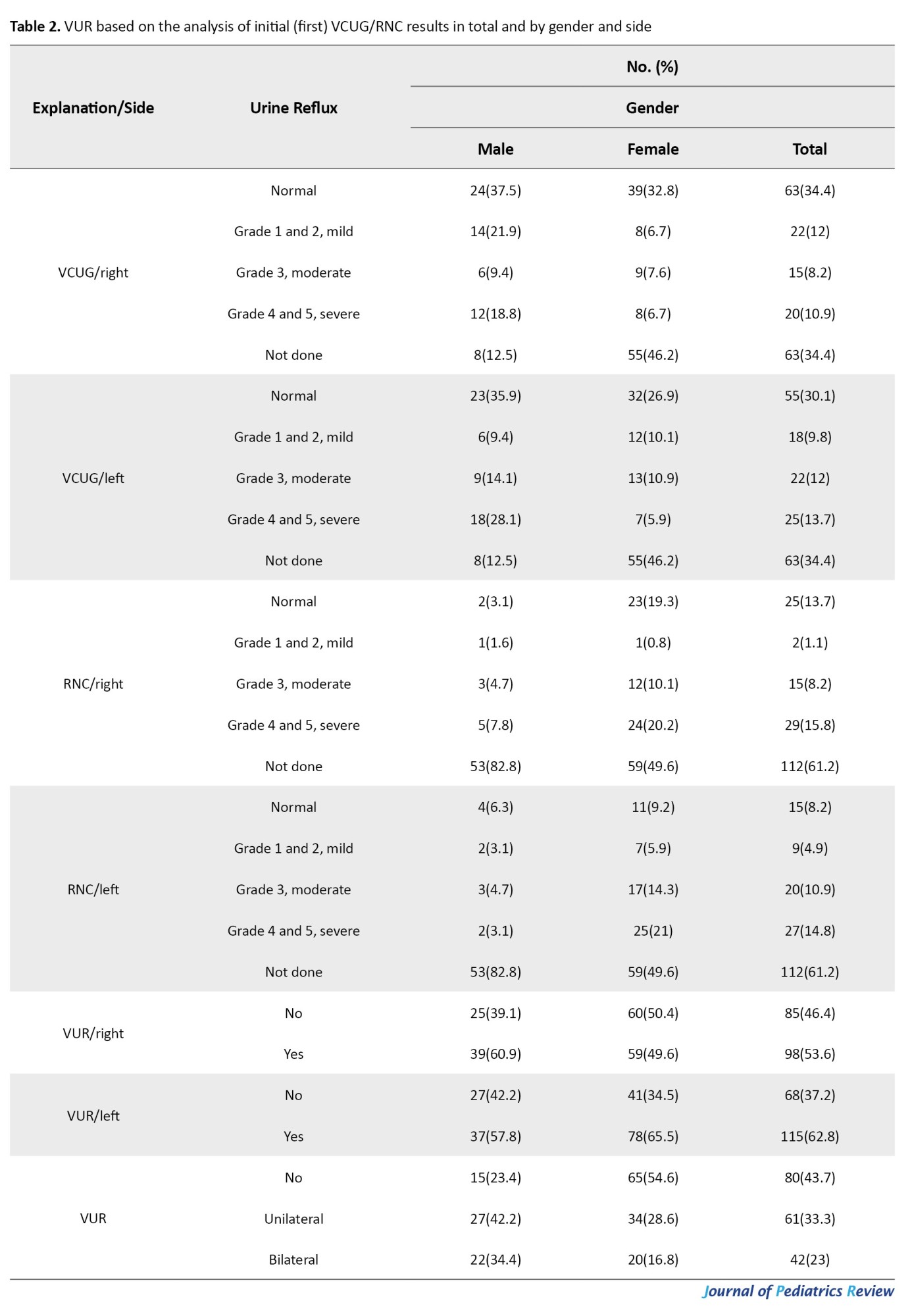
As seen in Table 2, 39 children(21.3%) did not have reflux, and the rest (144 children, 78.7%) had some degree of VUR, either unilateral or bilateral.
Table 3 shows the frequency distribution of the VUR diagnosis based on the results of VCUG/ RNC for normal and abnormal US findings.
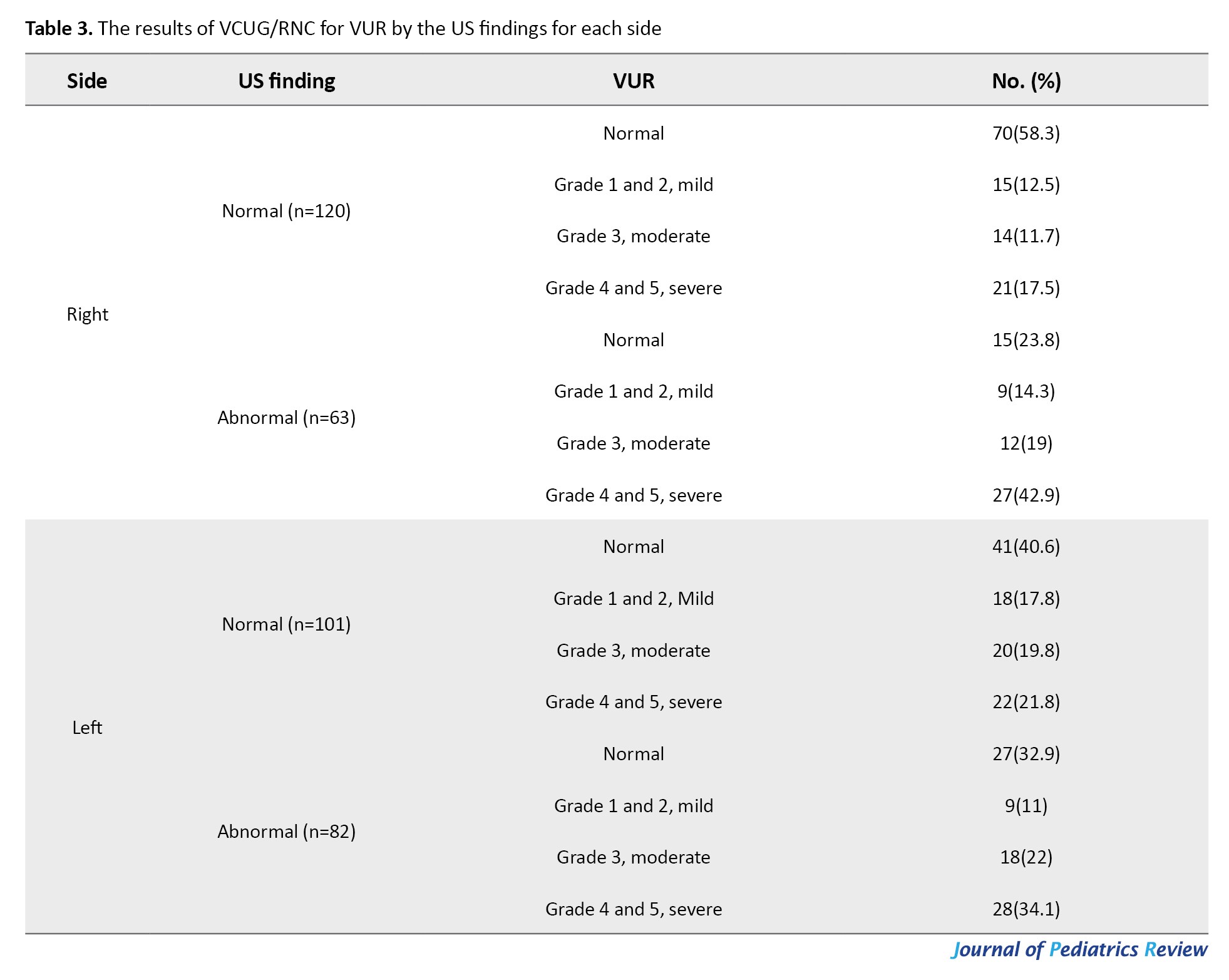
According to Table 3, 58.3% and 40.6% of normal reported US were reported normal for VUR. As the reflux grade increases, the percentage of US abnormalities increases (14.3% to 42.9%). However, as the grade decreases, the percentage of US normality decreases too (17.5% to 12.5%).
Table 4 shows the sensitivity and specificity of US findings for VUR diagnosis.
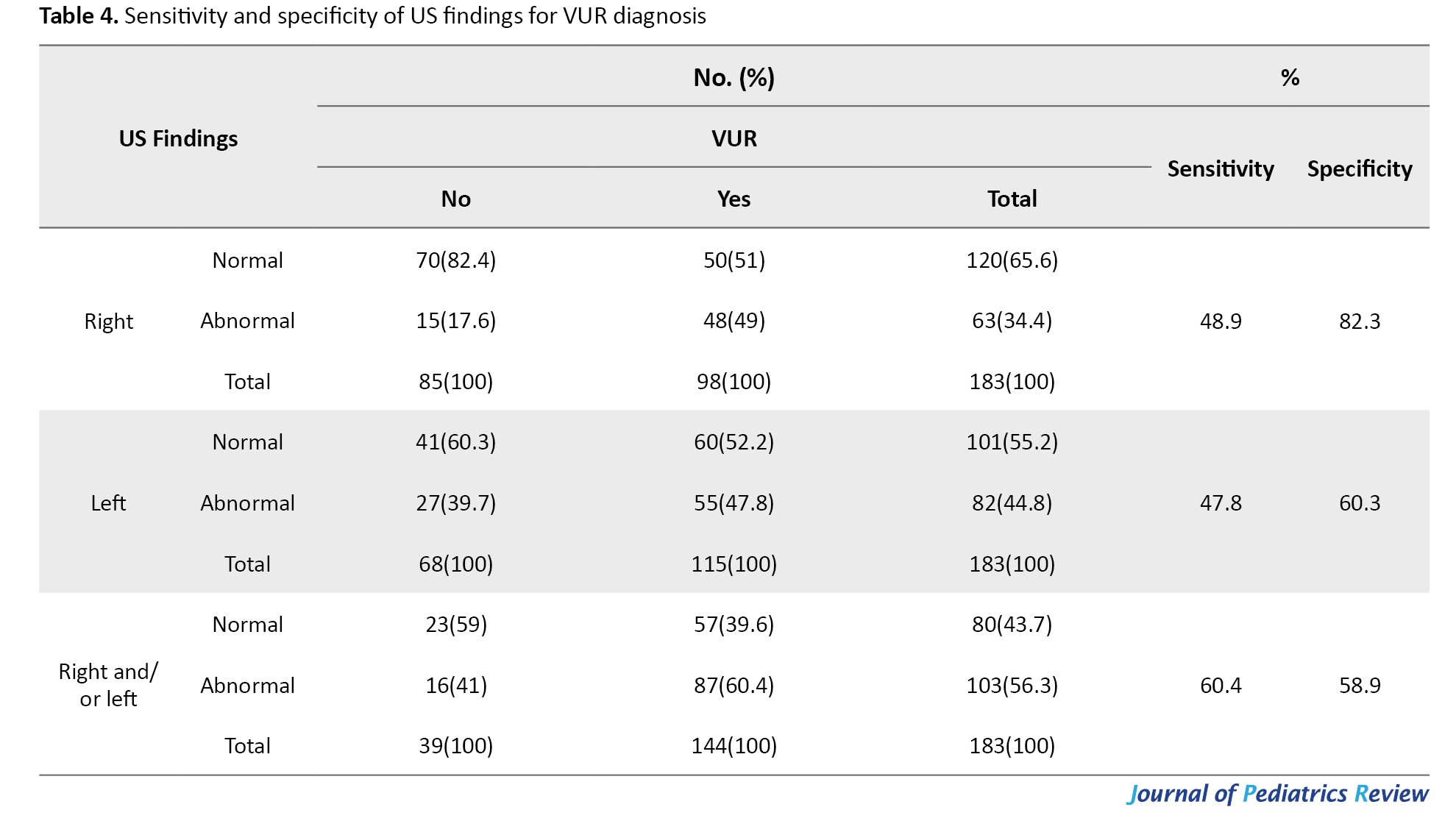
Based on Table 4, the sensitivity and specificity of the US for detecting VUR are 60.4% and 58.9%, respectively. The level of agreement between the two in terms of kappa statistic must be considered “none to slight” (k=0.14, P=0.003).
Discussion
Our findings show that the sensitivity and specificity of US for detecting VUR are 60.4% and 58.9%, respectively. Also, the agreement between the two methods (US vs gold standard VCUG/RNC) in terms of kappa statistic was calculated to be “none to slight” (k=0.14, P=0.003).
VUR may partially contribute to recurrent UTI in children. If not diagnosed in time, children’s normal growth and development may be affected. Currently, diagnostic techniques for VUR are continuously improved. Due to the characteristics of pediatrics, higher requirements for safety and accuracy of diagnosis are raised. VCUG is now widely used. However, repeated examination using VCUG is harmful to children’s health due to its significant radioactivity. RNC is a sensitive alternative method. However, its spatial resolution is not acceptable. In contrast, US stands out among many diagnostic methods due to its non-radioactive nature [15-17].
Studies have mentioned that US is effective in diagnosing diseases. However, for examination, it is necessary to take images of the urethra intermittently and continuously so the process of filling and excretion from the urethra cannot be observed accurately and in real-time. As a result, certain missing occurs. Due to the significant limitations of US showing the posterior urethra, the operator must pay more attention to the urinary system during voiding to see the structure of the urethra more clearly, which is a big problem [18].
Yang et al. evaluated the value and compatibility rate of urethral US in pediatric VUR. A total of 160 subjects were examined in their study. Among them, 56 cases had reflux; 46 renal ureteral units had reflux under both examination methods (28.75%), and 10 cases were detected only by US (6.25%). Thirty-four cases of VUR (42.50%) were diagnosed by US, of which 15 had bilateral reflux and 4 had unilateral reflux. Also, 25 cases (35.00%) were diagnosed by VCUG, of whom 10 cases had bilateral regurgitation and 5 had unilateral regurgitation. There was no significant difference in the rate of reflux detection between the two methods. A total of 146 diagnosed cases were consistent between the two methods (91.25%), and only 9.75% were not [19].
The current study shows that US does not match well with VCUG/ RNC for diagnosing VUR. Of course, in our study, the statistical difference between the two sets was not evaluated. Perhaps the reason for the difference between the results of the two studies was the sample size. In the present study, 183 children with VUR were examined, and in the study by Yang et al. [19], 56 children were examined with VUR, and the higher sample size was one of the advantages of the present study.
In Mane et al.’s study, 30 children were examined. Their mean age was 51.53 months. There were 21 boys and 9 girls. In VCUG, 16 patients did not have reflux, and 14 had reflux. Regarding the US, 14 patients did not have VUR, and 16 had VUR. Of 58 kidney-ureteral units (KUUs), VUR was diagnosed in 17 by VCUG and in 21 by US. Therefore, US identified 4 reflux units that were not seen on VCUG. In the right KUU, US detected VUR in 3 units without reflex on VCUG. In the 28 left KUU, 25 units in the US corresponded to the degree of VUR detected by VCUG. Two cases showed a VUR grade higher than the corresponding VCUG grade, and one had a lower grade. Regarding the US, 14 patients lacked VUR, and 16 had VUR. In total, US revealed 4 cases that VCUG did not detect them. This study concluded that US is a promising imaging modality compared to VCUG for evaluating pediatric ureteral reflux due to its superior diagnostic performance, feasibility, and radiation safety for children [20]. In the current study, it was seen that the US of the right urinary tract identified 83 cases as normal and 47 cases as abnormal, while these numbers for VCUG were 41 cases and 89 cases, respectively. Regarding the left kidney, it was also seen that the US diagnosed 78 cases as normal and 68 cases as abnormal, while VCUG diagnosed 45 cases as normal and 101 cases as abnormal, which, from this point of view, the present study was different from the study of Mane et al. Based on our findings, US does not seem to have a good diagnostic compatibility with VCUG.
Takahashi et al. compared the diagnostic compatibility of US with cystourethrography for diagnosing VUR. US failed to detect two cases of grade 1 VUR in adolescents, whereas it detected grade 4 VUR in one highly dilated renal-ureteral unit that was not detected on cystourethrography [21]. The results of our study are also in line with this study.
Conclusion
The current study shows that US does not match well with VCUG/ RNC for diagnosing VUR. The sensitivity and specificity of the US were 60.4% and 58.9%, respectively, which is not acceptable for a diagnostic test. The level of agreement between the two methods was significant, from “none to slight,” which was also not a good agreement. Thus, it can be said that US is not appropriate for diagnosing VUR and is not a good diagnostic method. Indeed, VCUG or RNC are preferable despite all their disadvantages. Although US is a cheap, accessible, and highly acceptable method for children and their families, its diagnostic compatibility with VCUG/RNC is not high, and if there is a suspicion of VUR, US may not be able to confirm it and VCUG/RNC should be used.
Ethical Considerations
Compliance with ethical guidelines
This research adhered to the principles outlined in the Declaration of Helsinki. For this study, the parents of the children consented to participate in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors express their gratitude for Mohammadamir Kakaee for his contribution and integrity in research and data gathering.
References
Urinary tract infection (UTI) is one of the most common bacterial infections in children. UTI usually occurs when bacteria migrate up the ureter into the urethra. Infection may occur anywhere from the urethra to the renal parenchyma [1]. Vesicoureteral reflux (VUR) is the retrograde urine flow from the bladder into the upper urinary tract, usually occurring during voiding [2]. VUR is associated with frequent UTIs, scarring of the renal cortex, and permanent kidney damage, especially in children. It is the most common neonatal urologic abnormality, occurring in approximately 1% of infants and up to 15% of children born with prenatal hydronephrosis [3, 4].
VUR is often discovered during the initial evaluation of UTI. However, the prevalence of VUR in children with UTI varies among different races and groups. VUR prevalence is 10% to 51.4% of children with the first UTI episode, with the lowest prevalence in black children [5, 6, 7].
VUR has some complications. Studies have shown that at the time of diagnosis, 30% to 54% of children with VUR have renal parenchymal scarring [5, 8]. High-grade VUR and recurrent pyelonephritis are considered the most important risk factors for renal scarring in children. In addition, gender differences in the development of renal parenchymal damage have been reported, with severe bilateral VUR being more common in boys. Girls are usually first diagnosed at an older age, and their VUR is often less severe, but girls are more prone to the occurrence of recurrent UTIs [9, 10].
The gold standard diagnostic procedure for assessing VUR in children is voiding cystourethrography (VCUG). This exam provides accurate anatomic imaging, detects bladder diverticula, identifies ureteral duplication, demonstrates the extent of bladder wall trabeculation, and facilitates VUR grading. However, performing VCUG in infants and young children requires specialized knowledge to minimize psychological and physical damage and reduce radiation exposure [11-13].
Radionuclide cystography (RNC) is an alternative, sensitive method that lacks spatial resolution. Many efforts have been made to use ultrasonography (US) to diagnose VUR and eliminate radiation exposure. Kidney US is recommended for initial and follow-up evaluations to evaluate kidney anatomy, cortical thickness, presence of hydronephrosis, and any structural abnormalities. Unfortunately, US lacks high sensitivity or specificity for diagnosing high-grade VUR. So far, limited studies have evaluated the sensitivity of US for diagnosing VUR. Therefore, this study evaluated the US findings in children with UTIs with and without VUR.
Methods
Data on 183 children with UTI in Loghman Hakim and Mofid hospitals, Tehran City, Iran, in 2024 was examined in this cross-sectional study. They had a US with or without VUR based on VCUG or RNC. The urine sample was taken midstream from children younger than 18 diagnosed with UTI. In the non-toilet-trained children, the urine sample was first collected using a urinary bag. If the urine sample was positive, the sample was retaken (as sterile) by a urinary catheter or suprapubic method. The selection of samples in this study was carried out using a convenience sampling approach. The samples were recruited from patients who underwent medical examination in the two above-mentioned hospitals for one year, from the beginning of October 2023 to the end of September 2024. All eligible samples were enrolled in the study according to the inclusion criteria. The exclusion criteria were failure to perform the VCUG or RNC due to lack of indication or parental consent to perform the procedures. Given the available scientific evidence that US has a sensitivity of at least 60% in diagnosing VUR (P=0.6), and with the hypothesis that US as a good method may have an acceptable level of diagnostic value in terms of sensitivity (i.e. a of 80%), the minimum sample size required for this study was estimated to be 160 people using the Equation 1 with α=0.05 and d=0.1 (d=0.08):
In examining urine culture results in the midstream sample, the growth of more than 50000 colonies of an organism, one colony in the suprapubic sample, or more than 1000 colonies in the urine culture catheter sample was considered positive. The US of the kidneys, urinary tract, and bladder was performed for all children with a UTI. Also, VCUG or RNC was performed for the patients if there was an indication. According to the guidelines, the indications include children under 2 years or 2-3 years of age who have febrile UTI, especially if it is recurrent or accompanied by US abnormalities or fetal anomalies. Patients who are involved with overactive bladder or have recurrent UTI or their urine cultures are reported to contain atypical microbes [14].
Statistical analysis
In this study, frequency distribution statistics were used to describe qualitative variables, and Mean±SD and range (minimum and maximum values) were used to report and describe the age, the only numerical variable. Sensitivity and specificity were calculated to investigate the US diagnostic value in determining VUR. Kappa statistic was used to examine the agreement between the two methods. Cohen suggested the kappa result be interpreted as follows: Values ≤0 are interpreted as no agreement; 0.01–0.20 as none to slight; 0.21–0.40 as fair; 0.41– 0.60 as moderate; 0.61–0.80 as substantial; and 0.81–1.00 as almost perfect agreement. The chi-square test was used to compare proportions. SPSS software, version 20 was used for analyses, and P<0.05 were considered significant in all statistical tests.
Results
In this study, 183 children were assessed. Their Mean±SD age was 6.98±4.07 years (minimum 1 year and maximum 17 years); 119(65%) were girls, and 64(35%) were boys. Table 1 presents the findings of the right and left urinary tract anatomy, based on the US, separated by gender and side.
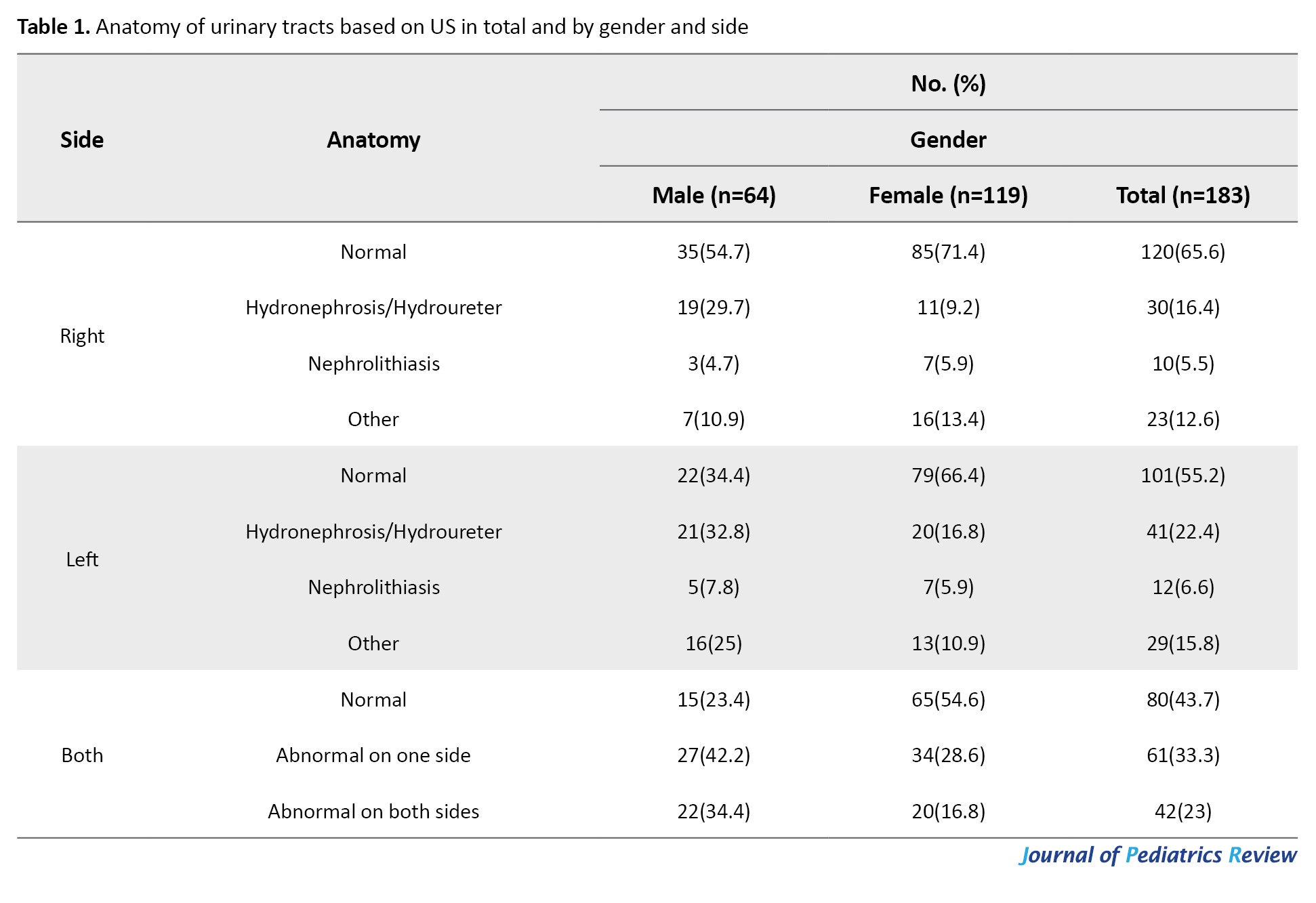
As seen in Table 1, out of the total 183 eligible children examined by US, 80(43.7%) were reported as normal, 63(34.4%), and 82(44.8%) were reported to have abnormalities in their right and left urinary systems, respectively. Also, 42 children (23%) had abnormalities in both sides.
VUR was assessed in 112 children (61.2%) using VCUG and 63(34.4%) using RNC, and both methods were used for only 8 children. In 8 patients who used both methods, the results of the two methods were in complete agreement in 6 patients, and there was a difference in results in only 2 patients, which, in the final analysis of the results, VCUG results were considered. Table 2 shows the status of VUR based on analysis of initial (first) VCUG/RNC results of urinary tracts by gender and side.
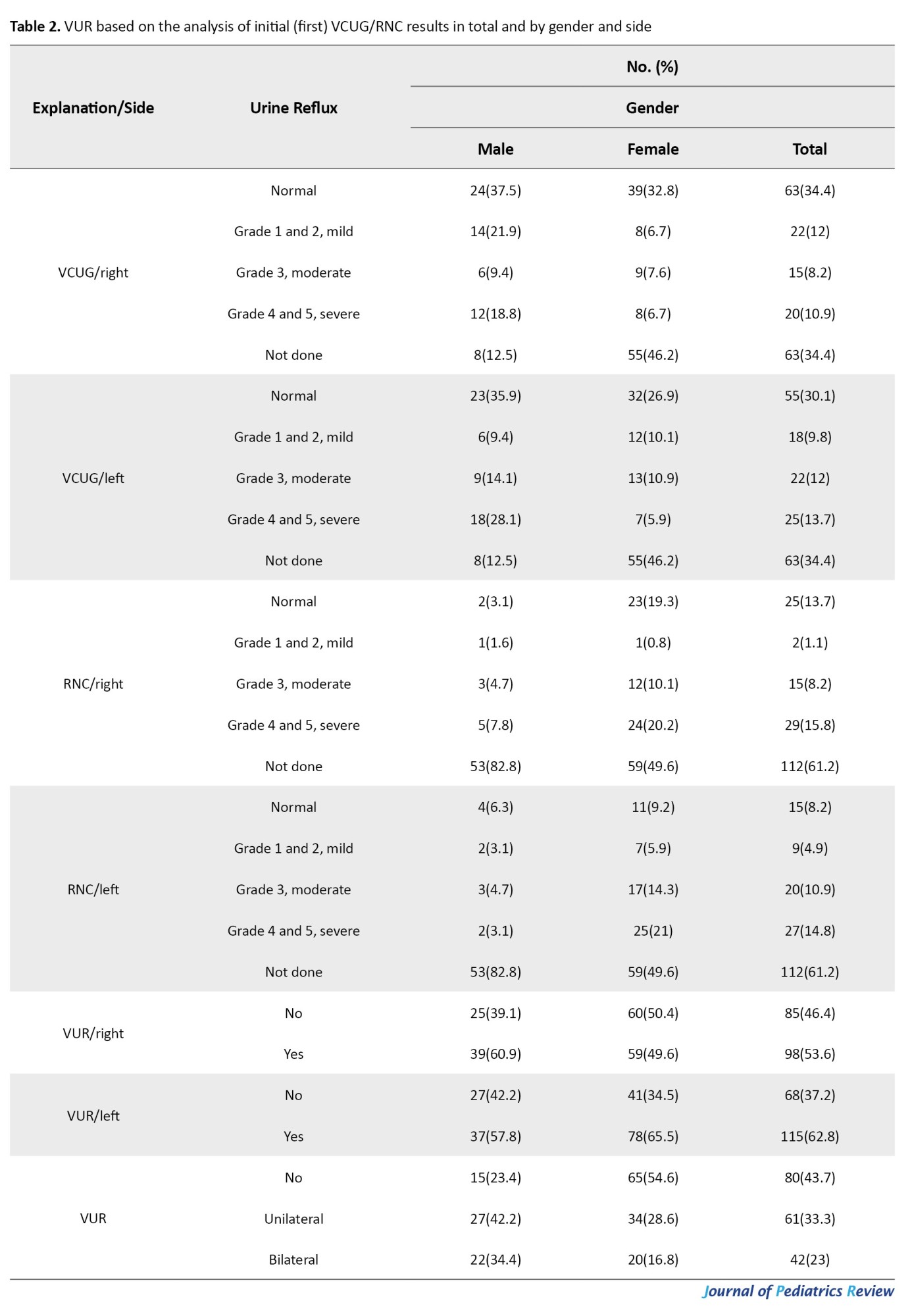
As seen in Table 2, 39 children(21.3%) did not have reflux, and the rest (144 children, 78.7%) had some degree of VUR, either unilateral or bilateral.
Table 3 shows the frequency distribution of the VUR diagnosis based on the results of VCUG/ RNC for normal and abnormal US findings.
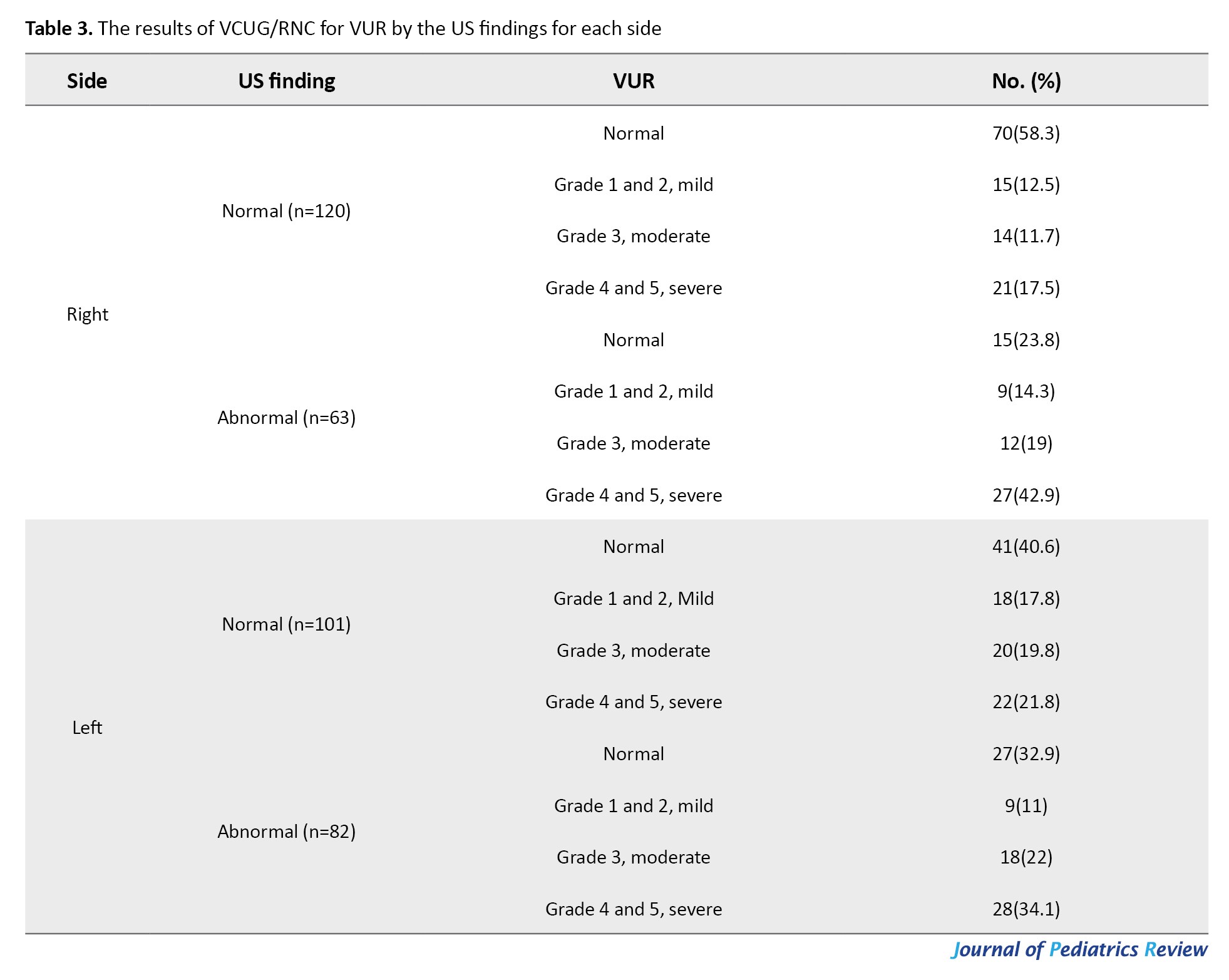
According to Table 3, 58.3% and 40.6% of normal reported US were reported normal for VUR. As the reflux grade increases, the percentage of US abnormalities increases (14.3% to 42.9%). However, as the grade decreases, the percentage of US normality decreases too (17.5% to 12.5%).
Table 4 shows the sensitivity and specificity of US findings for VUR diagnosis.
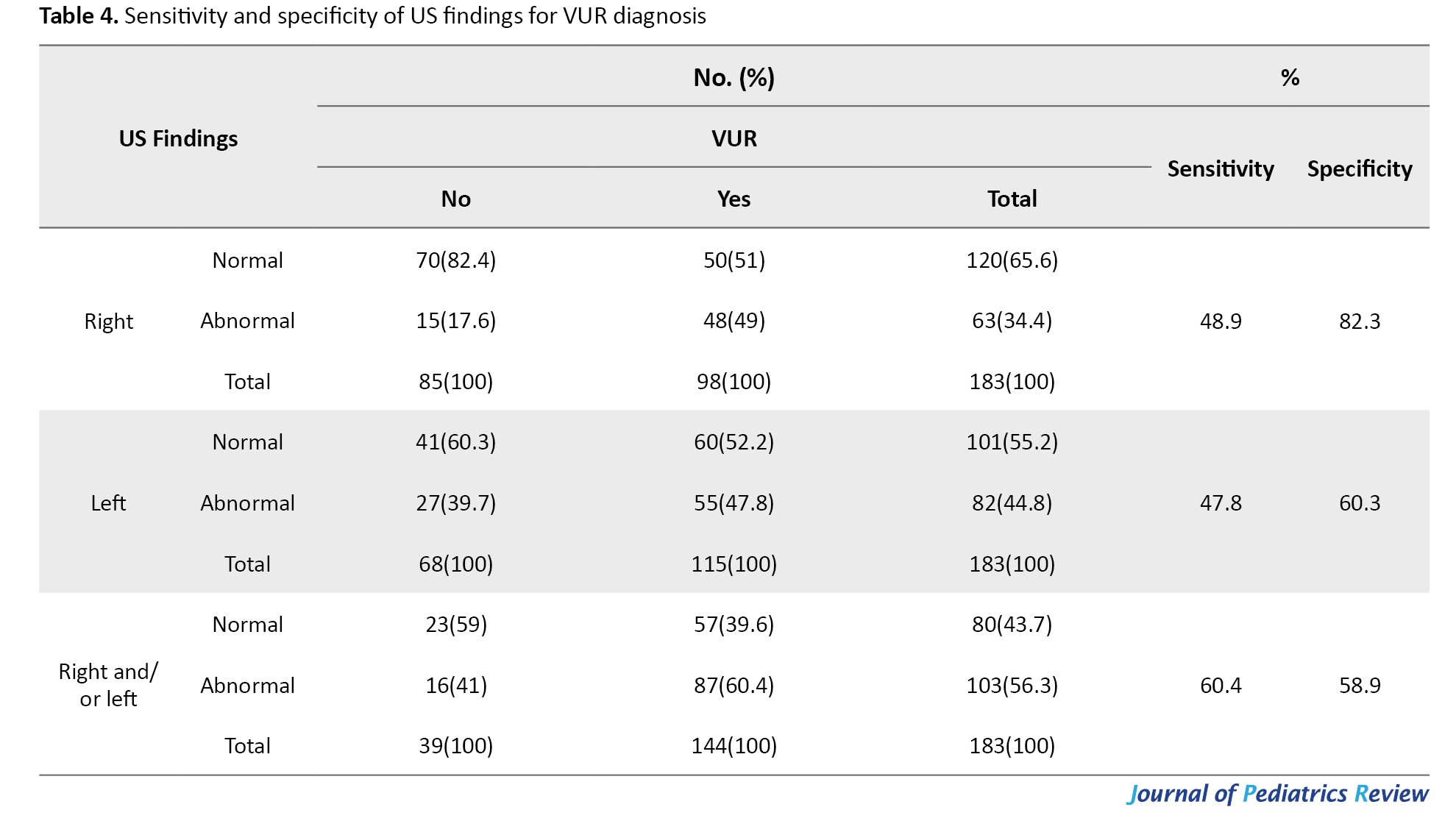
Based on Table 4, the sensitivity and specificity of the US for detecting VUR are 60.4% and 58.9%, respectively. The level of agreement between the two in terms of kappa statistic must be considered “none to slight” (k=0.14, P=0.003).
Discussion
Our findings show that the sensitivity and specificity of US for detecting VUR are 60.4% and 58.9%, respectively. Also, the agreement between the two methods (US vs gold standard VCUG/RNC) in terms of kappa statistic was calculated to be “none to slight” (k=0.14, P=0.003).
VUR may partially contribute to recurrent UTI in children. If not diagnosed in time, children’s normal growth and development may be affected. Currently, diagnostic techniques for VUR are continuously improved. Due to the characteristics of pediatrics, higher requirements for safety and accuracy of diagnosis are raised. VCUG is now widely used. However, repeated examination using VCUG is harmful to children’s health due to its significant radioactivity. RNC is a sensitive alternative method. However, its spatial resolution is not acceptable. In contrast, US stands out among many diagnostic methods due to its non-radioactive nature [15-17].
Studies have mentioned that US is effective in diagnosing diseases. However, for examination, it is necessary to take images of the urethra intermittently and continuously so the process of filling and excretion from the urethra cannot be observed accurately and in real-time. As a result, certain missing occurs. Due to the significant limitations of US showing the posterior urethra, the operator must pay more attention to the urinary system during voiding to see the structure of the urethra more clearly, which is a big problem [18].
Yang et al. evaluated the value and compatibility rate of urethral US in pediatric VUR. A total of 160 subjects were examined in their study. Among them, 56 cases had reflux; 46 renal ureteral units had reflux under both examination methods (28.75%), and 10 cases were detected only by US (6.25%). Thirty-four cases of VUR (42.50%) were diagnosed by US, of which 15 had bilateral reflux and 4 had unilateral reflux. Also, 25 cases (35.00%) were diagnosed by VCUG, of whom 10 cases had bilateral regurgitation and 5 had unilateral regurgitation. There was no significant difference in the rate of reflux detection between the two methods. A total of 146 diagnosed cases were consistent between the two methods (91.25%), and only 9.75% were not [19].
The current study shows that US does not match well with VCUG/ RNC for diagnosing VUR. Of course, in our study, the statistical difference between the two sets was not evaluated. Perhaps the reason for the difference between the results of the two studies was the sample size. In the present study, 183 children with VUR were examined, and in the study by Yang et al. [19], 56 children were examined with VUR, and the higher sample size was one of the advantages of the present study.
In Mane et al.’s study, 30 children were examined. Their mean age was 51.53 months. There were 21 boys and 9 girls. In VCUG, 16 patients did not have reflux, and 14 had reflux. Regarding the US, 14 patients did not have VUR, and 16 had VUR. Of 58 kidney-ureteral units (KUUs), VUR was diagnosed in 17 by VCUG and in 21 by US. Therefore, US identified 4 reflux units that were not seen on VCUG. In the right KUU, US detected VUR in 3 units without reflex on VCUG. In the 28 left KUU, 25 units in the US corresponded to the degree of VUR detected by VCUG. Two cases showed a VUR grade higher than the corresponding VCUG grade, and one had a lower grade. Regarding the US, 14 patients lacked VUR, and 16 had VUR. In total, US revealed 4 cases that VCUG did not detect them. This study concluded that US is a promising imaging modality compared to VCUG for evaluating pediatric ureteral reflux due to its superior diagnostic performance, feasibility, and radiation safety for children [20]. In the current study, it was seen that the US of the right urinary tract identified 83 cases as normal and 47 cases as abnormal, while these numbers for VCUG were 41 cases and 89 cases, respectively. Regarding the left kidney, it was also seen that the US diagnosed 78 cases as normal and 68 cases as abnormal, while VCUG diagnosed 45 cases as normal and 101 cases as abnormal, which, from this point of view, the present study was different from the study of Mane et al. Based on our findings, US does not seem to have a good diagnostic compatibility with VCUG.
Takahashi et al. compared the diagnostic compatibility of US with cystourethrography for diagnosing VUR. US failed to detect two cases of grade 1 VUR in adolescents, whereas it detected grade 4 VUR in one highly dilated renal-ureteral unit that was not detected on cystourethrography [21]. The results of our study are also in line with this study.
Conclusion
The current study shows that US does not match well with VCUG/ RNC for diagnosing VUR. The sensitivity and specificity of the US were 60.4% and 58.9%, respectively, which is not acceptable for a diagnostic test. The level of agreement between the two methods was significant, from “none to slight,” which was also not a good agreement. Thus, it can be said that US is not appropriate for diagnosing VUR and is not a good diagnostic method. Indeed, VCUG or RNC are preferable despite all their disadvantages. Although US is a cheap, accessible, and highly acceptable method for children and their families, its diagnostic compatibility with VCUG/RNC is not high, and if there is a suspicion of VUR, US may not be able to confirm it and VCUG/RNC should be used.
Ethical Considerations
Compliance with ethical guidelines
This research adhered to the principles outlined in the Declaration of Helsinki. For this study, the parents of the children consented to participate in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors express their gratitude for Mohammadamir Kakaee for his contribution and integrity in research and data gathering.
References
- Barola S, Grossman OK, Abdelhalim A. Urinary Tract Infections In Children. 2024 Jan 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan. [PMID]
- Lotfollahzadeh S, Leslie S, Aeddula N. Vesicoureteral Reflux. StatPearls. 2024. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. [PMID]
- Skoog SJ, Peters CA, Arant BS Jr, Copp HL, Elder JS, Hudson RG, et al. Pediatric vesicoureteral reflux guidelines panel summary report: clinical practice guidelines for screening siblings of children with vesicoureteral reflux and neonates/infants with prenatal hydronephrosis. J Urol. 2010; 184(3):1145-51. [DOI:10.1016/j.juro.2010.05.066] [PMID]
- Sencan A, Carvas F, Hekimoglu IC, Caf N, Sencan A, Chow J, et al. Urinary tract infection and vesicoureteral reflux in children with mild antenatal hydronephrosis. J Pediatr Urol. 2014; 10(6):1008-13. [DOI:10.1016/j.jpurol.2014.04.001] [PMID]
- Chang JW, Liu CS, Tsai HL. Vesicoureteral reflux in children with urinary tract infections in the inpatient setting in Taiwan. Clin Epidemiol. 2022; 14:299-307. [DOI:10.2147/CLEP.S346645] [PMID]
- Meena J, Mathew G, Hari P, Sinha A, Bagga A. Prevalence of bladder and bowel dysfunction in toilet-trained children with urinary tract infection and/or primary vesicoureteral reflux: A systematic review and meta-analysis. Front Pediatr. 2020; 8:84. [DOI:10.3389/fped.2020.00084] [PMID]
- Naseri M, Tafazoli N, Tafazoli N. Prevalence of Vesicoureteral Reflux in Children with Urinary Tract Infection. Saudi J Kidney Dis Transpl. 2022; 33(Supplement):S111-20. [DOI:10.4103/1319-2442.384183] [PMID]
- Capozza N, Gulia C, Heidari Bateni Z, Zangari A, Gigli S, Briganti V, et al. Vesicoureteral reflux in infants: What do we know about the gender prevalence by age? Eur Rev Med Pharmacol Sci. 2017; 21(23):5321-9. [PMID]
- Shaikh N, Ewing AL, Bhatnagar S, Hoberman A. Risk of renal scarring in children with a first urinary tract infection: A systematic review. Pediatrics. 2010; 126(6):1084-91.[DOI:10.1542/peds.2010-0685] [PMID]
- Lee YJ, Lee JH, Park YS. Risk factors for renal scar formation in infants with first episode of acute pyelonephritis: A prospective clinical study. J Urol. 2012; 187(3):1032-6. [DOI:10.1016/j.juro.2011.10.164] [PMID]
- Kobayashi Y, Mishina H, Michihata N, Miyasaka M, Takayama JI. Indication for voiding cystourethrography during first urinary tract infection. Pediatr Int. 2019; 61(6):595-600. [DOI:10.1111/ped.13835] [PMID]
- Caillaud C, Abély M, Pons A, Brunel D, Viprey M, Pietrement C. [A retrospective study to evaluate a protocol aimed at reducing the number of unnecessary voiding cystourethrographies performed after a first episode of febrile urinary tract infection (French)]. Arch Pediatr. 2013; 20(5):476-83. [DOI:10.1016/j.arcped.2013.02.069] [PMID]
- Mazzi S, Rohner K, Hayes W, Weitz M. Timing of voiding cystourethrography after febrile urinary tract infection in children: A systematic review. Arch Dis Child. 2020; 105(3):264-9. [DOI:10.1136/archdischild-2019-316958] [PMID]
- Emma F, Goldstein SL, Bagga A, Bates CM, Shroff R. Pediatric nephrology. Berlin: Springer Nature; 2022. [DOI:10.1007/978-3-030-52719-8]
- Merrikhi AR, Keivanfar M, Gheissari A, Mousavinasab F. Urine interlukein-8 as a diagnostic test for vesicoureteral reflux in children. J Pak Med Assoc. 2012; 62(3 Suppl 2):S52-4. [PMID]
- Tagliati C, Argalia G, Giuseppetti GM. Contrast-enhanced US performance in predicting blunt splenic injuries requiring only observation and monitoring. Med Ultrason. 2019; 21(1):16-21. [DOI:10.11152/mu-1700] [PMID]
- Shirazi M, Eslahi A, Sharifi V, Rahimi F, Safarpour A. Evaluation of Caspase 3 Enzyme and TNF-alpha as Biomarkers in Ureteropelvic Junction Obstruction in Children-a preliminary report. Pak J Med Sci. 2017; 33(2):315-9. [DOI:10.12669/pjms.332.11934] [PMID]
- Theek B, Opacic T, Möckel D, Schmitz G, Lammers T, Kiessling F. Automated generation of reliable blood velocity parameter maps from contrast-enhanced US data. Contrast Media Mol Imaging. 2017; 2017:2098324.[DOI:10.1155/2017/2098324] [PMID]
- Yang B, Wang J, Di Z, Zhao S, Ma Y, Qu Y. Comparison of voiding vesicoureteral urosonography with fluoroscopic voiding cystourethrography in children with vesicoureteral reflux. Pak J Med Sci. 2023; 39(4):967-71. [DOI:10.12669/pjms.39.4.6665] [PMID]
- Mane N, Sharma A, Patil A, Gadekar C, Andankar M, Pathak H. Comparison of contrast-enhanced voiding urosonography with voiding cystourethrography in pediatric vesicoureteral reflux. Turk J Urol. 2018; 44(3):261-7. [DOI:10.5152/tud.2018.76702] [PMID]
- Straus Takahashi M, Gustavo Ieiri Yamanari M, Henrique de Marqui Moraes P, Lopes RI, Chammas MC. Vesicoureteral reflux by contrast US, comparison with voiding and retrograde urethrocystography: A prospective accuracy study. J Pediatr Urol. 2024; 20(1):133.e1-9. [DOI:10.1016/j.jpurol.2023.10.014] [PMID]
Type of Study: Original Article |
Subject:
Pediatric Nephrology
Received: 2024/12/25 | Accepted: 2024/12/30 | Published: 2025/01/21
Received: 2024/12/25 | Accepted: 2024/12/30 | Published: 2025/01/21
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









