Volume 13, Issue 3 (7-2025)
J. Pediatr. Rev 2025, 13(3): 225-234 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hullumani S, Qureshi I, Raghumahant R. Effect of Physiotherapy Intervention on Neonates With Respiratory Distress Syndrome: A Systematic Review of Evidence in Neonates. J. Pediatr. Rev 2025; 13 (3) :225-234
URL: http://jpr.mazums.ac.ir/article-1-728-en.html
URL: http://jpr.mazums.ac.ir/article-1-728-en.html
1- Department of Paediatric Physiotherapy, Ravi Nair Physiotherapy College, Datta Meghe Institute Higher Education and Research (DU), SWardha, India. , sharathhullumani@gmail.com
2- Department of Neuro Physiotherapy, Ravi Nair Physiotherapy College, Datta Meghe Institute Higher Education and Research (DU), Wardha, India.
2- Department of Neuro Physiotherapy, Ravi Nair Physiotherapy College, Datta Meghe Institute Higher Education and Research (DU), Wardha, India.
Keywords: Neonatal respiratory distress syndrome (NRDS), Chest physiotherapy, Respiratory distress, Infantile respiratory distress syndrome, Newborn
Full-Text [PDF 688 kb]
(987 Downloads)
| Abstract (HTML) (1194 Views)
Full-Text: (685 Views)
Introduction
About 40–60% of preterm neonates born before 28 weeks of gestation and 15–30% of those born between 32 and 36 weeks of gestation suffer from neonatal respiratory distress syndrome (NRDS), a major cause of morbidity and mortality in these babies. The main cause of respiratory distress in infants, NRDS, presents a complex range of challenges for medical professionals, requiring early diagnosis and treatment to maximize results. Premature babies, especially those born before 28 weeks of gestation, have a higher prevalence of NRDS, which has an inverse relationship with gestational age. Hyaline membrane disease, also known as NRDS, is a serious respiratory illness that primarily affects premature babies. The disease is characterized by decreased lung function due to the absence of pulmonary surfactant, which is necessary to maintain alveolar stability and prevent collapse during expiration [1-3]. Although improvements in newborn treatment, such as mechanical ventilation and surfactant therapy, have increased survival rates, improving supportive therapies to improve respiratory function and lower complications remains a top objective [4].
The use of physiotherapy procedures as supplemental treatments for neonatal respiratory problems has grown in popularity. The goals of techniques, including vibration, posture, respiratory exercises, and chest physical therapy, are to increase lung capacity, improve mucus clearance, and maximize oxygenation [5]. Although PT therapies are frequently used in neonatal facilities, there is still conflicting information regarding their efficacy in treating newborns with NRDS. While some studies point to possible hazards, like oxygen desaturation and stress reactions in newborns, others indicate that these therapies may lessen respiratory problems and enhance clinical outcomes [6]. The typical treatment approach for non-reversible dysplasia of the lungs (NRDS) includes the administration of exogenous surfactant to improve lung function and reduce the severity of symptoms. Respiratory support methods, such as mechanical ventilation and continuous positive airway pressure (CPAP), are commonly employed to guarantee proper ventilation and oxygenation. Even after these treatments, some neonates experience significant respiratory problems, which necessitate the use of additional therapeutic techniques to enhance outcomes [7, 8].
It is crucial to collect the existing data in order to assess the efficacy and safety of physiotherapy, given the critical nature of NRDS and the growing interest in this non-invasive supportive intervention. Assessing the effects of physiotherapy therapies on respiratory function and clinical outcomes in newborns with NRDS is the goal of this comprehensive review. A surfactant shortage that results in poor gas exchange and respiratory failure is a hallmark of NRDS. It is a major cause of newborn mortality and morbidity globally and mainly affects preterm infants. The use of surfactants and respiratory support devices, like mechanical ventilation and CPAP are example of current treatments. Despite being frequently incorporated into neonatal care, physiotherapy’s precise function in managing NRDS is yet unknown. The existing literature discusses physiotherapy in neonatal intensive care unit (NICU) settings in general, but does not focus on its use in NRDS. Therefore, a focused review is required to investigate its possible efficacy, safety, and standardization. The purpose of this systematic review was to address the following question: How do clinical outcomes, including oxygenation, respiratory rate, need/duration of ventilation, and death (outcomes), change when physiotherapy interventions (interventions) are compared to normal medical care without physiotherapy (comparisons) in newborns with NRDS (participants)? The study design incorporates cohort, quasi-experimental, and randomized controlled trials.
Methods
The protocol was registered on the International Prospective Register of Systematic Reviews (PROSPERO) under ID: CRD42025635782. It was registered on 22 January 2025).
Research question
In neonates with NRDS, how does physiotherapy intervention compare to standard care without physiotherapy in improving respiratory function, reducing the duration of mechanical ventilation, or decreasing the length of hospital stay?
Data sources
To find papers pertinent to our study issue, we utilized both manual and electronic searches. Four databases—PubMed, Pedro, Medline, and the Cochrane Library—along with clinical trial registries (ClinicalTrials.gov and WHO ICTRP) were searched electronically from 2000 to December 2024. The reference lists of the included studies and conference proceedings were also checked. Although it is acknowledged as a search engine rather than a formal database, Google Scholar was used to supplement the search. Depending on the needs of each database, our search algorithms blended free text and medical subject headings (MeSH). Due to the low quality of the evidence, individual expert views were not included in the data extraction process. Articles that are not published or available in full text were also excluded. The current study conducted the review between October and November 2024, adhering to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines. This adherence ensures that the research is thorough.
The following criteria must be met for the papers to be eligible for the current study:
Population (P): Preterm infants (less than 37 weeks of gestation) with NRDS were included in the review. To guarantee uniformity in pathophysiology and intervention results, term neonates were not included.
Intervention (I): Physiotherapy procedures carried out either after extubation or during mechanical ventilation were covered. This covers treatments, such as early mobilization, posture, airway clearance techniques, and chest physical therapy. Depending on each trial, we clearly indicated whether the therapies were pre-extubation, post-extubation, or both.
Comparison (C): Standard NICU treatment, which may have included mechanical ventilation or CPAP without the use of physiotherapy, was provided to the comparator groups. The included studies were those in which only the intervention group underwent physiotherapy, while the other group received the same ventilatory support. The updated version now provides a detailed description of this distinction.
Normal treatment without physiotherapy: This includes standard medical care for neonates with NRDS, such as surfactant replacement therapy and mechanical ventilation, including invasive ventilation or CPAP.
Supportive treatment: This includes controlling body temperature and managing fluid intake. Other non-physiotherapy therapies, such as medication or surgery, aimed at targeting respiratory function, are also administered to neonates with NRDS.
Outcome measures (O): Oxygen saturation levels (SpO₂), arterial blood gas (ABG) analysis (e.g. PaO₂, PaCO₂, and pH), respiratory rate (breaths per minute), and lung compliance (static or dynamic) were used to quantify respiratory function. Validated scoring methods, such as the Downes or Silverman-Andersen scores, were used to assess the degree of respiratory distress reduction.
Length of hospital stay
Study design: Only RCTs and quasi-experimental studies were included. Cross-sectional and purely observational studies were excluded to maintain focus on intervention effectiveness.
Language: Only English-language research or studies with available translations were eligible for this study due to translation restrictions and timing constraints within the project deadline and the lack of trustworthy translation resources.
Publication date: Studies published from 2000 to 2025 were considered.
Publication type: Both published articles and grey literature.
Study selection
PubMed, Pedro, Medline, and the Cochrane Library were thoroughly searched. Physiotherapy was used, along with MeSH and pertinent keywords such as “infantile respiratory distress syndrome”, “neonatal respiratory distress syndrome”, “respiratory distress syndrome, infant”, “respiratory distress syndrome”, and “new-born”, and “ physiotherapy”, “chest physiotherapy”. To ensure the inclusion of the most recent research, searches were conducted again prior to the final analysis. Additionally, trial registers, investigator contacts, and conference proceedings were searched for unpublished studies. ProQuest Dissertations & Theses Global and Google Scholar were used to consult the grey literature. Medline and the Cochrane Library, employing the MeSH phrases, were used to find other relevant publications. Truncation (*) and Boolean operators (OR, AND) were used for different suffixes.
PRISMA provides guidance on conducting a systematic literature search and documenting the data. Consequently, identifying the pertinent sources is the first step. To find relevant works, a paper search was conducted in the PubMed, Pedro, Medline, and Cochrane Library databases. The search yielded documents from these databases.
Data extraction
The features of the 10 publications examined in this study are compiled in the following section by database and journal, publication date, and research nation. According to PRISMA, screening is the second phase. As a result, every source was examined to rule out any potential duplicates. In this stage, a built-in duplicate detection tool in EndNote software, version 9 was used to find and eliminate duplicate articles, followed by a manual verification step to ensure accuracy. Verifying the final list of documents that satisfied the study’s eligibility requirements was the third step.
We were able to choose documents from the database that were not open access or available in the language. Two calibrated and independent reviewers, Sharath Hullumani and Irshad Qureshi, conducted the study selection in two stages. The first step involved screening abstracts and titles for alignment with the inclusion criteria and research question. In the second stage, the full texts of potentially relevant studies were examined to decide on final inclusion. This procedure was guided by the inclusion and exclusion criteria.
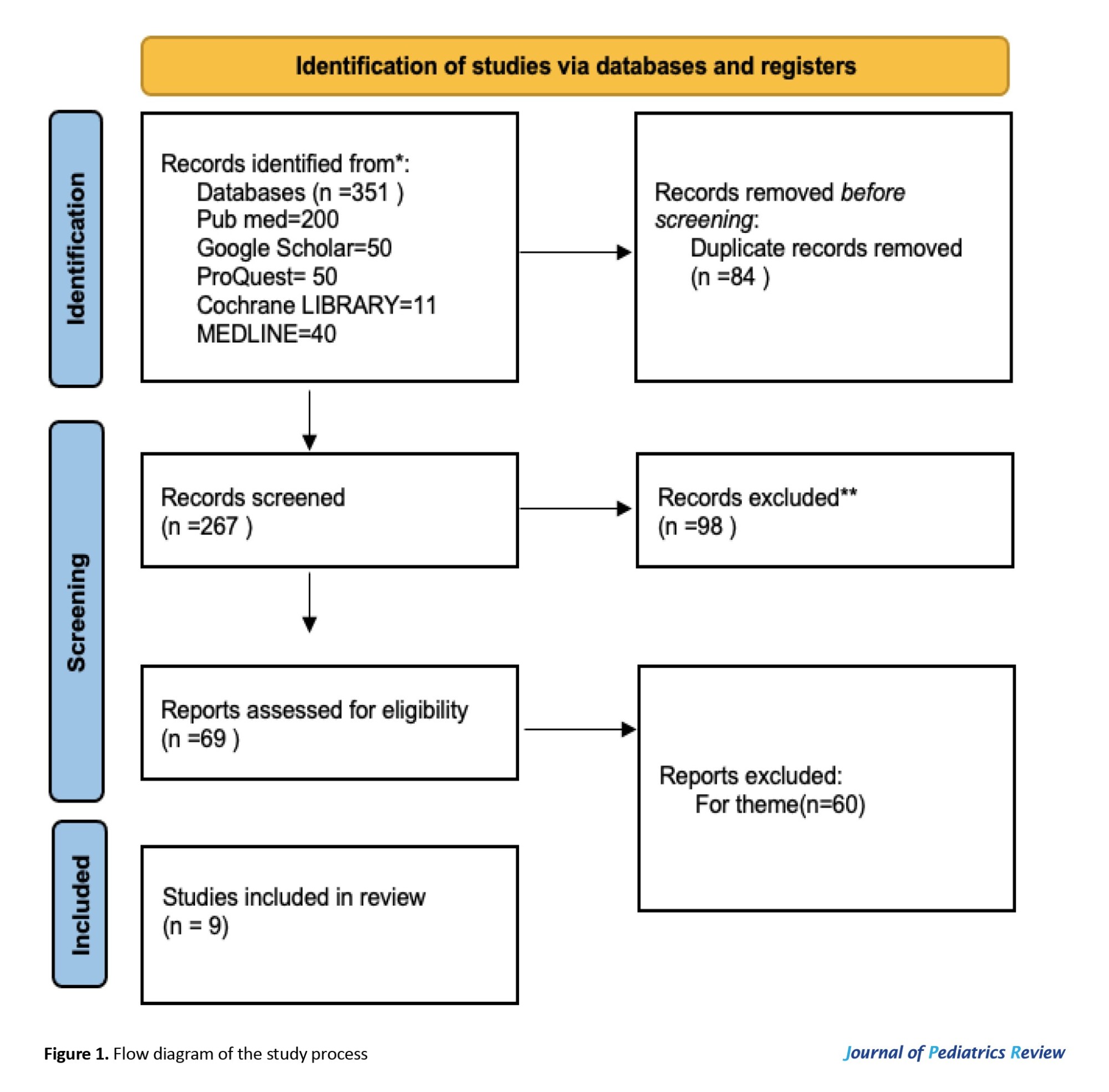
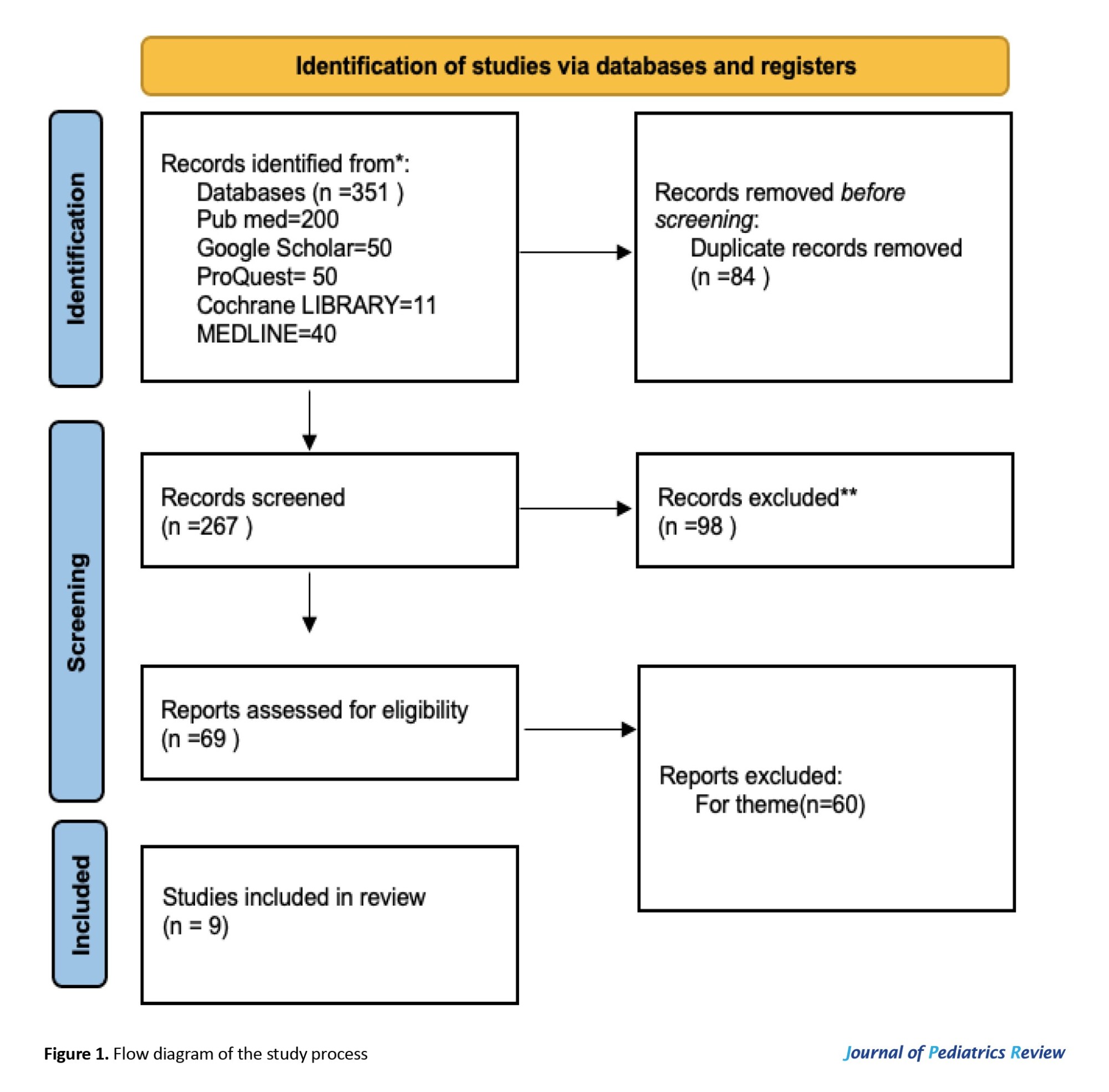
In phase 1, the titles and abstracts of the chosen papers were reviewed by the two reviewers, Sharath Hullumani and Irshad Qureshi. In phase 2, the same reviewers (Sharath Hullumani and Irshad Qureshi) read the full texts of the previously included papers. The selection criteria remained the same as those from the first round. A third reviewer (Raghuveer Raghumahanti) made the final decision in case of any disputes. A summary of the study selection procedure is provided in Figure 1.
Quality assessment
The PEDro scale for cross-sectional and experimental research and the Newcastle–Ottawa scale (NOS) were used to evaluate the papers’ quality. With a maximum of nine points, the NOS is divided into three sections: Result (up to three points), comparability (up to two points), and patient selection (up to four points). The PEDro scale consists of eleven questions [9, 10].
Results
Nine trials involving 398 preterm newborns diagnosed with respiratory-related problems or NRDS were included. The range of gestational ages was 28–37 weeks. The physiotherapy interventions that varied among the studies included cardio-respiratory physiotherapy, reflex rolling, lung squeeze techniques, chest physiotherapy, and structured early interventions.
Selection process and data collection process
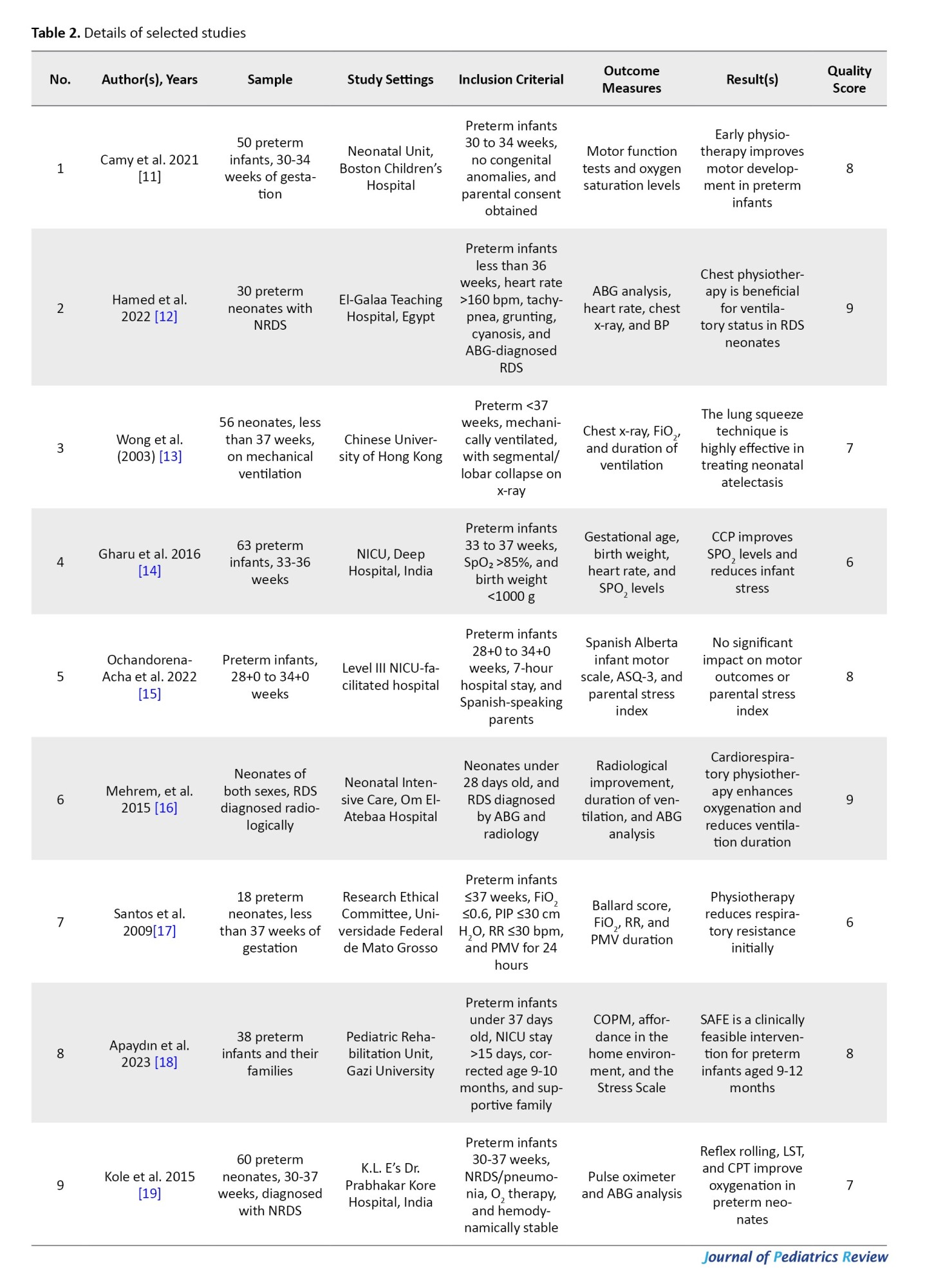
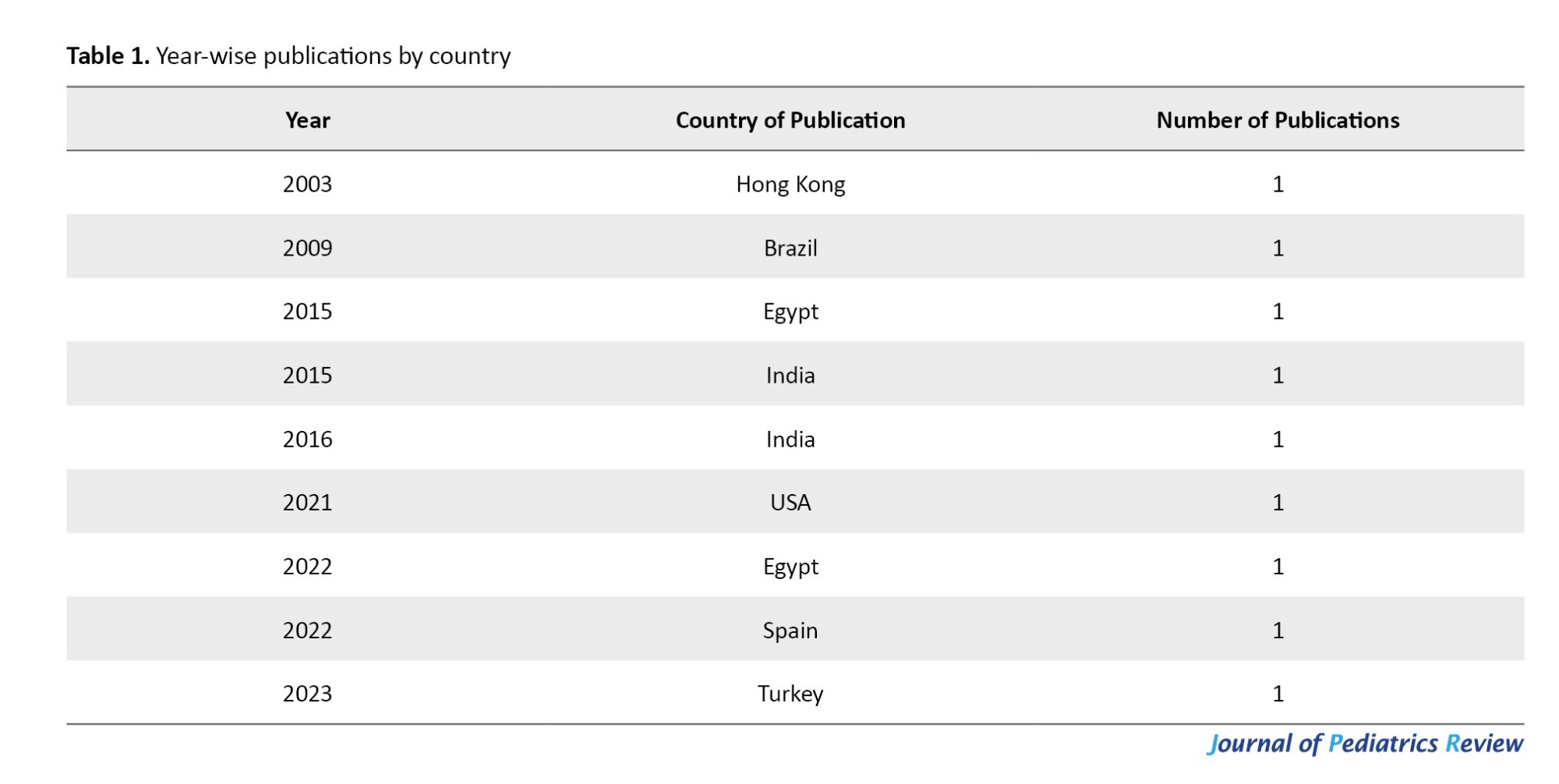
Table 1 and Figure 2 display the total number of publications and the distribution of articles by country in the NRDS domain throughout the year.
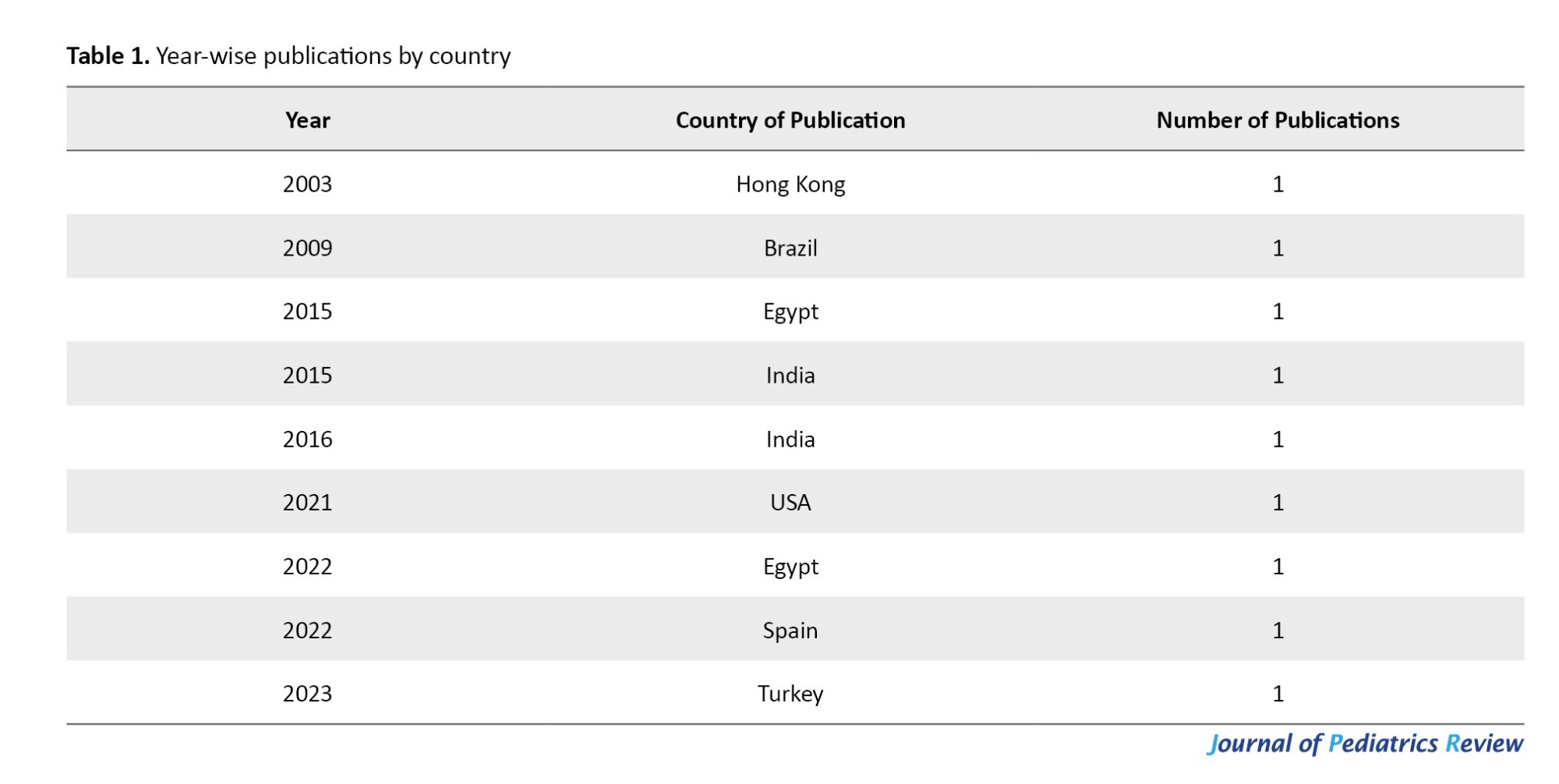
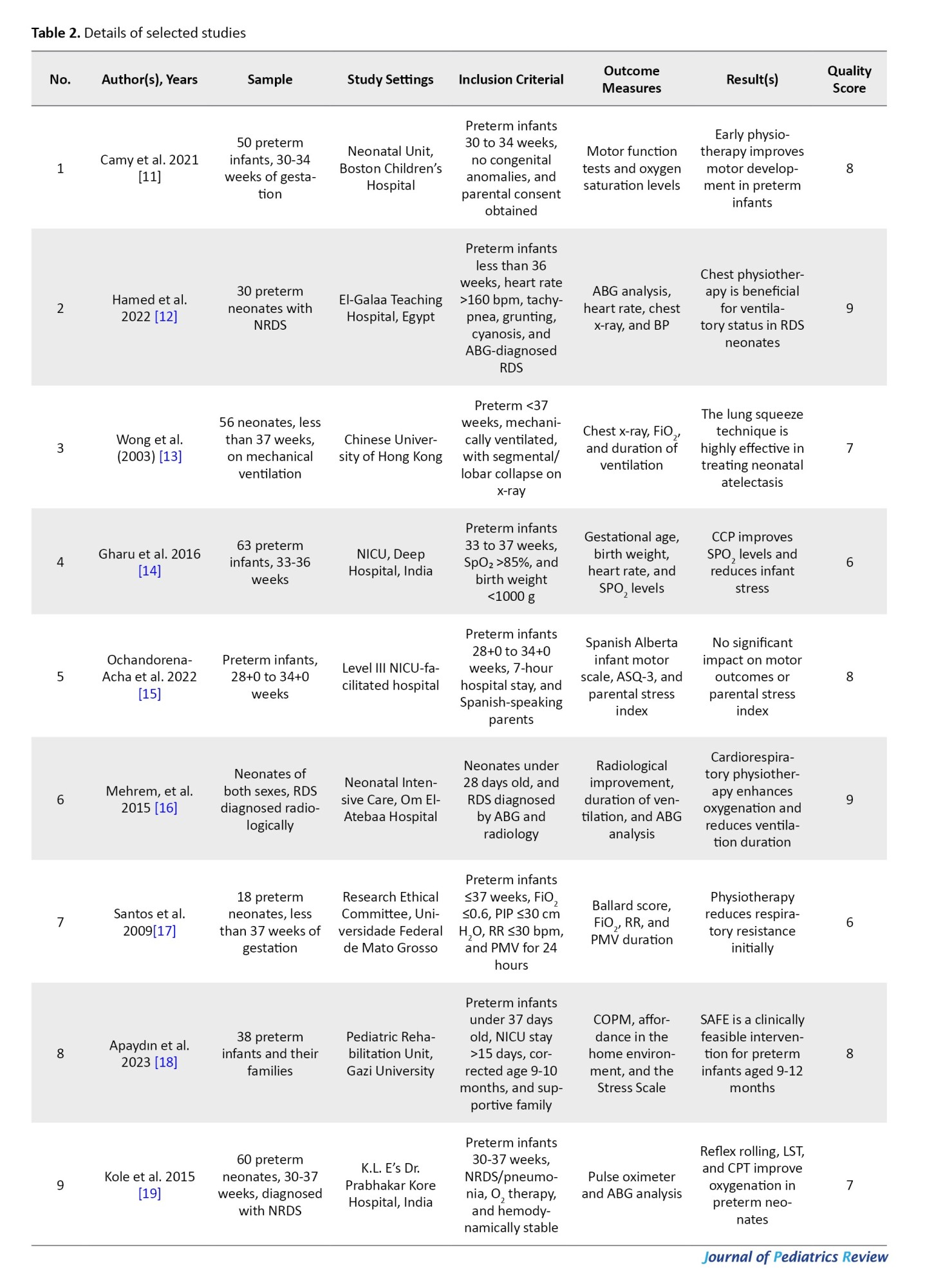
The graph shows a notable decline due to restricted access to download the articles; however, the overall trend indicates that it is one of the newer themes in neonatology. Table 2 presents the details of the selected studies.
The table and graphs show trends in studies conducted across different countries and offer a thorough summary of year-by-year publications on physiotherapy therapies in NRDS. The table aids in identifying research contributions worldwide by categorizing studies by year, number of publications, and place of origin.
The line graph depicting publication trends by nation indicates increased research activity in recent years, particularly from Spain, Romania, India, Egypt, the UK, and the USA. The bar graph offers a more complete picture of the annual number of publications, showing a noticeable increase in research, especially in 2022 and 2025, suggesting that neonatal physiotherapy is becoming increasingly popular. Overall, these visuals demonstrate the growing emphasis on physiotherapy for neonatal RDS, highlighting both international contributions and historical research patterns.
Discussion
A major problem in newborn care remains NRDS, especially in preterm infants who are more susceptible to pulmonary issues because of their immature lungs. Due to the immature lung architecture and surfactant deficiency, NRDS continues to be a significant cause of morbidity and mortality in premature infants. The current study assessed the effectiveness of physiotherapy therapies, when used in conjunction with standard care, in improving respiratory outcomes in newborns with NRDS. Key outcomes included standardized respiratory distress scores (e.g. Downes, Silverman-Andersen), respiratory rate, lung compliance, arterial blood gas (ABG) measurements, and oxygen saturation (SpO₂). A critical review of the research suggests that physiotherapy may be beneficial; however, results remain inconsistent, and methodological limitations prevent firm conclusions from being drawn.
Physiotherapy therapies, including reflex rolling, lung squeeze techniques, chest vibration, and the PROMPT strategy, were linked to statistically significant increases in SpO₂ in multiple investigations. For example, post-intervention SpO₂ values were higher in the groups studied by Kole et al. [19] and Hamed et al. [11] compared to those receiving standard treatment. Greater lung expansion, enhanced alveolar ventilation, and improved mucus clearance are likely the reasons for these gains. Heterogeneity in results was attributed to differences in physiotherapy procedures, session length, and timing (e.g. before or after extubation). Despite having a small sample size, Wong et al. [13] further highlighted the advantages of lung squeeze therapy over conventional techniques.
More unbiased information about gas exchange efficiency was obtained through ABG analysis. According to research conducted by Mehrem et al. [16] and Sharath et al. [7], interventions had positive effects, improving pH and PaO₂ while lowering PaCO₂. These enhancements indicate physiotherapy’s potential contribution to stabilizing acid-base balance and maximizing alveolar ventilation. However, contradictory results by Ochandorena-Acha et al. [15] suggest that individual approaches, the severity of NRDS, and the timing of interventions may influence efficacy. Notably, this underscores the need for future studies to standardize physiotherapy protocols.
Studies by Apaydın et al. [18] found that physiotherapy interventions dramatically decreased respiratory rate, a non-invasive indicator of respiratory distress. These results suggest better lung mechanics and less respiratory effort. These findings were further confirmed by improvements in lung compliance, as demonstrated by dos Santos et al. [17]. However, the interpretation of therapeutic relevance was limited because the majority of trials did not specify whether improvements were observed during spontaneous breathing or with ventilatory support.
Several studies assessed the severity of symptoms using validated respiratory distress ratings, such as the Downes and Silverman-Andersen scores. Significant score reductions after intervention were reported by Mehrem et al. [16] suggesting symptomatic alleviation. These rating systems have a strong correlation with clinical outcomes and are useful in NICU settings.
Despite the encouraging patterns displayed in many studies, there was a moderate to high overall risk of bias due to small sample sizes, a lack of blinding, and selective outcome reporting. Furthermore, some studies used cross-sectional or quasi-experimental designs without a clear rationale, or they lacked suitable control groups, which limited the ability to draw conclusions about causality. This diminishes the strength of the conclusions and emphasizes the necessity of conducting thorough RCTs in the field. Notably, few studies explicitly compared the two groups, and reports on the efficacy of physiotherapy in comparison to standard care—such as CPAP or mechanical ventilation—were varied.
Although the majority of the included studies demonstrate the potential of physiotherapy, direct comparisons are complicated by the significant variation in interventions, populations (term vs preterm), and outcome categories. This diversity restricts generalizability and reflects the absence of a cohesive therapeutic strategy.
Clinical implications and future directions
The combined data from this research highlights how physiotherapy therapies may help improve respiratory function in newborns with NRDS. The benefits of physiotherapy in promoting pulmonary function and lessening the intensity of respiratory distress are evidenced by the noted increases in SpO₂, ABG values, respiratory rate, lung compliance, and validated distress levels. There is a need for more research on the best intervention procedures, timing, and patient selection criteria, as some studies, including Ochandorena-Acha et al. [15], reported no discernible benefits.
Conclusion
In summary, the findings of this systematic review indicate that physiotherapy interventions, including post-extubation support, airway clearance techniques, and gentle positioning, can serve as useful supplements to standard NICU care in the treatment of NRDS, particularly in preterm infants. These therapies should be administered by trained neonatal physiotherapists and customized based on the infant’s clinical stability, gestational age, and respiratory condition. Gentle, non-invasive methods are advised to prevent complications or physiological stress. Neonatologists and physiotherapists must collaborate closely as a multidisciplinary team to integrate physiotherapy into standard NICU protocols. Based on the currently available evidence, developing standardized protocols for the use of physical therapy in NRDS care may enhance clinical outcomes, especially in situations where access to prolonged mechanical ventilation is limited.
Standardizing physiotherapy methods, carrying out extensive randomized controlled trials, and assessing the long-term effects of physiotherapy interventions in neonates with NRDS should be the main objectives of future research. Furthermore, utilizing advanced monitoring techniques such as lung ultrasonography and pulmonary function testing may enhance the accuracy of outcome evaluations.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization, methodology and investigation: Sharath Hullumani and Irshad Qureshi; Data curation, software and writing: Sharath Hullumani; Funding acquisition and project administration: Sharath Hullumani and Raghumahanti Raghuveer; Supervision: Irshad Qureshi and Raghumahanti Raghuveer; Validation and visualization: All authors.
Conflicts of interest
The authors declared no conflict of interest.
References
About 40–60% of preterm neonates born before 28 weeks of gestation and 15–30% of those born between 32 and 36 weeks of gestation suffer from neonatal respiratory distress syndrome (NRDS), a major cause of morbidity and mortality in these babies. The main cause of respiratory distress in infants, NRDS, presents a complex range of challenges for medical professionals, requiring early diagnosis and treatment to maximize results. Premature babies, especially those born before 28 weeks of gestation, have a higher prevalence of NRDS, which has an inverse relationship with gestational age. Hyaline membrane disease, also known as NRDS, is a serious respiratory illness that primarily affects premature babies. The disease is characterized by decreased lung function due to the absence of pulmonary surfactant, which is necessary to maintain alveolar stability and prevent collapse during expiration [1-3]. Although improvements in newborn treatment, such as mechanical ventilation and surfactant therapy, have increased survival rates, improving supportive therapies to improve respiratory function and lower complications remains a top objective [4].
The use of physiotherapy procedures as supplemental treatments for neonatal respiratory problems has grown in popularity. The goals of techniques, including vibration, posture, respiratory exercises, and chest physical therapy, are to increase lung capacity, improve mucus clearance, and maximize oxygenation [5]. Although PT therapies are frequently used in neonatal facilities, there is still conflicting information regarding their efficacy in treating newborns with NRDS. While some studies point to possible hazards, like oxygen desaturation and stress reactions in newborns, others indicate that these therapies may lessen respiratory problems and enhance clinical outcomes [6]. The typical treatment approach for non-reversible dysplasia of the lungs (NRDS) includes the administration of exogenous surfactant to improve lung function and reduce the severity of symptoms. Respiratory support methods, such as mechanical ventilation and continuous positive airway pressure (CPAP), are commonly employed to guarantee proper ventilation and oxygenation. Even after these treatments, some neonates experience significant respiratory problems, which necessitate the use of additional therapeutic techniques to enhance outcomes [7, 8].
It is crucial to collect the existing data in order to assess the efficacy and safety of physiotherapy, given the critical nature of NRDS and the growing interest in this non-invasive supportive intervention. Assessing the effects of physiotherapy therapies on respiratory function and clinical outcomes in newborns with NRDS is the goal of this comprehensive review. A surfactant shortage that results in poor gas exchange and respiratory failure is a hallmark of NRDS. It is a major cause of newborn mortality and morbidity globally and mainly affects preterm infants. The use of surfactants and respiratory support devices, like mechanical ventilation and CPAP are example of current treatments. Despite being frequently incorporated into neonatal care, physiotherapy’s precise function in managing NRDS is yet unknown. The existing literature discusses physiotherapy in neonatal intensive care unit (NICU) settings in general, but does not focus on its use in NRDS. Therefore, a focused review is required to investigate its possible efficacy, safety, and standardization. The purpose of this systematic review was to address the following question: How do clinical outcomes, including oxygenation, respiratory rate, need/duration of ventilation, and death (outcomes), change when physiotherapy interventions (interventions) are compared to normal medical care without physiotherapy (comparisons) in newborns with NRDS (participants)? The study design incorporates cohort, quasi-experimental, and randomized controlled trials.
Methods
The protocol was registered on the International Prospective Register of Systematic Reviews (PROSPERO) under ID: CRD42025635782. It was registered on 22 January 2025).
Research question
In neonates with NRDS, how does physiotherapy intervention compare to standard care without physiotherapy in improving respiratory function, reducing the duration of mechanical ventilation, or decreasing the length of hospital stay?
Data sources
To find papers pertinent to our study issue, we utilized both manual and electronic searches. Four databases—PubMed, Pedro, Medline, and the Cochrane Library—along with clinical trial registries (ClinicalTrials.gov and WHO ICTRP) were searched electronically from 2000 to December 2024. The reference lists of the included studies and conference proceedings were also checked. Although it is acknowledged as a search engine rather than a formal database, Google Scholar was used to supplement the search. Depending on the needs of each database, our search algorithms blended free text and medical subject headings (MeSH). Due to the low quality of the evidence, individual expert views were not included in the data extraction process. Articles that are not published or available in full text were also excluded. The current study conducted the review between October and November 2024, adhering to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines. This adherence ensures that the research is thorough.
The following criteria must be met for the papers to be eligible for the current study:
Population (P): Preterm infants (less than 37 weeks of gestation) with NRDS were included in the review. To guarantee uniformity in pathophysiology and intervention results, term neonates were not included.
Intervention (I): Physiotherapy procedures carried out either after extubation or during mechanical ventilation were covered. This covers treatments, such as early mobilization, posture, airway clearance techniques, and chest physical therapy. Depending on each trial, we clearly indicated whether the therapies were pre-extubation, post-extubation, or both.
Comparison (C): Standard NICU treatment, which may have included mechanical ventilation or CPAP without the use of physiotherapy, was provided to the comparator groups. The included studies were those in which only the intervention group underwent physiotherapy, while the other group received the same ventilatory support. The updated version now provides a detailed description of this distinction.
Normal treatment without physiotherapy: This includes standard medical care for neonates with NRDS, such as surfactant replacement therapy and mechanical ventilation, including invasive ventilation or CPAP.
Supportive treatment: This includes controlling body temperature and managing fluid intake. Other non-physiotherapy therapies, such as medication or surgery, aimed at targeting respiratory function, are also administered to neonates with NRDS.
Outcome measures (O): Oxygen saturation levels (SpO₂), arterial blood gas (ABG) analysis (e.g. PaO₂, PaCO₂, and pH), respiratory rate (breaths per minute), and lung compliance (static or dynamic) were used to quantify respiratory function. Validated scoring methods, such as the Downes or Silverman-Andersen scores, were used to assess the degree of respiratory distress reduction.
Length of hospital stay
Study design: Only RCTs and quasi-experimental studies were included. Cross-sectional and purely observational studies were excluded to maintain focus on intervention effectiveness.
Language: Only English-language research or studies with available translations were eligible for this study due to translation restrictions and timing constraints within the project deadline and the lack of trustworthy translation resources.
Publication date: Studies published from 2000 to 2025 were considered.
Publication type: Both published articles and grey literature.
Study selection
PubMed, Pedro, Medline, and the Cochrane Library were thoroughly searched. Physiotherapy was used, along with MeSH and pertinent keywords such as “infantile respiratory distress syndrome”, “neonatal respiratory distress syndrome”, “respiratory distress syndrome, infant”, “respiratory distress syndrome”, and “new-born”, and “ physiotherapy”, “chest physiotherapy”. To ensure the inclusion of the most recent research, searches were conducted again prior to the final analysis. Additionally, trial registers, investigator contacts, and conference proceedings were searched for unpublished studies. ProQuest Dissertations & Theses Global and Google Scholar were used to consult the grey literature. Medline and the Cochrane Library, employing the MeSH phrases, were used to find other relevant publications. Truncation (*) and Boolean operators (OR, AND) were used for different suffixes.
PRISMA provides guidance on conducting a systematic literature search and documenting the data. Consequently, identifying the pertinent sources is the first step. To find relevant works, a paper search was conducted in the PubMed, Pedro, Medline, and Cochrane Library databases. The search yielded documents from these databases.
Data extraction
The features of the 10 publications examined in this study are compiled in the following section by database and journal, publication date, and research nation. According to PRISMA, screening is the second phase. As a result, every source was examined to rule out any potential duplicates. In this stage, a built-in duplicate detection tool in EndNote software, version 9 was used to find and eliminate duplicate articles, followed by a manual verification step to ensure accuracy. Verifying the final list of documents that satisfied the study’s eligibility requirements was the third step.
We were able to choose documents from the database that were not open access or available in the language. Two calibrated and independent reviewers, Sharath Hullumani and Irshad Qureshi, conducted the study selection in two stages. The first step involved screening abstracts and titles for alignment with the inclusion criteria and research question. In the second stage, the full texts of potentially relevant studies were examined to decide on final inclusion. This procedure was guided by the inclusion and exclusion criteria.
In phase 1, the titles and abstracts of the chosen papers were reviewed by the two reviewers, Sharath Hullumani and Irshad Qureshi. In phase 2, the same reviewers (Sharath Hullumani and Irshad Qureshi) read the full texts of the previously included papers. The selection criteria remained the same as those from the first round. A third reviewer (Raghuveer Raghumahanti) made the final decision in case of any disputes. A summary of the study selection procedure is provided in Figure 1.
Quality assessment
The PEDro scale for cross-sectional and experimental research and the Newcastle–Ottawa scale (NOS) were used to evaluate the papers’ quality. With a maximum of nine points, the NOS is divided into three sections: Result (up to three points), comparability (up to two points), and patient selection (up to four points). The PEDro scale consists of eleven questions [9, 10].
Results
Nine trials involving 398 preterm newborns diagnosed with respiratory-related problems or NRDS were included. The range of gestational ages was 28–37 weeks. The physiotherapy interventions that varied among the studies included cardio-respiratory physiotherapy, reflex rolling, lung squeeze techniques, chest physiotherapy, and structured early interventions.
Selection process and data collection process
Table 1 and Figure 2 display the total number of publications and the distribution of articles by country in the NRDS domain throughout the year.
The graph shows a notable decline due to restricted access to download the articles; however, the overall trend indicates that it is one of the newer themes in neonatology. Table 2 presents the details of the selected studies.
The table and graphs show trends in studies conducted across different countries and offer a thorough summary of year-by-year publications on physiotherapy therapies in NRDS. The table aids in identifying research contributions worldwide by categorizing studies by year, number of publications, and place of origin.
The line graph depicting publication trends by nation indicates increased research activity in recent years, particularly from Spain, Romania, India, Egypt, the UK, and the USA. The bar graph offers a more complete picture of the annual number of publications, showing a noticeable increase in research, especially in 2022 and 2025, suggesting that neonatal physiotherapy is becoming increasingly popular. Overall, these visuals demonstrate the growing emphasis on physiotherapy for neonatal RDS, highlighting both international contributions and historical research patterns.
Discussion
A major problem in newborn care remains NRDS, especially in preterm infants who are more susceptible to pulmonary issues because of their immature lungs. Due to the immature lung architecture and surfactant deficiency, NRDS continues to be a significant cause of morbidity and mortality in premature infants. The current study assessed the effectiveness of physiotherapy therapies, when used in conjunction with standard care, in improving respiratory outcomes in newborns with NRDS. Key outcomes included standardized respiratory distress scores (e.g. Downes, Silverman-Andersen), respiratory rate, lung compliance, arterial blood gas (ABG) measurements, and oxygen saturation (SpO₂). A critical review of the research suggests that physiotherapy may be beneficial; however, results remain inconsistent, and methodological limitations prevent firm conclusions from being drawn.
Physiotherapy therapies, including reflex rolling, lung squeeze techniques, chest vibration, and the PROMPT strategy, were linked to statistically significant increases in SpO₂ in multiple investigations. For example, post-intervention SpO₂ values were higher in the groups studied by Kole et al. [19] and Hamed et al. [11] compared to those receiving standard treatment. Greater lung expansion, enhanced alveolar ventilation, and improved mucus clearance are likely the reasons for these gains. Heterogeneity in results was attributed to differences in physiotherapy procedures, session length, and timing (e.g. before or after extubation). Despite having a small sample size, Wong et al. [13] further highlighted the advantages of lung squeeze therapy over conventional techniques.
More unbiased information about gas exchange efficiency was obtained through ABG analysis. According to research conducted by Mehrem et al. [16] and Sharath et al. [7], interventions had positive effects, improving pH and PaO₂ while lowering PaCO₂. These enhancements indicate physiotherapy’s potential contribution to stabilizing acid-base balance and maximizing alveolar ventilation. However, contradictory results by Ochandorena-Acha et al. [15] suggest that individual approaches, the severity of NRDS, and the timing of interventions may influence efficacy. Notably, this underscores the need for future studies to standardize physiotherapy protocols.
Studies by Apaydın et al. [18] found that physiotherapy interventions dramatically decreased respiratory rate, a non-invasive indicator of respiratory distress. These results suggest better lung mechanics and less respiratory effort. These findings were further confirmed by improvements in lung compliance, as demonstrated by dos Santos et al. [17]. However, the interpretation of therapeutic relevance was limited because the majority of trials did not specify whether improvements were observed during spontaneous breathing or with ventilatory support.
Several studies assessed the severity of symptoms using validated respiratory distress ratings, such as the Downes and Silverman-Andersen scores. Significant score reductions after intervention were reported by Mehrem et al. [16] suggesting symptomatic alleviation. These rating systems have a strong correlation with clinical outcomes and are useful in NICU settings.
Despite the encouraging patterns displayed in many studies, there was a moderate to high overall risk of bias due to small sample sizes, a lack of blinding, and selective outcome reporting. Furthermore, some studies used cross-sectional or quasi-experimental designs without a clear rationale, or they lacked suitable control groups, which limited the ability to draw conclusions about causality. This diminishes the strength of the conclusions and emphasizes the necessity of conducting thorough RCTs in the field. Notably, few studies explicitly compared the two groups, and reports on the efficacy of physiotherapy in comparison to standard care—such as CPAP or mechanical ventilation—were varied.
Although the majority of the included studies demonstrate the potential of physiotherapy, direct comparisons are complicated by the significant variation in interventions, populations (term vs preterm), and outcome categories. This diversity restricts generalizability and reflects the absence of a cohesive therapeutic strategy.
Clinical implications and future directions
The combined data from this research highlights how physiotherapy therapies may help improve respiratory function in newborns with NRDS. The benefits of physiotherapy in promoting pulmonary function and lessening the intensity of respiratory distress are evidenced by the noted increases in SpO₂, ABG values, respiratory rate, lung compliance, and validated distress levels. There is a need for more research on the best intervention procedures, timing, and patient selection criteria, as some studies, including Ochandorena-Acha et al. [15], reported no discernible benefits.
Conclusion
In summary, the findings of this systematic review indicate that physiotherapy interventions, including post-extubation support, airway clearance techniques, and gentle positioning, can serve as useful supplements to standard NICU care in the treatment of NRDS, particularly in preterm infants. These therapies should be administered by trained neonatal physiotherapists and customized based on the infant’s clinical stability, gestational age, and respiratory condition. Gentle, non-invasive methods are advised to prevent complications or physiological stress. Neonatologists and physiotherapists must collaborate closely as a multidisciplinary team to integrate physiotherapy into standard NICU protocols. Based on the currently available evidence, developing standardized protocols for the use of physical therapy in NRDS care may enhance clinical outcomes, especially in situations where access to prolonged mechanical ventilation is limited.
Standardizing physiotherapy methods, carrying out extensive randomized controlled trials, and assessing the long-term effects of physiotherapy interventions in neonates with NRDS should be the main objectives of future research. Furthermore, utilizing advanced monitoring techniques such as lung ultrasonography and pulmonary function testing may enhance the accuracy of outcome evaluations.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization, methodology and investigation: Sharath Hullumani and Irshad Qureshi; Data curation, software and writing: Sharath Hullumani; Funding acquisition and project administration: Sharath Hullumani and Raghumahanti Raghuveer; Supervision: Irshad Qureshi and Raghumahanti Raghuveer; Validation and visualization: All authors.
Conflicts of interest
The authors declared no conflict of interest.
References
- Jobe AH, Ikegami M. Mechanisms initiating lung injury in the preterm. Early Hum Dev. 1998; 53(1):81-94. [DOI:10.1016/s0378-3782(98)00045-0] [PMID]
- Choudhary PK, Piparsania S, Sagar U. A study to determine the incidence of respiratory distress syndrome among neonates in a tertiary care hospital. J Adv Med Dent Sci Res. 2020; 8(9):173-5. [DOI:10.21276/jamdsr]
- Kumar A, Bhat BV. Epidemiology of respiratory distress of newborns. Indian J Pediatr. 1996; 63(1):93-8. [DOI:10.1007/BF02823875] [PMID]
- Stylianou-Riga P, Boutsikou T, Kouis P, Kinni P, Krokou M, Ioannou A, et al. Maternal and neonatal risk factors for neonatal respiratory distress syndrome in term neonates in Cyprus: A prospective case-control study. Ital J Pediatr. 2021; 47(1):129. [DOI:10.1186/s13052-021-01086-5] [PMID] [PMCID]
- Igual Blasco A, Piñero Peñalver J, Fernández-Rego FJ, Torró-Ferrero G, Pérez-López J. Effects of chest physiotherapy in preterm infants with respiratory distress syndrome: A systematic review. Healthcare. 2023; 11(8):1091. [DOI:10.3390/healthcare11081091] [PMID] [PMCID]
- Ekhaguere OA, Okonkwo IR, Batra M, Hedstrom AB. Respiratory distress syndrome management in resource limited settings-current evidence and opportunities in 2022. Front Pediatr. 2022; 10:961509. [DOI:10.3389/fped.2022.961509] [PMID] [PMCID]
- Sharath HV, Raghuveer R, Saklecha A, Nadipena PT, HV S, Nadipena PT. The effect of physical rehabilitation on oro-motor stimulation, manual airway clearance, positioning, and tactile stimulation (PROMPT) on neonates with respiratory distress syndrome. Cureus. 16(7):e64656. [DOI:10.7759/cureus.64656]
- Xu H, Xu P. Efficacy analysis of different pulmonary surfactants in premature infants with respiratory distress syndrome. Zhonghua wei Zhong Bing ji jiu yi xue. 2021; 33(2):174-9. [DOI:10.3760/cma.j.cn121430-20201009-00660]
- Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa scale (NOS) for assess- ing the quality if nonrandomized studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute. 2011. [Link]
- de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust J Physiother. 2009; 55(2):129-33. [DOI:10.1016/S0004-9514(09)70043-1] [PMID]
- Camy LF, Mezzacappa MA. Expiratory flow increase technique and acid esophageal exposure in infants born preterm with bronchopulmonary dysplasia. Pediatr Phys Ther. 2011; 23(4):328-33. [DOI:10.1097/PEP.0b013e31823565c3] [PMID]
- S Hamed AE, El Din Mohamed RS. The effectiveness of chest physiotherapy on mechanically ventilated neonates with respiratory distress syndrome: A randomized control trial. J Med Sci Res. 2022; 5(2):9. [DOI:10.4103/jmisr.jmisr_87_21]
- Wong I, Fok TF. Effects of lung squeezing technique on lung mechanics in mechanically-ventilated preterm infants with respiratory distress syndrome. Hong Kong Phys J. 2006; 24(1):39-46. [DOI:10.1016/S1013-7025(07)70007-6]
- Gharu RG. Bhanu effect of vojta therapy and chest physiotherapy on preterm infants with respiratory distress syndrome-an experimental study. Indian J Physio Occup Ther. 2016; 10(72):10-5958. [DOI:10.5958/0973-5674.2016.00122.2]
- Ochandorena-Acha M, Terradas-Monllor M, López Sala L, Cazorla Sánchez ME, Fornaguera Marti M, Muñoz Pérez I, et al. Early physiotherapy intervention program for preterm infants and parents: A randomized, single-blind clinical trial. Children. 2022; 9(6):895. [DOI:10.3390/children9060895] [PMID] [PMCID]
- Mehrem E, El-Mazary AA, Mabrouk MI, Mahmoud R. Study of chest physical therapy effect on full term neonates with primary pneumonia: A clinical trial study. International J Pediatrics. 2018; 6(7):7893-9. [DOI:10.22038/ijp.2018.30883.2721]
- Santos ML de MD, Souza LA de, Batiston AP, Palhares DB. Results of airway clearance techniques in respiratory mechanics of preterm neonates under mechanical ventilation. Rev Bras Ter Intensiva. 2009; 21(2):183-9. [DOI:10.1590/S0103-507X2009000200011] [PMID]
- Apaydın U, Yıldız R, Yıldız A, Acar ŞS, Gücüyener K, Elbasan B. Short-term effects of SAFE early intervention approach in infants born preterm: A randomized controlled single-blinded study. Brain Behav. 2023; 13(10):e3199. [DOI:10.1002/brb3.3199] [PMID] [PMCID]
- Kole J, Metgud D. Effect of lung squeeze technique and reflex rolling on oxygenation in preterm neonates with respiratory problems: A randomized controlled trial. Indian J Health Sci Biomed Res KLEU. 2014; 7(1):15-21. [DOI:10.4103/2349-5006.135028]
Type of Study: Systematic Review |
Subject:
Pediatric Neurology
Received: 2025/02/17 | Accepted: 2025/07/20 | Published: 2025/07/19
Received: 2025/02/17 | Accepted: 2025/07/20 | Published: 2025/07/19
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |