Volume 7, Issue 4 (10-2019)
J. Pediatr. Rev 2019, 7(4): 239-248 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bemanian M H, Arshi S, Nabavi M, Fallahpour M, Aarabi M, Karbasi M, et al . Anaphylactic Reaction to Bee Stings in the Rural Areas of Gorgan City: Iran’s First Epidemiological Study of Hymenoptera-Induced Anaphylaxis. J. Pediatr. Rev 2019; 7 (4) :239-248
URL: http://jpr.mazums.ac.ir/article-1-199-en.html
URL: http://jpr.mazums.ac.ir/article-1-199-en.html
Mohammad Hasan Bemanian1 

 , Saba Arshi1
, Saba Arshi1 

 , Mohammad Nabavi1
, Mohammad Nabavi1 

 , Morteza Fallahpour1
, Morteza Fallahpour1 

 , Mohsen Aarabi2
, Mohsen Aarabi2 

 , Maryam Karbasi3
, Maryam Karbasi3 

 , Vahid Ghobadidana4
, Vahid Ghobadidana4 

 , Mehdi Torabizadeh5
, Mehdi Torabizadeh5 

 , Mohammad reza Honarvar6
, Mohammad reza Honarvar6 

 , Seyed Ali Aghapour
, Seyed Ali Aghapour 

 7
7


 , Saba Arshi1
, Saba Arshi1 

 , Mohammad Nabavi1
, Mohammad Nabavi1 

 , Morteza Fallahpour1
, Morteza Fallahpour1 

 , Mohsen Aarabi2
, Mohsen Aarabi2 

 , Maryam Karbasi3
, Maryam Karbasi3 

 , Vahid Ghobadidana4
, Vahid Ghobadidana4 

 , Mehdi Torabizadeh5
, Mehdi Torabizadeh5 

 , Mohammad reza Honarvar6
, Mohammad reza Honarvar6 

 , Seyed Ali Aghapour
, Seyed Ali Aghapour 

 7
7
1- Department of Allergy, Rasool-e-Akram Hospital, Iran University of Medical Sciences, Tehran, Iran.
2- Health Sciences Research Center, Mazandaran University of Medical Sciences, Sari, Iran.
3- Neonatal & Children᾿s Health Research Center, Golestan University of Medical Sciences, Gorgan, Iran.
4- Asthma and Allergy Center, Branch of Academic Center and Research (ACECR), Tehran Medical Sciences, Tehran, Iran.
5- Golestan Hospital Clinical Research Development Unit, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
6- Health Management and Social Development Research Center, Golestan University of Medical Sciences, Gorgan, Iran.
7- Neonatal & Children᾿s Health Research Center, Golestan University of Medical Sciences, Gorgan, Iran. , s.a.aghapour@googlemail.com
2- Health Sciences Research Center, Mazandaran University of Medical Sciences, Sari, Iran.
3- Neonatal & Children᾿s Health Research Center, Golestan University of Medical Sciences, Gorgan, Iran.
4- Asthma and Allergy Center, Branch of Academic Center and Research (ACECR), Tehran Medical Sciences, Tehran, Iran.
5- Golestan Hospital Clinical Research Development Unit, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
6- Health Management and Social Development Research Center, Golestan University of Medical Sciences, Gorgan, Iran.
7- Neonatal & Children᾿s Health Research Center, Golestan University of Medical Sciences, Gorgan, Iran. , s.a.aghapour@googlemail.com
Keywords: Epidemiology, Bites and stings
Full-Text [PDF 418 kb]
(3038 Downloads)
| Abstract (HTML) (5888 Views)
Full-Text: (2760 Views)
1. Introduction
Bees are of the Hymenoptera family, and their sting has been among the leading causes of anaphylaxis reactions in humans for thousands of years (1, 2). The first recorded death by a bee sting was due to a Paper Wasp sting; it was related to the Egyptian pharaoh based on a Bee sting in 2000 BC. The common response to this plain sting is usually transient pain, itching, and swelling. However,, it can lead to severe localized reactions or systemic reactions. Five percent of people experience large or prolonged localized swellings at the relevant site following a bee sting. Hymenoptera is a large group of insects that include three main families; Apidate (honeybee and bumblebees), Vespidae (hornets, wasps and Yellow jackets), and Formicidae (fire ants) (3).
The incidence of deadly anaphylactic reactions caused by insect stings, like bees, is between 0.03 to 0.48 deaths per million annually, accounting for approximately 20% of deadly anaphylactic reactions. Bee sting allergy is observed in 26% of adults. However, it can increase to 30-40% in cases with a history of bee stings in recent weeks (4). With the advancement of allergy science, many preventive measures, especially therapeutic ones, have been proposed to improve the condition of patients with anaphylaxis caused by bee stings; the most important type of which are diagnostic measures for identifying the bee causing anaphylaxis and performing immunotherapy for said bee venom (5).
Extensive strategic planning and appropriate diagnostic and therapeutic measures for patients with anaphylactic reactions caused by bee stings are required to be implements; thus, health policymakers require detailed information about the various epidemiological indicators of this reaction at the national level as well as assessing physicians, medical staffs, and patients’ level of knowledge on this case. There is no comprehensive study on the frequency distribution of patients with bee sting-induced anaphylaxis reactions and their symptoms as well as the necessary diagnostic and therapeutic measures at different levels in the Iranian healthcare settings.
Golestan Province, Iran, is among the leading provinces in terms of recording and completing population health data in the country’s healthcare network. All health data is being completed in electronic form; i.e. collected and recorded online through the E-health software (NAB Program). It seems that conducting an appropriate epidemiological study in this field can provide the grounds in Golestan, as one of the leading provinces, for establishing the basis of a national registration system and database for patients with anaphylaxis reaction caused by bee stings. Accordingly, the present study was conducted to evaluate the epidemiological determinants of anaphylaxis cases caused by bee stings in Gorgan Province up to 2018.
2. Methods
This cross-sectional epidemiological study was performed on patients residing in the rural areas of Gorgan County, Iran, in 2017, with a history of anaphylactic reactions to bee stings. Patients’ data were collected through house-to-house visits by the Iranian community rural health workers (Behvarz). To record such data, patients with a history of severe bee sting allergy and those with a history of bee stings were identified in the initial stage via questionnaires completion. Then, individuals with a history of possible anaphylaxis were selected. All identified cases were referred to an allergy and clinical immunology specialist who evaluated the patient’s history of anaphylactic reactions and confirmed its cause as bee stings.
The individuals with non-systemic reactions caused by bee stings or their anaphylaxis (mild, moderate, and severe) allergy induced by a fire ant venom were excluded from the database in the final stage of registration. The census sampling method was coducted, and all the data registered in the database up to 2018 were studied. The basic information and clinical records obtained from the database were collected through oral interviews.
Statistical analysis: The obtained data were analyzed in SPSS. Quantitative and categorical qualitative variables were described using mean±SD, and frequency and percentage. The quantitative variables were compared using t-test, or Mann-Whitney U test in case of abnormal distribution. The comparison between qualitative variables was also performed using Chi-squared or Fisher›s Exact tests. Pearson’s correlation coefficient and Spearman’s rank correlation were also applied to investigate the relationships between the quantitative variables. Multivariate logistic regression analysis was used to determine the differences between the study indices in the patients; the presence of the patients› baseline, characteristics, as confounding factors, and the results were expressed as odds ratio (95% confidence interval). P<0.05 was considered as the statistical significance level.
3. Results
The required data were collected from a database of bee stings in 84 health houses in villages around Gorgan County with a population of 140000 people (NAB program). A total of 201 patients with bee sting-induced anaphylactic reaction were present in the database throughout the study period. Of them, 129(64%) were men with the Mean±SD age of 34.53±18 years, and 72(36%) patients were women with the Mean±SD age of 35.25±15.7 years. The frequency distribution of the anaphylaxis was 188 and 103 cases in men and women respectively, with a total of 144 cases per 100000 population of the total population of men and women covered. The anaphylaxis reaction frequency in adults and children was 169 and 46 cases per 100000 population covered, respectively.
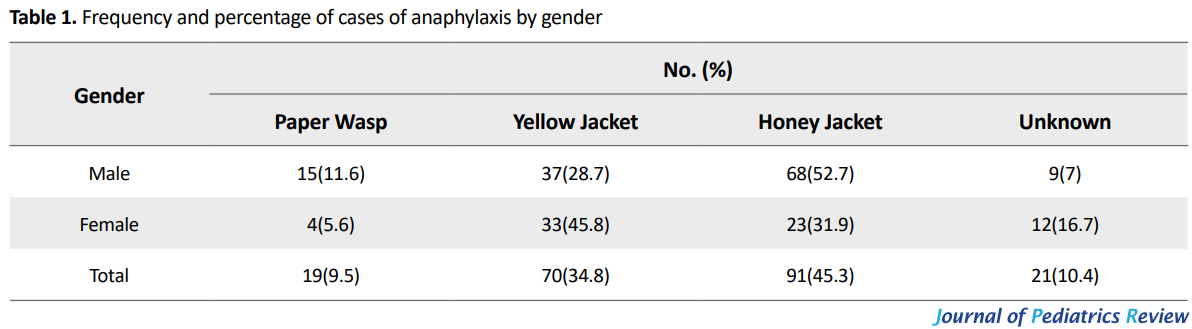
The frequency of mild, moderate, and severe anaphylaxis in this study was 43, 54, and 47 cases per 100000 population covered, respectively. The highest frequency of anaphylactic reaction was observed in the summer and after spring, with a frequency of 70 and 56 cases per 100000 population, respectively; this frequency was reported to be 15 and 1 cases per 100000 population in the autumn and winter, respectively. Of the patients whose information was included in the bee sting database, 105(52.2%) cases experienced anaphylactic shock (a very rapid attack) in <5 minutes after being stung; in 94(46.8%) cases, anaphylactic attacks occurred between 5-60 minutes after being stung (rapid attack). In this study, the frequency of anaphylactic reaction was 79(39.3%), 98(48.8%), 23(11.4%) and 1(0.5%) in the spring, summer, autumn and winter, respectively. The frequency and percentage of cases of anaphylaxis by gender and type of bee are presented in Table 1. Additionally, Figure 1 displays the error bar of various bees (Table 1).
In total, 91(45.3%), 70(34.8%), 19(9.5%) and 21(10.4%) reported bites in each gender, which occurred in respect of the bee type and anaphylaxis abundance between the two genders; the honey bee and Yellow jacket stings in males and females, respectively. This difference was statistically significant (P=0.003). The number of patients with CPR by the severity of disease and bee are listed in Table 2.
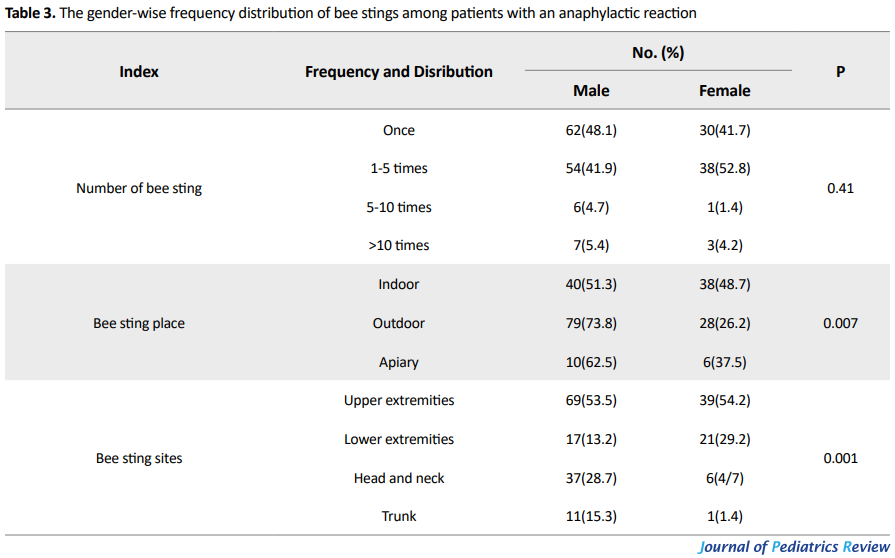
As per Table 2, anaphylaxis cases were significantly higher, despite the small number of Paper Wasp stings (a total of 7 cases of CPR, P=0.01). In the present study, the frequency of anaphylactic reaction in studied patients was significantly higher during the day as opposed to night (P=0.05). In addition, there were significant differences between the sting cases, especially in the case of male subjects and outdoors (P=0.007). The most cases of bee stings and the subsequent anaphylactic reactions were observed in the extremities (108 cases; 53.7%), followed by the head and neck (48 cases, 32.9%). Most of the bee sting cases occurred at a significantly higher rate in the mornings and evenings (92.5%) and outdoors (P=0.05) (Table 3).
According to patients’ data registered in the above database, the most frequent symptoms were itching (79%), hives (68%), and pulmonary symptoms, including cough, wheezing, and dyspnea (54%), and palpitations and hypotension (37%). The most affected systems involved in the patients with anaphylaxis were as follows: skin (85.6%), respiratory system (87.6%), cardiovascular system (35.8%), nervous system (17.4%), and digestive system (10.9%). In addition, system involvement was significantly higher in adults, compared to pediatric patients (P=0.05) (Tables 4 and 5).
In this study, a total of 7(9.5%) cases, out of 32 children with bee stings, and 67(39.64%) cases out of 169 adults with bee stings, experienced hypotension. The hypotension rate was significantly higher in adults than pediatric patients with bee stings (P=0.05). None of the children had a decreased level of consciousness in this research, but 6(3.6%) of the adults did; however, there was no significant difference between children and adults in terms of the frequency of decreased consciousness level (P=0.14). There was a significant difference between the two genders in terms of incidence of anaphylactic reactions in the affected system (P=0.01).
In this study, 78(38.8%), 107(53.2%) and 16(8%) of stings occurred indoors, outdoors, and beekeeping areas, respectively. Furthermore, there was a significant difference between the two groups in terms of the frequency severity of mild anaphylaxis in the stung organ (P=0.001). In the present study, most cases of severe bee stings have been reported in the head, neck, and upper extremities, which was statistically significant. In this study, 95% of the subjects experienced bee stings fewer than 10 times, and 80% of them had severe anaphylactic attacks after being stung more than 10 times; this difference was significant. Of all admitted cases, 58.3% were hospitalized for over 12 hours, and such difference was statistically significant (P=0.007) (Table 6).
In total, 132(65.7%) of patients with anaphylactic shock used corticosteroid and antihistamine (P=0.003). In addition, serum therapy was used for 40(19.9%) patients with anaphylaxis shock to control their condition. There was a significant relationship between the use of serum therapy and the severity of anaphylactic reaction (P=0.025). Although educating patients is necessary, no effective measures were taken to conduct subsequent follow-ups and referrals to an allergy specialist in studied patients.
4. Discussion
This cross-sectional study was conducted to determine the epidemiological status of the prevalence of anaphylaxis to bee stings in the rural areas of Gorgan City, north of Iran. The incidence of anaphylaxis was estimated equal to 1 per 700 people, which was far higher than similar studies, like the study in the United Kingdom (1 in 1333). A. Helbing also reported an annual anaphylactic reaction prevalence rate of 7.9 to 9.6 per 100000 people (6). In the present study, anaphylaxis was more prevalent in adults than children and the prevalence of anaphylaxis to bee stings was higher in both groups, than that of Bemanian et al. (ranging from 0.4 to 4% of all cases of anaphylaxis) (7). The prevalence of anaphylaxis seems to vary according to gender and age, study area, duration and anaphylaxis symptoms, geographical location, and subject selection. The obtained results revealed that the prevalence of anaphylaxis is 61.6% and 37.9% in males and females, respectively; it was more prevalent in male adults and children. Most patients were also male in the Alvarez-Twose et al. study which investigated patients with anaphylaxis to bee stings and mastocytosis (7). In another similar study, Linard et al. reported the highest cases of anaphylaxis in men, mainly in the head and neck areas (8).
In a study titled “the prevalence of anaphylaxis in Tasmania, Australia”, Blackhall et al., reported that 78.9% of adults and 21.7% of children were affected. However, contrary to our study, the prevalence of anaphylaxis in adult women was higher than that of men (9). It seems that as more men are present in open environments and carry out jobs such as farming and bee-keeping, they experience more bee stings. The higher number of anaphylaxis incidents as a result of being stung in the upper extremities, including the head and neck, can be due to the fact that these body parts were not covered; thus, were exposed to bee stings more frequently as most bees contact these areas whilst flying. The highest sting cases occurred at noon and afternoon, which can be mainly due to the fact that bees are more active during the day. Moreover, higher temperatures during the day may more irritate bees.
The findings also revealed that skin, respiratory, cardiovascular, and neuronal involvements were the most common symptoms in the patients, respectively. In line with the present study, Xie C et al. reported that the head and neck and upper extremities were the most affected areas (10). The results of this study were also consistent with Nabavi et al. study, performed by registering the diagnostic and therapeutic characteristics of patients with anaphylaxis caused by any agent during 2012-2015 in three university hospitals in Tehran, Iran. Consistent with our study, their results suggested the skin, respiratory, cardiovascular, and nervous systems as the most commonly involved organs, respectively (11). The anaphylaxis-related skin symptoms were also prevalent in the present study, which is consistent with Lieberman P study and affects up to 80% of the cases (12).
Respiratory complaints account for about half of the reactions in children and adults. Golden et al. explored patients with anaphylaxis caused by a bee sting; they concluded that skin, cardiovascular and respiratory systems were the most involved, and the nervous and digestive systems’ involvement was sometimes observed (13). A total of 19.9% of patients with anaphylactic reactions in the study mentioned above received intravenous liquids, and as the patients stated, 65.7% of them had been injected with antihistamines and corticosteroids, and epinephrine was injected only to 5% of them. Gelincik also argued that only 2.3% of patients required epinephrine for treatment, which is similar to our results (14, 15). A study conducted on Canadian physicians revealed that 76% of them were unaware of the epinephrine injection dose, and only 25% of them knew about the stages of epinephrine injection, which are similar to the present study (16).
It seems that most patients and even physicians are not aware of the importance of using epinephrine as an effective treatment; whereas if used promptly and with the correct dosage, can be a life-saving treatment. According to patients, in some cases, Zphysicians residing in the treatment centers have also refused to inject epinephrine prescribed by an allergy specialist in case of anaphylaxis. In addition, most patients were not well informed about the importance of epinephrine injections in the case of anaphylactic reactions. This can be justified by the fact that the epinephrine injection is scarce, and physicians’ concerns about epinephrine administration have pushed the patients towards a non-use strategy. These surveys reveal that medical staff have inadequate knowledge about the treatment of anaphylaxis; thus, conducting workshops and retraining sessions for physicians and other health professionals can improve their level of knowledge as well as the patients’ health.
In this study, the occurrence of anaphylaxis with honey bee and Yellow jacket was higher than other bees. There was also a significant difference between bee and gender; where women were more likely to be stung by a Yellow jacket and experience anaphylaxis. Regarding the type of bee and the severity of the occurrence of anaphylaxis in patients, the most severe cases have occurred in the studied area with a significant difference (P=0.007). Gelincik et al. surveyed the prevalence of allergy to honey bee in adults in the busy Eurasia area, with the most frequent types of bee stings.
Our study was based on a patient’s history of experiencing one bee sting (45.8%), in contrast to their study, which recorded more than 56.3% of patients having been stung more than once. However, more than 54.2% of patients reported a history of multiple bee stings and were not referred to an allergy specialist after the first systemic response for diagnostic and therapeutic purposes.
Almost half of the patients were admitted to the emergency department, which is very similar to our study. Only about one-tenth of them received adrenaline in the emergency department. None of the patients were examined, received immunotherapy, or referred to an allergy specialist. Similar to this study, the most important agent of the defendant has also been reported (16). Based on the obtained results, anaphylaxis was more severe in the Paper Wasp stings than other bees, and the incidence of CPR cases, despite the small number, was due to Paper Wasp stings, which was also significant (P=0.01).
Applying the history of previous cases of bee stings in health houses might have affected our data by the recall bias. Moreover, despite included several questions in the questionnaire regarding patients’ education requirements, subsequent follow-ups, and referrals to an allergy specialist, they were not completed adequately. Furthermore, none of the cases were referred to an allergy specialist (even if they had experienced more than one anaphylactic event).
5. Conclusion
The bee sting-induced anaphylaxis can be deadly, if not treated correctly and on time. Based on our study, case finding was successful through the rural health network. To obtain accurate epidemiological information on the prevalence of anaphylaxis due to bee stings, an anaphylaxis registry and healthcare service packages are recommended. In this integrated model, raising people awareness and the introduction of a guideline for the treatment of anaphylaxis by the community health workers is suggested. It seems that reasonable steps can be taken in promoting the health status of these patients by providing necessary medicines, like epinephrine injection and the immunotherapy vaccine for bee stings while providing insurance coverage for patients who receive immunotherapy.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed about the purpose of the research and its implementation stages; they were also assured about the confidentiality of their information; Moreover, They were allowed to leave the study whenever they wish, and if desired, the results of the research would be available to them.
Funding
This research was funded by Golestan University of Medical Sciences.
Authors contributions
All authors contributed in preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
References
- Castells MC, Hornick JL, Akin C. Anaphylaxis after hymenoptera sting: is it venom allergy, a clonal disorder, or both? The Journal of Allergy and Clinical Immunology. 2015; 3(3):350-5. [DOI:10.1016/j.jaip.2015.03.015] [PMID]
- Mullins R, Wainstein B, Barnes E, Liew W, Campbell D. Increases in anaphylaxis fatalities in Australia from 1997 to 2013. Clinical & Experimental Allergy. 2016; 46(8):1099-110. [DOI:10.1111/cea.12748] [PMID]
- Hoffman DR. Hymenoptera venoms: Composition, standardization, stability. Monograph on insect allergy. Milwaukee: American Academy of Allergy, Asthma and Immunology; 2003.
- Golden DB. Anaphylaxis to insect stings. Immunology and Allergy Clinics of North America. 2015; 35(2):287-302. [DOI:10.1016/j.iac.2015.01.007] [PMID]
- O’Hehir RE, Holgate ST, Sheikh A. Middleton’s allergy essentials. Amsterdam: Elsevier; 2015.
- Helbling A, Hurni T, Mueller U, Pichler W. Incidence of anaphylaxis with circulatory symptoms: A study over a 3‐year period comprising 940 000 inhabitants of the Swiss Canton Bern. Clinical & Experimental Allergy. 2004; 34(2):285-90. [DOI:10.1111/j.1365-2222.2004.01882.x]
- Bemanian MH, Farhoudi A, Pourpak Z, Gharagozlou M, Movahedi M, Nabavi M, et al. Systemic and local reactions of bee venom immunotherapy in Iran. Iranian Journal of Allergy, Asthma and Immunology. 2007; 6(4):203-6. [DOI:06.04/ijaai.203206] [PMID]
- Linard ATS, Barros RM, Sousa JA, Leite RS. Epidemiology of bee stings in Campina Grande, Paraíba state, Northeastern Brazil. Journal of Venomous Animals and Toxins Including Tropical Diseases. 2014; 20:13. [DOI:10.1186/1678-9199-20-13] [PMID] [PMCID]
- Blackhall M, Edwards D. Incidence and patient demographics of pre-hospital anaphylaxis in Tasmania. Australasian Journal of Paramedicine. 2015; 12(3):1-7. [DOI:10.33151/ajp.12.3.235]
- Xie C, Xu S, Ding F, Xie M, Lv J, Yao J, et al. Clinical features of severe wasp sting patients with dominantly toxic reaction: analysis of 1091 cases. PLOS One. 2013; 8(12):e83164. [DOI:10.1371/journal.pone.0083164] [PMID] [PMCID]
- Nabavi M, Lavavpour M, Arshi S, Bemanian MH, Esmaeilzadeh H, Molatefi R, et al. Characteristics, etiology and treatment of pediatric and adult anaphylaxis in Iran. Iranian Journal of Allergy, Asthma and Immunology. 2017; 16(6):480-7. [PMID]
- Schuberth KC, Lichtenstein LM, Kagey-Sobotka A, Szklo M, Kwiterovich KA, Valentine MD. An epidemiologic study of insect allergy in children. I. characteristics of the disease. The Journal of Pediatrics. 1982; 100(4):546-51. [DOI:10.1016/S0022-3476(82)80750-6]
- Yocum MW, Butterfield JH, Klein JS, Volcheck GW, Schroeder DR, Silverstein MD. Epidemiology of anaphylaxis in Olmsted County: A population-based study. Journal of Allergy and Clinical Immunology. 1999; 104(2):452-6. [DOI:10.1016/S0091-6749(99)70392-1]
- Braun CT, Mikula M, Ricklin ME, Exadaktylos AK, Helbling A. Climate data, localisation of the sting, grade of anaphylaxis and therapy of hymenoptera stings. Swiss Medical Weekly. 2016; 146(w14272):1-9. [DOI:10.4414/smw.2016.14272]
- Gelincik A, Demirtürk M, Yılmaz E, Ertek B, Erdogdu D, Çolakoğlu B, et al. Anaphylaxis in a tertiary adult allergy clinic: A retrospective review of 516 patients. Annals of Allergy, Asthma & Immunology. 2013; 110(2):96-100. [DOI:10.1016/j.anai.2012.11.018] [PMID]
- Clark S, Gaeta TJ, Kamarthi GS, Camargo CA. ICD-9-CM coding of emergency department visits for food and insect sting allergy. Annals of Epidemiology. 2006; 16(9):696-700. [DOI:10.1016/j.annepidem.2005.12.003] [PMID]
Type of Study: Original Article |
Subject:
Allergy and Clinical Immunology
Received: 2018/08/4 | Accepted: 2018/09/30 | Published: 2019/10/1
Received: 2018/08/4 | Accepted: 2018/09/30 | Published: 2019/10/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |