Volume 10, Issue 2 (4-2022)
J. Pediatr. Rev 2022, 10(2): 167-174 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Roudi F, Sezavar M, Naseri M, Azadeh F, Khademi G. Nutrition Support among Critically Ill Pediatric Patients: The Current Practice. J. Pediatr. Rev 2022; 10 (2) :167-174
URL: http://jpr.mazums.ac.ir/article-1-427-en.html
URL: http://jpr.mazums.ac.ir/article-1-427-en.html
1- Department of Nutrition, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
2- Clinical Research Development Unit of Akbar Hospital, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
3- Department of Pediatrics, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
4- Health Deputy, Mashhad University of Medical Sciences, Mashhad, Iran.
5- Clinical Research Development Unit of Akbar Hospital, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran. , Khademigh@mums.ac.ir
2- Clinical Research Development Unit of Akbar Hospital, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
3- Department of Pediatrics, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
4- Health Deputy, Mashhad University of Medical Sciences, Mashhad, Iran.
5- Clinical Research Development Unit of Akbar Hospital, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran. , Khademigh@mums.ac.ir
Keywords: Critical careoutcomes, Critical illness, Intensive care unit, Pediatric, Nutrition Therapy, Nutrients
Full-Text [PDF 372 kb]
(988 Downloads)
| Abstract (HTML) (2121 Views)
Full-Text: (397 Views)
1. Introduction
Malnutrition is a major problem among critically ill patients due to decreased appetite, decreased energy and protein intake, increased energy requirements, and inflammation [1-5]. Critical illnesses can consequently cause malnutrition, which is associated with worsening clinical outcomes in patients admitted to the Pediatric Intensive Care Unit (PICU) [1, 3-7].
The effects of malnutrition on the spread of some complications, such as the prolonged hospital and PICU stay and reduced response to medication during treatment, are well-known [1, 3, 5, 8]. Moreover, malnutrition reduces the adhesion of the intestinal mucosa, leading to an increase in the susceptibility to bacteria and rates of infection [9]. Additionally, the coexistence of malnutrition and stress caused by acute illness in patients admitted to the ICU was found to be associated with negative energy balance and lean mass reduction. Increased catabolism of Lean Body Mass (LBM) aggravates the clinical condition and increases the length of hospital stay, recovery time, and treatment costs [2, 9]. According to the previous studies, along with increasing body mass loss in hospitalized patients as a result of malnutrition, the mortality rate also increases significantly. With a 10, 20, 30, and 40% decrease in LBM, the mortality rate increases by 10, 30, 50, and 100%, respectively [4].
Therefore, optimum nutrition support in PICU patients is of particular importance, to prevent muscle wasting and improving the functions of the organs. For example, adequate energy and protein delivery is associated with maintained gastrointestinal (GI) membrane integrity and reduced bacterial displacement, which results in better GI system function [2, 4, 8, 9]. Additionally, the immune system function is affected by the status of nutrition support in the PICU. Therefore, nutritional adequacy may have some beneficial effects on clinical outcomes, including the duration of mechanical ventilation, hospital and PICU stay, infection, mortality, and costs [2, 4, 8, 9].
Given the special importance of childhood due to the children’s growth and development during this period, proper nutritional management of critically ill children, in order to shorten the acute phase response of the disease and recovery period, discharge with minimal complications and in the shortest possible time, and compensate the disease-related delayed growth following recovery, is necessary, difficult, and challenging [5, 10, 11].
The present study was conducted to investigate the nutritional adequacy and its probable relations to clinical outcomes of PICU admitted patients, in order to have a better judgment on the nutrition support services status. Accordingly, this issue may lead to making realistic evidence-based decisions to improve the medical management of critically ill pediatric patients.
2. Methods
This retrospective cross-sectional study was performed in Akbar Children's Hospital (a university-affiliated, tertiary-level hospital with a 19-bed PICU) in Mashhad, Iran. The data of the patients with PICU length of stay >48 hours during May-June 2019 (8 weeks), were extracted. The patients who died or were discharged in the first 48 hours following PICU admission as well as those with unavailable documents were not recruited. According to the study by Nagrath et al. (2018) and considering protein adequacy as the main outcome of the study, the minimum estimated sample size was 65 patients [12]. The recorded variables included age, gender, primary diagnosis, and delivered energy and protein at the discharge time from PICU (in case of length of PICU stayeight days). The weight-for-height z-score (World Health Organization (WHO) Global Database) was applied for the assessment of the patients’ nutritional status upon admission to PICU. Moreover, clinical outcomes, including infection, the duration of mechanical ventilation, length of PICU and hospital stay, and possible mortality were recorded. Finally, to determine the basal energy requirement, the Schofield equation was used, and the European Society for Parenteral and Enteral Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines were used, in order to calculate the energy and protein requirements of patients in terms of age, height, weight, gender, and severity of the disease [13, 14]. Notably, the achievement of more than two-thirds of the target goals, energy and protein delivery, at the end of the first week of PICU staying or sooner was considered as positive nutritional adequacy [15].
Paper records of patients who were illegible and non-assessable or those with incomplete information were excluded from the study. The required information was recorded in a proper checklist, which was prepared according to the variables of the study by the researchers to ensure that all needed data are extracted from each document.
The Ethics Committee of Mashhad University of Medical Sciences (MUMS) approved the study protocol and the study was performed in terms of the Declaration of Helsinki. The MUMS ethical committee waived the patient consent because of the retrospective non-identifiable document-based nature of the study and the non-identifiable extracted data for the study variables.
Statistical analysis was done by IBMSPSS 20.0. Descriptive statistics were applied to present the demographic characteristics of the critically ill pediatric patients who were studied in this research. Numbers and percentages were applied to present the qualitative data of the study. The distribution of the quantitative data was checked through the Kolmogorov-Smirnov test. The Pearson/Spearman coefficient was also applied to investigate the probable correlations between nutritional indices (i.e., nutritional status, energy and protein delivery, and adequacy) and clinical outcomes. A P-value < 0.05 was considered the statistical significance level for all the analyses.
3. Results
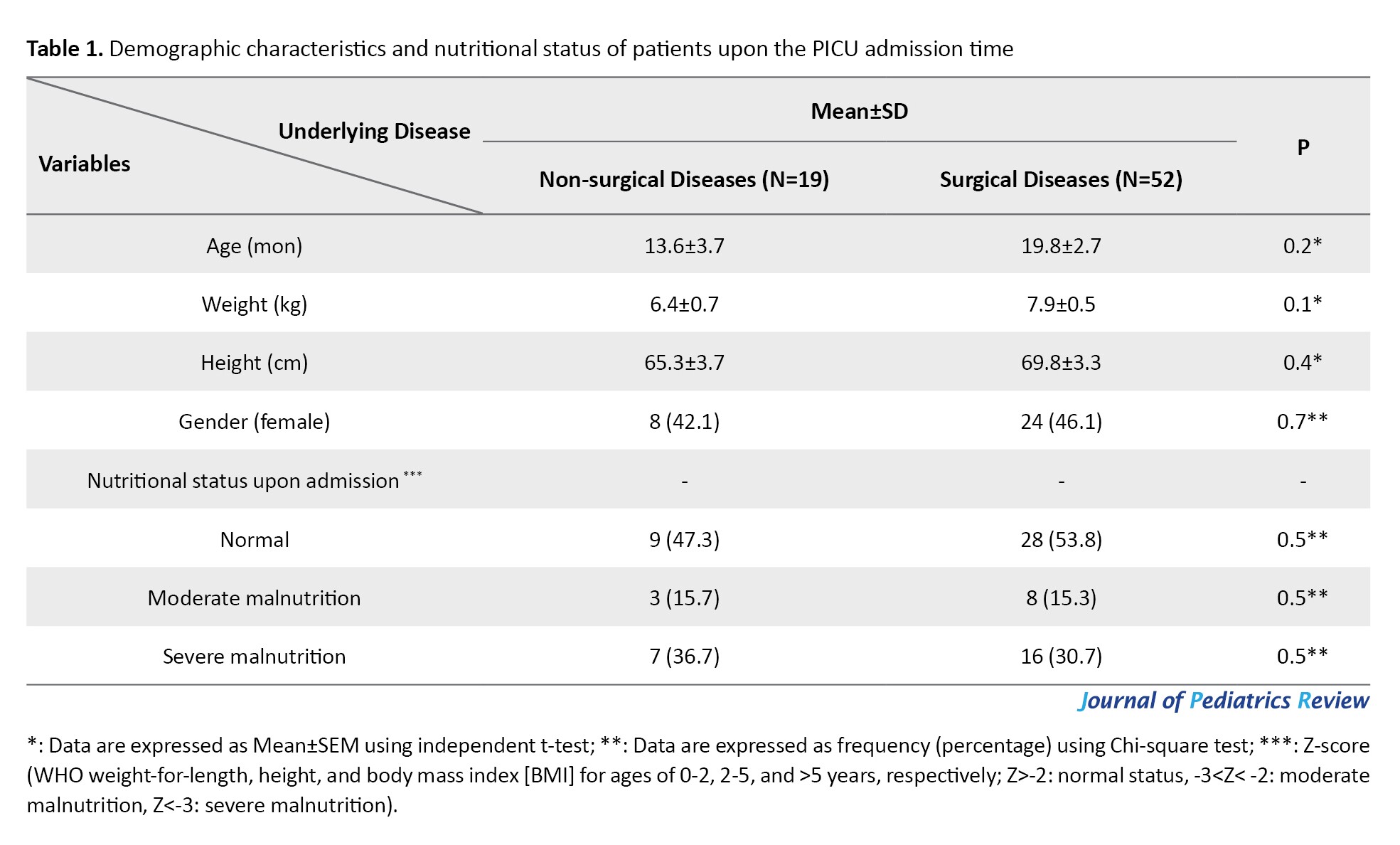
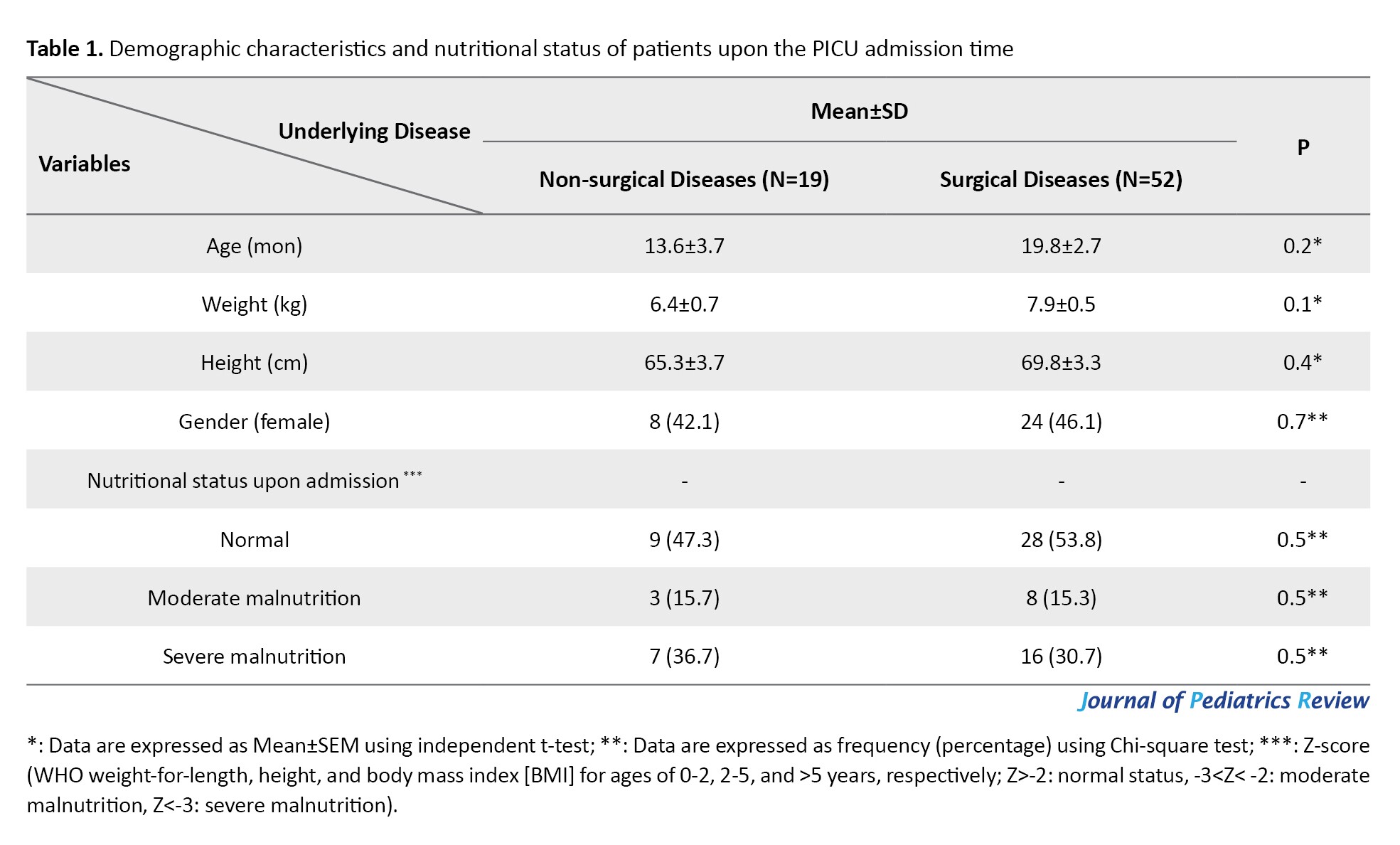
Totally, 71 critically ill pediatric patients with Mean±SD age of 18.1±2.2 months were enrolled in this study. The Mean±SD weight and height of the participants were 7.5±0.45 kg and 68.6±2.6 cm, respectively. There were 32 (45.5%) female and 39 (54.9%) male subjects in the studied patients.
Table 1 depicts the demographic characteristics of the patients. As shown in Table 1, there was no significant difference in terms of age, weight, height, gender, and nutrition status at the time of admission between the critically ill children with non-surgical underlying diseases and the children admitted to PICU due to their critical condition following surgeries.
According to the results of the present study, the mean±SEM values of the energy requirement and delivered energy were estimated as 85.7±1.6 and 68.3±2.1 kcal/kg/d, respectively. Additionally, the estimated protein requirement and delivered protein were 2.5±0.08 and 1.8±0.03 gr/kg/d, respectively. There was no significant difference in the aforementioned indices between the two studied groups (non-surgical and surgical underlying diseases (P>0.05).
As shown in Table 2, Enteral Nutrition (EN) was the most frequent route used for feeding critically ill children with surgical underlying diseases and the combination of EN and Parenteral Nutrition (PN) was the most frequent route of administration for the patients admitted to PICU due to non-surgical underlying diseases. However, the obtained data showed no significant difference between these two groups in terms of the feeding route. Energy and protein adequacy had similar frequencies, which were recorded in 15 (78.9%) and 45 (86.5%) patients in the two groups with non-surgical and surgical underlying diseases, respectively (Table 2).

The recorded clinical outcomes of the studied patients are shown in Table 3. As shown in Table 3, lengths of hospital and PICU stay, infection, and mortality rates were similar in these two groups. However, the duration of mechanical ventilation was significantly higher among critically ill children with non-surgical underlying diseases (P<0.001).

The results of the present study show that there were significant associations between nutritional status at the time of admission, infection, and mortality rates (P=0.001 and 0.004, respectively; Spearman’s correlation coefficient). However, the patients‘ nutritional status was not related to the duration of mechanical ventilation, PICU, and hospital stay (P>0.05; Spearman’s correlation coefficient).
There was a significant association between protein delivery and mechanical ventilation duration (P-value= 0.01). Also, a negative significant association was found between energy delivery and the infection rate (P=0.03).
Finally, in the present study, a subgroup analysis of the obtained data showed significant associations between energy delivery, length of PICU stay, and hospital stay in critically ill pediatric patients with non-surgical underlying diseases (P=0.02 and 0.03, respectively).
4. Discussion
This cross-sectional study was performed to investigate the current status of nutrition support services among critically ill pediatric patients. Correspondingly, this would be an important step for performing realistic monitoring, in order to improve nutrition support services in PICU. The results of the present study showed that almost half of the study participants had normal nutritional status upon the PICU admission time. Moreover, delivered energy and protein levels among the two studied groups were at acceptable ranges. The EN was the most frequent route used for feeding critically ill children with surgical underlying diseases and the combination of EN and PN was the most frequent administration route for the patients admitted to PICU due to non-surgical underlying diseases.
Optimal energy and macro and micronutrient delivery is considered a therapeutic strategy in the medical management of critically ill children [10, 16-19]. Stepwise nutritional assessment, intervention, and monitoring of such patients also are of particular importance used to minimize growth retardation, Fat-Free Mass (FFM) loss, and complications during PICU stay [20-22].
Nutritional status was considered as a predictor of the ventilation duration in the study by Grippa et al.; however, such a relationship was not seen in our study, which may be due to the normal nutritional status of most of the studied patients upon admission time [23]. On the other hand, the malnourished patients experienced higher infection and mortality rates, which are consistent with the systematic review performed by Costa et al. who reported that nutritionally depleted patients may experience worse clinical outcomes [24].
Additionally, the energy and protein delivery levels of the patients in the two groups were at an acceptable range. These findings may be inconsistent with those of some previously published articles. Accordingly, these disagreements may be due to different study populations as most of the studied patients were critically ill patients with abdominal/neurosurgical underlying diseases [16, 25-27]. Additionally, the presence of nutritionists in daily medical team visits in our study may be another effective factor affecting the nutrient delivery of the studied patients. Moreover, as nutrition delivery is considered an effective factor in clinical outcomes, this acceptable status would influence the recorded clinical outcomes in the present study as well [26, 28]. Consistently, energy intake had a negative association with infection rate. In addition, lower protein delivery was found to be negatively associated with prolonged mechanical ventilation.
The present study was the second retrospective study conducted on the nutritional adequacy of the critically ill children in our referral PICU. Accordingly, the nutrition support indices obviously improved following the regular daily presence of nutritionists in medical staff team visits [25]. Additionally, our study investigated the nutritional adequacy of gastrointestinal surgical critically ill neonates and showed a high prevalence of underfeeding in such patients [16]. The aforementioned issue highlights the importance of the necessity of coordinated teamwork for the better management of PICU patients.
However, recording no nutrient delivery barriers was the main limitation of the present study, because we cannot have an evidence-based judgment on the probable barriers to optimum nutrient delivery in our PICU to make more realistic decisions. For example, rare post-pyloric tube insertion obviously was a routine barrier for us, but we found no records in hospital documents regarding this issue. Moreover, as our ward was not considered as a referral PICU for nephrological and oncological patients as well as cardiac surgical subjects, we cannot generalize the obtained results to all pediatric critically ill patients. Therefore, performing further prospective, large-population-based, multi-center studies is necessary to have a proper realistic opinion on the current nutrition support status and the nutrient delivery barriers in PICU patients. This step would be an important pivotal step to make customized nutrition support instructions and guidelines for such patients.
5. Conclusion
According to the results of the present study, energy and nutrient delivery levels were at acceptable status in 78.9% of the critically ill children with non-surgical underlying diseases and in 86.5% of the surgical PICU patients. The EN was the most frequent route used for feeding critically ill children with surgical underlying diseases and the combination of EN and PN was more used for the patients admitted to PICU due to non-surgical underlying diseases. This finding revealed the improved quality of nutrition support services during the last year. Moreover, some significant associations between energy/protein delivery and some clinical outcomes, including mechanical ventilation duration, infection rate, length of PICU, and hospital stay indicated the necessity of further reasonable, realistic, and evidence-based nutritional interventions as well as monitoring optimal nutrition support barriers in critically ill pediatric patients.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Mashhad University of Medical Sciences (IR.MUMS.MEDICAL.REC.1399.166).
Funding
This research was supported by the research project (IR.MUMS.MEDICAL.REC.1399.166), funded by Mashhad University of Medical Sciences.
Authors' contributions
Conceptualization: Fatemeh Roudi and Gholamreza Khademi; Data Collection: Fahimeh Azadeh and Maryam Naseri; Methodology: Fatemeh Roudi and Majid Sezavar; Fatemeh Roudi: Writing–original draft and Statistical analysis; Fatemeh Roudi; Writing–Review & Editing and Supervision: Gholamreza Khademi and Majid Sezavar.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
We would thank all the staff of Akbar Children's Hospital for helping us, the Clinical Research Development Unit of Akbar Hospital, and the deputy of research of Mashhad University of Medical Sciences (MUMS) due to financially support of the project.
References
Malnutrition is a major problem among critically ill patients due to decreased appetite, decreased energy and protein intake, increased energy requirements, and inflammation [1-5]. Critical illnesses can consequently cause malnutrition, which is associated with worsening clinical outcomes in patients admitted to the Pediatric Intensive Care Unit (PICU) [1, 3-7].
The effects of malnutrition on the spread of some complications, such as the prolonged hospital and PICU stay and reduced response to medication during treatment, are well-known [1, 3, 5, 8]. Moreover, malnutrition reduces the adhesion of the intestinal mucosa, leading to an increase in the susceptibility to bacteria and rates of infection [9]. Additionally, the coexistence of malnutrition and stress caused by acute illness in patients admitted to the ICU was found to be associated with negative energy balance and lean mass reduction. Increased catabolism of Lean Body Mass (LBM) aggravates the clinical condition and increases the length of hospital stay, recovery time, and treatment costs [2, 9]. According to the previous studies, along with increasing body mass loss in hospitalized patients as a result of malnutrition, the mortality rate also increases significantly. With a 10, 20, 30, and 40% decrease in LBM, the mortality rate increases by 10, 30, 50, and 100%, respectively [4].
Therefore, optimum nutrition support in PICU patients is of particular importance, to prevent muscle wasting and improving the functions of the organs. For example, adequate energy and protein delivery is associated with maintained gastrointestinal (GI) membrane integrity and reduced bacterial displacement, which results in better GI system function [2, 4, 8, 9]. Additionally, the immune system function is affected by the status of nutrition support in the PICU. Therefore, nutritional adequacy may have some beneficial effects on clinical outcomes, including the duration of mechanical ventilation, hospital and PICU stay, infection, mortality, and costs [2, 4, 8, 9].
Given the special importance of childhood due to the children’s growth and development during this period, proper nutritional management of critically ill children, in order to shorten the acute phase response of the disease and recovery period, discharge with minimal complications and in the shortest possible time, and compensate the disease-related delayed growth following recovery, is necessary, difficult, and challenging [5, 10, 11].
The present study was conducted to investigate the nutritional adequacy and its probable relations to clinical outcomes of PICU admitted patients, in order to have a better judgment on the nutrition support services status. Accordingly, this issue may lead to making realistic evidence-based decisions to improve the medical management of critically ill pediatric patients.
2. Methods
This retrospective cross-sectional study was performed in Akbar Children's Hospital (a university-affiliated, tertiary-level hospital with a 19-bed PICU) in Mashhad, Iran. The data of the patients with PICU length of stay >48 hours during May-June 2019 (8 weeks), were extracted. The patients who died or were discharged in the first 48 hours following PICU admission as well as those with unavailable documents were not recruited. According to the study by Nagrath et al. (2018) and considering protein adequacy as the main outcome of the study, the minimum estimated sample size was 65 patients [12]. The recorded variables included age, gender, primary diagnosis, and delivered energy and protein at the discharge time from PICU (in case of length of PICU stay
Paper records of patients who were illegible and non-assessable or those with incomplete information were excluded from the study. The required information was recorded in a proper checklist, which was prepared according to the variables of the study by the researchers to ensure that all needed data are extracted from each document.
The Ethics Committee of Mashhad University of Medical Sciences (MUMS) approved the study protocol and the study was performed in terms of the Declaration of Helsinki. The MUMS ethical committee waived the patient consent because of the retrospective non-identifiable document-based nature of the study and the non-identifiable extracted data for the study variables.
Statistical analysis was done by IBMSPSS 20.0. Descriptive statistics were applied to present the demographic characteristics of the critically ill pediatric patients who were studied in this research. Numbers and percentages were applied to present the qualitative data of the study. The distribution of the quantitative data was checked through the Kolmogorov-Smirnov test. The Pearson/Spearman coefficient was also applied to investigate the probable correlations between nutritional indices (i.e., nutritional status, energy and protein delivery, and adequacy) and clinical outcomes. A P-value < 0.05 was considered the statistical significance level for all the analyses.
3. Results
Totally, 71 critically ill pediatric patients with Mean±SD age of 18.1±2.2 months were enrolled in this study. The Mean±SD weight and height of the participants were 7.5±0.45 kg and 68.6±2.6 cm, respectively. There were 32 (45.5%) female and 39 (54.9%) male subjects in the studied patients.
Table 1 depicts the demographic characteristics of the patients. As shown in Table 1, there was no significant difference in terms of age, weight, height, gender, and nutrition status at the time of admission between the critically ill children with non-surgical underlying diseases and the children admitted to PICU due to their critical condition following surgeries.
According to the results of the present study, the mean±SEM values of the energy requirement and delivered energy were estimated as 85.7±1.6 and 68.3±2.1 kcal/kg/d, respectively. Additionally, the estimated protein requirement and delivered protein were 2.5±0.08 and 1.8±0.03 gr/kg/d, respectively. There was no significant difference in the aforementioned indices between the two studied groups (non-surgical and surgical underlying diseases (P>0.05).
As shown in Table 2, Enteral Nutrition (EN) was the most frequent route used for feeding critically ill children with surgical underlying diseases and the combination of EN and Parenteral Nutrition (PN) was the most frequent route of administration for the patients admitted to PICU due to non-surgical underlying diseases. However, the obtained data showed no significant difference between these two groups in terms of the feeding route. Energy and protein adequacy had similar frequencies, which were recorded in 15 (78.9%) and 45 (86.5%) patients in the two groups with non-surgical and surgical underlying diseases, respectively (Table 2).

The recorded clinical outcomes of the studied patients are shown in Table 3. As shown in Table 3, lengths of hospital and PICU stay, infection, and mortality rates were similar in these two groups. However, the duration of mechanical ventilation was significantly higher among critically ill children with non-surgical underlying diseases (P<0.001).

The results of the present study show that there were significant associations between nutritional status at the time of admission, infection, and mortality rates (P=0.001 and 0.004, respectively; Spearman’s correlation coefficient). However, the patients‘ nutritional status was not related to the duration of mechanical ventilation, PICU, and hospital stay (P>0.05; Spearman’s correlation coefficient).
There was a significant association between protein delivery and mechanical ventilation duration (P-value= 0.01). Also, a negative significant association was found between energy delivery and the infection rate (P=0.03).
Finally, in the present study, a subgroup analysis of the obtained data showed significant associations between energy delivery, length of PICU stay, and hospital stay in critically ill pediatric patients with non-surgical underlying diseases (P=0.02 and 0.03, respectively).
4. Discussion
This cross-sectional study was performed to investigate the current status of nutrition support services among critically ill pediatric patients. Correspondingly, this would be an important step for performing realistic monitoring, in order to improve nutrition support services in PICU. The results of the present study showed that almost half of the study participants had normal nutritional status upon the PICU admission time. Moreover, delivered energy and protein levels among the two studied groups were at acceptable ranges. The EN was the most frequent route used for feeding critically ill children with surgical underlying diseases and the combination of EN and PN was the most frequent administration route for the patients admitted to PICU due to non-surgical underlying diseases.
Optimal energy and macro and micronutrient delivery is considered a therapeutic strategy in the medical management of critically ill children [10, 16-19]. Stepwise nutritional assessment, intervention, and monitoring of such patients also are of particular importance used to minimize growth retardation, Fat-Free Mass (FFM) loss, and complications during PICU stay [20-22].
Nutritional status was considered as a predictor of the ventilation duration in the study by Grippa et al.; however, such a relationship was not seen in our study, which may be due to the normal nutritional status of most of the studied patients upon admission time [23]. On the other hand, the malnourished patients experienced higher infection and mortality rates, which are consistent with the systematic review performed by Costa et al. who reported that nutritionally depleted patients may experience worse clinical outcomes [24].
Additionally, the energy and protein delivery levels of the patients in the two groups were at an acceptable range. These findings may be inconsistent with those of some previously published articles. Accordingly, these disagreements may be due to different study populations as most of the studied patients were critically ill patients with abdominal/neurosurgical underlying diseases [16, 25-27]. Additionally, the presence of nutritionists in daily medical team visits in our study may be another effective factor affecting the nutrient delivery of the studied patients. Moreover, as nutrition delivery is considered an effective factor in clinical outcomes, this acceptable status would influence the recorded clinical outcomes in the present study as well [26, 28]. Consistently, energy intake had a negative association with infection rate. In addition, lower protein delivery was found to be negatively associated with prolonged mechanical ventilation.
The present study was the second retrospective study conducted on the nutritional adequacy of the critically ill children in our referral PICU. Accordingly, the nutrition support indices obviously improved following the regular daily presence of nutritionists in medical staff team visits [25]. Additionally, our study investigated the nutritional adequacy of gastrointestinal surgical critically ill neonates and showed a high prevalence of underfeeding in such patients [16]. The aforementioned issue highlights the importance of the necessity of coordinated teamwork for the better management of PICU patients.
However, recording no nutrient delivery barriers was the main limitation of the present study, because we cannot have an evidence-based judgment on the probable barriers to optimum nutrient delivery in our PICU to make more realistic decisions. For example, rare post-pyloric tube insertion obviously was a routine barrier for us, but we found no records in hospital documents regarding this issue. Moreover, as our ward was not considered as a referral PICU for nephrological and oncological patients as well as cardiac surgical subjects, we cannot generalize the obtained results to all pediatric critically ill patients. Therefore, performing further prospective, large-population-based, multi-center studies is necessary to have a proper realistic opinion on the current nutrition support status and the nutrient delivery barriers in PICU patients. This step would be an important pivotal step to make customized nutrition support instructions and guidelines for such patients.
5. Conclusion
According to the results of the present study, energy and nutrient delivery levels were at acceptable status in 78.9% of the critically ill children with non-surgical underlying diseases and in 86.5% of the surgical PICU patients. The EN was the most frequent route used for feeding critically ill children with surgical underlying diseases and the combination of EN and PN was more used for the patients admitted to PICU due to non-surgical underlying diseases. This finding revealed the improved quality of nutrition support services during the last year. Moreover, some significant associations between energy/protein delivery and some clinical outcomes, including mechanical ventilation duration, infection rate, length of PICU, and hospital stay indicated the necessity of further reasonable, realistic, and evidence-based nutritional interventions as well as monitoring optimal nutrition support barriers in critically ill pediatric patients.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Mashhad University of Medical Sciences (IR.MUMS.MEDICAL.REC.1399.166).
Funding
This research was supported by the research project (IR.MUMS.MEDICAL.REC.1399.166), funded by Mashhad University of Medical Sciences.
Authors' contributions
Conceptualization: Fatemeh Roudi and Gholamreza Khademi; Data Collection: Fahimeh Azadeh and Maryam Naseri; Methodology: Fatemeh Roudi and Majid Sezavar; Fatemeh Roudi: Writing–original draft and Statistical analysis; Fatemeh Roudi; Writing–Review & Editing and Supervision: Gholamreza Khademi and Majid Sezavar.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgments
We would thank all the staff of Akbar Children's Hospital for helping us, the Clinical Research Development Unit of Akbar Hospital, and the deputy of research of Mashhad University of Medical Sciences (MUMS) due to financially support of the project.
References
- Mehta NM, Duggan CP. Nutritional deficiencies during critical illness. Pediatr Clin North Am. 2009; 56(5):1143-60. [DOI:10.1016/j.pcl.2009.06.007] [PMID] [PMCID]
- Allard JP, Keller H, Jeejeebhoy KN, Laporte M, Duerksen DR, Gramlich L, et al. Decline in nutritional status is associated with prolonged length of stay in hospitalized patients admitted for 7 days or more: A prospective cohort study. Clin Nutr. 2016; 35(1):144-52. [DOI:10.1016/j.clnu.2015.01.009] [PMID]
- Hejazi N, Mazloom Z, Zand F, Rezaianzadeh A, Amini A. Nutritional assessment in critically Ill patients. Iran J Med Sci. 2016; 41(3):171-9. [PMID]
- Barker LA, Gout BS, Crowe TC. Hospital malnutrition: Prevalence, identification and impact on patients and the healthcare system. Int J Environ Res Public Health. 2011; 8(2):514-27. [DOI:10.3390/ijerph8020514] [PMID] [PMCID]
- Prieto MB, Cid JL. Malnutrition in the critically ill child: The importance of enteral nutrition. Int J Environ Res Public Health. 2011; 8(11):4353-66. [DOI:10.3390/ijerph8114353] [PMID] [PMCID]
- Reid ME, Stratton MS, Lillico AJ, Fakih M, Natarajan R, Clark LC, et al. A report of high-dose selenium supplementation: Response and toxicities. J Trace Elem Med Biol. 2004; 18(1):69-74. [DOI:10.1016/j.jtemb.2004.03.004] [PMID]
- Elia M. Defining, recognizing, and reporting malnutrition. Int J Low Extrem Wounds. 2017; 16(4):230-7. [DOI:10.1177/1534734617733902] [PMID]
- Roudi F, Zakerian M, Ranjbar G. The beneficial anti-inflammatory and anti-oxidative effects of selenium supplementation in critically Ill post-surgical pediatric patients. J Nutr Fasting Health. 2020; 8(2):75-9. [DOI:10.22038/JNFH.2019.42549.1213]
- Álvarez-Hernández J, Planas Vila M, León-Sanz M, García de Lorenzo A, Celaya-Pérez S, García-Lorda P, et al. Prevalence and costs of malnutrition in hospitalized patients; The PREDyCES Study. Nutr Hosp. 2012; 27(4):1049-59. [PMID]
- Roudi F, Khademi G, Ranjbar G, Rafatpanah H, Esmaily H, Nematy M. Effects of high-dose selenium supplementation on oxidative stress and inflammatory markers in critically ill children after gastrointestinal surgery: A randomized clinical trial. Iran J Pediatr. 2020; 30(4):e102118. [DOI:10.5812/ijp.102118]
- Roudi F, Sezavar M, Rajabi O, Safarian M, Khademi G, Nematy M, et al. The effects of high-dose selenium supplementation on the oxidative stress status and inflammatory markers in critically ill pediatric patients after gastrointestinal surgery: A randomized clinical trial protocol study. J Nutr Fasting Health. 2020; 8(3):159-68. [DOI:10.22038/JNFH.2020.48170.1261]
- Nagrath D, Ghosh Jerath S, Jerath N, Gagneja K. Abstract P-255: Evaluation of adequacy of nutritional support in critically ill children in a tertiary level paediatric intensive care unit (Picu) in New Delhi, India. Pediatr Crit Care Med. 2018; 19(65):124-5. [DOI:10.1097/01.pcc.0000537712.75150.25]
- Joosten K, Embleton N, Yan W, Senterre T; ESPGHAN/ESPEN/ESPR/CSPEN working group on pediatric parenteral nutrition. ESPGHAN/ESPEN/ESPR/CSPEN guidelines on pediatric parenteral nutrition: Energy. Clin Nutr. 2018; 37(6 Pt B):2309-14. [DOI:10.1016/j.clnu.2018.06.944] [PMID]
- Mihatsch W, Shamir R, van Goudoever JB, Fewtrell M, Lapillonne A, Lohner S, et al. ESPGHAN/ESPEN/ESPR/CSPEN guidelines on pediatric parenteral nutrition: Guideline development process for the updated guidelines. Clin Nutr. 2018; 37(6 Pt B):2306-8. [DOI:10.1016/j.clnu.2018.06.943]
- Mehta NM, Compher C; A.S.P.E.N. Board of Directors. A.S.P.E.N. Clinical Guidelines: Nutrition support of the critically ill child. JPEN J Parenter Enteral Nutr. 2009; 33(3):260-76. [DOI:10.1177/0148607109333114] [PMID]
- Boskabady A, Dehnavi Z, Khademi G, Nematy M, Esmaily H, Roudi F. Nutritional support of critically ill neonates in post-gastrointestinal surgery state: Adequacy and barriers. Iran J Neonatol. 2020; 11(4):57-63. [DOI:10.22038/IJN.2020.46286.1782]
- Abad-Jorge A. Nutrition management of the critically ill pediatric patient: Minimizing Barriers to optimal nutrition support. Child Obes Nutr. 2013; 5(4):221-30. [DOI:10.1177/1941406413492821]
- Bronsky J, Campoy C, Braegger C; ESPGHAN/ESPEN/ESPR/CSPEN working group on pediatric parenteral nutrition. ESPGHAN/ESPEN/ESPR/CSPEN guidelines on pediatric parenteral nutrition: Vitamins. Clin Nutr. 2018; 37(6 Pt B):2366-78. [PMID]
- Domellöf M, Szitanyi P, Simchowitz V, Franz A, Mimouni F; ESPGHAN/ESPEN/ESPR/CSPEN working group on pediatric parenteral nutrition. ESPGHAN/ESPEN/ESPR/CSPEN guidelines on pediatric parenteral nutrition: Iron and trace minerals. Clin Nutr. 2018; 37(6 Pt B):2354-9. [PMID]
- Khademi G, Imani B, Mehdizadeh A. Assessment, intervention, and monitoring: Stepwise nutritional management in pediatric intensive care units: A short review. J Compr Ped. 2019; 10(1):e66474. [DOI:10.5812/compreped.66474]
- Khademi G, Nematy M, Ranjbar G, Pouryazdanpanah M, Rahimi R, Roudi F. Clinical nutrition approaches to medical management of children with obesity and critical illnesses. J Compr Ped. 2019; 11(1):e92108. [DOI:10.5812/compreped.92108]
- Mehta NM, Skillman HE, Irving SY, Coss-Bu JA, Vermilyea S, Farrington EA, et al. Guidelines for the provision and assessment of nutrition support therapy in the pediatric critically ill patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition. JPEN J Parenter Enteral Nutr. 2017; 41(5):706-42. [DOI:10.1177/0148607117711387] [PMID]
- Grippa RB, Silva PS, Barbosa E, Bresolin NL, Mehta NM, Moreno YM. Nutritional status as a predictor of duration of mechanical ventilation in critically ill children. Nutrition. 2017; 33:91-5. [DOI:10.1016/j.nut.2016.05.002] [PMID]
- Costa CA, Tonial CT, Garcia PC. Association between nutritional status and outcomes in critically-ill pediatric patients a systematic review. J Pediatr (Rio J). 2016; 92(3):223-9. [PMID]
- Roudi F, Nematy M, Khademi G, Safarian M, Sezavar M. Nutritional adequacy of children with critical illnesses: Where are we now? Clin Nutr ESPEN. 2020; 40:671. [DOI:10.1016/j.clnesp.2020.09.800]
- Kyle UG, Jaimon N, Coss-Bu JA. Nutrition Support in Critically Ill Children: Underdelivery of energy and protein compared with current recommendations. J Acad Nutr Diet. 2012; 112(12):1987-92. [DOI:10.1016/j.jand.2012.07.038] [PMID]
- Rogers EJ, Gilbertson HR, Heine RG, Henning R. Barriers to adequate nutrition in critically ill children. Nutrition. 2003; 19(10):865-8. [DOI:10.1016/S0899-9007(03)00170-9]
- Mehta NM, Bechard LJ, Cahill N, Wang M, Day A, Duggan CP, et al. Nutritional practices and their relationship to clinical outcomes in critically ill children--an international multicenter cohort study. Crit Care Med. 2012; 40(7):2204-11. [PMID]
Type of Study: Original Article |
Subject:
Pediatric Intensivist
Received: 2021/08/4 | Accepted: 2021/11/8 | Published: 2022/04/25
Received: 2021/08/4 | Accepted: 2021/11/8 | Published: 2022/04/25
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








