Volume 9, Issue 2 (4-2021)
J. Pediatr. Rev 2021, 9(2): 105-114 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Firooz M, Eidy F, Abbasi Z, Hosseini S J. Parental Factors Affecting the Incidence of Infantile Colic: A Systematic Review. J. Pediatr. Rev 2021; 9 (2) :105-114
URL: http://jpr.mazums.ac.ir/article-1-356-en.html
URL: http://jpr.mazums.ac.ir/article-1-356-en.html
1- Department of Nursing, Esfarayen Faculty of Medical Sciences, Esfarayen, Iran.
2- Department of Biostatistics, Esfarayen Faculty of Medical Sciences, Esfarayen, Iran.
3- Department of Midwifery, School of Nursing and Midwifery, North Khorasan University of Medical Sciences, North Khorasan, Iran.
4- Department of Nursing, Esfarayen Faculty of Medical Sciences, Esfarayen, Iran. , s.j.hoseini2016@gmail.com
2- Department of Biostatistics, Esfarayen Faculty of Medical Sciences, Esfarayen, Iran.
3- Department of Midwifery, School of Nursing and Midwifery, North Khorasan University of Medical Sciences, North Khorasan, Iran.
4- Department of Nursing, Esfarayen Faculty of Medical Sciences, Esfarayen, Iran. , s.j.hoseini2016@gmail.com
Full-Text [PDF 561 kb]
(1482 Downloads)
| Abstract (HTML) (4147 Views)
Full-Text: (1147 Views)
1. Context
nfantile Colic (IC) is a prevalent disease in early infancy that can present significant adverse effects on infants and their families (1). IC refers to uncontrollable crying for more than 3 hours a day, 3 days per week, and 3 consecutive weeks (2). This behavioral phenomenon (i.e. crying & restlessness) usually manifests at the age of 4-16 weeks with the peak of incidence in 6 weeks of age. The prevalence of IC was reported to be 15%-30%. Besides, it is more common in families experiencing childcare for the first time (3, 4, 5). They not only have periods of abdominal pain, excessive crying, and insomnia in early infancy but also may experience behavioral and mood disorders, hyperactivity, and migraine at older ages (6, 7). Additionally, uncontrollable crying causes stress and anxiety in parents and can even impose the risk of abuse on the infant (8). Despite extensive research, the main cause of IC remains unknown; various factors in the infant, such as insufficient neurodevelopment, Gastrointestinal Tract (GIT) disease (the inflammation & imbalance of intestinal flora), and the psychosocial problems of parents have been associated with IC (9, 10). A closer look at the classification of IC risk factors reveals that a number of them are related to infants and others to parents. Parental characteristics, such psychological status, and maternal diet were assessed in different studies with controversy in the obtained data (11, 12, 13).
Identifying parental risk factors is of high significance; a number of these characteristics can be prevented by education and require no pharmacotherapy. Therefore, these factors can reduce or eliminate with precise planning even during pregnancy. For example, the swallowing of air due to improper breastfeeding techniques exacerbates IC symptoms. Accordingly, this issue can be relieved through teaching the correct techniques by the medical staff. However, infant-related factors, such as the conditions of intestinal microbial flora require probiotic (containing beneficial bacteria) administration (14, 15).
Recent review studies on IC revealed that researchers put more emphasis on treatment, especially using probiotics, and pay less attention to the role of the parental factors on IC. Our search also leads to no comprehensive review study that assessed different parental risk factors on IC incidence. Therefore, conducting a review study focusing on parental risk factors that systematically collects information from reliable scientific databases was necessary.
The present study was conducted to investigate related parental risk factors affecting IC incidence. The Population, Intervention, Comparison, and Outcome (PICO) criterion was used to clarify the goal and select appropriate studies for this review. Accordingly, the study population was parents (mother, father, or both) of infants with colic. IC was defined based on Wesel (the rule of three), Rome III and IV criteria, or referrals to physicians due to excessive crying and the lack of other physical problems. The intervention was not applicable for this review study and only observational studies were evaluated. Furthermore, comparisons were conducted between the parents of infants with colic and controls in prospective and case-control as well as cross-sectional studies (if there was a control group). The relevant outcome was considered the studies that have examined parental factors on IC incidence.
2. Evidence Acquisition
We searched major databases, such as PubMed, Web of Science, Scopus, Science Direct, Google Scholar (the first 100 articles), as well as Scientific Information Database (SID) and Magiran (Iranian websites) after selecting the relevant keywords based on Medical Subject Heading (MESH). For example, we used the following search strategy in PubMed database: “((parents(MeSH Terms)) OR (mothers(MeSH Terms))) OR (fathers(MeSH Terms)) AND (causality(MeSH Terms)) OR (risk factors(MeSH Terms)) AND colic(MeSH Terms) AND infant(MeSH Terms)”.
The PRISMA checklist was applied to retrieve the final articles (Figure 1).
.jpg)
The inclusion criteria were as follows: Observational studies (case-control, prospective, & cross-sectional); English or Persian language articles; IC was defined based on Wessel’s criteria and Rome III and IV criteria, or visiting a physician due to the excessive crying of the infant; parental factors affecting IC, i.e. discussed and separately presented in study results, and the availability of the full text of the articles. The exclusion criteria included experimental, letter to the editor, and review studies. No time limitation was considered for searching in databases. The systematic review registration number in the International Prospective Registration of Systematic Reviews (PROSPERO) was CRD42020163518.
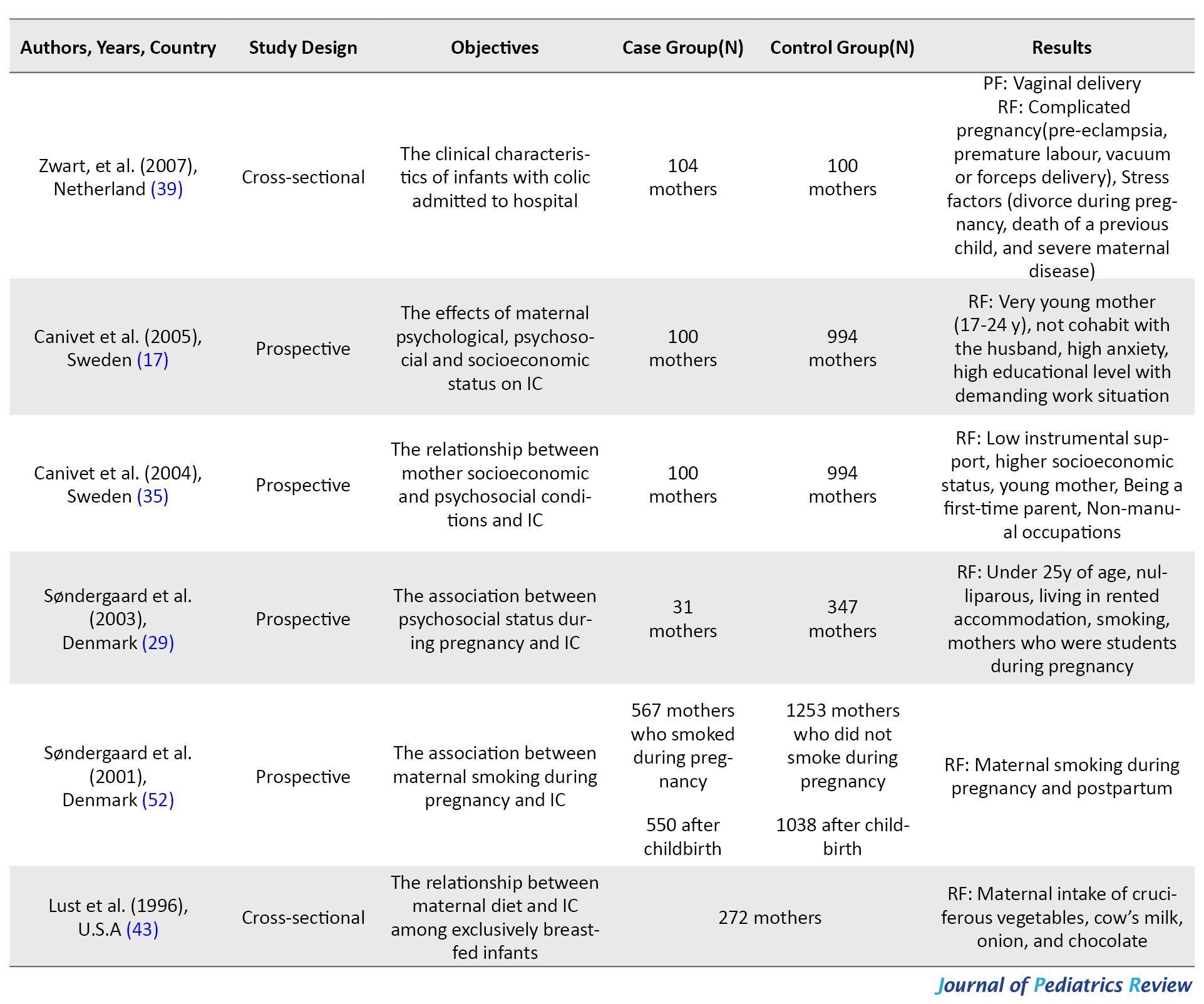
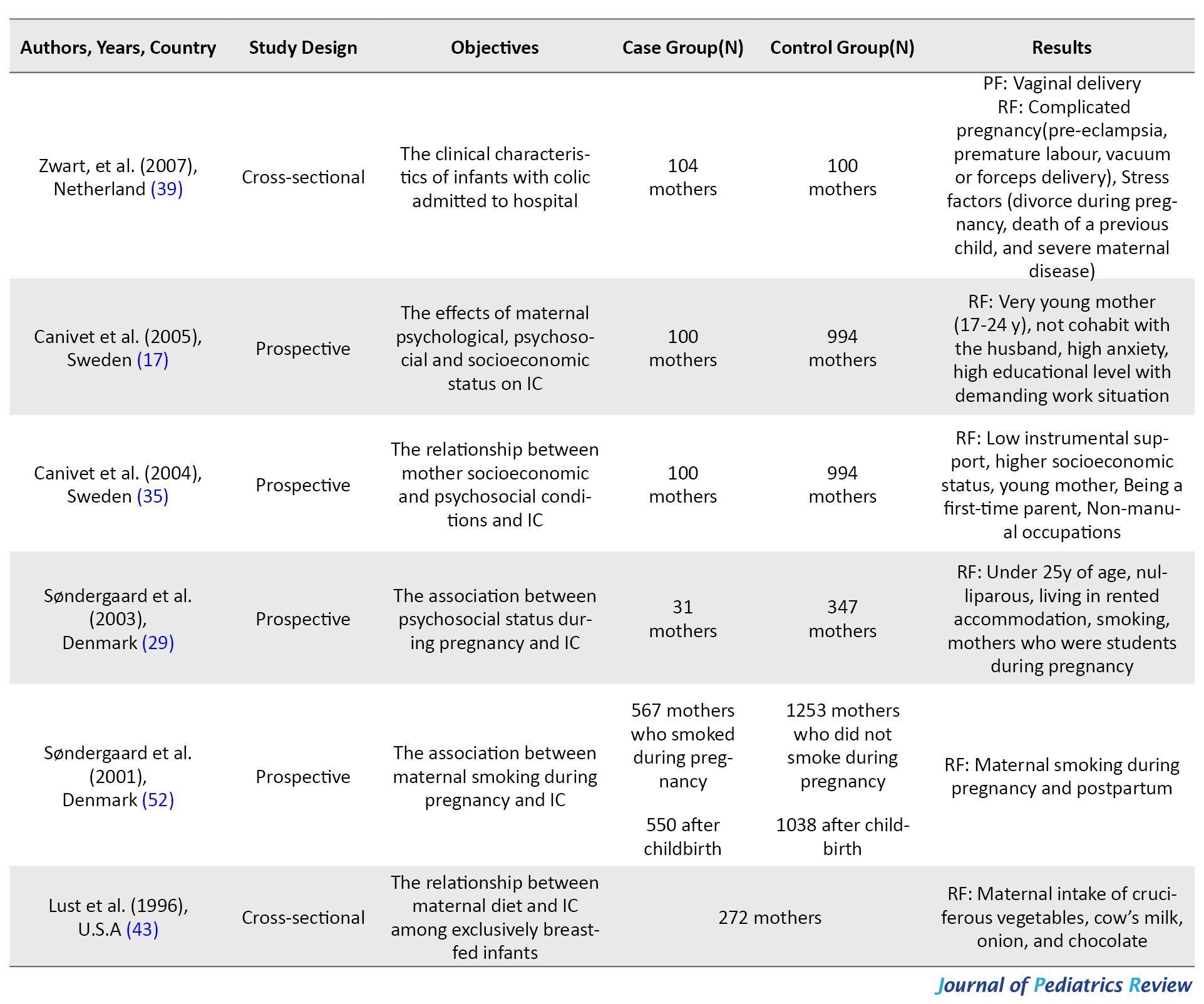
A total of 423 articles were selected from the databases and transferred to the Endnote. Next, duplicate (n=21) and non-relevant articles were removed (n=350). The abstracts of the remaining articles were reviewed in terms of study design and the availability of full text, where 16 articles were omitted in this step. The full texts of the selected articles were assessed according to the clarification of IC definition, parental results, and quality assessment by two researchers; subsequently, 23 articles were excluded (Figure 1). Finally, the data of 18 papers, including the names of the authors, year, country, the purpose of the study, the number of parents participating in the study, and the main results were recorded in Table 1.
.jpg)
Additionally, the main detected risk factors were listed in Table 2.
.jpg)
The compliance of studies with the inclusion and exclusion criteria was evaluated by two researchers (MSc in nursing) and consulting with a statistician. Besides, the quality of articles was checked by the STROBE checklist (Table 3).
.jpg)
This checklist includes 22 items and is suggested for the quality promotion of observational studies. Some items of this checklist are study design, sample selection, data collection, analysis, and potential bias (16). The discrepancy for each item was resolved through a scientific discussion between two researchers. Papers that received scores above the average were included for data extraction. No articles were not excluded due to quality appraisal.
3. Results
Eighteen articles with a total sample size of 13523 (infants’ parents) were selected; accordingly, their results were extracted, including 10 prospective, 6 cross-sectional, and 2 case-control studies. The databases were searched for articles published at any time up to the end of December 2019. Among the studies, 5(27.77%) were from Turkey, 3(16.66%) from Sweden, 3(16.66%) from the United States, 3(16.66%) from the Netherlands, 2(11.11%) from Denmark, and 2(11.11%) from Iran. The data of the conducted studies are summarized in Table 1 based on the objectives, sample size, and results. Eventually, the effective factors were placed in 6 categories, as follows: psychological factors; physical factors; perinatal factors; family socioeconomic status; the type of diet, and taking medications. These factors are described in detail in the discussion section (Table 2).
4. Discussion
The present systematic review examined the parental factors influencing IC incidence. To facilitate the description of the results, we divided them into 6 categories, as follows: psychological, physical, and perinatal factors, family socioeconomic status, maternal diet, and taking medications, i.e. discussed below.
In this category, studies have mostly focused on maternal depression and anxiety during pregnancy and after childbirth (13, 17, 18, 19, 20). Both of them are considered destructive factors in mother-infant interaction and even affect the parents’ relationship with each other (21). Depressed mothers pay less attention to hygiene, including washing their hands before breastfeeding; thus, the germs can be transferred to the infant’s GIT during feeding and cause changes in the normal GIT flora (22). This alteration is considered a contributing factor for IC, and probiotic prescription is a relevant therapeutic strategy (23). In one study, paternal depression was associated with IC (24). The father can influence the development of IC indirectly by interacting with the mother during pregnancy; as well as directly after childbirth by lowering the father-infant interaction and not paying attention to its needs (25).
Another study also found that maternal self-efficacy in breastfeeding is associated with the incidence of IC. This is because of high maternal anxiety and incorrect breastfeeding technique (swallowing large amounts of air by the infant during breastfeeding and not taking the infant’s burp) (26, 27).
In this category, most studies have concentrated on the effect of migraine and smoking (28, 29, 30, 31). An infant who is born to a mother with migraine is hereditarily more prone to IC. The brains of such infants are more sensitive to environmental stimuli and manifest this sensitivity in the form of excessive crying (32). IC is recognized to be associated with the development of migraine in older ages (6).
Moreover, maternal smoking presents various effects on the infant. Tobacco metabolites transmit through the placenta during pregnancy and post-birth by exclusive breastfeeding or secondhand smoke from the environment. As a result, motilin hormone levels are increased in the infant’s GIT; subsequently, it increases its motility and leads to abdominal pain (33, 34). Maternal anxiety affects fetal blood circulation during pregnancy and can lead to decreased infant neuronal development and disturb the mother-infant interaction (35). In this category, other factors, such as young maternal age (17, 18, 29), the experience of the first child (35), and failure to breastfeed (26) were classified. These make the mother incapable of fully managing the infant. For example, if the correct technique of breastfeeding is observed, it can protect the infant against colic (20, 36). In this regard, Kheirkhah et al. suggested that formula feeding increased the risk of IC, compared to exclusive breastfeeding (37).
High Body Mass Index (BMI) (over 25 kg/m2) in pre-pregnancy (28) and vitamin B12 deficiency (13) are also risk factors for IC. Mothers with high BMI are less inclined to interact with their infants (38). They also have less control over their diet status during the breastfeeding period. These conditions can accelerate the IC incidence. Moreover, maternal vitamin deficiency is correlated with IC. Vitamin B12 causes the myelination of neurons; infants born to mothers with vitamin B12 deficiency may encounter a delay in neural system development (38). Delayed neural development is among the IC development causes.
The type of delivery, pregnancy, labor complications and the history of parity were classified in this category (17, 18, 39). Previous studies provided conflicting results concerning the type of delivery; therefore, further research is required in this respect (39, 40). In a study by Heydarian et al., infants with colic were mostly born through Normal Vaginal Delivery (NVD); however, it has been cited as a supportive factor via providing the normal intestinal flora while the infant passes through the birth canal (18, 41).
Moreover, high-risk pregnancies (eclampsia & pre-eclampsia) and delivery (vacuum or preterm delivery) have complications for the mother and infant after delivery. As a result, the mother-infant emotional relationship is affected and the risk of IC incidence is increased. Besides, increased mother parity reduces the risk of IC due to further experiences of coping with anxiety, stress management, and breastfeeding success (17, 42).
The paternal support of the mother is undoubtedly a significant factor that can reduce family anxiety and promote interaction with the infant (17). High social support of the mother is also considered as a supportive factor against IC due to benefiting from the experiences of other mothers (12). Additionally, maternal occupational and educational status fell into this category. Pregnant women who hold academic degrees, are studying in a school, or are involved in intensive and stressful jobs have a higher chance of bearing an infant with colic due to higher anxiety (17, 29).
In one study, parental high socioeconomic status was a contributing factor to IC (35). They indicated more sensitivity toward their infants and more frequently visited physicians’ offices. Furthermore, these parents spend extensive time outside the home, which affects their interaction with each other as well as with the infant.
This category is related to “maternal diet” during breastfeeding, i.e. investigated in two studies (11, 43). In one study, cow milk was found to be effective in the incidence of IC. The protein in cow milk can cause allergy and inflammation in the GIT (44). In some studies, a hypoallergenic diet and the elimination of cow milk were proposed as appropriate options for mothers whose infants experience the signs of atopy (45).
Another study reported that protein intake presented a protective role on IC (46); therefore, further research in this field is warranted. The consumption of vegetables and fruits, such as celery, onions, and bananas (they contain derivatives that can be secreted into breast milk) causes abdominal cramps and increases the risk of IC. Bananas contain indigestible starch; most of which is not hydrolyzed in the GIT. Therefore, it causes bloating in the colon through gas production and eventually leads to abdominal pain (34, 47). In addition, chocolate consumption in one study was also associated with IC, which may be due to the presence of caffeine in its composition (30). The relationship between maternal diet and IC provided contradictory results in different studies; accordingly, further research is needed in this field. Overall, it was recommended to not manipulate the mother’s diet to reduce IC (48).
In the last category, the results of studies mostly referred to the maternal use of antibiotics during pregnancy and postpartum (20, 49). Taking antibiotics, changes the normal flora of the infant’s GIT, i.e. nourished by breast milk. Thus, the disorder in normal microbial flora can cause IC (50). Moreover, maternal iron supplement uptake during pregnancy was associated with IC in one study; however, that was not reported in other studies and requires further investigations (28).
This study had some limitations, including the lack of accurate definition of IC and medium quality in some studies. Furthermore, observational studies were assessed in this research and other types were disregarded.
5. Conclusion
The present review results suggested that several parental factors were related to IC incidence. The most important factors predisposing to IC were parental depression, anxiety, smoking, maternal migraine, young age, primiparity, and low family support. A majority of studies focused on the effect of maternal factors on IC incidence, and paternal role has been less described. These characteristics were classified into 6 categories; these factors should be considered in future studies to implement appropriate prevention programs. However, several factors present conflicting effects on IC and require properly designed studies in the future.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Esfarayen, Faculty of Medical Sciences (Code: IR.ESFARAYENUMS.REC.1398.012). All ethical principles were considered in this article.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, supervision, and methodology: Mahbobeh Firooz, Seyed Javad Hosseini; Investigation, writing -review & editing, writing - original draft: All authors.
Conflicts of interest
The authors declared no conflicts of interest.
References
nfantile Colic (IC) is a prevalent disease in early infancy that can present significant adverse effects on infants and their families (1). IC refers to uncontrollable crying for more than 3 hours a day, 3 days per week, and 3 consecutive weeks (2). This behavioral phenomenon (i.e. crying & restlessness) usually manifests at the age of 4-16 weeks with the peak of incidence in 6 weeks of age. The prevalence of IC was reported to be 15%-30%. Besides, it is more common in families experiencing childcare for the first time (3, 4, 5). They not only have periods of abdominal pain, excessive crying, and insomnia in early infancy but also may experience behavioral and mood disorders, hyperactivity, and migraine at older ages (6, 7). Additionally, uncontrollable crying causes stress and anxiety in parents and can even impose the risk of abuse on the infant (8). Despite extensive research, the main cause of IC remains unknown; various factors in the infant, such as insufficient neurodevelopment, Gastrointestinal Tract (GIT) disease (the inflammation & imbalance of intestinal flora), and the psychosocial problems of parents have been associated with IC (9, 10). A closer look at the classification of IC risk factors reveals that a number of them are related to infants and others to parents. Parental characteristics, such psychological status, and maternal diet were assessed in different studies with controversy in the obtained data (11, 12, 13).
Identifying parental risk factors is of high significance; a number of these characteristics can be prevented by education and require no pharmacotherapy. Therefore, these factors can reduce or eliminate with precise planning even during pregnancy. For example, the swallowing of air due to improper breastfeeding techniques exacerbates IC symptoms. Accordingly, this issue can be relieved through teaching the correct techniques by the medical staff. However, infant-related factors, such as the conditions of intestinal microbial flora require probiotic (containing beneficial bacteria) administration (14, 15).
Recent review studies on IC revealed that researchers put more emphasis on treatment, especially using probiotics, and pay less attention to the role of the parental factors on IC. Our search also leads to no comprehensive review study that assessed different parental risk factors on IC incidence. Therefore, conducting a review study focusing on parental risk factors that systematically collects information from reliable scientific databases was necessary.
The present study was conducted to investigate related parental risk factors affecting IC incidence. The Population, Intervention, Comparison, and Outcome (PICO) criterion was used to clarify the goal and select appropriate studies for this review. Accordingly, the study population was parents (mother, father, or both) of infants with colic. IC was defined based on Wesel (the rule of three), Rome III and IV criteria, or referrals to physicians due to excessive crying and the lack of other physical problems. The intervention was not applicable for this review study and only observational studies were evaluated. Furthermore, comparisons were conducted between the parents of infants with colic and controls in prospective and case-control as well as cross-sectional studies (if there was a control group). The relevant outcome was considered the studies that have examined parental factors on IC incidence.
2. Evidence Acquisition
We searched major databases, such as PubMed, Web of Science, Scopus, Science Direct, Google Scholar (the first 100 articles), as well as Scientific Information Database (SID) and Magiran (Iranian websites) after selecting the relevant keywords based on Medical Subject Heading (MESH). For example, we used the following search strategy in PubMed database: “((parents(MeSH Terms)) OR (mothers(MeSH Terms))) OR (fathers(MeSH Terms)) AND (causality(MeSH Terms)) OR (risk factors(MeSH Terms)) AND colic(MeSH Terms) AND infant(MeSH Terms)”.
The PRISMA checklist was applied to retrieve the final articles (Figure 1).
.jpg)
The inclusion criteria were as follows: Observational studies (case-control, prospective, & cross-sectional); English or Persian language articles; IC was defined based on Wessel’s criteria and Rome III and IV criteria, or visiting a physician due to the excessive crying of the infant; parental factors affecting IC, i.e. discussed and separately presented in study results, and the availability of the full text of the articles. The exclusion criteria included experimental, letter to the editor, and review studies. No time limitation was considered for searching in databases. The systematic review registration number in the International Prospective Registration of Systematic Reviews (PROSPERO) was CRD42020163518.
A total of 423 articles were selected from the databases and transferred to the Endnote. Next, duplicate (n=21) and non-relevant articles were removed (n=350). The abstracts of the remaining articles were reviewed in terms of study design and the availability of full text, where 16 articles were omitted in this step. The full texts of the selected articles were assessed according to the clarification of IC definition, parental results, and quality assessment by two researchers; subsequently, 23 articles were excluded (Figure 1). Finally, the data of 18 papers, including the names of the authors, year, country, the purpose of the study, the number of parents participating in the study, and the main results were recorded in Table 1.
.jpg)
Additionally, the main detected risk factors were listed in Table 2.
.jpg)
The compliance of studies with the inclusion and exclusion criteria was evaluated by two researchers (MSc in nursing) and consulting with a statistician. Besides, the quality of articles was checked by the STROBE checklist (Table 3).
.jpg)
This checklist includes 22 items and is suggested for the quality promotion of observational studies. Some items of this checklist are study design, sample selection, data collection, analysis, and potential bias (16). The discrepancy for each item was resolved through a scientific discussion between two researchers. Papers that received scores above the average were included for data extraction. No articles were not excluded due to quality appraisal.
3. Results
Eighteen articles with a total sample size of 13523 (infants’ parents) were selected; accordingly, their results were extracted, including 10 prospective, 6 cross-sectional, and 2 case-control studies. The databases were searched for articles published at any time up to the end of December 2019. Among the studies, 5(27.77%) were from Turkey, 3(16.66%) from Sweden, 3(16.66%) from the United States, 3(16.66%) from the Netherlands, 2(11.11%) from Denmark, and 2(11.11%) from Iran. The data of the conducted studies are summarized in Table 1 based on the objectives, sample size, and results. Eventually, the effective factors were placed in 6 categories, as follows: psychological factors; physical factors; perinatal factors; family socioeconomic status; the type of diet, and taking medications. These factors are described in detail in the discussion section (Table 2).
4. Discussion
The present systematic review examined the parental factors influencing IC incidence. To facilitate the description of the results, we divided them into 6 categories, as follows: psychological, physical, and perinatal factors, family socioeconomic status, maternal diet, and taking medications, i.e. discussed below.
In this category, studies have mostly focused on maternal depression and anxiety during pregnancy and after childbirth (13, 17, 18, 19, 20). Both of them are considered destructive factors in mother-infant interaction and even affect the parents’ relationship with each other (21). Depressed mothers pay less attention to hygiene, including washing their hands before breastfeeding; thus, the germs can be transferred to the infant’s GIT during feeding and cause changes in the normal GIT flora (22). This alteration is considered a contributing factor for IC, and probiotic prescription is a relevant therapeutic strategy (23). In one study, paternal depression was associated with IC (24). The father can influence the development of IC indirectly by interacting with the mother during pregnancy; as well as directly after childbirth by lowering the father-infant interaction and not paying attention to its needs (25).
Another study also found that maternal self-efficacy in breastfeeding is associated with the incidence of IC. This is because of high maternal anxiety and incorrect breastfeeding technique (swallowing large amounts of air by the infant during breastfeeding and not taking the infant’s burp) (26, 27).
In this category, most studies have concentrated on the effect of migraine and smoking (28, 29, 30, 31). An infant who is born to a mother with migraine is hereditarily more prone to IC. The brains of such infants are more sensitive to environmental stimuli and manifest this sensitivity in the form of excessive crying (32). IC is recognized to be associated with the development of migraine in older ages (6).
Moreover, maternal smoking presents various effects on the infant. Tobacco metabolites transmit through the placenta during pregnancy and post-birth by exclusive breastfeeding or secondhand smoke from the environment. As a result, motilin hormone levels are increased in the infant’s GIT; subsequently, it increases its motility and leads to abdominal pain (33, 34). Maternal anxiety affects fetal blood circulation during pregnancy and can lead to decreased infant neuronal development and disturb the mother-infant interaction (35). In this category, other factors, such as young maternal age (17, 18, 29), the experience of the first child (35), and failure to breastfeed (26) were classified. These make the mother incapable of fully managing the infant. For example, if the correct technique of breastfeeding is observed, it can protect the infant against colic (20, 36). In this regard, Kheirkhah et al. suggested that formula feeding increased the risk of IC, compared to exclusive breastfeeding (37).
High Body Mass Index (BMI) (over 25 kg/m2) in pre-pregnancy (28) and vitamin B12 deficiency (13) are also risk factors for IC. Mothers with high BMI are less inclined to interact with their infants (38). They also have less control over their diet status during the breastfeeding period. These conditions can accelerate the IC incidence. Moreover, maternal vitamin deficiency is correlated with IC. Vitamin B12 causes the myelination of neurons; infants born to mothers with vitamin B12 deficiency may encounter a delay in neural system development (38). Delayed neural development is among the IC development causes.
The type of delivery, pregnancy, labor complications and the history of parity were classified in this category (17, 18, 39). Previous studies provided conflicting results concerning the type of delivery; therefore, further research is required in this respect (39, 40). In a study by Heydarian et al., infants with colic were mostly born through Normal Vaginal Delivery (NVD); however, it has been cited as a supportive factor via providing the normal intestinal flora while the infant passes through the birth canal (18, 41).
Moreover, high-risk pregnancies (eclampsia & pre-eclampsia) and delivery (vacuum or preterm delivery) have complications for the mother and infant after delivery. As a result, the mother-infant emotional relationship is affected and the risk of IC incidence is increased. Besides, increased mother parity reduces the risk of IC due to further experiences of coping with anxiety, stress management, and breastfeeding success (17, 42).
The paternal support of the mother is undoubtedly a significant factor that can reduce family anxiety and promote interaction with the infant (17). High social support of the mother is also considered as a supportive factor against IC due to benefiting from the experiences of other mothers (12). Additionally, maternal occupational and educational status fell into this category. Pregnant women who hold academic degrees, are studying in a school, or are involved in intensive and stressful jobs have a higher chance of bearing an infant with colic due to higher anxiety (17, 29).
In one study, parental high socioeconomic status was a contributing factor to IC (35). They indicated more sensitivity toward their infants and more frequently visited physicians’ offices. Furthermore, these parents spend extensive time outside the home, which affects their interaction with each other as well as with the infant.
This category is related to “maternal diet” during breastfeeding, i.e. investigated in two studies (11, 43). In one study, cow milk was found to be effective in the incidence of IC. The protein in cow milk can cause allergy and inflammation in the GIT (44). In some studies, a hypoallergenic diet and the elimination of cow milk were proposed as appropriate options for mothers whose infants experience the signs of atopy (45).
Another study reported that protein intake presented a protective role on IC (46); therefore, further research in this field is warranted. The consumption of vegetables and fruits, such as celery, onions, and bananas (they contain derivatives that can be secreted into breast milk) causes abdominal cramps and increases the risk of IC. Bananas contain indigestible starch; most of which is not hydrolyzed in the GIT. Therefore, it causes bloating in the colon through gas production and eventually leads to abdominal pain (34, 47). In addition, chocolate consumption in one study was also associated with IC, which may be due to the presence of caffeine in its composition (30). The relationship between maternal diet and IC provided contradictory results in different studies; accordingly, further research is needed in this field. Overall, it was recommended to not manipulate the mother’s diet to reduce IC (48).
In the last category, the results of studies mostly referred to the maternal use of antibiotics during pregnancy and postpartum (20, 49). Taking antibiotics, changes the normal flora of the infant’s GIT, i.e. nourished by breast milk. Thus, the disorder in normal microbial flora can cause IC (50). Moreover, maternal iron supplement uptake during pregnancy was associated with IC in one study; however, that was not reported in other studies and requires further investigations (28).
This study had some limitations, including the lack of accurate definition of IC and medium quality in some studies. Furthermore, observational studies were assessed in this research and other types were disregarded.
5. Conclusion
The present review results suggested that several parental factors were related to IC incidence. The most important factors predisposing to IC were parental depression, anxiety, smoking, maternal migraine, young age, primiparity, and low family support. A majority of studies focused on the effect of maternal factors on IC incidence, and paternal role has been less described. These characteristics were classified into 6 categories; these factors should be considered in future studies to implement appropriate prevention programs. However, several factors present conflicting effects on IC and require properly designed studies in the future.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committee of Esfarayen, Faculty of Medical Sciences (Code: IR.ESFARAYENUMS.REC.1398.012). All ethical principles were considered in this article.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, supervision, and methodology: Mahbobeh Firooz, Seyed Javad Hosseini; Investigation, writing -review & editing, writing - original draft: All authors.
Conflicts of interest
The authors declared no conflicts of interest.
References
- Raak C, Krueger P, Klement P, De Jaegere S, Weber S, Keller T, et al. Effectiveness of a homeopathic complex medicine in infantile colic: A randomized multicenter study. Complementary Therapies in Medicine. 2019; 45:136-41. [DOI:10.1016/j.ctim.2019.05.026] [PMID]
- Mansouri S, Kazemi I, Baghestani AR, Zayeri F, Nahidi F, Gazerani N. A placebo-controlled clinical trial to evaluate the effectiveness of massaging on infantile colic using a random-effects joint model. Pediatric Health, Medicine and Therapeutics. 2018; 9:157-63. [DOI:10.2147/PHMT.S185214] [PMID] [PMCID]
- Indrio F, Dargenio VN, Giordano P, Francavilla R. Preventing and treating colic. Advances in experimental medicine and biology. 2019; 1125:49-56. [DOI:10.1007/5584_2018_315] [PMID]
- Mohammadi G, Ghazanfarpour M, Kargarfard L, Babakhanian M. Effectiveness of herbal medicines containing phytoestrogens to treat infantile colic: A meta-analysis review. Journal of Pediatrics Review. 2019; 7(1):1-10. [DOI:10.32598/jpr.7.1.1]
- Cohen-Bendahan CC, van Doornen LJ, de Weerth C. Young adults’ reactions to infant crying. Infant behavior and development. 2014; 37(1):33-43. [DOI:10.1016/j.infbeh.2013.12.004] [PMID]
- Zhang D, Zhang Y, Sang Y, Zheng N, Liu X. The relationship between infant colic and migraine as well as tension-type headache: A meta-analysis. Pain research & management. 2019; 2019:8307982. [DOI:10.1155/2019/8307982] [PMID] [PMCID]
- Smarius LJ, Strieder TG, Loomans EM, Doreleijers TA, Vrijkotte TG, Gemke RJ, et al. Excessive infant crying doubles the risk of mood and behavioral problems at age 5: Evidence for mediation by maternal characteristics. European Child & Adolescent Psychiatry. 2017; 26(3):293-302. [DOI:10.1007/s00787-016-0888-4] [PMCID]
- Zeifman DM, St James-Roberts I. Parenting the crying infant. Current Opinion in Psychology. 2017; 15:149-54. [DOI:10.1016/j.copsyc.2017.02.009] [PMID] [PMCID]
- Zeevenhooven J, Browne PD, L’Hoir MP, de Weerth C, Benninga MA. Infant colic: Mechanisms and management. Nature Reviews. Gastroenterology & Hepatology. 2018; 15(8):479-96. [DOI:10.1038/s41575-018-0008-7] [PMID]
- Rhoads JM, Collins J, Fatheree NY, Hashmi SS, Taylor CM, Luo M, et al. Infant colic represents gut inflammation and dysbiosis. Journal of Pediatrics. 2018; 203:55-61 e3. [DOI:10.1016/j.jpeds.2018.07.042] [PMID] [PMCID]
- Aksoy Okan M, Gunduz M, Okur M, Akgun C, Esin K. Does maternal diet affect infantile colic? The Journal of Maternal-Fetal & Neonatal Medicine. 2016; 29(19):3139-41. [DOI:10.3109/14767058.2015.1115011] [PMID]
- Alexander CP, Zhu J, Paul IM, Kjerulff KH. Fathers make a difference: Positive relationships with mother and baby in relation to infant colic. Child: Care, Health and Development. 2017; 43(5):687-96. [DOI:10.1111/cch.12445] [PMID]
- Goedhart G, van der Wal MF, van Eijsden M, Bonsel GJ. Maternal vitamin B-12 and folate status during pregnancy and excessive infant crying. Early Human Development. 2011; 87(4):309-14. [DOI:10.1016/j.earlhumdev.2011.01.037] [PMID]
- Johnson JD, Cocker K, Chang E. Infantile colic: Recognition and treatment. American Family Physician. 2015; 92(7):577-82. [PMID]
- FitzGibbon K, Ju NR. Can the probiotic lactobacillus reuteri be used to treat infant colic? Annals of Emergency Medicine. 2019; 73(3):272-3. [DOI:10.1016/j.annemergmed.2018.09.016] [PMID]
- Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): Explanation and elaboration. International Journal of Surgery. 2014; 12(12):1500-24. [DOI:10.1016/j.ijsu.2014.07.014] [PMID]
- Canivet CA, Ostergren PO, Rosen AS, Jakobsson IL, Hagander BM. Infantile colic and the role of trait anxiety during pregnancy in relation to psychosocial and socioeconomic factors. The Scandinavian Journal of Public Health. 2005; 33(1):26-34. [DOI:10.1080/14034940410028316] [PMID]
- Heydarian F, Kharazmi A, Khatami F, Omidian M. Maternal and other risk factors including bovine IgG in developing infantile colic. Iranian Journal of Pediatrics. 2007; 17(1):19-22. https://www.researchgate.net/publication/43559807_Maternal_and_Other_Risk_Factors_Including_Bovine_IgG_in_Developing_Infantile_Colic
- Abacı FB, Gökçe S, Tuygun N, Karacan CD, Öner Ö. Psychosocial status and quality of life in mothers of infants with colic. The Turkish Journal of Pediatrics. 2013; 55(4):391-5. [PMID]
- Güngör Ş, Kırık S, Yaşar Özkars M, Korulmaz A. Effect of maternal depression and environmental factors on infantile colic. Erciyes Medical Journal. 2019; 41(1):80-4. [DOI:10.14744/etd.2018.18185]
- Maxted AE, Dickstein S, Miller-Loncar C, High P, Spritz B, Liu J, et al. Infant colic and maternal depression. Infant Mental Health Journal. 2005; 26(1):56-68. [DOI:10.1002/imhj.20035] [PMID]
- Foster JA, McVey Neufeld KA. Gut-brain axis: How the microbiome influences anxiety and depression. Trends in Neurosciences. 2013; 36(5):305-12. [DOI:10.1016/j.tins.2013.01.005] [PMID]
- Sung V, D’Amico F, Cabana MD, Chau K, Koren G, Savino F, et al. Lactobacillus reuteri to Treat Infant Colic: A meta-analysis. Pediatrics. 2018; 141(1):e20171811. [DOI:10.1542/peds.2017-1811] [PMID]
- van den Berg MP, van der Ende J, Crijnen AA, Jaddoe VW, Moll HA, Mackenbach JP, et al. Paternal depressive symptoms during pregnancy are related to excessive infant crying. Pediatrics. 2009; 124(1):e96-103. [DOI:10.1542/peds.2008-3100] [PMID]
- Raiha H, Lehtonen L, Huhtala V, Saleva K, Korvenranta H. Excessively crying infant in the family: Mother-infant, father-infant and mother-father interaction. Child: Care, Health and Development. 2002; 28(5):419-29. [DOI:10.1046/j.1365-2214.2002.00292.x] [PMID]
- Aktas S, Kucuk Alemdar D. Correlation between infantile colic and maternal breastfeeding self-efficacy, breastfeeding success and breast milk amount. Journal of Tropical Pediatrics. 2019; 65(4):321-7. [DOI:10.1093/tropej/fmy054] [PMID]
- Yalcin SS, Kuskonmaz BB. Relationship of lower breastfeeding score and problems in infancy. Breastfeeding medicine. 2011; 6(4):205-8. [DOI:10.1089/bfm.2010.0092] [PMID]
- Kaymaz N, Yildirim S, Topaloglu N, Gencer M, Binnetoglu FK, Tekin M, et al. Prenatal maternal risk factors for infantile colic. Nursing Children and Young People. 2015; 27(10):32-8. [DOI:10.7748/ncyp.27.10.32.s28] [PMID]
- Søndergaard C, Olsen J, Friis-Haschè E, Dirdal M, Thrane N, Toft Sørensen H. Psychosocial distress during pregnancy and the risk of infantile colic: A follow-up study. Acta Paediatrica, International Journal of Paediatrics. 2003; 92(7):811-6. [DOI:10.1111/j.1651-2227.2003.tb02538.x]
- Søndergaard C, Henriksen TB, Obel C, Wisborg K. Smoking during pregnancy and infantile colic. Pediatrics. 2001; 108(2):342-6. [DOI:10.1542/peds.108.2.342] [PMID]
- Gelfand AA, Buse DC, Cabana MD, Grimes B, Goadsby PJ, Allen IE. The association between parental migraine and infant colic: A cross-sectional, web-based, U.S. survey study. Headache. 2019; 59(7):988-1001. [DOI:10.1111/head.13575] [PMID]
- Gelfand AA. Infant colic: A baby’s migraine? Cephalalgia. 2015; 35(14):1243-5. [DOI:10.1177/0333102415576224] [PMID]
- Shenassa ED, Brown MJ. Maternal smoking and infantile gastrointestinal dysregulation: The case of colic. Pediatrics. 2004; 114(4):e497-505. [DOI:10.1542/peds.2004-1036] [PMID]
- Lothe L, Ivarsson SA, Ekman R, Lindberg T. Motilin and infantile Colic. Acta Paediatrica. 1990; 79(4):410-6. [DOI:10.1111/j.1651-2227.1990.tb11485.x]
- Canivet CA, Ostergren PO, Jakobsson IL, Dejin-Karlsson E, Hagander BM. Infantile colic, maternal smoking and infant feeding at 5 weeks of age. Scandinavian Journal of Public Health. 2008; 36(3):284-91. [DOI:10.1177/1403494807086981] [PMID]
- Kheirkhah D SM, Rezaei MH, Ardakani AT. Relationship between type of nutrition and infantile colic. International Journal of Medical Research & Health Sciences. 2016; 5(12):261-4. https://www.ijmrhs.com/abstract/relationship-between-type-of-nutrition-and-infantile-colic-6833.html.
- Rising R, Lifshitz F. Relationship between maternal obesity and infant feeding-interactions. Nutrition Journal. 2005; 4:17. [DOI:10.1186/1475-2891-4-17] [PMID] [PMCID]
- Zwart P, Vellema-Goud MG, Brand PL. Characteristics of infants admitted to hospital for persistent colic, and comparison with healthy infants. Acta Paediatrica. 2007; 96(3):401-5. [DOI:10.1111/j.1651-2227.2007.00090.x] [PMID]
- Fazil M. Prevalence and risk factors for infantile colic in District Mansehra. Journal of Ayub Medical College. 2011; 23(2):115-7. [PMID]
- Camilleri M, Park SY, Scarpato E, Staiano A. Exploring hypotheses and rationale for causes of infantile colic. Neurogastroenterology and Motility. 2017; 29(2):10.1111/nmo.12943. [DOI:10.1111/nmo.12943] [PMID] [PMCID]
- Clifford TJ, Campbell MK, Speechley KN, Gorodzinsky F. Infant colic: Empirical evidence of the absence of an association with source of early infant nutrition. Archives of Pediatrics & Adolescent Medicine. 2002; 156(11):1123-8. [DOI:10.1001/archpedi.156.11.1123] [PMID]
- Lust KD, Brown J, Thomas W. Maternal intake of cruciferous vegetables and other foods and colic symptoms in exclusively breast-fed infants. Journal of the American Dietetic Association. 1996; 96(1):46-8. [DOI:10.1016/S0002-8223(96)00013-2]
- Hill DJ, Hosking CS. Infantile colic and food hypersensitivity. Journal of Pediatric Gastroenterology and Nutrition. 2000; 30(suppl):S67-76. [DOI:10.1097/00005176-200001001-00011] [PMID]
- Nocerino R, Pezzella V, Cosenza L, Amoroso A, Di Scala C, Amato F, et al. The controversial role of food allergy in infantile colic: Evidence and clinical management. Nutrients. 2015; 7(3):2015-25. [DOI:10.3390/nu7032015] [PMID] [PMCID]
- Mhaske S, Mhaske S, Badrinarayan S, Zade R, Shirsath U. Role of protein rich maternal diet in infantile colic. Journal of the Indian Medical Association. 2012; 110(5):317-8. [PMID]
- Zhang P, Hamaker BR. Banana starch structure and digestibility. Carbohydrate Polymers. 2012; 87(2):1552-8. [DOI:10.1016/j.carbpol.2011.09.053]
- Gordon M, Biagioli E, Sorrenti M, Lingua C, Moja L, Banks SS, et al. Dietary modifications for infantile colic. The Cochrane Database of Systematic Reviews. 2018; 10:CD011029. [DOI:10.1002/14651858.CD011029.pub2] [PMID] [PMCID]
- Leppälehto E, Pärtty A, Kalliomäki M, Löyttyniemi E, Isolauri E, Rautava S. Maternal intrapartum antibiotic administration and infantile colic: Is there a connection? Neonatology. 2018:226-9. [DOI:10.1159/000489991] [PMID]
- Fatheree NY, Liu Y, Taylor CM, Hoang TK, Cai C, Rahbar MH, et al. Lactobacillus reuteri for infants with colic: A double-blind, placebo-controlled, randomized clinical trial. Journal of Pediatrics. 2017; 191:170-8.e2. [DOI:10.1016/j.jpeds.2017.07.036] [PMID] [PMCID]
- Talachian E, Bidari A, Rezaie MH. Incidence and risk factors for infantile colic in Iranian infants. World Journal of Gastroenterology. 2008; 14(29):4662-6. [DOI:10.3748/wjg.14.4662] [PMID] [PMCID]
- Søndergaard C, Olsen J, Dirdal M, Friis-Hasché E, Toft Sørensen H. [Infantile colic: An assessment of possible risk factors (Danish)]. Ugeskrift for Laeger. 2001; 163(45):6265-70. [PMID]
Type of Study: Systematic Review |
Subject:
Pediatrics
Received: 2020/08/28 | Accepted: 2020/10/28 | Published: 2021/04/1
Received: 2020/08/28 | Accepted: 2020/10/28 | Published: 2021/04/1
References
1. Raak C, Krueger P, Klement P, De Jaegere S, Weber S, Keller T, et al. Effectiveness of a homeopathic complex medicine in infantile colic: A randomized multicenter study. Complementary therapies in medicine. 2019;45:136-41. [DOI:10.1016/j.ctim.2019.05.026] [PMID]
2. Mansouri S, Kazemi I, Baghestani AR, Zayeri F, Nahidi F, Gazerani N. A placebo-controlled clinical trial to evaluate the effectiveness of massaging on infantile colic using a random-effects joint model. Pediatric health, medicine and therapeutics. 2018;9:157-63. [DOI:10.2147/PHMT.S185214] [PMID] [PMCID]
3. Indrio F, Dargenio VN, Giordano P, Francavilla R. Preventing and Treating Colic. Advances in experimental medicine and biology. 2019;1125:49-56. [DOI:10.1007/5584_2018_315] [PMID]
4. Mohammadi G, Ghazanfarpour M, Kargarfard L, Babakhanian M. Effectiveness of Herbal Medicines Containing Phytoestrogens to Treat Infantile Colic: A Meta-analysis Review. JPR. 2019;7(1):1-10. [DOI:10.32598/jpr.7.1.1]
5. Cohen-Bendahan CC, van Doornen LJ, de Weerth C. Young adults' reactions to infant crying. Infant behavior & development. 2014;37(1):33-43. [DOI:10.1016/j.infbeh.2013.12.004] [PMID]
6. Zhang D, Zhang Y, Sang Y, Zheng N, Liu X. The Relationship between Infant Colic and Migraine as well as Tension-Type Headache: A Meta-Analysis. Pain research & management. 2019;2019:8307982. [DOI:10.1155/2019/8307982] [PMID] [PMCID]
7. Smarius LJCA, Strieder TGA, Loomans EM, Doreleijers TAH, Vrijkotte TGM, Gemke RJ, et al. Excessive infant crying doubles the risk of mood and behavioral problems at age 5: evidence for mediation by maternal characteristics. Eur Child Adolesc Psychiatry. 2017;26(3):293-302. [DOI:10.1007/s00787-016-0888-4] [PMID] [PMCID]
8. Zeifman DM, St James-Roberts I. Parenting the Crying Infant. Curr Opin Psychol. 2017;15:149-54. [DOI:10.1016/j.copsyc.2017.02.009] [PMID] [PMCID]
9. Zeevenhooven J, Browne PD, L'Hoir MP, de Weerth C, Benninga MA. Infant colic: mechanisms and management. Nature reviews Gastroenterology & hepatology. 2018;15(8):479-96. [DOI:10.1038/s41575-018-0008-7] [PMID]
10. Rhoads JM, Collins J, Fatheree NY, Hashmi SS, Taylor CM, Luo M, et al. Infant Colic Represents Gut Inflammation and Dysbiosis. The Journal of pediatrics. 2018;203:55-61.e3. [DOI:10.1016/j.jpeds.2018.07.042] [PMID] [PMCID]
11. Aksoy Okan M, Gunduz M, Okur M, Akgun C, Esin K. Does maternal diet affect infantile colic? The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstet. 2016;29(19):3139-41. [DOI:10.3109/14767058.2015.1115011] [PMID]
12. Alexander CP, Zhu J, Paul IM, Kjerulff KH. Fathers make a difference: positive relationships with mother and baby in relation to infant colic. Child: care, health and development. 2017;43(5):687-96. [DOI:10.1111/cch.12445] [PMID]
13. Goedhart G, van der Wal MF, van Eijsden M, Bonsel GJ. Maternal vitamin B-12 and folate status during pregnancy and excessive infant crying. Early human development. 2011;87(4):309-14. [DOI:10.1016/j.earlhumdev.2011.01.037] [PMID]
14. Johnson JD, Cocker K, Chang E. Infantile Colic: Recognition and Treatment. American family physician. 2015;92(7):577-82.
15. FitzGibbon K, Ju NR. Can the Probiotic Lactobacillus reuteri Be Used to Treat Infant Colic? Annals of emergency medicine. 2019;73(3):272-3. [DOI:10.1016/j.annemergmed.2018.09.016] [PMID]
16. Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12(12):1500-24. [DOI:10.1016/j.ijsu.2014.07.014] [PMID]
17. Canivet CA, Ostergren PO, Rosen AS, Jakobsson IL, Hagander BM. Infantile colic and the role of trait anxiety during pregnancy in relation to psychosocial and socioeconomic factors. Scand J Public Health. 2005;33(1):26-34. [DOI:10.1080/14034940410028316] [PMID]
18. Heydarian F, Kharazmi A, Khatami F, Omidian M. Maternal and other risk factors including bovine IgG in developing infantile colic. Iranian Journal of Pediatrics. 2007;17(1):19-22.
19. Abaci FB, Gokce S, Tuygun N, Karacan CD, Oner O. Psychosocial status and quality of life in mothers of infants with colic. Turk J Pediatr. 2013;55(4):391-5.
20. Gungor S, Kirik S, Ozkars MY, Korulmaz A. Effect of Maternal Depression and Environmental Factors on Infantile Colic. Erciyes Medical Journal. 2019;41(1):80-4. [DOI:10.14744/etd.2018.18185]
21. Maxted AE, Dickstein S, Miller-Loncar C, High P, Spritz B, Liu J, et al. Infant colic and maternal depression. Infant Ment Health J. 2005;26(1):56-68. [DOI:10.1002/imhj.20035] [PMID]
22. Foster JA, McVey Neufeld KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 2013;36(5):305-12. [DOI:10.1016/j.tins.2013.01.005] [PMID]
23. Sung V, D'Amico F, Cabana MD, Chau K, Koren G, Savino F, et al. Lactobacillus reuteri to Treat Infant Colic: A Meta-analysis. Pediatrics. 2018;141(1):e20171811. [DOI:10.1542/peds.2017-1811] [PMID]
24. Van Den Berg MP, Van Der Ende J, Crijnen AAM, Jaddoe VWV, Moll HA, Mackenbach JP, et al. Paternal depressive symptoms during pregnancy are related to excessive infant crying. Pediatrics. 2009;124(1):e96-e103. [DOI:10.1542/peds.2008-3100] [PMID]
25. Raiha H, Lehtonen L, Huhtala V, Saleva K, Korvenranta H. Excessively crying infant in the family: mother-infant, father-infant and mother-father interaction. Child: care, health and development. 2002;28(5):419-29. [DOI:10.1046/j.1365-2214.2002.00292.x] [PMID]
26. Aktas S, Kucuk Alemdar D. Correlation between Infantile Colic and Maternal Breastfeeding Self-Efficacy, Breastfeeding Success and Breast Milk Amount. J Trop Pediatr. 2019;65(4):321-7. [DOI:10.1093/tropej/fmy054] [PMID]
27. Yalçin SS, Kuşkonmaz BB. Relationship of lower breastfeeding score and problems in infancy. Breastfeeding Medicine. 2011;6(4):205-8. [DOI:10.1089/bfm.2010.0092] [PMID]
28. Kaymaz N, Yıldırım Ş, Topaloğlu N, Gencer M, Binnetoğlu FK, Tekin M, et al. Prenatal maternal risk factors for infantile colic. Nursing children and young people. 2015;27(10):32-8. [DOI:10.7748/ncyp.27.10.32.s28] [PMID]
29. Søndergaard C, Olsen J, Friis-Haschè E, Dirdal M, Thrane N, Toft Sørensen H. Psychosocial distress during pregnancy and the risk of infantile colic: A follow-up study. Acta Paediatrica, International Journal of Paediatrics. 2003;92(7):811-6. [DOI:10.1111/j.1651-2227.2003.tb02538.x]
30. Søndergaard C, Henriksen TB, Obel C, Wisborg K. Smoking during pregnancy and infantile colic. Pediatrics. 2001;108(2 II):342-6. [DOI:10.1542/peds.108.2.342] [PMID]
31. Gelfand AA, Buse DC, Cabana MD, Grimes B, Goadsby PJ, Allen IE. The Association Between Parental Migraine and Infant Colic: A Cross-Sectional, Web-Based, U.S. Survey Study. Headache. 2019;59(7):988-1001. [DOI:10.1111/head.13575] [PMID]
32. Gelfand AA. Infant colic--a baby's migraine? Cephalalgia. 2015;35(14):1243-5. [DOI:10.1177/0333102415576224] [PMID]
33. Shenassa ED, Brown MJ. Maternal smoking and infantile gastrointestinal dysregulation: the case of colic. Pediatrics. 2004;114(4):e497-505. [DOI:10.1542/peds.2004-1036] [PMID]
34. Hosseini SJ, Firooz M, Khantaraj S, Firouzian AA, B M. Caring for Infant with colic. Mashhad: parastaran Javan; 2019. 23-4 p.
35. Canivet C, Ostergren PO, Jakobsson I, Hagander B. Higher risk of colic in infants of nonmanual employee mothers with a demanding work situation in pregnancy. Int J Behav Med. 2004;11(1):37-47. [DOI:10.1207/s15327558ijbm1101_5] [PMID]
36. Canivet CA, Östergren P-O, Jakobsson IL, Dejin-Karlsson E, Hagander BM. Infantile colic, maternal smoking and infant feeding at 5 weeks of age. Scandinavian Journal of Public Health. 2008;36(3):284-91. [DOI:10.1177/1403494807086981] [PMID]
37. Kheirkhah D, Sharif MR, Rezaei MH, Ardakani AT. Relationship between type of nutrition and infantile colic. International Journal of Medical Research & Health Sciences. 2016;5(12):261-4.
38. Rising R, Lifshitz F. Relationship between maternal obesity and infant feeding-interactions. Nutr J. 2005;4:17-. [DOI:10.1186/1475-2891-4-17] [PMID] [PMCID]
39. Zwart P, Vellema-Goud MGA, Brand PLP. Characteristics of infants admitted to hospital for persistent colic, and comparison with healthy infants. Acta Paediatrica, International Journal of Paediatrics. 2007;96(3):401-5. [DOI:10.1111/j.1651-2227.2007.00090.x] [PMID]
40. Fazil M. Prevalence and risk factors for infantile colic in District Mansehra. J Ayub Med Coll Abbottabad. 2011;23(2):115-7.
41. Camilleri M, Park SY, Scarpato E, Staiano A. Exploring hypotheses and rationale for causes of infantile colic. Neurogastroenterol Motil. 2017;29(2):10.1111/nmo.12943. [DOI:10.1111/nmo.12943] [PMID] [PMCID]
42. Clifford TJ, Campbell MK, Speechley KN, Gorodzinsky F. Infant Colic: Empirical Evidence of the Absence of an Association With Source of Early Infant Nutrition. Archives of Pediatrics & Adolescent Medicine. 2002;156(11):1123-8. [DOI:10.1001/archpedi.156.11.1123] [PMID]
43. Lust KD, Brown JE, Thomas W. Maternal intake of cruciferous vegetables and other foods and colic symptoms in exclusively breast-fed infants. J Am Diet Assoc. 1996;96(1):46-8. [DOI:10.1016/S0002-8223(96)00013-2]
44. Hill DJ, Hosking CS. Infantile colic and food hypersensitivity. J Pediatr Gastroenterol Nutr. 2000;30 Suppl:S67-76. [DOI:10.1097/00005176-200001001-00011] [PMID]
45. Nocerino R, Pezzella V, Cosenza L, Amoroso A, Di Scala C, Amato F, et al. The controversial role of food allergy in infantile colic: evidence and clinical management. Nutrients. 2015;7(3):2015-25. [DOI:10.3390/nu7032015] [PMID] [PMCID]
46. Mhaske S, Mhaske S, Badrinarayan S, Zade R, Shirsath U. Role of protein rich maternal diet in infantile colic. J Indian Med Assoc. 2012;110(5):317-8.
47. Zhang P, Hamaker BR. Banana starch structure and digestibility. Carbohydrate Polymers. 2012;87(2):1552-8. [DOI:10.1016/j.carbpol.2011.09.053]
48. Gordon M, Biagioli E, Sorrenti M, Lingua C, Moja L, Banks SS, et al. Dietary modifications for infantile colic. Cochrane Database Syst Rev. 2018;10(10):CD011029-CD. [DOI:10.1002/14651858.CD011029.pub2] [PMID] [PMCID]
49. Leppälehto E, Pärtty A, Kalliomäki M, Löyttyniemi E, Isolauri E, Rautava S. Maternal Intrapartum Antibiotic Administration and Infantile Colic: Is there a Connection? Neonatology. 2018:226-9. [DOI:10.1159/000489991] [PMID]
50. Sung V, D'Amico F, Cabana MD, Chau K, Koren G, Savino F, et al. Lactobacillus reuteri to Treat Infant Colic: A Meta-analysis. Pediatrics. 2018;141(1). [DOI:10.1542/peds.2017-1811] [PMID]
51. Kaymaz N, Yıldırım Ş, Topaloğlu N, Gencer M, Binnetoğlu FK, Tekin M, et al. Prenatal maternal risk factors for infantile colic. Nurs Child Young People. 2015;27(10):32-8. [DOI:10.7748/ncyp.27.10.32.s28] [PMID]
52. Talachian E, Bidari A, Rezaie MH. Incidence and risk factors for infantile colic in Iranian infants. World Journal of Gastroenterology. 2008;14(29):4662-6. [DOI:10.3748/wjg.14.4662] [PMID] [PMCID]
53. Søndergaard C, Olsen J, Dirdal M, Friis-Hasché E, Toft Sørensen H. Infantile colic: An assessment of possible risk factors. Ugeskrift for Laeger. 2001;163(45):6265-70.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








