Volume 13, Issue 1 (1-2025)
J. Pediatr. Rev 2025, 13(1): 65-72 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sadeghi M, Razavi Z, Khanlarzade E. A Comparative Study Between the Frequency of New Cases of Type 1 Diabetes Two Years Before and Two Years During COVID-19 Pandemic in Be’sat Hospital, Hamadan City, Iran. J. Pediatr. Rev 2025; 13 (1) :65-72
URL: http://jpr.mazums.ac.ir/article-1-639-en.html
URL: http://jpr.mazums.ac.ir/article-1-639-en.html
1- School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran.
2- Department of Pediatrics, School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran. ,razavizahra@yahoo.com
3- Department of Community Medicine, School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran.
2- Department of Pediatrics, School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran. ,
3- Department of Community Medicine, School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran.
Full-Text [PDF 376 kb]
(691 Downloads)
| Abstract (HTML) (1790 Views)
Full-Text: (457 Views)
Introduction
Following the emergence of COVID-19 disease in December 2019 in Wuhan, China, and its rapid change into a global pandemic, millions of people died in the world [1]. Severe acute respiratory syndrome coronavirus 2 became a newly emerging viral disease that caused serious complications in people with chronic diseases, changed the pattern and severity of morbidities, and increased the incidence of other diseases. A few recent studies indicated that the incidence of type 1 diabetes had increased during the COVID-19 pandemic [2, 3]. An increase in new cases of type 1 diabetes is expected by triggering islet cell autoimmunity following this viral infection or as the effects of its vaccines [4, 5]. There is limited data regarding the increased incidence of type 1 diabetes mellitus (T1DM) during the COVID-19 pandemic [6, 7]. In addition, there are conflicting results regarding the incidence of newly diagnosed T1DM in children during the COVID-19 pandemic [8].
Given the limited information about the short- and long-term effects of SARS-CoV-2 on the incidence of autoimmune diseases, this study aimed to determine the impact of the COVID-19 pandemic on the frequency of T1DM and compare the obtained data with pre-pandemic period. The results of this study can enrich our epidemiological data on the role of the COVID-19 epidemic as a trigger for type 1 diabetes.
Methods
This research is a retrospective cross-sectional study in Be’sat Hospital, Hamadan City, Iran, in 2023. The hospital is where the newly diagnosed cases of T1DM are registered. We assessed and compared the frequency of new cases of T1DM. Our hospital is a tertiary referral center, and all patients with newly diagnosed type 1 diabetes are admitted to this center to assess the required daily dose of insulin and educate the patients and their families about living with T1DM. All new diabetic subjects younger than 19 years registered as “new cases of T1DM” in the hospital’s archive from March 2018 to March 2022 were included. Those without the required information of the study were excluded.
The primary outcome was the frequency of new cases of T1DM with or without diabetic ketoacidosis (DKA) at presentation two years before and during the first 2 years of the COVID-19 pandemic. Required information included age, gender, seasonality of disease onset, place of residence, clinical and laboratory characteristics, duration of clinical symptoms before diagnosis, type of feeding during infancy, maternal factors during pregnancy, incidence of COVID-19 disease in patients and their families were extracted from the medical records of the patients. The inclusion criteria were the diagnosis of type 1 diabetes between March 2018 and March 2022. The exclusion criteria were incomplete information and lacking access to the participants’ parents to complete the questionnaire. Missing data were supplemented by telephone contact with the participants. All study variables were collected retrospectively and compared with the frequency two years before the COVID-19 pandemic.
The diagnosis of T1DM was confirmed by a pediatric endocrinologist based on the following laboratory measurements [9]: The presence of classic symptoms of hyperglycemia (polydipsia, polyuria), weight loss, random plasma glucose ≥200 mg/dL or fasting glucose level ≥126 mg accompanied by the daily need for insulin injection. The International Society for Pediatric and Adolescent Diabetes (ISPAD) guidelines were used to define DKA criteria [10].
Statistical analysis
Data were analyzed using SPSS software, version 26. The Mean±SD were used to describe the participants’ quantitative characteristics. The student t-test was used to compare the frequency of T1DM before and during the COVID-19 pandemic. The chi-squared test and Fisher exact test were used to compare qualitative data. A P<0.05 was considered statistically significant.
Results
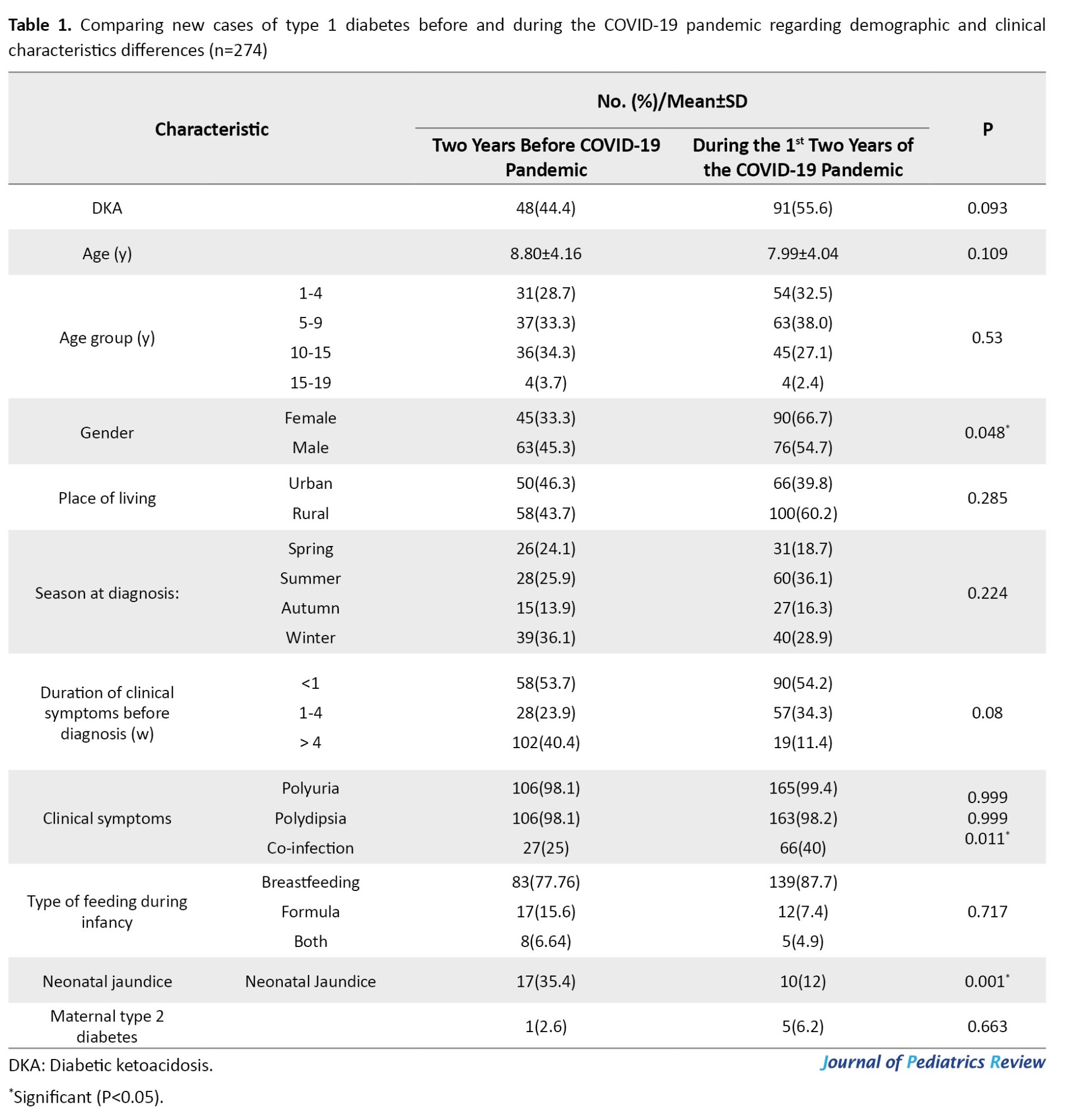
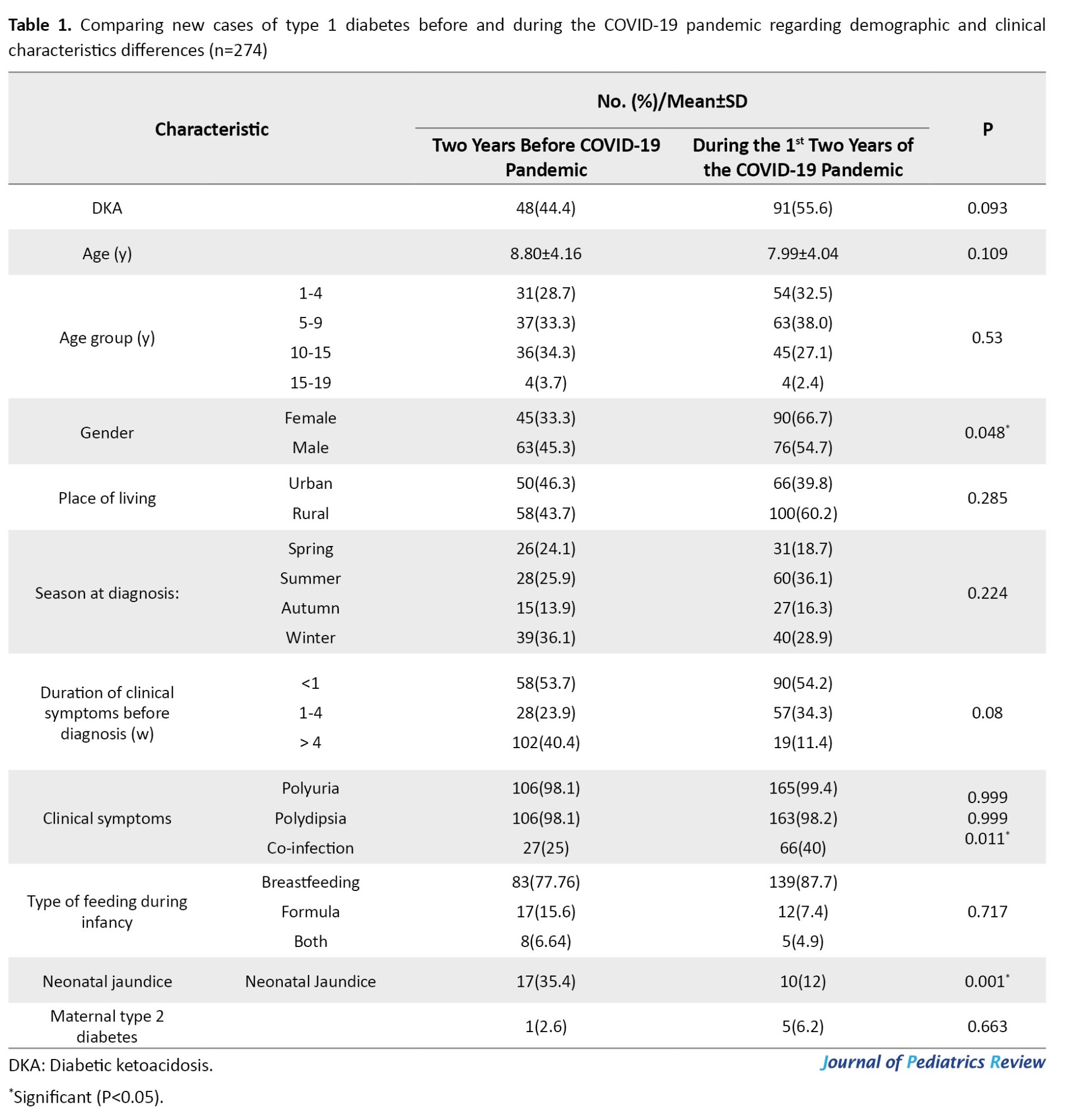
In total, 274 new cases of diabetes were included in the study. The characteristics of the studied population are shown in Table 1.
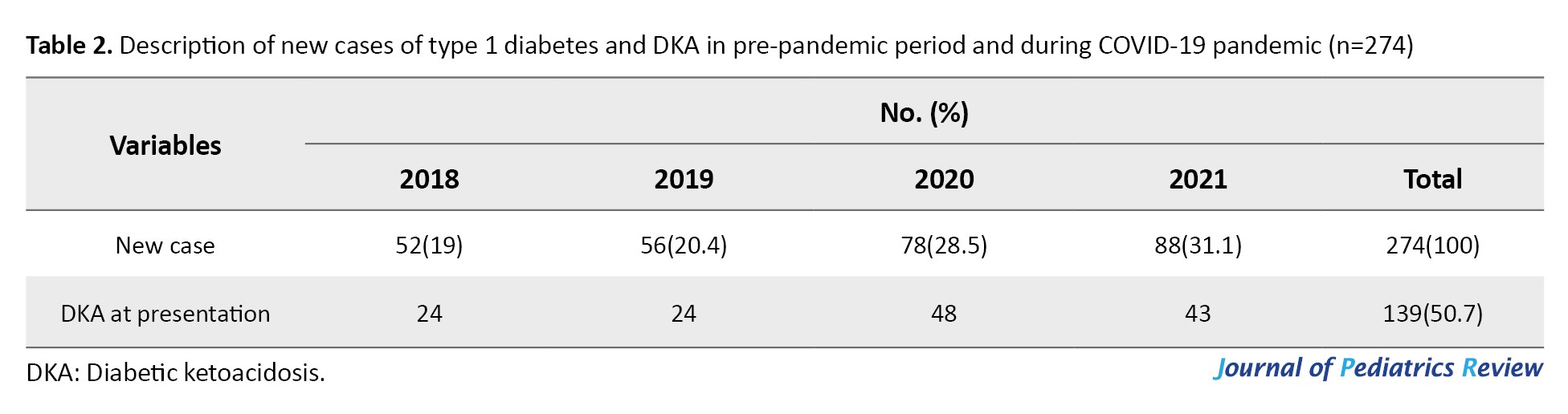
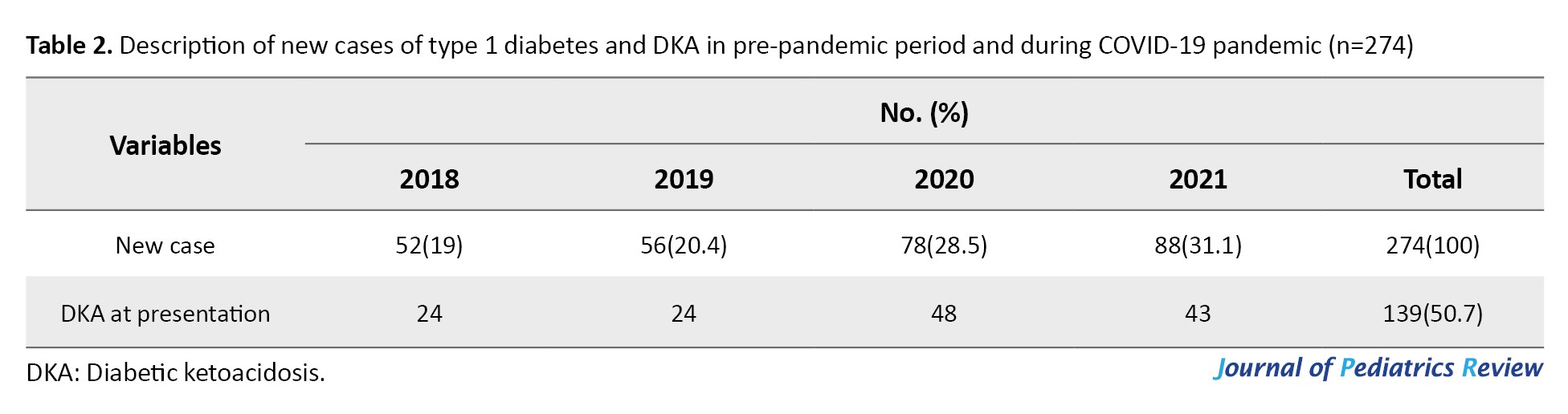
The frequency rates of new cases of T1DM during 2018, 2019, 2020, and 2021 were 52, 56, 78, and 88, respectively. The occurrence of new cases of T1DM increased significantly during the COVID-19 pandemic. The frequencies of new cases of T1DM and DKA at presentation before and during the COVID-19 pandemic are presented in Table 2.
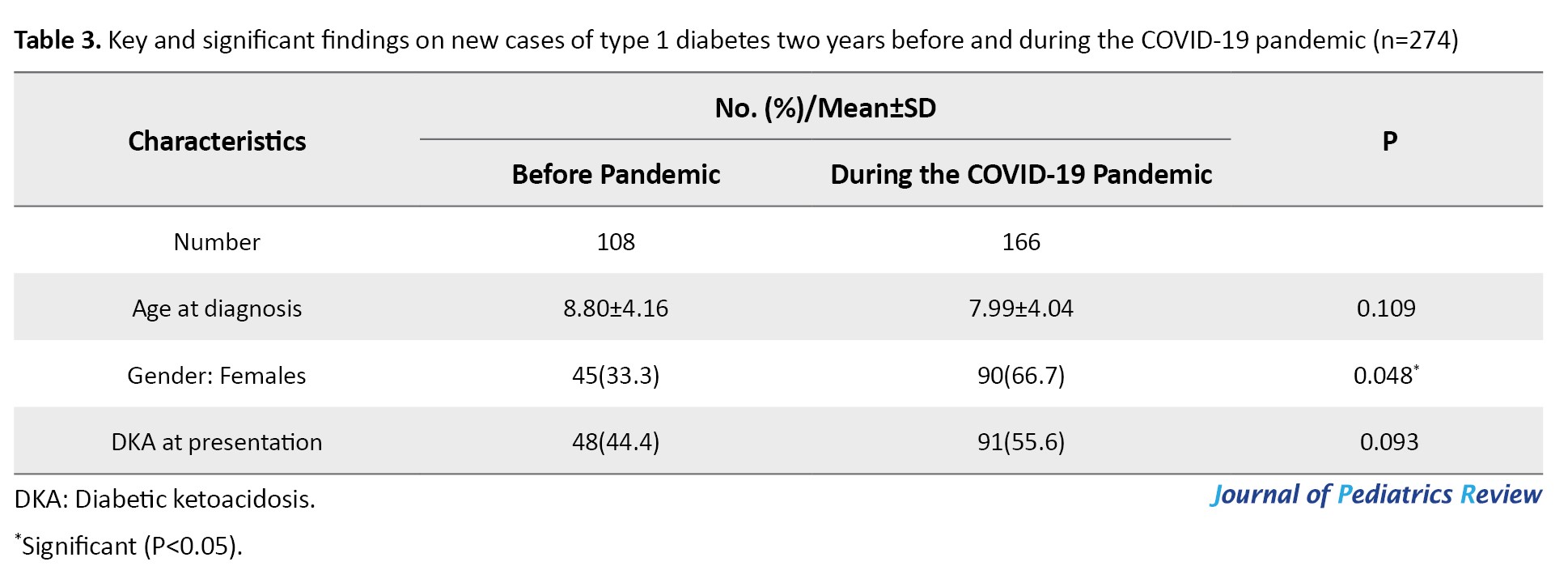
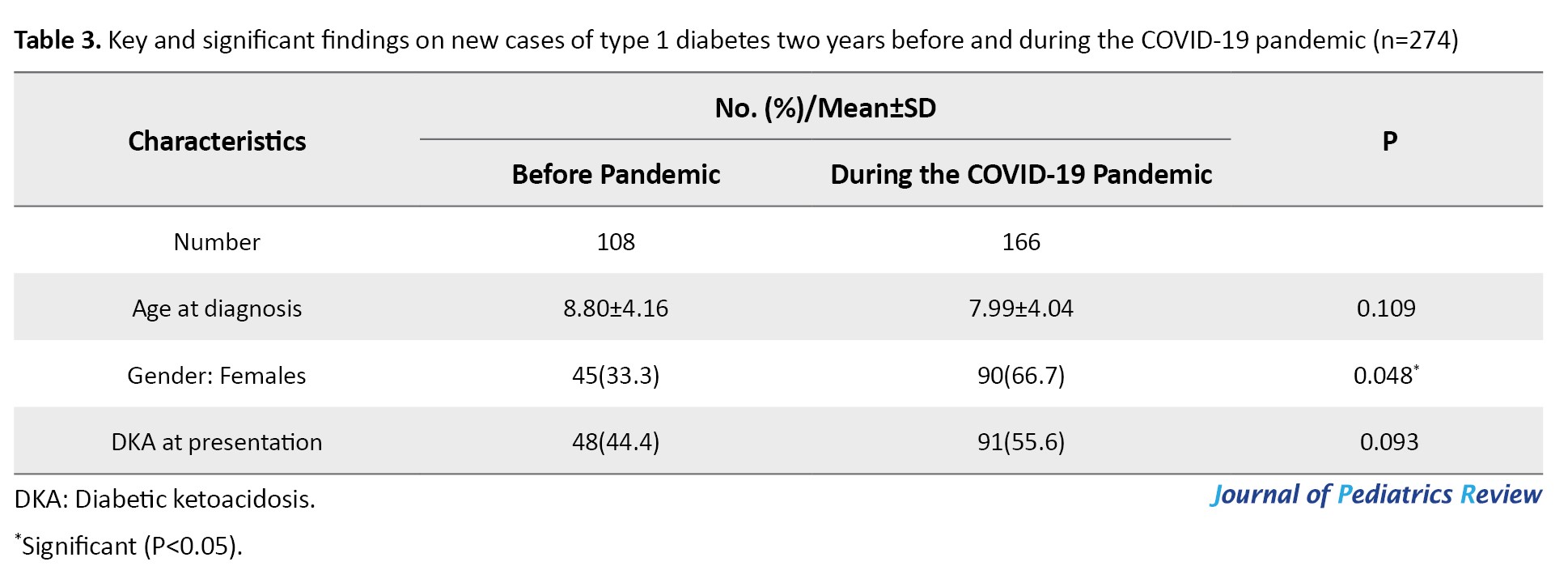
The Mean±SD ages of the study population before and during the COVID-19 pandemic were 8.80±4.16 and 7.99±4.04 years, respectively. There was no significant difference between the mean age of diagnosis of patients with T1DM two years before and during the COVID-19 pandemic (P=0.109). During the COVID-19 pandemic, most patients with type 1 diabetes were in the age group of 1-4 and 5-9 years, whereas two years earlier, most cases were in the age group of 5-9 and 10-14 years. However, there was no significant difference between the age groups of patients before and during the COVID-19 pandemic (P=0.53). During the COVID-19 pandemic, the frequency of new cases of type 1 diabetes was higher in girls than boys. This ratio was significantly higher than before the pandemic (P=0.048). The data of this study showed that the frequency of cases of ketoacidosis at the onset of T1DM during the COVID-19 crisis was higher than two years before (55.2 vs 44.5). However, this difference was not statistically significant. During the COVID-19 crisis, most cases of T1DM occurred in summer, whereas two years earlier, most cases were diagnosed in winter (P=0.224). There was no significant difference in the place of living before and during the COVID-19 pandemic. No significant difference was observed between new cases of type 1 diabetes two years before and during the COVID-19 pandemic in terms of duration and initial clinical symptoms, including polyuria and polydipsia (P=0.08 and P=0.99, respectively). No significant difference was observed between new cases of T1DM during the COVID-19 pandemic and the pre-pandemic period in terms of history of gestational diabetes, type of infant feeding, and other perinatal factors. However, the frequency of neonatal jaundice in patients diagnosed before the COVID-19 pandemic was significantly higher than during the COVID-19 pandemic (P=0.001). The frequency of history of previous or concurrent COVID-19 infection in the participants and their close relatives was 42(25.3%) and 37(22.3%), respectively. The prominent and significant data of the study are presented in Table 3.
Discussion
Several recently published articles suggest that the COVID-19 pandemic has increased the incidence of type 1 diabetes or DKA in children. However, the data in this area are controversial.
The current study’s data indicate that the frequency of type 1 diabetes has increased significantly during the COVID-19 pandemic compared to before that period. The rate of increase of newly diagnosed T1DM was 50% in the first year and 69.23% in the second year of the COVID-19 outbreak. This finding confirms the findings of studies by Unsworth et al., Dżygało et al., Al-Qahtani et al., and Vlad et al. [7, 11-13]. In confirmation of the findings of our study, Baechle et al. reported that the COVID-19 pandemic caused an increase in the number of new cases of T1DM and DKA in Germany [14]. Giorda et al. demonstrated that the incidence of T1DM increased dramatically in northern Italy during the COVID-19 pandemic [2]. A similar apparent increase in the incidence of T1DM during the COVID-19 pandemic was reported in the UK and Spain [7, 15]. A review and meta-analysis conducted by Rahmati et al. regarding the global impact of the COVID-19 pandemic on the incidence of new cases of type 1 diabetes in children compared to the pre-pandemic period showed a 5.9% increase in the incidence of type 1 diabetes [16]. Gottesman et al. evaluated the incidence of newly diagnosed type 1 diabetes among children in the United States during the COVID-19 pandemic years and compared data to the pre-pandemic period and found a 57% increase in hospitalizations due to type 1 diabetes [3]. Salmi et al. conducted a similar retrospective cohort study in Finland and reported an increase in the incidence of new cases of type 1 diabetes in 2020 compared to the years before the COVID-19 pandemic [17]. The findings of our study are consistent with the results of these studies on the increase in new cases of type 1 diabetes during the COVID-19 crisis. However, some other authors believe that it is too early to judge whether the COVID-19 pandemic has increased the incidence of type 1 diabetes or itself causes T1DM [18-20].
There is no clear mechanism that can explain the increase in the incidence of type 1 diabetes during the COVID-19 pandemic. A potential explanation is that SARS-CoV-2 infection may cause dysregulation of glucose metabolism, and thus, susceptible children may develop diabetes following SARS-CoV-2 infection. SARS-CoV-2 virus may also be a potential and novel trigger of beta-cell autoimmune destruction [7, 13]. In our study, nearly 75% of the participants had no history of COVID-19 infection. Similar reports describe several children with new-onset diabetes unrelated to infection during the COVID-19 pandemic [7, 21]. Another explanation is that COVID-19 or subsequent lockdown as a stressful event may trigger type 1 diabetes [6, 10].
Consistent with numerous reports [14, 22, 23], we found that the COVID-19 pandemic has increased the frequency of DKA at the onset of T1DM. Although there is conflicting evidence regarding the prevalence of newly diagnosed T1DM in children during epidemics, all studies agree that DKA increases in frequency and severity during the diagnosis of T1DM [20]. According to the previous report by Rabbone et al. [24], we assume that the COVID-19 pandemic may have changed the clinical presentation of T1DM. Contrary to our hypothesis, previous authors believed that more cases of ketoacidosis during the COVID-19 crisis may result from parents’ delayed search for medical assistance due to the fear of becoming infected with SARS-CoV-2 [20, 22, 25]. This study found more cases of the disease in the age group of 4-9 years than before the pandemic. A difference in age distribution was found by Leiva-Gea et al., which showed an increase in the number of T1DM in children less than 4 years of age [26].
In the present study, the frequency of new cases of T1DM in girls was significantly higher than in boys during the COVID-19 crisis. Consistent with our findings, Gottesman et al. in the United States found a higher incidence of new cases of type 1 diabetes in girls compared to boys during the pandemic (7.56% vs 3.43%) [3]. However, in a study by Matsuda et al. in Japan, the incidence of type 1 diabetes during the COVID-19 pandemic in boys under 15 years was higher than the overall incidence (1.8% vs 3.5%) [19]. Similarly, in the study by Kamrath et al. in Germany, boys accounted for 55.6% of the patients [25]. Overall, there are conflicting results regarding the gender differences of T1DM during the COVID-19 pandemic in different parts of the world. The results of the current study revealed that during the COVID-19 crisis, an increasing trend of T1D onset from winter to summer was found. However, the seasonality pattern of new onsets was not significantly different during the COVID-19 year compared to the previous year. Kostopoulou et al. [18] reported a different seasonality of new-onset T1DM during COVID-19 compared to the previous year, with an increasing trend from spring to winter.
Conclusion
A significant increase in the frequency of T1DM was observed during the two years of the COVID-19 crisis. The frequency of new cases of type 1 diabetes was higher in girls than boys during the COVID-19 crisis. The history of neonatal jaundice in patients diagnosed before the COVID-19 pandemic was significantly higher than that during the COVID-19 pandemic. The presence or history of infectious diseases, including COVID-19, was higher during the pandemic (P=0.011).
Further research should investigate the long-term impact of SARS-CoV-2 on the incidence of diabetes, ketoacidosis, and its characteristics, clarify its mechanism, and identify the causes of high incidence and preventive interventions in this field.
Study limitations
Our study has some limitations. First, this study was conducted in only one center, which may differ from other provinces in terms of the state of the COVID-19 crisis and the prevalence of infection. Therefore, the study results cannot be generalized to other regions of the country. Further research should investigate the effect of SARS-CoV-2 on the incidence of diabetes in Iran. Secondly, some cases may not have been included in the study due to the unavailability of their information or referrals to other centers. Third, this study shows the short-term effects of COVID-19 on the incidence of type 1 diabetes. Further studies are needed to examine the background information, data on specific antibodies to COVID-19 in patients with newly diagnosed T1DM, and the long-term effects of the COVID-19 virus on the incidence of type 1 diabetes. At that time, it is possible to comment more confidently about the impact of the COVID-19 crisis on the occurrence of type 1 diabetes.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Hamadan University of Medical Sciences, Hamadan, Iran (Code: IR.UMSHA.REC.1401.3690).
Funding
This paper was extracted from the PhD dissertation of Mina Sadeghi, approved by the School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran. This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Investigation, review and editing: Mina Sadeghi and Zahra Razavi; Data acquisition: Mina Sadeghi; Data analysis, interpretation, writing the original draft, and final approval: All authors.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors thank all patients who participated in the study. The authors are sincerely grateful to the staff of the Medical Records Archive of Hamadan Be’sat Hospital for their help in completing this research. The authors also would like to express their thanks to the staff of the Clinical Research Center of Be’sat Hospital, Hamadan University of Medical Sciences, Hamadan, Iran, for their cooperation in conducting this research.
References
Following the emergence of COVID-19 disease in December 2019 in Wuhan, China, and its rapid change into a global pandemic, millions of people died in the world [1]. Severe acute respiratory syndrome coronavirus 2 became a newly emerging viral disease that caused serious complications in people with chronic diseases, changed the pattern and severity of morbidities, and increased the incidence of other diseases. A few recent studies indicated that the incidence of type 1 diabetes had increased during the COVID-19 pandemic [2, 3]. An increase in new cases of type 1 diabetes is expected by triggering islet cell autoimmunity following this viral infection or as the effects of its vaccines [4, 5]. There is limited data regarding the increased incidence of type 1 diabetes mellitus (T1DM) during the COVID-19 pandemic [6, 7]. In addition, there are conflicting results regarding the incidence of newly diagnosed T1DM in children during the COVID-19 pandemic [8].
Given the limited information about the short- and long-term effects of SARS-CoV-2 on the incidence of autoimmune diseases, this study aimed to determine the impact of the COVID-19 pandemic on the frequency of T1DM and compare the obtained data with pre-pandemic period. The results of this study can enrich our epidemiological data on the role of the COVID-19 epidemic as a trigger for type 1 diabetes.
Methods
This research is a retrospective cross-sectional study in Be’sat Hospital, Hamadan City, Iran, in 2023. The hospital is where the newly diagnosed cases of T1DM are registered. We assessed and compared the frequency of new cases of T1DM. Our hospital is a tertiary referral center, and all patients with newly diagnosed type 1 diabetes are admitted to this center to assess the required daily dose of insulin and educate the patients and their families about living with T1DM. All new diabetic subjects younger than 19 years registered as “new cases of T1DM” in the hospital’s archive from March 2018 to March 2022 were included. Those without the required information of the study were excluded.
The primary outcome was the frequency of new cases of T1DM with or without diabetic ketoacidosis (DKA) at presentation two years before and during the first 2 years of the COVID-19 pandemic. Required information included age, gender, seasonality of disease onset, place of residence, clinical and laboratory characteristics, duration of clinical symptoms before diagnosis, type of feeding during infancy, maternal factors during pregnancy, incidence of COVID-19 disease in patients and their families were extracted from the medical records of the patients. The inclusion criteria were the diagnosis of type 1 diabetes between March 2018 and March 2022. The exclusion criteria were incomplete information and lacking access to the participants’ parents to complete the questionnaire. Missing data were supplemented by telephone contact with the participants. All study variables were collected retrospectively and compared with the frequency two years before the COVID-19 pandemic.
The diagnosis of T1DM was confirmed by a pediatric endocrinologist based on the following laboratory measurements [9]: The presence of classic symptoms of hyperglycemia (polydipsia, polyuria), weight loss, random plasma glucose ≥200 mg/dL or fasting glucose level ≥126 mg accompanied by the daily need for insulin injection. The International Society for Pediatric and Adolescent Diabetes (ISPAD) guidelines were used to define DKA criteria [10].
Statistical analysis
Data were analyzed using SPSS software, version 26. The Mean±SD were used to describe the participants’ quantitative characteristics. The student t-test was used to compare the frequency of T1DM before and during the COVID-19 pandemic. The chi-squared test and Fisher exact test were used to compare qualitative data. A P<0.05 was considered statistically significant.
Results
In total, 274 new cases of diabetes were included in the study. The characteristics of the studied population are shown in Table 1.
The frequency rates of new cases of T1DM during 2018, 2019, 2020, and 2021 were 52, 56, 78, and 88, respectively. The occurrence of new cases of T1DM increased significantly during the COVID-19 pandemic. The frequencies of new cases of T1DM and DKA at presentation before and during the COVID-19 pandemic are presented in Table 2.
The Mean±SD ages of the study population before and during the COVID-19 pandemic were 8.80±4.16 and 7.99±4.04 years, respectively. There was no significant difference between the mean age of diagnosis of patients with T1DM two years before and during the COVID-19 pandemic (P=0.109). During the COVID-19 pandemic, most patients with type 1 diabetes were in the age group of 1-4 and 5-9 years, whereas two years earlier, most cases were in the age group of 5-9 and 10-14 years. However, there was no significant difference between the age groups of patients before and during the COVID-19 pandemic (P=0.53). During the COVID-19 pandemic, the frequency of new cases of type 1 diabetes was higher in girls than boys. This ratio was significantly higher than before the pandemic (P=0.048). The data of this study showed that the frequency of cases of ketoacidosis at the onset of T1DM during the COVID-19 crisis was higher than two years before (55.2 vs 44.5). However, this difference was not statistically significant. During the COVID-19 crisis, most cases of T1DM occurred in summer, whereas two years earlier, most cases were diagnosed in winter (P=0.224). There was no significant difference in the place of living before and during the COVID-19 pandemic. No significant difference was observed between new cases of type 1 diabetes two years before and during the COVID-19 pandemic in terms of duration and initial clinical symptoms, including polyuria and polydipsia (P=0.08 and P=0.99, respectively). No significant difference was observed between new cases of T1DM during the COVID-19 pandemic and the pre-pandemic period in terms of history of gestational diabetes, type of infant feeding, and other perinatal factors. However, the frequency of neonatal jaundice in patients diagnosed before the COVID-19 pandemic was significantly higher than during the COVID-19 pandemic (P=0.001). The frequency of history of previous or concurrent COVID-19 infection in the participants and their close relatives was 42(25.3%) and 37(22.3%), respectively. The prominent and significant data of the study are presented in Table 3.
Discussion
Several recently published articles suggest that the COVID-19 pandemic has increased the incidence of type 1 diabetes or DKA in children. However, the data in this area are controversial.
The current study’s data indicate that the frequency of type 1 diabetes has increased significantly during the COVID-19 pandemic compared to before that period. The rate of increase of newly diagnosed T1DM was 50% in the first year and 69.23% in the second year of the COVID-19 outbreak. This finding confirms the findings of studies by Unsworth et al., Dżygało et al., Al-Qahtani et al., and Vlad et al. [7, 11-13]. In confirmation of the findings of our study, Baechle et al. reported that the COVID-19 pandemic caused an increase in the number of new cases of T1DM and DKA in Germany [14]. Giorda et al. demonstrated that the incidence of T1DM increased dramatically in northern Italy during the COVID-19 pandemic [2]. A similar apparent increase in the incidence of T1DM during the COVID-19 pandemic was reported in the UK and Spain [7, 15]. A review and meta-analysis conducted by Rahmati et al. regarding the global impact of the COVID-19 pandemic on the incidence of new cases of type 1 diabetes in children compared to the pre-pandemic period showed a 5.9% increase in the incidence of type 1 diabetes [16]. Gottesman et al. evaluated the incidence of newly diagnosed type 1 diabetes among children in the United States during the COVID-19 pandemic years and compared data to the pre-pandemic period and found a 57% increase in hospitalizations due to type 1 diabetes [3]. Salmi et al. conducted a similar retrospective cohort study in Finland and reported an increase in the incidence of new cases of type 1 diabetes in 2020 compared to the years before the COVID-19 pandemic [17]. The findings of our study are consistent with the results of these studies on the increase in new cases of type 1 diabetes during the COVID-19 crisis. However, some other authors believe that it is too early to judge whether the COVID-19 pandemic has increased the incidence of type 1 diabetes or itself causes T1DM [18-20].
There is no clear mechanism that can explain the increase in the incidence of type 1 diabetes during the COVID-19 pandemic. A potential explanation is that SARS-CoV-2 infection may cause dysregulation of glucose metabolism, and thus, susceptible children may develop diabetes following SARS-CoV-2 infection. SARS-CoV-2 virus may also be a potential and novel trigger of beta-cell autoimmune destruction [7, 13]. In our study, nearly 75% of the participants had no history of COVID-19 infection. Similar reports describe several children with new-onset diabetes unrelated to infection during the COVID-19 pandemic [7, 21]. Another explanation is that COVID-19 or subsequent lockdown as a stressful event may trigger type 1 diabetes [6, 10].
Consistent with numerous reports [14, 22, 23], we found that the COVID-19 pandemic has increased the frequency of DKA at the onset of T1DM. Although there is conflicting evidence regarding the prevalence of newly diagnosed T1DM in children during epidemics, all studies agree that DKA increases in frequency and severity during the diagnosis of T1DM [20]. According to the previous report by Rabbone et al. [24], we assume that the COVID-19 pandemic may have changed the clinical presentation of T1DM. Contrary to our hypothesis, previous authors believed that more cases of ketoacidosis during the COVID-19 crisis may result from parents’ delayed search for medical assistance due to the fear of becoming infected with SARS-CoV-2 [20, 22, 25]. This study found more cases of the disease in the age group of 4-9 years than before the pandemic. A difference in age distribution was found by Leiva-Gea et al., which showed an increase in the number of T1DM in children less than 4 years of age [26].
In the present study, the frequency of new cases of T1DM in girls was significantly higher than in boys during the COVID-19 crisis. Consistent with our findings, Gottesman et al. in the United States found a higher incidence of new cases of type 1 diabetes in girls compared to boys during the pandemic (7.56% vs 3.43%) [3]. However, in a study by Matsuda et al. in Japan, the incidence of type 1 diabetes during the COVID-19 pandemic in boys under 15 years was higher than the overall incidence (1.8% vs 3.5%) [19]. Similarly, in the study by Kamrath et al. in Germany, boys accounted for 55.6% of the patients [25]. Overall, there are conflicting results regarding the gender differences of T1DM during the COVID-19 pandemic in different parts of the world. The results of the current study revealed that during the COVID-19 crisis, an increasing trend of T1D onset from winter to summer was found. However, the seasonality pattern of new onsets was not significantly different during the COVID-19 year compared to the previous year. Kostopoulou et al. [18] reported a different seasonality of new-onset T1DM during COVID-19 compared to the previous year, with an increasing trend from spring to winter.
Conclusion
A significant increase in the frequency of T1DM was observed during the two years of the COVID-19 crisis. The frequency of new cases of type 1 diabetes was higher in girls than boys during the COVID-19 crisis. The history of neonatal jaundice in patients diagnosed before the COVID-19 pandemic was significantly higher than that during the COVID-19 pandemic. The presence or history of infectious diseases, including COVID-19, was higher during the pandemic (P=0.011).
Further research should investigate the long-term impact of SARS-CoV-2 on the incidence of diabetes, ketoacidosis, and its characteristics, clarify its mechanism, and identify the causes of high incidence and preventive interventions in this field.
Study limitations
Our study has some limitations. First, this study was conducted in only one center, which may differ from other provinces in terms of the state of the COVID-19 crisis and the prevalence of infection. Therefore, the study results cannot be generalized to other regions of the country. Further research should investigate the effect of SARS-CoV-2 on the incidence of diabetes in Iran. Secondly, some cases may not have been included in the study due to the unavailability of their information or referrals to other centers. Third, this study shows the short-term effects of COVID-19 on the incidence of type 1 diabetes. Further studies are needed to examine the background information, data on specific antibodies to COVID-19 in patients with newly diagnosed T1DM, and the long-term effects of the COVID-19 virus on the incidence of type 1 diabetes. At that time, it is possible to comment more confidently about the impact of the COVID-19 crisis on the occurrence of type 1 diabetes.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Hamadan University of Medical Sciences, Hamadan, Iran (Code: IR.UMSHA.REC.1401.3690).
Funding
This paper was extracted from the PhD dissertation of Mina Sadeghi, approved by the School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran. This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Investigation, review and editing: Mina Sadeghi and Zahra Razavi; Data acquisition: Mina Sadeghi; Data analysis, interpretation, writing the original draft, and final approval: All authors.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors thank all patients who participated in the study. The authors are sincerely grateful to the staff of the Medical Records Archive of Hamadan Be’sat Hospital for their help in completing this research. The authors also would like to express their thanks to the staff of the Clinical Research Center of Be’sat Hospital, Hamadan University of Medical Sciences, Hamadan, Iran, for their cooperation in conducting this research.
References
- Kim DH, Choe YJ, Jeong JY. Understanding and interpretation of case fatality rate of coronavirus disease 2019. J Korean Med Sci. 2020; 35(12):e137. [DOI:10.3346/jkms.2020.35.e137] [PMID]
- Giorda CB, Gnavi R, Tartaglino B, Manti R, Migliardi A, Favella L, et al. Increased incidence of type 1 diabetes in 2 years of COVID-19 pandemic. Acta Diabetol. 2023; 60(4):587-9. [DOI:10.1007/s00592-022-01986-w] [PMID]
- Gottesman BL, Yu J, Tanaka C, Longhurst CA, Kim JJ. Incidence of new-onset type 1 diabetes among US children during the COVID-19 global pandemic. AMA Pediatr. 2022; 176(4):414-5. [DOI:10.1001/jamapediatrics.2021.5801] [PMID]
- Sakurai K, Narita D, Saito N, Ueno T, Sato R, Niitsuma S, etal. Type 1 diabetes mellitus following COVID-19 RNA-based vaccine. J Diabetes Investig. 2022; 13(7):1290-2. [DOI:10.1111/jdi.13781] [PMID]
- Ata A, Jalilova A, Kırkgöz T, Işıklar H, Demir G, Altınok YA, et al. Does COVID-19 predispose patients to type 1 diabetes mellitus? Clin Pediatr Endocrinol. 2022; 31(1):33-7. [DOI:10.1297/cpe.2021-0050] [PMID]
- Tittel SR, Rosenbauer J, Kamrath C, Ziegler J, Reschke F, Hammersen J, et al. Did the COVID-19 lockdown affect the incidence of pediatric type 1 diabetes in Germany? Diabetes Care. 2020; 43(11):e172-3. [DOI:10.2337/dc20-1633] [PMID]
- Unsworth R, Wallace S, Oliver NS, Yeung S, Kshirsagar A, Naidu H, et al. New-onset type 1 diabetes in children during COVID-19: Multicenter regional findings in the UK. Diabetes Care. 2020; 43(11):e170-1. [DOI:10.2337/dc20-1551] [PMID]
- Anindya R, Rutter GA, Meur G. New-onset type 1 diabetes and severe acute respiratory syndrome coronavirus 2 infection. Immunol Cell Biol. 2023; 101(3):191-203.[DOI:10.1111/imcb.12615] [PMID]
- Craig ME, Jefferies C, Dabelea D, Balde N, Seth A, Donaghue KC, et al. ISPAD Clinical Practice Consensus Guidelines 2014. Definition, epidemiology, and classification of diabetes in children and adolescents. Pediatr Diabetes. 2014; 15(Suppl 20):4-17. [DOI:10.1111/pedi.12186] [PMID]
- Wolfsdorf JI, Allgrove J, Craig ME, Edge J, Glaser N, Jain V, et al. ISPAD clinical practice consensus guidelines 2014. diabetic ketoacidosis and hyperglycemic hyperosmolar state. Pediatr Diabetes. 2014; 15(Suppl 20):154-79.[DOI:10.1111/pedi.12165] [PMID]
- Dżygało K, Nowaczyk J, Szwilling A, Kowalska A. Increased frequency of severe diabetic ketoacidosis at type 1 diabetes onset among children during COVID-19 pandemic lockdown: An observational cohort study. Pediatr Endocrinol Diabetes Metab. 2020; 26(4):167-75. [DOI:10.5114/pedm.2020.101003] [PMID]
- Al-Qahtani MH, Bukhamseen FM, Al-Qassab AT, Yousef AA, Awary BH, Albuali WH, etal. The Impact of COVID-19 Lockdown on the Incidence of Type 1 DM and the Glycemic Control of Diabetic Children: Findings from a Teaching Hospital, Saudi Arabia. Rev Diabet Stud. 2022; 18(3):152-6. [DOI:10.1900/RDS.2022.18.152] [PMID]
- Vlad A, Serban V, Timar R, Sima A, Botea V, Albai O, et al. Increased incidence of type 1 diabetes during the covid-19 pandemic in Romanian Children. Medicina (Kaunas). 2021; 57(9):973. [DOI:10.3390/medicina57090973] [PMID]
- Baechle C, Eckert A, Kamrath C, Neu A, Manuwald U, Thiele-Schmitz S, et al. Incidence and presentation of new-onset type 1 diabetes in children and adolescents from Germany during the COVID-19 pandemic 2020 and 2021: Current data from the DPV Registry. Diabetes Res Clin Pract. 2023; 197:110559. [DOI:10.1016/j.diabres.2023.110559] [PMID]
- Hernández Herrero M, Terradas Mercader P, Latorre Martinez E, Feliu Rovira A, Rodríguez Zaragoza N, Parada Ricart E. [New diagnoses of type 1 diabetes mellitus in children during the COVID-19 pandemic. Regional multicenter study in Spain (Spanish)]. Endocrinol Diabetes Nutr. 2022; 69(9):709-14. [DOI:10.1016/j.endinu.2021.12.003]
- Rahmati M, Keshvari M, Mirnasuri S, Yon DK, Lee SW, Il Shin J, et al. The global impact of COVID-19 pandemic on the incidence of pediatric new-onset type 1 diabetes and ketoacidosis: A systematic review and meta-analysis. J Med Virol. 2022; 94(11):5112-27. [DOI:10.1002/jmv.27996] [PMID]
- Salmi H, Heinonen S, Hästbacka J, Lääperi M, Rautiainen P, Miettinen PJ, et al. New-onset type 1 diabetes in Finnish children during the COVID-19 pandemic. Arch Dis Child. 2022; 107(2):180-5. [DOI:10.1136/archdischild-2020-321220] [PMID]
- Kostopoulou E, Eliopoulou MI, Rojas Gil AP, Chrysis D. Impact of COVID-19 on new-onset type 1 diabetes mellitus - A one-year prospective study. Eur Rev Med Pharmacol Sci. 2021; 25(19):5928-35. [PMID]
- Matsuda F, Itonaga T, Maeda M, Ihara K. Long-term trends of pediatric type 1 diabetes incidence in Japan before and after the COVID-19 pandemic. Sci Rep. 2023; 13(1):5803.[DOI:10.1038/s41598-023-33037-x] [PMID]
- Boddu SK, Aurangabadkar G, Kuchay MS. New onset diabetes, type 1 diabetes and COVID-19. Diabetes Metab Syndr. 2020; 14(6):2211-7. [DOI:10.1016/j.dsx.2020.11.012] [PMID]
- International Society of Pediatric and Adolescent Diabetes (ISPAD). Summary of recommendations regarding COVID-19 in children with diabetes: Keep Calm and Mind your Diabetes Care and Public Health Advice. Pediatr Diabetes. 2020; 21(3):413-4. [DOI:10.1111/pedi.13013] [PMID]
- Basatemur E, Jones A, Peters M, Ramnarayan P. Paediatric critical care referrals of children with diabetic ketoacidosis during the COVID-19 pandemic. Arch Dis Child. 2021; 106(4):e21. [DOI:10.1136/archdischild-2020-320471] [PMID]
- Luciano TM, Halah MP, Sarti MTA, Floriano VG, da Fonseca BAL, Del Roio Liberatore R Junior, et al. DKA and new-onset type 1 diabetes in Brazilian children and adolescents during the COVID-19 pandemic. Arch Endocrinol Metab. 2022; 66(1):88-91. [DOI:10.20945/2359-3997000000433] [PMID]
- Rabbone I, Schiaffini R, Cherubini V, Maffeis C, Scaramuzza A. Diabetes Study Group of the Italian Society for Pediatric Endocrinology and Diabetes. Has Covid-19 delayed the diagnosis and worsened the presentation of type 1 diabetes in children? Diabetes Care. 2020; 43(11):2870-2. [DOI:10.2337/dc20-1321]
- Kamrath C, Rosenbauer J, Eckert AJ, Pappa A, Reschke F, Rohrer TR, et al. Incidence of COVID-19 and risk of diabetic ketoacidosis in new-onset type 1 diabetes. Pediatrics. 2021; 148(3):e2021050856. [DOI:10.1542/peds.2021-050856] [PMID]
- Leiva-Gea I, Fernández CA, Cardona-Hernandez R, Lozano MF, Bahíllo-Curieses P, Arroyo-Díez J, etal. Increased presentation of diabetic ketoacidosis and changes in age and month of type 1 diabetes at onset during the covid-19 pandemic in Spain. J Clin Med. 2022; 11(15):4338. [DOI:10.3390/jcm11154338] [PMID]
Type of Study: Original Article |
Subject:
Pediatric Endocrinology
Received: 2024/05/25 | Accepted: 2025/02/1 | Published: 2025/01/21
Received: 2024/05/25 | Accepted: 2025/02/1 | Published: 2025/01/21
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









