Volume 13, Issue 2 (4-2025)
J. Pediatr. Rev 2025, 13(2): 113-118 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Soleymani A H, Kazemi S A, Taji M, Nazari H, Farhadi R. Investigating Neonatal Tail Associated With Tethered Cord and Spinal Dysraphism: Case Report and Literature Review. J. Pediatr. Rev 2025; 13 (2) :113-118
URL: http://jpr.mazums.ac.ir/article-1-725-en.html
URL: http://jpr.mazums.ac.ir/article-1-725-en.html
1- Student Research Committee, Mazandaran University of Medical Sciences, Sari, Iran.
2- Department of Radiology, Mazandaran University of Medical Sciences, Sari, Iran.
3- Pediatric Infectious Diseases Research Center, Communicable Diseases Institute, Mazandaran University of Medical Sciences, Sari, Iran. & Division of Neonatology, Department of Pediatrics, Boo Ali Sina Hospital, Mazandaran University of Medical Sciences, Sari, Iran. ,dr.royafarhadi@gmail.com
2- Department of Radiology, Mazandaran University of Medical Sciences, Sari, Iran.
3- Pediatric Infectious Diseases Research Center, Communicable Diseases Institute, Mazandaran University of Medical Sciences, Sari, Iran. & Division of Neonatology, Department of Pediatrics, Boo Ali Sina Hospital, Mazandaran University of Medical Sciences, Sari, Iran. ,
Full-Text [PDF 1290 kb]
(1059 Downloads)
| Abstract (HTML) (1785 Views)
Full-Text: (519 Views)
Introduction
Neonatal tail is a very rare birth defect that can be associated with tethered cord syndrome (TCS) and spinal dysraphism. TCS is when the spinal cord is attached abnormally within the spine and can cause neurological deficits, pain, and functional limitations. Spinal dysraphism is a spectrum of neural tube defects, including spina bifida and myelomeningocele, which can have skin lesions, including neonatal tails [1, 2].
A neonatal tail, which is a fibrous or fleshy appendage from the coccygeal area, has been reported in various case reports and may be associated with underlying spinal anomalies [3]. These tails may be remnants of embryonic development or could be indicators of more complex dysraphic conditions [4]. The importance of recognizing this association is that if the tethered cord is left untreated, it can be very morbid.
In recent years, there have been advances in imaging technology, especially ultrasound and magnetic resonance imaging (MRI), which have improved the ability to diagnose tethered cord and associated spinal conditions early in life [5]. Studies show that many infants with a neonatal tail may also have signs of tethered cord, such as lower extremity weakness, bladder dysfunction, or orthopedic deformities [6]. However, there is no comprehensive systematic review that consolidates the existing knowledge on the clinical implications of neonatal tails concerning tethered cord and spinal dysraphism.
Management of these conditions often requires a multidisciplinary approach, involving pediatricians, neurologists, and neurosurgeons. Surgery may be needed for the tethered cord to relieve symptoms and prevent further neurological deterioration [7, 8]. However, the decision to operate is not straightforward and should be based on a comprehensive evaluation, including clinical features, imaging findings, and potential for neurological deterioration over time.
Despite the existing literature, there is still a big gap in understanding the full spectrum of clinical implications of neonatal tails. This gap highlights the need for reviews that can synthesize data from case reports and studies to provide clarity on the prevalence of tethered cord in infants with neonatal tails, management, and long-term outcome [9]. The neonatal tails, TCS, and spinal dysraphism are a big clinical problem; awareness and recognition of this triad are key to early diagnosis and intervention and better outcomes for the babies. Such a review will inform clinical practice but also guide future research to clarify the underlying pathophysiology of these anomalies.
Case Presentation
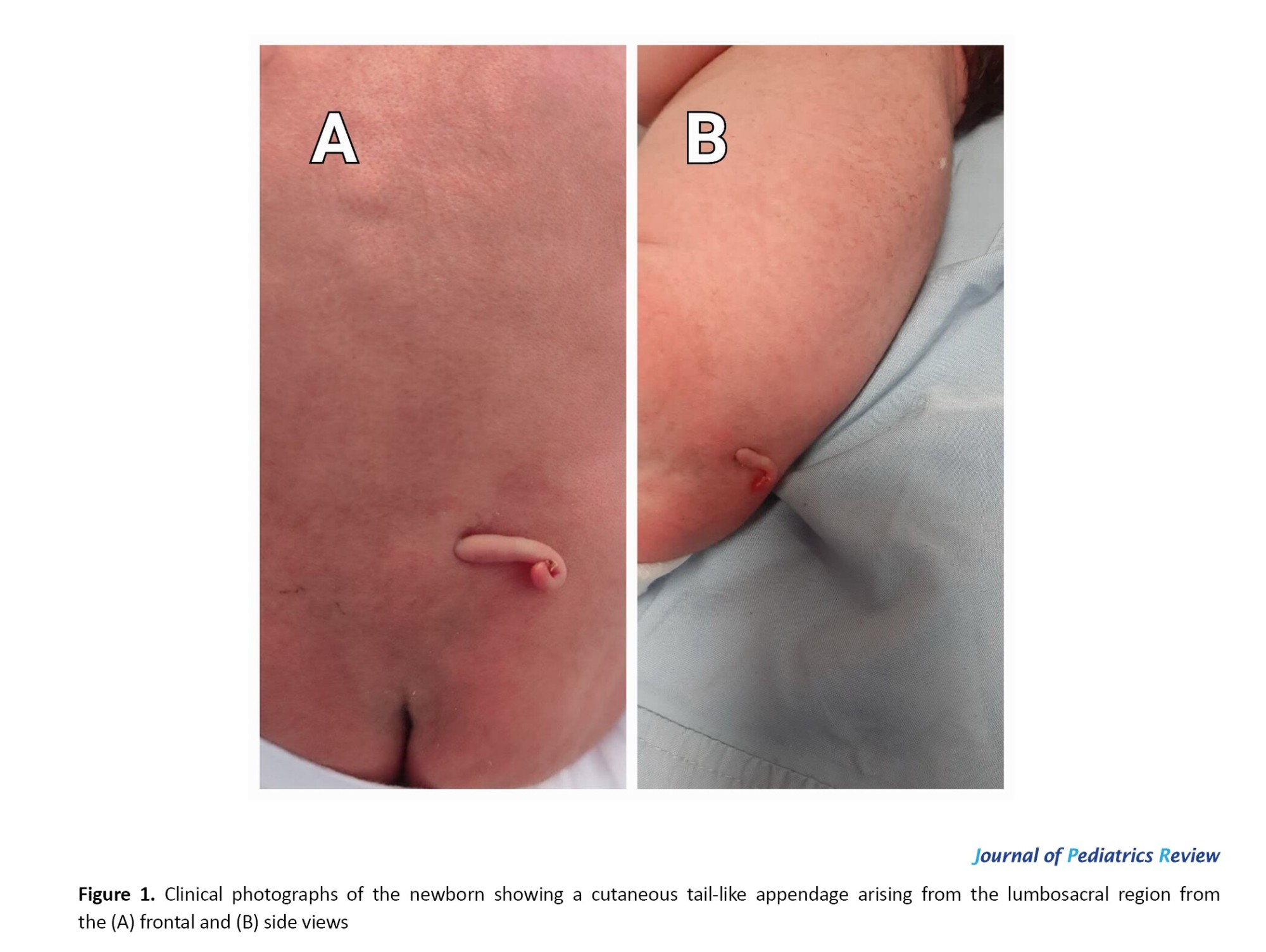
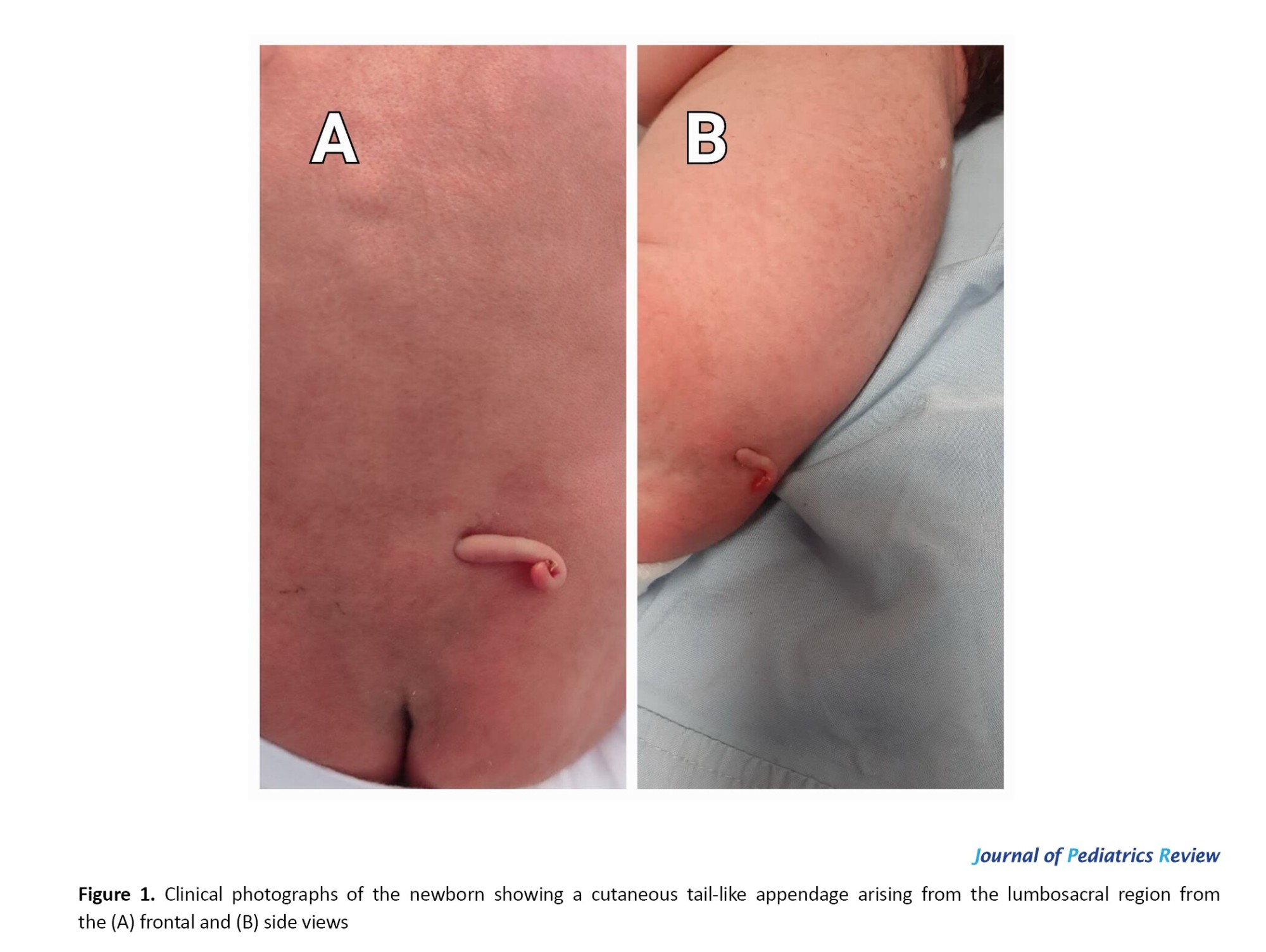
A male neonate was born at our maternal hospital, and during the initial evaluation, a skin protrusion resembling a tail was noted on the lumbosacral region. The neonate was born via elective cesarean section at 38 weeks of gestation due to maternal hypertension. The prenatal ultrasound did not reveal any significant abnormalities. At physical examination, a 3-cm-long, fleshy tail-like appendage was observed to protrude from the lumbosacral region. The skin surrounding the tail appeared normal, with no signs of infection or ulceration. The end of this appendage had a twisted shape resembling a pig’s tail, and when touched, it had a firm consistency (Figure 1). The baby was otherwise normal, showing normal vital signs and physical examination.
Neurologic examination showed normal reflexes in the upper and lower extremities, with a normal range of motion in the lower extremities. Urination and defecation were normal.
Subsequent evaluation included an ultrasonography of the lumbosacral segments, showing that the conus medullaris lies below its normal anatomical position at the level of the S1 vertebra. Bone defects were noted at the sacral vertebrae posteriorly. Additionally, a 16×4 mm echogenic structure was observed in the epidural space, significantly narrowing the cauda equina, consistent with an epidural lipoma. These results imply the presence of an accompanying tethered cord and sacral spinal dysraphism. Moreover, the brain ultrasound was unremarkable, and there was no evidence of hydrocephalus. An MRI was indicated for the neonate, but the parents declined consent for additional workup, and the neonate left the hospital with the parents’ consent. Although the efforts were made, there was no possibility for follow-up, and there has been no access to the patient for a visit.
Materials and Methods
A literature review was carried out using online databases, including Google Scholar, PubMed, Scopus, and Web of Science. The selected keywords were “neonatal tail,” “tethered cord syndrome,” and “spinal dysraphism.” The inclusion criteria included case reports, case series, and descriptions of prospective studies of the correlation between congenital tail and congenital vertebral dysplasia. Meanwhile, English language publications until December 2024 were included. However, articles that addressed cases outside of the neonatal period were excluded from the study. Accordingly, the selected studies were limited to a two-stage process: first, searching for articles by title, and then having two of the authors independently screen titles and abstracts of the electronic database searches for any paper that was thought to match the inclusion criteria. In this review, ten articles were selected from 240 initially searched papers because the others were somehow underrepresented in the field or were found to be duplicates of citations in different databases.
Results
Initially, a total of 240 articles were searched across three databases: Google Scholar, PubMed, Scopus, and Web of Science. From these search results, 29 articles were identified for further evaluation. After screening, 16 articles were excluded for not meeting the inclusion criteria, 2 articles were removed due to duplication, and 1 article was excluded because it was purely theoretical. In the end, 10 articles were chosen for the final review. Results showed a consistent association between neonatal tails and spinal dysraphism, especially TSCS.
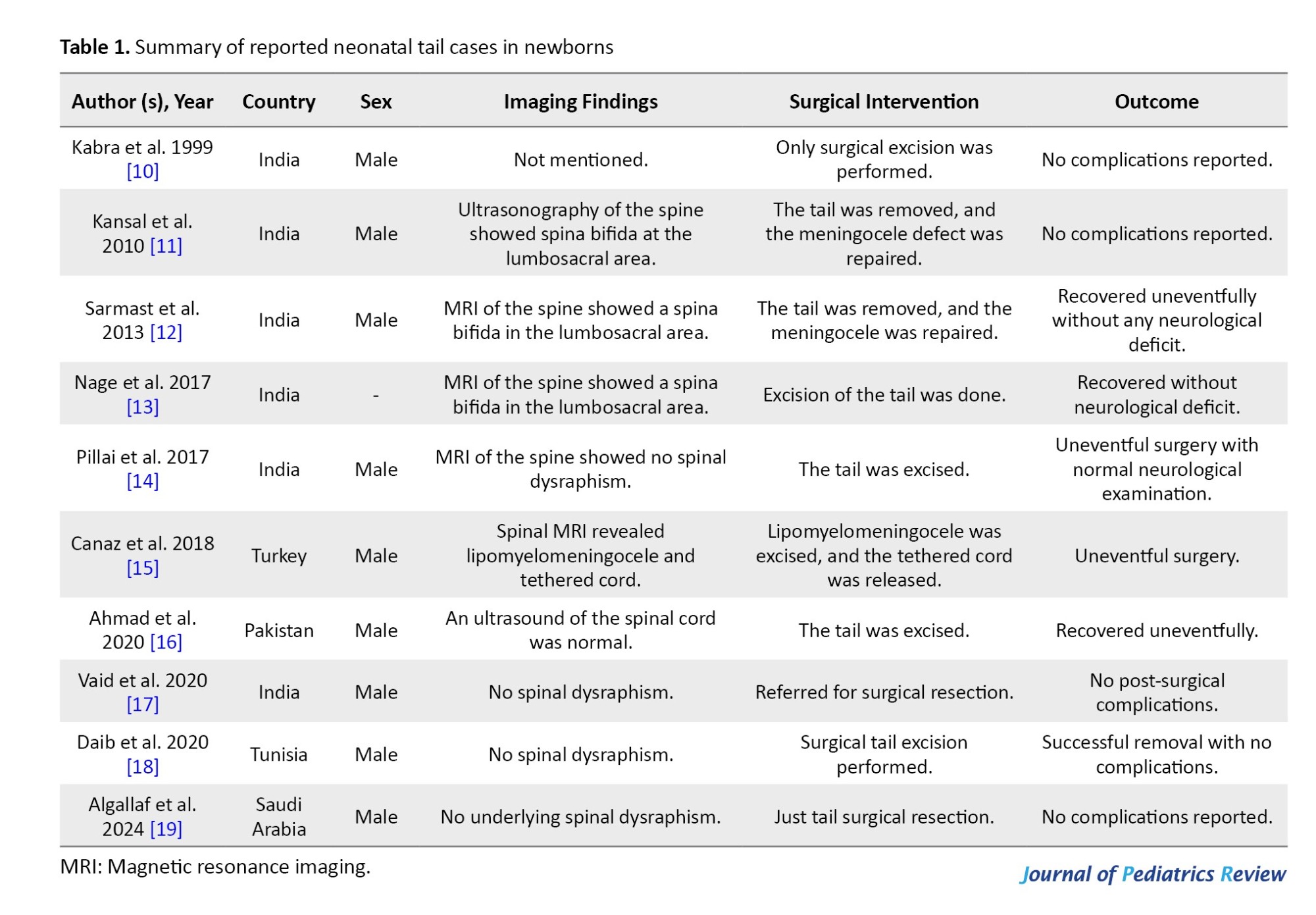
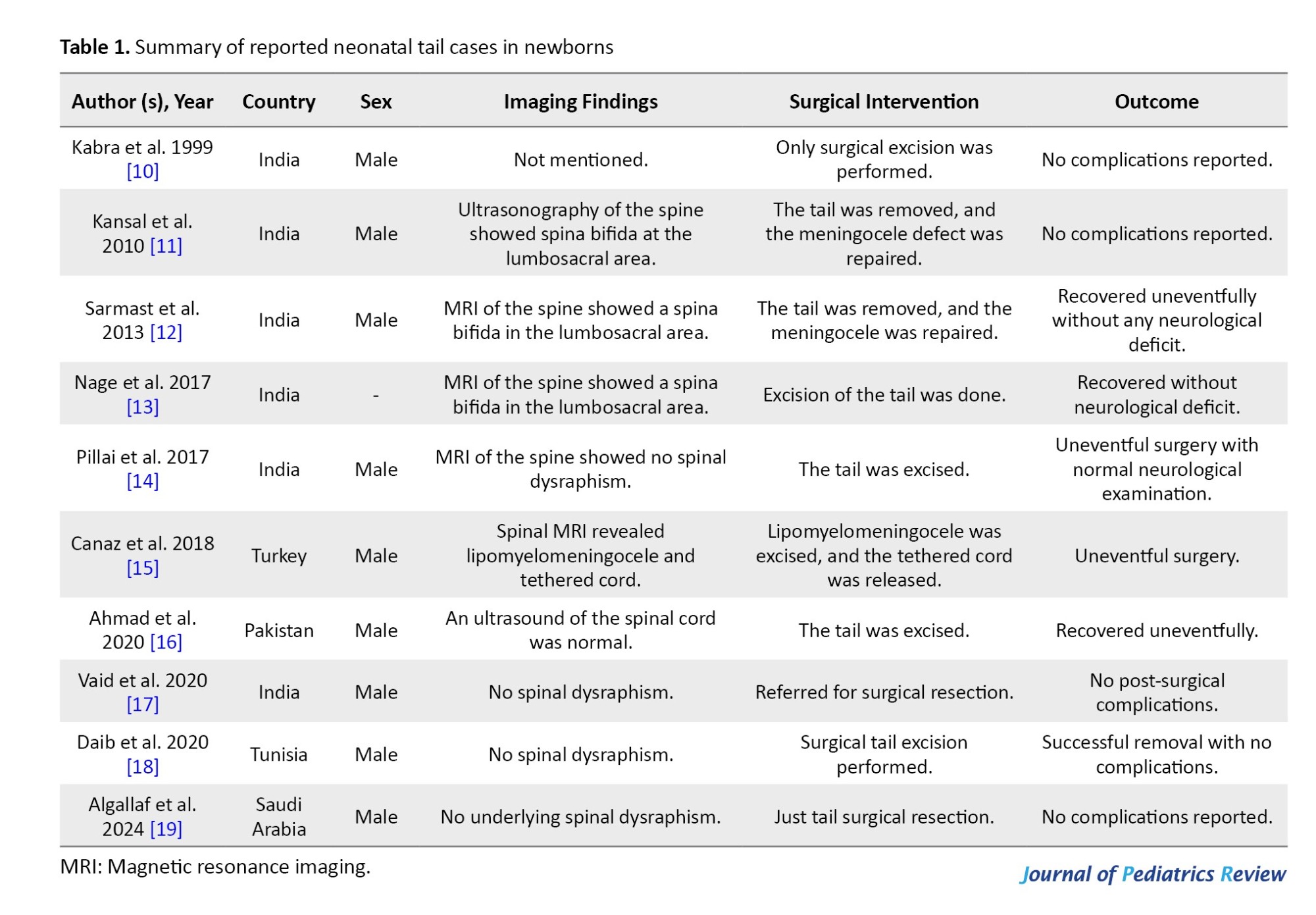
Most were male infants, with the tail at the lumbosacral region. Imaging, especially MRI, was key in diagnosing tethered cords and associated malformations. Surgery was common, detethering and excision of associated lesions was the main treatment. Most of the patients are reported from India. Most are true tails which are benign.
Most have normal neurologic function, and other systems were normal. Surgery is done for cosmetic or medical complications, and most do well. Table 1 shows the details of the investigated cases. The research by Kabra et al. [10] and Kansal et al. [11] highlights the occurrence of congenital conditions like neonatal tails and spinal dysraphism in India, emphasizing the urgent need for better screening protocols in neonatal care. They recommend that the presence of a tail in newborns may be a genetic trait. Supporting this, Sarmast et al. [12] and Nage et al. [13] illustrate the varied clinical presentations and outcomes linked to these anomalies, including instances of human tail syndrome with neurological effects. Pillai et al. [14] enhance our understanding of surgical management techniques, showing how timely surgical intervention can positively influence patient outcomes. Canaz et al. [15] describe a unique case of a human tail associated with lipomyelomeningocele and TSCS, highlighting the complex comorbidities that can occur. Ahmad et al. [16] refer to this phenomenon as an anatomical enigma, urging further exploration into the genetic and developmental factors at play. Importantly, Vaid et al. [17] document a case of a true neonatal tail alongside limb defects, stressing the necessity for thorough evaluations in such situations. Additionally, Vaid et al. [17] and Daib et al. [18] afford strong evidence for the importance of longterm follow-up and multidisciplinary care in managing complications related to TSCS. Recent findings by Algallaf et al. [19] demonstrate new trends in understanding and addressing congenital anomalies, setting the stage for future research.
The collective understandings from these studies highlight the persistent need for awareness, timely diagnosis, and comprehensive treatment strategies to improve the quality of life for neonates affected by TCS and spinal dysraphism in different regions. The documentation of these rare and unusual cases calls for continued examination into their genetic basis and related factors.
Discussion
The occurrence of a neonatal tail, or true human tail, is a rare phenomenon that has drawn attention from both researchers and clinicians. In the background of neonatal tails, it is necessary to differentiate between true neonatal tails and pseudotails for exact diagnosis and treatment. According to Lu et al. [20], true tails are benign coccygeal or gluteal lesions that can be effectively treated with basic resection. On the other hand, pseudotails present as tail-like lesions related to spinal dysraphism and may suggest primary ectodermal anomalies. This distinction is predominantly vital when assessing neonates, as pseudotails are often associated with disorders like spina bifida, which necessitates a thorough assessment to uncover any potential spinal issues. Managing these neonates involves a careful evaluation of related defects to decide on the best therapeutic strategy, emphasizing the necessity of a detailed investigation in the clinical assessment of neonatal tails. The presence of a fleshy appendage in the lumbosacral area, as seen in our case report, raises important questions about its embryological origins, related conditions, and management suggestions. Our case highlights the need for further investigation into its clinical relevance and possible underlying complications. From an embryological viewpoint, the formation of a true human tail is supposed to result from irregularities in the regression of the embryonic tail, which is typically a normal aspect of early gestation. In most human embryos, the tail usually regresses by the eighth week of gestation; however, if this process fails, a remaining tail may develop [21]. The present case demonstrates the physical aspect of this anomaly as a suedotail and highlights the importance of assessing for associated spinal and neurological issues. The detection of tethered cord and spinal dysraphism, as shown by the ultrasonography results, is principally significant. TCS, which involves abnormal attachment of the spinal cord leading to neurological deficiencies, is frequently linked with other spinal dysraphisms, such as lipomyelomeningocele or dermal sinus tracts [22]. In the present case, the ultrasonography indicated that the conus medullaris was positioned below the normal anatomical level, along with an echogenic structure in the epidural space that was consistent with an epidural lipoma. These observations support former studies suggesting a strong association between congenital tail-like appendages and spinal dysraphism, emphasizing the necessity of comprehensive imaging when evaluating such anomalies [23]. Healthcare providers need to remain alert to these associations to avert potential complications, including progressive neurological deficits that may arise if the tethered cord is left untreated.
While our patient exhibited normal neurological function, including reflexes and range of motion, we cannot ignore the possibility of upcoming complications. Literature shows that symptoms of tethered cord may not surface until later in childhood, potentially leading to problems with bowel and bladder control, gait abnormalities, and scoliosis [24]. The parents’ choice to decline further MRI imaging presents a challenge for monitoring the child’s development, as many cases of TCS require rapid intervention to prevent worsening conditions [25]. Another critical aspect to consider is the psychosocial impact of having a congenital anomaly like a tail. The visibility of this appendage can produce various reactions from families and communities, which can significantly affect the psychological well-being of both the baby and the family [26]. The rarity of such cases often leads to misunderstandings and stigma, possibly influencing the baby’s social interactions as they mature. Healthcare providers need to suggest thorough counseling and support to families of affected newborns, addressing both the medical and psychosocial aspects of this condition. The literature presents a wide range of reports on true human tails, showcasing various presentations and associated conditions. For example, several studies highlight the importance of identifying the potential for simultaneous anomalies, such as spina bifida and other forms of spinal dysraphism [27]. This highlights the need for a multidisciplinary approach in management, involving pediatric neurosurgeons, radiologists, and family support services. To put it briefly, the case of the neonate with a lumbosacral tail-like appendage highlights the complexity of congenital anomalies and their potential effects on neurological health. As healthcare providers, we must stay aware in our evaluations and consider the broader implications of such findings. Ongoing research and case documentation are crucial for deepening our understanding of true human tail presentations, their embryological origins, and long-term outcomes. Future studies should focus on creating guidelines for managing these cases, ensuring that affected neonates receive the essential care and monitoring to enhance their health courses.
Conclusion
This case report on a newborn with a human tail highlights the link between congenital anomalies and neurological disorders, such as spinal dysraphism and TCS. It emphasizes the importance of thorough assessment and imaging, as these anomalies may signal underlying spinal abnormalities. A multidisciplinary care approach is necessary to address both medical and emotional needs. Future research is vital for developing management guidelines and raising awareness of potential complications, ultimately improving the well-being of affected neonates.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval for this report was provided by the Research Ethics Committee of Mazandaran University of Medical Sciences, Sari, Iran, (Code: IR.MAZUMS.REC.1403.549).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization and supervision: Roya Farhadi and Amir Hossein Soleymani; Data collection: Seyed Amir Kazemi and Hengameh Nazari; Writing the original draft: Marzieh Taji; Review and editing: All authors.
Conflicts of interest
The authors declared no conflict of interest.
References
Neonatal tail is a very rare birth defect that can be associated with tethered cord syndrome (TCS) and spinal dysraphism. TCS is when the spinal cord is attached abnormally within the spine and can cause neurological deficits, pain, and functional limitations. Spinal dysraphism is a spectrum of neural tube defects, including spina bifida and myelomeningocele, which can have skin lesions, including neonatal tails [1, 2].
A neonatal tail, which is a fibrous or fleshy appendage from the coccygeal area, has been reported in various case reports and may be associated with underlying spinal anomalies [3]. These tails may be remnants of embryonic development or could be indicators of more complex dysraphic conditions [4]. The importance of recognizing this association is that if the tethered cord is left untreated, it can be very morbid.
In recent years, there have been advances in imaging technology, especially ultrasound and magnetic resonance imaging (MRI), which have improved the ability to diagnose tethered cord and associated spinal conditions early in life [5]. Studies show that many infants with a neonatal tail may also have signs of tethered cord, such as lower extremity weakness, bladder dysfunction, or orthopedic deformities [6]. However, there is no comprehensive systematic review that consolidates the existing knowledge on the clinical implications of neonatal tails concerning tethered cord and spinal dysraphism.
Management of these conditions often requires a multidisciplinary approach, involving pediatricians, neurologists, and neurosurgeons. Surgery may be needed for the tethered cord to relieve symptoms and prevent further neurological deterioration [7, 8]. However, the decision to operate is not straightforward and should be based on a comprehensive evaluation, including clinical features, imaging findings, and potential for neurological deterioration over time.
Despite the existing literature, there is still a big gap in understanding the full spectrum of clinical implications of neonatal tails. This gap highlights the need for reviews that can synthesize data from case reports and studies to provide clarity on the prevalence of tethered cord in infants with neonatal tails, management, and long-term outcome [9]. The neonatal tails, TCS, and spinal dysraphism are a big clinical problem; awareness and recognition of this triad are key to early diagnosis and intervention and better outcomes for the babies. Such a review will inform clinical practice but also guide future research to clarify the underlying pathophysiology of these anomalies.
Case Presentation
A male neonate was born at our maternal hospital, and during the initial evaluation, a skin protrusion resembling a tail was noted on the lumbosacral region. The neonate was born via elective cesarean section at 38 weeks of gestation due to maternal hypertension. The prenatal ultrasound did not reveal any significant abnormalities. At physical examination, a 3-cm-long, fleshy tail-like appendage was observed to protrude from the lumbosacral region. The skin surrounding the tail appeared normal, with no signs of infection or ulceration. The end of this appendage had a twisted shape resembling a pig’s tail, and when touched, it had a firm consistency (Figure 1). The baby was otherwise normal, showing normal vital signs and physical examination.
Neurologic examination showed normal reflexes in the upper and lower extremities, with a normal range of motion in the lower extremities. Urination and defecation were normal.
Subsequent evaluation included an ultrasonography of the lumbosacral segments, showing that the conus medullaris lies below its normal anatomical position at the level of the S1 vertebra. Bone defects were noted at the sacral vertebrae posteriorly. Additionally, a 16×4 mm echogenic structure was observed in the epidural space, significantly narrowing the cauda equina, consistent with an epidural lipoma. These results imply the presence of an accompanying tethered cord and sacral spinal dysraphism. Moreover, the brain ultrasound was unremarkable, and there was no evidence of hydrocephalus. An MRI was indicated for the neonate, but the parents declined consent for additional workup, and the neonate left the hospital with the parents’ consent. Although the efforts were made, there was no possibility for follow-up, and there has been no access to the patient for a visit.
Materials and Methods
A literature review was carried out using online databases, including Google Scholar, PubMed, Scopus, and Web of Science. The selected keywords were “neonatal tail,” “tethered cord syndrome,” and “spinal dysraphism.” The inclusion criteria included case reports, case series, and descriptions of prospective studies of the correlation between congenital tail and congenital vertebral dysplasia. Meanwhile, English language publications until December 2024 were included. However, articles that addressed cases outside of the neonatal period were excluded from the study. Accordingly, the selected studies were limited to a two-stage process: first, searching for articles by title, and then having two of the authors independently screen titles and abstracts of the electronic database searches for any paper that was thought to match the inclusion criteria. In this review, ten articles were selected from 240 initially searched papers because the others were somehow underrepresented in the field or were found to be duplicates of citations in different databases.
Results
Initially, a total of 240 articles were searched across three databases: Google Scholar, PubMed, Scopus, and Web of Science. From these search results, 29 articles were identified for further evaluation. After screening, 16 articles were excluded for not meeting the inclusion criteria, 2 articles were removed due to duplication, and 1 article was excluded because it was purely theoretical. In the end, 10 articles were chosen for the final review. Results showed a consistent association between neonatal tails and spinal dysraphism, especially TSCS.
Most were male infants, with the tail at the lumbosacral region. Imaging, especially MRI, was key in diagnosing tethered cords and associated malformations. Surgery was common, detethering and excision of associated lesions was the main treatment. Most of the patients are reported from India. Most are true tails which are benign.
Most have normal neurologic function, and other systems were normal. Surgery is done for cosmetic or medical complications, and most do well. Table 1 shows the details of the investigated cases. The research by Kabra et al. [10] and Kansal et al. [11] highlights the occurrence of congenital conditions like neonatal tails and spinal dysraphism in India, emphasizing the urgent need for better screening protocols in neonatal care. They recommend that the presence of a tail in newborns may be a genetic trait. Supporting this, Sarmast et al. [12] and Nage et al. [13] illustrate the varied clinical presentations and outcomes linked to these anomalies, including instances of human tail syndrome with neurological effects. Pillai et al. [14] enhance our understanding of surgical management techniques, showing how timely surgical intervention can positively influence patient outcomes. Canaz et al. [15] describe a unique case of a human tail associated with lipomyelomeningocele and TSCS, highlighting the complex comorbidities that can occur. Ahmad et al. [16] refer to this phenomenon as an anatomical enigma, urging further exploration into the genetic and developmental factors at play. Importantly, Vaid et al. [17] document a case of a true neonatal tail alongside limb defects, stressing the necessity for thorough evaluations in such situations. Additionally, Vaid et al. [17] and Daib et al. [18] afford strong evidence for the importance of longterm follow-up and multidisciplinary care in managing complications related to TSCS. Recent findings by Algallaf et al. [19] demonstrate new trends in understanding and addressing congenital anomalies, setting the stage for future research.
The collective understandings from these studies highlight the persistent need for awareness, timely diagnosis, and comprehensive treatment strategies to improve the quality of life for neonates affected by TCS and spinal dysraphism in different regions. The documentation of these rare and unusual cases calls for continued examination into their genetic basis and related factors.
Discussion
The occurrence of a neonatal tail, or true human tail, is a rare phenomenon that has drawn attention from both researchers and clinicians. In the background of neonatal tails, it is necessary to differentiate between true neonatal tails and pseudotails for exact diagnosis and treatment. According to Lu et al. [20], true tails are benign coccygeal or gluteal lesions that can be effectively treated with basic resection. On the other hand, pseudotails present as tail-like lesions related to spinal dysraphism and may suggest primary ectodermal anomalies. This distinction is predominantly vital when assessing neonates, as pseudotails are often associated with disorders like spina bifida, which necessitates a thorough assessment to uncover any potential spinal issues. Managing these neonates involves a careful evaluation of related defects to decide on the best therapeutic strategy, emphasizing the necessity of a detailed investigation in the clinical assessment of neonatal tails. The presence of a fleshy appendage in the lumbosacral area, as seen in our case report, raises important questions about its embryological origins, related conditions, and management suggestions. Our case highlights the need for further investigation into its clinical relevance and possible underlying complications. From an embryological viewpoint, the formation of a true human tail is supposed to result from irregularities in the regression of the embryonic tail, which is typically a normal aspect of early gestation. In most human embryos, the tail usually regresses by the eighth week of gestation; however, if this process fails, a remaining tail may develop [21]. The present case demonstrates the physical aspect of this anomaly as a suedotail and highlights the importance of assessing for associated spinal and neurological issues. The detection of tethered cord and spinal dysraphism, as shown by the ultrasonography results, is principally significant. TCS, which involves abnormal attachment of the spinal cord leading to neurological deficiencies, is frequently linked with other spinal dysraphisms, such as lipomyelomeningocele or dermal sinus tracts [22]. In the present case, the ultrasonography indicated that the conus medullaris was positioned below the normal anatomical level, along with an echogenic structure in the epidural space that was consistent with an epidural lipoma. These observations support former studies suggesting a strong association between congenital tail-like appendages and spinal dysraphism, emphasizing the necessity of comprehensive imaging when evaluating such anomalies [23]. Healthcare providers need to remain alert to these associations to avert potential complications, including progressive neurological deficits that may arise if the tethered cord is left untreated.
While our patient exhibited normal neurological function, including reflexes and range of motion, we cannot ignore the possibility of upcoming complications. Literature shows that symptoms of tethered cord may not surface until later in childhood, potentially leading to problems with bowel and bladder control, gait abnormalities, and scoliosis [24]. The parents’ choice to decline further MRI imaging presents a challenge for monitoring the child’s development, as many cases of TCS require rapid intervention to prevent worsening conditions [25]. Another critical aspect to consider is the psychosocial impact of having a congenital anomaly like a tail. The visibility of this appendage can produce various reactions from families and communities, which can significantly affect the psychological well-being of both the baby and the family [26]. The rarity of such cases often leads to misunderstandings and stigma, possibly influencing the baby’s social interactions as they mature. Healthcare providers need to suggest thorough counseling and support to families of affected newborns, addressing both the medical and psychosocial aspects of this condition. The literature presents a wide range of reports on true human tails, showcasing various presentations and associated conditions. For example, several studies highlight the importance of identifying the potential for simultaneous anomalies, such as spina bifida and other forms of spinal dysraphism [27]. This highlights the need for a multidisciplinary approach in management, involving pediatric neurosurgeons, radiologists, and family support services. To put it briefly, the case of the neonate with a lumbosacral tail-like appendage highlights the complexity of congenital anomalies and their potential effects on neurological health. As healthcare providers, we must stay aware in our evaluations and consider the broader implications of such findings. Ongoing research and case documentation are crucial for deepening our understanding of true human tail presentations, their embryological origins, and long-term outcomes. Future studies should focus on creating guidelines for managing these cases, ensuring that affected neonates receive the essential care and monitoring to enhance their health courses.
Conclusion
This case report on a newborn with a human tail highlights the link between congenital anomalies and neurological disorders, such as spinal dysraphism and TCS. It emphasizes the importance of thorough assessment and imaging, as these anomalies may signal underlying spinal abnormalities. A multidisciplinary care approach is necessary to address both medical and emotional needs. Future research is vital for developing management guidelines and raising awareness of potential complications, ultimately improving the well-being of affected neonates.
Ethical Considerations
Compliance with ethical guidelines
Ethical approval for this report was provided by the Research Ethics Committee of Mazandaran University of Medical Sciences, Sari, Iran, (Code: IR.MAZUMS.REC.1403.549).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization and supervision: Roya Farhadi and Amir Hossein Soleymani; Data collection: Seyed Amir Kazemi and Hengameh Nazari; Writing the original draft: Marzieh Taji; Review and editing: All authors.
Conflicts of interest
The authors declared no conflict of interest.
References
- Kobets AJ, Oliver J, Cohen A, Jallo GI, Groves ML. Split cord malformation and tethered cord syndrome: Case series with long-term follow-up and literature review. Childs Nerv Syst. 2021; 37(4):1301-6. [DOI: 10.1007/s00381-020-04978-9] [PMID]
- Mualem W, Nathani KR, Durrani S, Zamanian C, Ghaith AK, Michalopoulos GD, et al. Utilizing pre- and postoperative radiological parameters to predict surgical outcomes following untethering for tethered cord syndrome in a pediatric population. J Neurosurg Pediatr. 2022; 31(2):159-68. [DOI: 10.3171/2022.10.PEDS22459] [PMID]
- Bilyalova G, Zhumadilova Z, Jaxalykova K, Turgumbaeva A. Caudal appendage in infant: Diagnostic approach of the true tail. BMJ Case Rep. 2024; 17(8):e260351. [DOI: 10.1136/bcr-2024-260351] [PMID]
- He K, Wang K, Liu Z, Zhang L, Liu S, Zhang X, Wang Y, et al. Tethered cord syndrome from pediatric and adult perspectives: A comprehensive systematic review of 6135 cases. Neurosurg Focus. 2024; 56(6):E18. [DOI: 10.3171/2024.3.FOCUS23899] [PMID]
- Wang J, Zhou Q, Fu Z, Xiao X, Lu Y, Zhang G, Zhang H. MRI evaluation of fetal tethered-cord syndrome: Correlation with ultrasound findings and clinical follow-up after birth. Clin Radiol. 2021; 76(4):314.e1-314.e8. [DOI: 10.1016/j.crad.2020.12.010] [PMID]
- Turk CC, Kara NN, Bacanli A. The human tail: A simple skin appendage or cutaneous stigma of an anomaly? Turk Neurosurg. 2016; 26(1):140-5. [DOI: 10.5137/1019-5149.JTN.12199-14.1] [PMID]
- Vetrano IG, Barbotti A, Erbetta A, Mariani S, Bova SM, Colombo L, et al. Multidisciplinary Management of Children with Occult Spinal Dysraphism: A Comprehensive Journey from Birth to Adulthood. Children (Basel). 2022; 9(10):1546. [DOI: 10.3390/children9101546] [PMID]
- Farhadi R, Kazemi SA, Godazandeh F. Lumbosacral tuft of hair as a key stigma for early detection of occult spinal dysraphism: A case report of diastematomyelia with tethered cord in a newborn. Clin Case Rep. 2024; 12(9):e9267. [DOI:10.1002/ccr3.9267] [PMID]
- Deo RC, Acharya A, Mahapatra AK, Panigrahi S. Thoracic bony human tail in a newborn baby: A rare case and review of literature. Childs Nerv Syst. 2023; 39(11):3317-21. [DOI:10.1007/s00381-023-06013-z] [PMID]
- Kabra NS, Srinivasan G, Udani RH. True tail in a neonate. Indian Pediatr. 1999; 36(7):712-3. [PMID]
- Kansal R, Agrawal N, Khare S, Khare A, Jain S, Singhal BM. Newborn with a tail-a genetic throwback. Peoples J Sci Res. 2010; 3:15-7. [Link]
- Sarmast AH, Showkat HI, Mir SF, Ahmad SR, Bhat AR, Kirmani AR. Human born with a tail: A case report. South Afr J Child Health. 2013; 7(1):38-9. [Link]
- Nage AR, Bendre PS, D'souza F, Palse N. A case of human tail syndrome with spinal dysraphism. Sri Lanka J Child Health. 2017; 46(1):5. [Link]
- Pillai MK, Nair ST. A true human tail in a neonate: Case report and literature review. Sultan Qaboos Univ Med J. 2017; 17(1):e109-11. [DOI:10.18295/squmj.2016.17.01.020] [PMID]
- Canaz G, Akkoyun N, Emel E, Cevik OM, Baydin S, Gokcedag A. A rare case of “human tail” associated with lipomyelomeningocele and tethered cord. J Pediatr Neurosci. 2018; 13(2):241-4. [DOI:10.4103/JPN.JPN_74_17] [PMID]
- Ahmad A, Bangash MH, Saleem I. Human tail - a rare anatomical mystery: A case report. J Pediatr Adolesc Surg. 2020; 1(1):44-6. [DOI:10.46831/jpas.v1i1.3]
- Vaid A, Thakur AS, Bajaj M. A true neonatal tail with limb defect: A rare case report. Pediatr Oncall J. 2020; 17:58-9. [DOI:10.7199/ped.oncall.2020.21]
- Daib A, Saadi C, Rabiaa Ben Abdallah R, Barguellil M, Hellal Y, Trabelsi F, et al. A rare case of lumbosacrococcygeal mass in newborn: A human tail. J Surg Case Rep. 2020; 2020(11):rjaa426. [DOI:10.1093/jscr/rjaa426]
- Algallaf SA, Alobaid MA, Alghamdi SG, Alanazi KS. A true human tail in a neonate born in Saudi Arabia: A case report. Cureus. 2024; 16(1):e53346. [DOI:10.7759/cureus.53346] [PMID]
- Lu FL, Wang PJ, Teng RJ, Yau KI. The human tail. Pediatr Neurol. 1998; 19(3):230-3. [DOI:10.1016/S0887-8994(98)00046-0] [PMID]
- Santos C, Marshall AR, Murray A, Metcalfe K, Narayan P, de Castro SCP, Maniou E, et al. Spinal neural tube formation and tail development in human embryos. Elife. 2024; 12:RP88584. [DOI: 10.7554/eLife.88584] [PMID]
- Baskurt O, Hicdonmez T, Gazioglu MN. Aberrant dorsal nerve root as a concomitant cause of spinal cord tethering associated with a dorsal type lipomyelomeningocele in a child with caudal agenesis. Niger J Clin Pract. 2024; 27(4):537-40. [DOI: 10.4103/njcp.njcp_838_23] [PMID]
- Reghunath A, Ghasi RG, Aggarwal A. Unveiling the tale of the tail: An illustration of spinal dysraphisms. Neurosurg Rev. 2021; 44(1):97-114. [DOI: 10.1007/s10143-019-01215-z] [PMID]
- Menezes AH, Seaman SC, Iii MAH, Hitchon PW, Takacs EB. Tethered spinal cord syndrome in adults in the MRI era: Recognition, pathology, and long-term objective outcomes. J Neurosurg Spine. 2021; 34(6):942-54. [DOI:10.3171/2020.9.SPINE201453] [PMID]
- Mosleh MM, Sohn MJ. Optimizing Therapeutic Strategies for Syringomyelia Associated with Tethered Cord Syndrome: A Comprehensive Review. Children (Basel). 2024; 11(8):961. [DOI: 10.3390/children11080961] [PMID]
- Miller R, Mackenzie A, Welman T, Bodger S, Horwitz MD. Establishing the psychological impact of congenital upper limb differences on parents and families. J Hand Surg Eur Vol. 2025; 50(2):247-52. [DOI: 10.1177/17531934241256793] [PMID]
- Islam MN, Adhikari SB, Alam MM, Dilshad Munmun UH. Experience with human tail and its outcome. Afr J Paediatr Surg. 2021; 18(1):43-6. [DOI: 10.4103/ajps.AJPS_48_20] [PMID]
Type of Study: Case & Review |
Subject:
Neonatology
Received: 2025/02/15 | Accepted: 2025/03/17 | Published: 2025/04/1
Received: 2025/02/15 | Accepted: 2025/03/17 | Published: 2025/04/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |