Volume 11, Issue 1 (1-2023)
J. Pediatr. Rev 2023, 11(1): 25-36 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rashidi Fakari F, Atarodi Kashani Z, Alizadeh S, Talebi A, Pakzad R, Abdi F. Effect of Hypnosis in Adolescents: A Narrative Review. J. Pediatr. Rev 2023; 11 (1) :25-36
URL: http://jpr.mazums.ac.ir/article-1-486-en.html
URL: http://jpr.mazums.ac.ir/article-1-486-en.html
Farzaneh Rashidi Fakari1 

 , Zahra Atarodi Kashani2
, Zahra Atarodi Kashani2 

 , Shiva Alizadeh3
, Shiva Alizadeh3 

 , Afsaneh Talebi4
, Afsaneh Talebi4 

 , Reza Pakzad5
, Reza Pakzad5 

 , Fatemeh Abdi
, Fatemeh Abdi 

 6
6


 , Zahra Atarodi Kashani2
, Zahra Atarodi Kashani2 

 , Shiva Alizadeh3
, Shiva Alizadeh3 

 , Afsaneh Talebi4
, Afsaneh Talebi4 

 , Reza Pakzad5
, Reza Pakzad5 

 , Fatemeh Abdi
, Fatemeh Abdi 

 6
6
1- Department of Midwifery, School of Medicine, North Khorasan University of Medical Sciences, Bojnurd, Iran.
2- Iranshahr University of Medical Sciences, Iranshahr, Iran.
3- Department of Midwifery, Zeynab School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Midwifery, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
5- Department of Epidemiology, Faculty of Health, Ilam University of Medical Sciences, Ilam, Iran.
6- Non-Communicable Diseases Research Center, Alborz University of Medical Sciences, Karaj, Iran. , fatemeh.abdi87@yahoo.com
2- Iranshahr University of Medical Sciences, Iranshahr, Iran.
3- Department of Midwifery, Zeynab School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Midwifery, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
5- Department of Epidemiology, Faculty of Health, Ilam University of Medical Sciences, Ilam, Iran.
6- Non-Communicable Diseases Research Center, Alborz University of Medical Sciences, Karaj, Iran. , fatemeh.abdi87@yahoo.com
Full-Text [PDF 551 kb]
(723 Downloads)
| Abstract (HTML) (1137 Views)
Full-Text: (418 Views)
Introduction
Dysmenorrhea is a cramping or pelvic pain that begins with or shortly before menstruation and persists for the first 1–7 days 1. More than half of menstruating women experience dysmenorrhea or menstrual cramps [1]. A wide variation exists in the prevalence of dysmenorrhea from studies around the world reporting a range between 28% and 71.7% [2, 3] Current evidence shows that the pathogenesis of primary dysmenorrhea may be caused by prostaglandin F2α (PGF2α), a potent myometrial stimulant of myometrial contractions). The production of these prostaglandins is closely associated with the intensity of pain experienced. The production rate of these cases continues from the proliferative phase to the luteal phase and their release increases three times during the menstrual phase [4]. If pregnancy does not occur, the corpus luteum will regress. This leads to a reduction in progesterone levels and lysosomal membrane labialization so that it breaks easily and releases the enzyme phospholipase A2 (PLA2). The phospholipase A2 (PLA2) will hydrolyze phospholipid compounds found in the endometrial cell membrane and produce arachidonic acid (AA) [5]. Arachidonic acid together with endometrial damage will stimulate the arachidonic acid cascade and produce prostaglandins prostaglandin E2 (PGE2) and PGF2 alpha. Prostaglandin E2 (PGE2) and PGF2 alpha are increased in the endometrium. They are involved in uterine smooth muscle contractions and endometrial excretion [6]. Early age at menarche is another cause of primary dysmenorrhea because the genital tract is not yet developed and the cervix is narrow and prostaglandins and blood are not quickly expelled [1].
Dysmenorrhea can be defined as a predictable pain in the lower abdomen, accompanied by symptoms, including headache, nausea, fatigue, vomiting, irritability, diarrhea, and discomfort [7, 8]. Of patients reporting pain, 12% described it as severe, 37% as moderate, and 49% as mild [9]. People who have moderate dysmenorrhea should take medication but do not require rest and stop doing the daily activities of life, and also those with severe dysmenorrhea should take medication and require rest to stop doing the daily activities of life. Therefore, in addition to negative impacts on physical health, dysmenorrhea may also affect the socioeconomic status, leading to school and work absenteeism, lower educational achievement, reduced quality of work, decreased welfare, and poor quality of life of patients with dysmenorrhea [10].
Pharmacological or non-pharmacological methods are used to treat dysmenorrhea. The conventional treatment approaches focus on the use of non-steroidal anti-inflammatory drugs (NSAIDs). NSAIDs are effective in relieving pain, but people who take them daily for long periods should have the symptoms, such as headache, dizziness, drowsiness, loss of appetite, nausea, vomiting, gastrointestinal bleeding, and asthma exacerbation and also NSAIDs can damage the whole gastrointestinal tract and patients with gastrointestinal symptoms should stop taking them which are not always available similar to herbal remedies [11, 12]. Non-pharmacological methods used to treat dysmenorrhea include exercise, heat therapy, and the use of medicinal herbs [13]. Another non-pharmacological method for pain is hypnotherapy, also referred to as hypnosis, which has attracted undue attention in recent years and is effective in the treatment of psychosomatic disorders, improving pain management and relieving anxiety [3]. A theory that defined psychological factors can affect dysmenorrhea and lower pain thresholds, caused by underlying psychosomatic conditions in some people [14, 15]. Employing the methods that can affect the interaction of these two cases can provide a good justification for the use of hypnotherapy [16]. Therefore, in situations where patients do not respond to drug therapy or suffer from side effects and are reluctant to take the drug, the alternative to the conventional NSAIDs may be welcomed and the need to use it [17].
When hypnotherapy is performed, the patient is guided to relax. This relaxation response occurs through a significant reduction in the body’s need for oxygen, and then the body’s muscles relax, leading to a feeling of calm and comfort. The blood flow will be smooth, the calming neurotransmitters will be released and the nervous system can work properly after reaching a state of relaxation, and gates of the subconscious mind will open naturally, so that it will be easier to accept the suggestions of healing given, in this case, the pain gate is called subtansia. Gelatinosa (kornudorsalis medulla spinalis) is closed and the impulses transmitted to the brain are reduced or slightly so that the perception of pain is lost or decreased [6, 18].
Hypnosis is a temporary condition of altered attention in a subject that may be induced by another person and in which various phenomena may appear spontaneously or in response to verbal or other stimuli. These phenomena include alterations in consciousness and memory, increased susceptibility to suggestion, and the production in the subject of responses and ideas unfamiliar to him in his usual state of mind. Moreover, phenomena, such as anesthesia, paralysis, and rigidity of muscles, and vasomotor changes can be produced and removed in the hypnotic state. Thus, hypnotherapy may be useful in the effective management of pain in a wide range of situations [19].
Evidence has shown that burn pain [20], labor pain [21], surgical outcome [22], cancer pain [23], and a range of chronic pain [24] can be effectively controlled by hypnotherapy. Hypnosis is an effective treatment in health care and some cases, it can save the time and money for healthcare providers [25].
Given that narrative reviews are the standard source of evidence for health care due to their exact structure, and the high prevalence of dysmenorrhea can have a negative effect on the performance and quality of life of people, as well as a growing tendency exists to use the alternative therapies; therefore, this study, which was the first narrative review, was conducted to evaluate the effect of hypnosis on dysmenorrhea in adolescent.
Methods
The guidelines of preferred reporting items for systematic reviews and meta-analyses (PRISMA) were followed while reporting the study protocol [26, 27]. By the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines, the following steps were also taken, a literature search, organization of documents for the review, the assessment of the quality of abstracts of empirical studies, synthesizing data, and writing the report.
Search strategy
The literature search was conducted in databases, including Scopus, PubMed Central, Science Direct, ProQuest, ISI Web of Knowledge, and EMBASE. The search terms were extracted from published reviews and primary studies. They were also identified through PubMed medical subject headings (MeSH). According to the PICO framework for formulating clinical questions, queries include four aspects, patient problem (P), intervention (I), comparison (C), and outcome (O). The Boolean search method was used and keywords were linked with AND, OR and the suggested entry terms were the main keywords in the search strategy.
“Dysmenorrhea”[MeSH], OR “Pain, Menstrual” [MeSH], OR “Menstrual Pain” [MeSH],OR “Menstrual Pains” [MeSH] OR “Pains, Menstrual” [MeSH], OR “Menstruation, Painful” [MeSH], OR “Menstruations, Painful” [MeSH], OR “Painful Menstruation” [MeSH], OR “Painful Menstruations” [MeSH]
“Hypnotism” [MeSH], OR “Hypnoanalysis” [MeSH], OR “Hypnotherapy” [MeSH], OR “Hypnotherapies” [MeSH], OR “Mesmerism” [MeSH].
Type of studies
Papers were obtained from randomized and quasi-experimental clinical trials. No limit exists to the study date.
Study participants
Women of reproductive age diagnosed with primary dysmenorrhea were eligible for inclusion in this review. Patients with secondary dysmenorrhea caused by endometriosis, adenomyosis, uterine fibroids, uterine malformation, chronic pelvic inflammation, and other organic pelvic pathological changes were excluded from the study, though they may have symptoms similar to the primary symptoms.
Intervention
Hypnosis was chosen as the intervention measure. Clinical hypnosis is a method of deliberately inducing a hypnosis state in a patient through verbal guidance and using its characteristic properties for targeted therapeutic purposes.
Outcomes measure
The primary outcome was menstrual pain intensity measured by visual analog scale (VAS) scores, pain self-efficacy questionnaire (PSEQ), and numerical rating scale.
Study selection
The titles and abstracts of all papers retrieved during the electronic and manual follow-up search process were assessed based on the inclusion criteria. The full texts of relevant papers were evaluated based on the aforementioned criteria.
Data extraction
After screening and assessing the quality of the selected studies, the data were extracted and recorded in pre-designed forms, including the first author’s name, year, study design, number of participants, age, type of intervention, country of the study, data collection method, assessment of pain intensity and main outcome.
Quality assessment
Table 1 lists the studies included in this review and given that they had different study designs by FA and ZA, they were assessed by two quality assessment methods (Tables 2 and 3).
.jpg)
The randomized controlled trials were assessed by “Cochrane collaboration’s tool high risk of bias”, “low risk of bias”, or “unclear risk of bias” which was assigned to each assessment item. Also, the risk of bias in the non-randomized studies of interventions (ROBINS-I) tool was used for quasi-experimental studies that have three and four domains in pre- and post-intervention [28, 29].
Results
Studies were found by searching databases. After removing duplicates, the remaining studies were screened. The screening was done in three steps. In the first step, studies were excluded after reviewing the remaining titles, and articles. After reviewing abstracts, studies were excluded from the list. Then, the full texts of the remaining studies were reviewed, and the studies were excluded. Finally, 9 studies with a total sample size of 5203 participants were included in the analysis (Table 1).
.jpg)
.jpg)
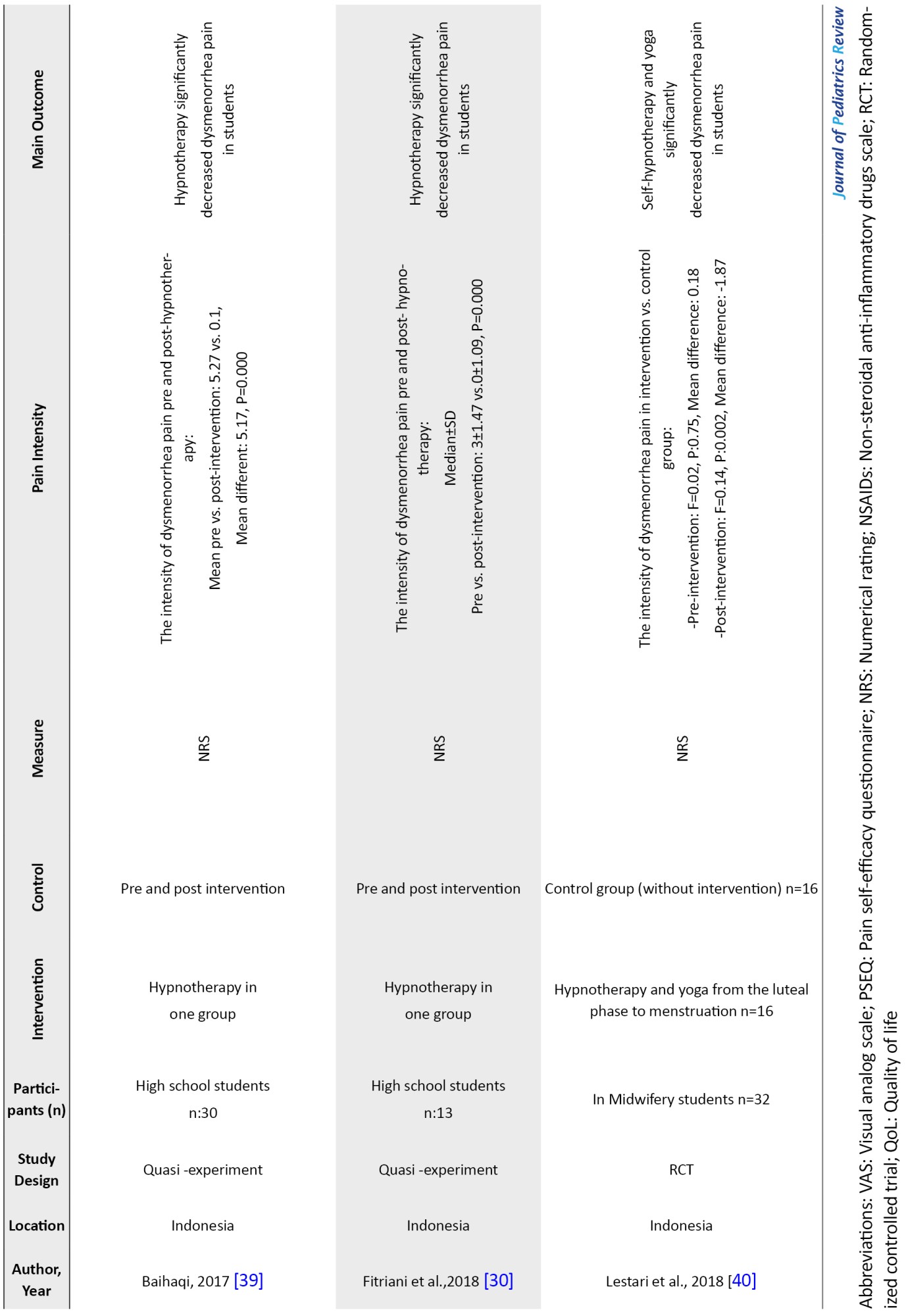
Figure 1 shows the flowchart of this selection process. Studies were published from 1943 to 2020, and 6 studies (66.6%) were conducted in Indonesia, the countries where the studies were conducted were the USA, California=1, Iran=1, and India=1.
.jpg)
Factors examined in the studies
The factors studied in Table 2 included the first author’s name, year, study location, study design, participants (sample size), intervention and control, measurement scale, result (pain intensity), main outcome, and quality score.
.jpg)
In the selected studies, the study population consisted of women of reproductive age diagnosed with primary dysmenorrhea without underlying disease and secondary dysmenorrhea. Of the 9 studies included, 2 were randomized controlled trials (RCTs) and 7 were quasi-experimental studies.
Randomized controlled trials (RCTs)
In the RCTs, the scores of functional activity restriction due to menstrual pain in women with dysmenorrhea who received hypnosis and drug therapy were significantly reduced in each treatment cycle as compared to the scores at the baseline. Additionally, no statistically significant difference was observed between drug therapy and hypnotherapy groups concerning the mean pain dysmenorrhea scores across treatment cycles (first cycle to third cycle) and non-therapeutic cycles (from 4th to 6th cycle).
The critical point in these studies was that a significant difference was observed between pain scores of dysmenorrhea and scores at the baseline in the drug therapy group during three treatment cycles but no significant difference was found in the subsequent cycles where the medication was discontinued. However, in the hypnosis groups, in addition to observing a significant difference in the treatment cycles compared to the baseline, in the subsequent three cycles when the hypnotherapy was stopped, the dysmenorrhea pain scores in these cycles were significantly reduced compared to the baseline. It should be noted that the mean dysmenorrhea pain scores in the drug therapy group in the first and second treatment cycles were significantly lower than the hypnosis group.
Quasi-experimental studies
In quasi-experimental studies, the pain scores in the hypnosis group were significantly lower than the control group, and results from cognitive-behavioral intervention (CBI) showed that hypnotherapy significantly reduced the pain scores. Also, when hypnotherapy was performed on consecutive days of a cycle, the pain scores were significantly decreased in the first days of the intervention compared to before the intervention and in the second days of the intervention compared to the first days. In addition, the pain score in each cycle was significantly reduced compared to the previous cycle.
Other quasi-experimental studies demonstrated that hypnotherapy significantly reduced pain scores in teenage girls before and after the intervention. Table 2 presents other results in detail.
Discussion
The present study aimed to investigate the effect of hypnosis on dysmenorrhea. The results from a review of 7 clinical trial studies showed the effectiveness of applying the hypnosis method on primary dysmenorrhea. The use of hypnotherapy significantly reduced the severity of dysmenorrhea in the intervention group compared to the drug therapy group and also quasi-experimental studies demonstrated that the severity of dysmenorrhea significantly reduced during the intervention compared to before the intervention.
Hypnotherapy is a non-pharmacological intervention that can be performed to decrease the pain experienced by adolescents with dysmenorrhea, this action is currently applied by many people to overcome both psychological and physical [6].
Hypnosis can reduce the pain intensity of primary dysmenorrhea through two mechanisms, namely hypnotic induction, and deepening procedures. The first mechanism aims to reduce the pain intensity of dysmenorrhea. An induction and deepening process occurs, typically involving relaxation procedures designed to bring the body into a state of deep relaxation, and bring the brain to the theta wave state [30]. These conditions stimulate the body’s relaxation through the HPA axis to produce the corticotrophin-releasing factor (CRF). In addition, corticotrophin-releasing factor (CRF) stimulates the pituitary gland to reduce the production of adrenocorticotropic hormone (ACTH), increase the production of endorphins, and reduce the production of cortisol and other stress hormones to reduce pain. Endorphins act to suppress pain impulses in the spinal cord. By keeping pain impulses in the spinal cord, pain impulses are not transmitted to the thalamus, and thus no pain impulses are transmitted to the cerebral cortex [6, 30].
The second mechanism aims to relieve pain from hypnosis received by the subconscious, which can change the cerebral cortex’s pain perception. This hypnotic procedure is an attempt to present new data and enter the subconscious mind in the limbic system. In the conscious state, the subconscious mind can affect the cerebral cortex, that is, it presents data based on suggestions. When the cerebral cortex contracts the impulses, they are perceived as happiness and gratitude. The hypnotic induction and deepening procedures revealed that hypnotherapy can reduce the pain intensity of dysmenorrhea and these reductions remain forever [6, 30].
Hypnotherapy can reduce pain intensity and duration by enhancing theta waves and better acceptance of impulses and increasing the effect of hypnosis and the release of endorphins. Hypnosis affects the anterior cortex involved in accepting negative emotional responses and inhibits pain by suppressing the neural activity between the sensory cortex and the limbic system of the amygdala [31].
Gay et al. also found that, unlike other behavioral techniques s of pain treatment, hypnosis can provide rapid pain relief that can be maintained for long periods [32]. Hypnosis is an effective tool to access the mind-body connection that a person can affect neurotransmitter release and relieve pain using a set of regulations. Hypnosis can effectively relieve pain and reduce the need for analgesia in various medical conditions [33, 34]. Additionally, hypnosis can have a lasting effect on pain relief in cases of primary dysmenorrhea [28].
Farshbaf et al. in a study found that hypnotherapy is more effective than cognitive behavioral therapy [19]. Hypnotherapy is also effective in increasing pain self-efficacy [35]. The effectiveness of hypnosis for pain relief may be due to the instincts given to the patient. In many cases, dysmenorrhea is associated with conditioned pain in the cerebral cortex.
By identifying severe menstrual cramps, instincts in hypnotic sleep hypnosis, and training in self-hypnosis, a hypnotherapist can guide a person to achieve deep relaxation by relieving the stress and anxiety caused by illness and has a regular menstrual cycle [33].
The results indicate that hypnotherapy can significantly improve the quality of life as compared to NSAIDs [28]. Hypnosis can reduce the distress and anxiety related to dysmenorrhea [36]. It also helps people develop coping strategies and achieve some healthy lifestyle changes [37] and thus can improve their quality of life.
In the studies included, no possible side effects due to applying hypnotherapy were observed. One of the limitations of this study is the lack of access to all published studies and reports due to the limited search for studies in non-English languages.
Conclusion
Hypnosis can be effective in reducing the severity and duration of pain in women with primary dysmenorrhea. Compared to drug therapy, hypnotherapy could reduce dysmenorrhea even after discontinuation of intervention for several menstrual cycles and without the need for any treatment. The use of hypnotherapy can improve individuals’ quality of life. Therefore, to reduce the side effects of NSAIDs in the treatment of dysmenorrhea, it is recommended to use the most effective non-pharmacological method, such as hypnosis by providing education to women and girls.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The authors declared no conflict of interest regarding the publication of this study.
Acknowledgements
We sincerely express our gratitude to the staff of Alborz University of Medical Sciences and the Research Deputy of the University for their support. We are also more grateful to the women who participated in this study.
References
Dysmenorrhea is a cramping or pelvic pain that begins with or shortly before menstruation and persists for the first 1–7 days 1. More than half of menstruating women experience dysmenorrhea or menstrual cramps [1]. A wide variation exists in the prevalence of dysmenorrhea from studies around the world reporting a range between 28% and 71.7% [2, 3] Current evidence shows that the pathogenesis of primary dysmenorrhea may be caused by prostaglandin F2α (PGF2α), a potent myometrial stimulant of myometrial contractions). The production of these prostaglandins is closely associated with the intensity of pain experienced. The production rate of these cases continues from the proliferative phase to the luteal phase and their release increases three times during the menstrual phase [4]. If pregnancy does not occur, the corpus luteum will regress. This leads to a reduction in progesterone levels and lysosomal membrane labialization so that it breaks easily and releases the enzyme phospholipase A2 (PLA2). The phospholipase A2 (PLA2) will hydrolyze phospholipid compounds found in the endometrial cell membrane and produce arachidonic acid (AA) [5]. Arachidonic acid together with endometrial damage will stimulate the arachidonic acid cascade and produce prostaglandins prostaglandin E2 (PGE2) and PGF2 alpha. Prostaglandin E2 (PGE2) and PGF2 alpha are increased in the endometrium. They are involved in uterine smooth muscle contractions and endometrial excretion [6]. Early age at menarche is another cause of primary dysmenorrhea because the genital tract is not yet developed and the cervix is narrow and prostaglandins and blood are not quickly expelled [1].
Dysmenorrhea can be defined as a predictable pain in the lower abdomen, accompanied by symptoms, including headache, nausea, fatigue, vomiting, irritability, diarrhea, and discomfort [7, 8]. Of patients reporting pain, 12% described it as severe, 37% as moderate, and 49% as mild [9]. People who have moderate dysmenorrhea should take medication but do not require rest and stop doing the daily activities of life, and also those with severe dysmenorrhea should take medication and require rest to stop doing the daily activities of life. Therefore, in addition to negative impacts on physical health, dysmenorrhea may also affect the socioeconomic status, leading to school and work absenteeism, lower educational achievement, reduced quality of work, decreased welfare, and poor quality of life of patients with dysmenorrhea [10].
Pharmacological or non-pharmacological methods are used to treat dysmenorrhea. The conventional treatment approaches focus on the use of non-steroidal anti-inflammatory drugs (NSAIDs). NSAIDs are effective in relieving pain, but people who take them daily for long periods should have the symptoms, such as headache, dizziness, drowsiness, loss of appetite, nausea, vomiting, gastrointestinal bleeding, and asthma exacerbation and also NSAIDs can damage the whole gastrointestinal tract and patients with gastrointestinal symptoms should stop taking them which are not always available similar to herbal remedies [11, 12]. Non-pharmacological methods used to treat dysmenorrhea include exercise, heat therapy, and the use of medicinal herbs [13]. Another non-pharmacological method for pain is hypnotherapy, also referred to as hypnosis, which has attracted undue attention in recent years and is effective in the treatment of psychosomatic disorders, improving pain management and relieving anxiety [3]. A theory that defined psychological factors can affect dysmenorrhea and lower pain thresholds, caused by underlying psychosomatic conditions in some people [14, 15]. Employing the methods that can affect the interaction of these two cases can provide a good justification for the use of hypnotherapy [16]. Therefore, in situations where patients do not respond to drug therapy or suffer from side effects and are reluctant to take the drug, the alternative to the conventional NSAIDs may be welcomed and the need to use it [17].
When hypnotherapy is performed, the patient is guided to relax. This relaxation response occurs through a significant reduction in the body’s need for oxygen, and then the body’s muscles relax, leading to a feeling of calm and comfort. The blood flow will be smooth, the calming neurotransmitters will be released and the nervous system can work properly after reaching a state of relaxation, and gates of the subconscious mind will open naturally, so that it will be easier to accept the suggestions of healing given, in this case, the pain gate is called subtansia. Gelatinosa (kornudorsalis medulla spinalis) is closed and the impulses transmitted to the brain are reduced or slightly so that the perception of pain is lost or decreased [6, 18].
Hypnosis is a temporary condition of altered attention in a subject that may be induced by another person and in which various phenomena may appear spontaneously or in response to verbal or other stimuli. These phenomena include alterations in consciousness and memory, increased susceptibility to suggestion, and the production in the subject of responses and ideas unfamiliar to him in his usual state of mind. Moreover, phenomena, such as anesthesia, paralysis, and rigidity of muscles, and vasomotor changes can be produced and removed in the hypnotic state. Thus, hypnotherapy may be useful in the effective management of pain in a wide range of situations [19].
Evidence has shown that burn pain [20], labor pain [21], surgical outcome [22], cancer pain [23], and a range of chronic pain [24] can be effectively controlled by hypnotherapy. Hypnosis is an effective treatment in health care and some cases, it can save the time and money for healthcare providers [25].
Given that narrative reviews are the standard source of evidence for health care due to their exact structure, and the high prevalence of dysmenorrhea can have a negative effect on the performance and quality of life of people, as well as a growing tendency exists to use the alternative therapies; therefore, this study, which was the first narrative review, was conducted to evaluate the effect of hypnosis on dysmenorrhea in adolescent.
Methods
The guidelines of preferred reporting items for systematic reviews and meta-analyses (PRISMA) were followed while reporting the study protocol [26, 27]. By the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines, the following steps were also taken, a literature search, organization of documents for the review, the assessment of the quality of abstracts of empirical studies, synthesizing data, and writing the report.
Search strategy
The literature search was conducted in databases, including Scopus, PubMed Central, Science Direct, ProQuest, ISI Web of Knowledge, and EMBASE. The search terms were extracted from published reviews and primary studies. They were also identified through PubMed medical subject headings (MeSH). According to the PICO framework for formulating clinical questions, queries include four aspects, patient problem (P), intervention (I), comparison (C), and outcome (O). The Boolean search method was used and keywords were linked with AND, OR and the suggested entry terms were the main keywords in the search strategy.
“Dysmenorrhea”[MeSH], OR “Pain, Menstrual” [MeSH], OR “Menstrual Pain” [MeSH],OR “Menstrual Pains” [MeSH] OR “Pains, Menstrual” [MeSH], OR “Menstruation, Painful” [MeSH], OR “Menstruations, Painful” [MeSH], OR “Painful Menstruation” [MeSH], OR “Painful Menstruations” [MeSH]
“Hypnotism” [MeSH], OR “Hypnoanalysis” [MeSH], OR “Hypnotherapy” [MeSH], OR “Hypnotherapies” [MeSH], OR “Mesmerism” [MeSH].
Type of studies
Papers were obtained from randomized and quasi-experimental clinical trials. No limit exists to the study date.
Study participants
Women of reproductive age diagnosed with primary dysmenorrhea were eligible for inclusion in this review. Patients with secondary dysmenorrhea caused by endometriosis, adenomyosis, uterine fibroids, uterine malformation, chronic pelvic inflammation, and other organic pelvic pathological changes were excluded from the study, though they may have symptoms similar to the primary symptoms.
Intervention
Hypnosis was chosen as the intervention measure. Clinical hypnosis is a method of deliberately inducing a hypnosis state in a patient through verbal guidance and using its characteristic properties for targeted therapeutic purposes.
Outcomes measure
The primary outcome was menstrual pain intensity measured by visual analog scale (VAS) scores, pain self-efficacy questionnaire (PSEQ), and numerical rating scale.
Study selection
The titles and abstracts of all papers retrieved during the electronic and manual follow-up search process were assessed based on the inclusion criteria. The full texts of relevant papers were evaluated based on the aforementioned criteria.
Data extraction
After screening and assessing the quality of the selected studies, the data were extracted and recorded in pre-designed forms, including the first author’s name, year, study design, number of participants, age, type of intervention, country of the study, data collection method, assessment of pain intensity and main outcome.
Quality assessment
Table 1 lists the studies included in this review and given that they had different study designs by FA and ZA, they were assessed by two quality assessment methods (Tables 2 and 3).
.jpg)
The randomized controlled trials were assessed by “Cochrane collaboration’s tool high risk of bias”, “low risk of bias”, or “unclear risk of bias” which was assigned to each assessment item. Also, the risk of bias in the non-randomized studies of interventions (ROBINS-I) tool was used for quasi-experimental studies that have three and four domains in pre- and post-intervention [28, 29].
Results
Studies were found by searching databases. After removing duplicates, the remaining studies were screened. The screening was done in three steps. In the first step, studies were excluded after reviewing the remaining titles, and articles. After reviewing abstracts, studies were excluded from the list. Then, the full texts of the remaining studies were reviewed, and the studies were excluded. Finally, 9 studies with a total sample size of 5203 participants were included in the analysis (Table 1).
.jpg)
.jpg)
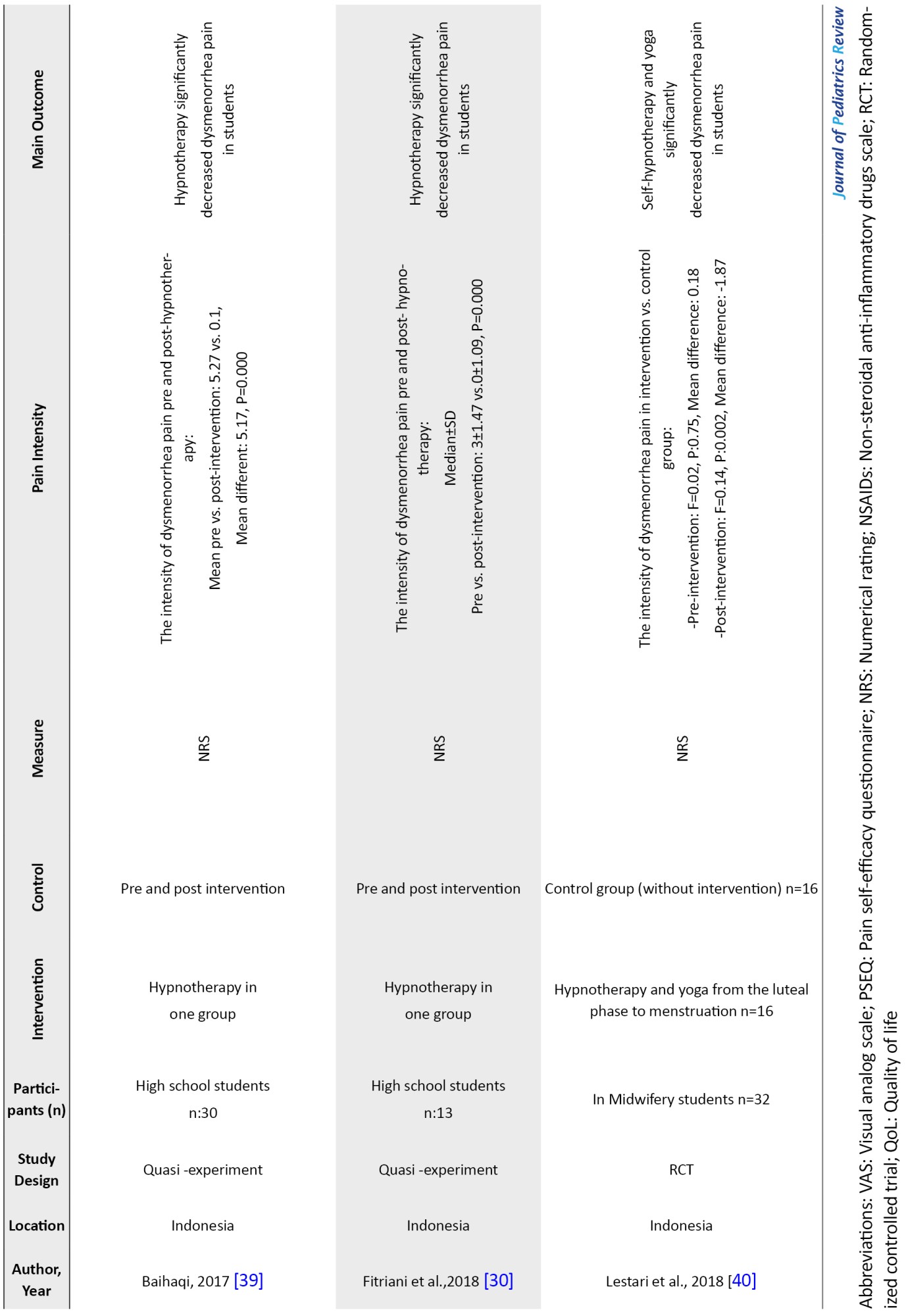
Figure 1 shows the flowchart of this selection process. Studies were published from 1943 to 2020, and 6 studies (66.6%) were conducted in Indonesia, the countries where the studies were conducted were the USA, California=1, Iran=1, and India=1.
.jpg)
Factors examined in the studies
The factors studied in Table 2 included the first author’s name, year, study location, study design, participants (sample size), intervention and control, measurement scale, result (pain intensity), main outcome, and quality score.
.jpg)
In the selected studies, the study population consisted of women of reproductive age diagnosed with primary dysmenorrhea without underlying disease and secondary dysmenorrhea. Of the 9 studies included, 2 were randomized controlled trials (RCTs) and 7 were quasi-experimental studies.
Randomized controlled trials (RCTs)
In the RCTs, the scores of functional activity restriction due to menstrual pain in women with dysmenorrhea who received hypnosis and drug therapy were significantly reduced in each treatment cycle as compared to the scores at the baseline. Additionally, no statistically significant difference was observed between drug therapy and hypnotherapy groups concerning the mean pain dysmenorrhea scores across treatment cycles (first cycle to third cycle) and non-therapeutic cycles (from 4th to 6th cycle).
The critical point in these studies was that a significant difference was observed between pain scores of dysmenorrhea and scores at the baseline in the drug therapy group during three treatment cycles but no significant difference was found in the subsequent cycles where the medication was discontinued. However, in the hypnosis groups, in addition to observing a significant difference in the treatment cycles compared to the baseline, in the subsequent three cycles when the hypnotherapy was stopped, the dysmenorrhea pain scores in these cycles were significantly reduced compared to the baseline. It should be noted that the mean dysmenorrhea pain scores in the drug therapy group in the first and second treatment cycles were significantly lower than the hypnosis group.
Quasi-experimental studies
In quasi-experimental studies, the pain scores in the hypnosis group were significantly lower than the control group, and results from cognitive-behavioral intervention (CBI) showed that hypnotherapy significantly reduced the pain scores. Also, when hypnotherapy was performed on consecutive days of a cycle, the pain scores were significantly decreased in the first days of the intervention compared to before the intervention and in the second days of the intervention compared to the first days. In addition, the pain score in each cycle was significantly reduced compared to the previous cycle.
Other quasi-experimental studies demonstrated that hypnotherapy significantly reduced pain scores in teenage girls before and after the intervention. Table 2 presents other results in detail.
Discussion
The present study aimed to investigate the effect of hypnosis on dysmenorrhea. The results from a review of 7 clinical trial studies showed the effectiveness of applying the hypnosis method on primary dysmenorrhea. The use of hypnotherapy significantly reduced the severity of dysmenorrhea in the intervention group compared to the drug therapy group and also quasi-experimental studies demonstrated that the severity of dysmenorrhea significantly reduced during the intervention compared to before the intervention.
Hypnotherapy is a non-pharmacological intervention that can be performed to decrease the pain experienced by adolescents with dysmenorrhea, this action is currently applied by many people to overcome both psychological and physical [6].
Hypnosis can reduce the pain intensity of primary dysmenorrhea through two mechanisms, namely hypnotic induction, and deepening procedures. The first mechanism aims to reduce the pain intensity of dysmenorrhea. An induction and deepening process occurs, typically involving relaxation procedures designed to bring the body into a state of deep relaxation, and bring the brain to the theta wave state [30]. These conditions stimulate the body’s relaxation through the HPA axis to produce the corticotrophin-releasing factor (CRF). In addition, corticotrophin-releasing factor (CRF) stimulates the pituitary gland to reduce the production of adrenocorticotropic hormone (ACTH), increase the production of endorphins, and reduce the production of cortisol and other stress hormones to reduce pain. Endorphins act to suppress pain impulses in the spinal cord. By keeping pain impulses in the spinal cord, pain impulses are not transmitted to the thalamus, and thus no pain impulses are transmitted to the cerebral cortex [6, 30].
The second mechanism aims to relieve pain from hypnosis received by the subconscious, which can change the cerebral cortex’s pain perception. This hypnotic procedure is an attempt to present new data and enter the subconscious mind in the limbic system. In the conscious state, the subconscious mind can affect the cerebral cortex, that is, it presents data based on suggestions. When the cerebral cortex contracts the impulses, they are perceived as happiness and gratitude. The hypnotic induction and deepening procedures revealed that hypnotherapy can reduce the pain intensity of dysmenorrhea and these reductions remain forever [6, 30].
Hypnotherapy can reduce pain intensity and duration by enhancing theta waves and better acceptance of impulses and increasing the effect of hypnosis and the release of endorphins. Hypnosis affects the anterior cortex involved in accepting negative emotional responses and inhibits pain by suppressing the neural activity between the sensory cortex and the limbic system of the amygdala [31].
Gay et al. also found that, unlike other behavioral techniques s of pain treatment, hypnosis can provide rapid pain relief that can be maintained for long periods [32]. Hypnosis is an effective tool to access the mind-body connection that a person can affect neurotransmitter release and relieve pain using a set of regulations. Hypnosis can effectively relieve pain and reduce the need for analgesia in various medical conditions [33, 34]. Additionally, hypnosis can have a lasting effect on pain relief in cases of primary dysmenorrhea [28].
Farshbaf et al. in a study found that hypnotherapy is more effective than cognitive behavioral therapy [19]. Hypnotherapy is also effective in increasing pain self-efficacy [35]. The effectiveness of hypnosis for pain relief may be due to the instincts given to the patient. In many cases, dysmenorrhea is associated with conditioned pain in the cerebral cortex.
By identifying severe menstrual cramps, instincts in hypnotic sleep hypnosis, and training in self-hypnosis, a hypnotherapist can guide a person to achieve deep relaxation by relieving the stress and anxiety caused by illness and has a regular menstrual cycle [33].
The results indicate that hypnotherapy can significantly improve the quality of life as compared to NSAIDs [28]. Hypnosis can reduce the distress and anxiety related to dysmenorrhea [36]. It also helps people develop coping strategies and achieve some healthy lifestyle changes [37] and thus can improve their quality of life.
In the studies included, no possible side effects due to applying hypnotherapy were observed. One of the limitations of this study is the lack of access to all published studies and reports due to the limited search for studies in non-English languages.
Conclusion
Hypnosis can be effective in reducing the severity and duration of pain in women with primary dysmenorrhea. Compared to drug therapy, hypnotherapy could reduce dysmenorrhea even after discontinuation of intervention for several menstrual cycles and without the need for any treatment. The use of hypnotherapy can improve individuals’ quality of life. Therefore, to reduce the side effects of NSAIDs in the treatment of dysmenorrhea, it is recommended to use the most effective non-pharmacological method, such as hypnosis by providing education to women and girls.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The authors declared no conflict of interest regarding the publication of this study.
Acknowledgements
We sincerely express our gratitude to the staff of Alborz University of Medical Sciences and the Research Deputy of the University for their support. We are also more grateful to the women who participated in this study.
References
- Abdi F, Amjadi MA, Zaheri F, Rahnemaei FA. Role of vitamin D and calcium in the relief of primary dysmenorrhea: A systematic review. Obstet Gynecol Sci. 2021; 64(1):13-26. [DOI:10.5468/ogs.20205] [PMID] [PMCID]
- Shahrahmani H, Ghazanfarpour M, Shahrahmani N, Abdi F, Sewell RD, Rafieian-Kopaei M. Effect of fennel on primary dysmenorrhea: A systematic review and meta-analysis. J Complement Integr Med. 2021; 18(2):261-9. [DOI:10.1515/jcim-2019-0212] [PMID]
- Pitts MK, Ferris JA, Smith AM, Shelley JM, Richters J. Prevalence and correlates of three types of pelvic pain in a nationally representative sample of Australian women. Med J Aust. 2008; 189(3):138-43. [DOI:10.5694/j.1326-5377.2008.tb01945.x] [PMID]
- Aprilyadi N, Feri HJ, Ridawati ID. [The effectiveness of hypnotherapy on reducing dysmenorrhea pain in high school students (Indonesian)]. J Perawat Indonesia. 2018; 2(1):10-9. [DOI:10.32584/jpi.v2i1.39]
- Avasarala AK, Panchangam S. Dysmenorrhoea in different settings: Are the rural and urban adolescent girls perceiving and managing the dysmenorrhoea problem differently? Indian J Community Med. 2008; 33(4):246-9. [DOI:10.4103/0970-0218.43231] [PMID]
- Amelia S, Dewi R, Febrina W. The effect of hypnotherapy to reduce dysmenorrhea pain. Padjadjaran Acute Care Nurs J. 2020; 2(1). [Link]
- Hailemeskel S, Demissie A, Assefa N. Primary dysmenorrhea magnitude, associated risk factors, and its effect on academic performance: Evidence from female university students in Ethiopia. Int J Womens Health. 2016; 8:489. [DOI:10.2147/IJWH.S112768] [PMID]
- Midilli TS, Yasar E, Baysal E. Dysmenorrhea characteristics of female students of health school and affecting factors and their knowledge and use of complementary and alternative medicine methods. Holist Nurs Pract. 2015; 29(4):194-204. [DOI:10.1097/HNP.0000000000000091] [PMID]
- Insani WN. The effects of self hypnosis technique towards the decreasing of menstruation pain level to girls teenager at smkn 2 sumedang of sumedang regency in 2019. J Ilmiah Bidan. 2020; 5(1):22-8. [Link]
- Alp Yılmaz F, Dilek A. Effect of dysmenorrhea on quality of life in university students: A case-control study. Cukurova Med J. 2020; 45(2):648-55. [DOI:10.17826/cumj.659813]
- Rigi SN, Navidian A, Safabakhsh L, Safarzadeh A, Khazaian S, Shafie S, et al. Comparing the analgesic effect of heat patch containing iron chip and ibuprofen for primary dysmenorrhea: A randomized controlled trial. BMC Women’s Health. 2012; 12(1):25. [DOI:10.1186/1472-6874-12-25] [PMID]
- Sharghi M, Mansurkhani SM, Larky DA, Kooti W, Niksefat M, Firoozbakht M, et al. An update and systematic review on the treatment of primary dysmenorrhea. JBRA assisted reproduction. 2019; 23(1):51. [DOI:10.5935/1518-0557.20180083] [PMID]
- Gharloghi S, Torkzahrani S, Akbarzadeh AR, Heshmat R. The effects of acupressure on severity of primary dysmenorrhea. Patient Prefer Adherence. 2012; 6:137-42. [DOI:10.2147/PPA.S27127] [PMID] [PMCID]
- Maryam M, Ritonga MA, Istriati I. Relationship between menstrual profile and psychological stress with dysmenorrhea. Althea Med J. 2016; 3(3):382-7. [DOI:10.15850/amj.v3n3.884]
- Kroger W, Freed S. The psychosomatic treatment of functional dysmenorrhea by hypnosis: A preliminary report. Am J Obstetrics Gynecol. 1943; 46(6):817-22. [DOI:10.1016/S0002-9378(43)90360-6]
- Lefebvre G, Pinsonneault O, Antao V, Black A, Burnett M, Feldman K, et al. Primary dysmenorrhea consensus guideline. J Obstet Gynaecol Can. 2005; 27(12):1117-46. [DOI:10.1016/S1701-2163(16)30395-4] [PMID]
- Shah M, Monga A, Patel SV, Shah M, Bakshi H. Pain relief in dysmenorrhea: Exploring hypnosis as an alternative therapy. CHRISMED J Health Res. 2016; 3(3):197-202. [DOI:10.4103/2348-3334.183741]
- Elkins G, Jensen MP, Patterson DR. Hypnotherapy for the management of chronic pain. Int J Clin Exp Hypn. 2007; 55(3):275-87. [DOI:10.1080/00207140701338621] [PMID] [PMCID]
- Farshbaf Manei Sefat F, Abolghasemi A, Barahmand U, Hajloo N. [Comparing the effectiveness of cognitive behavioral therapy and hypnosis therapy pain self-efficacy and pain severity in girls with primary dysmenorrhea (Persian)]. Armaghane Danesh. 2017; 22(1):87-103. [Link]
- Jafarizadeh H, Lotfi M, Ajoudani F, Kiani A, Alinejad V. Hypnosis for reduction of background pain and pain anxiety in men with burns: A blinded, randomised, placebo-controlled study. Burns. 2018; 44(1):108-17. [DOI:10.1016/j.burns.2017.06.001] [PMID]
- Beevi Z, Low WY, Hassan J. The effectiveness of hypnosis intervention for labor: An experimental study. Am J Clin Hypn. 2017; 60(2):172-91. [DOI:10.1080/00029157.2017.1280659] [PMID]
- Tefikow S, Barth J, Maichrowitz S, Beelmann A, Strauss B, Rosendahl J. Efficacy of hypnosis in adults undergoing surgery or medical procedures: A meta-analysis of randomized controlled trials. Clin Psychol Rev. 2013; 33(5):623-36. [DOI:10.1016/j.cpr.2013.03.005] [PMID]
- Wortzel J, Spiegel D. Hypnosis in cancer care. American J Clin Hypn. 2017; 60(1):4-17. [DOI:10.1080/00029157.2017.1290577]
- Jensen MP, Patterson DR. Hypnotic approaches for chronic pain management: Clinical implications of recent research findings. Am Psychol. 2014; 69(2):167-77. [DOI:10.1037/a0035644] [PMID]
- Lynn SJ, Laurence J-R, Kirsch I. Hypnosis, suggestion, and suggestibility: An integrative model. American Journal of Clinical Hypnosis. 2015; 57(3):314-29. [DOI:10.1080/00029157.2014.976783] [PMID]
- Abdi F, Roozbeh N. [The effects of humulus lupulus l. (hops) on menopausal vasomotor symptoms: A systematic review and meta-analysis (Persian)]. Iran J Obstet Gynecol Infertil. 2016; 19(26):9-17. [DOI:10.22038/ijogi.2016.7797]
- Abdi F, Kazemi F, Tehrani FR, Roozbeh N. Protocol for systematic review and meta-analysis: Hop (humulus lupulus l.) for menopausal vasomotor symptoms. BMJ Open. 2016; 6(4):e010734. [DOI:10.1136/bmjopen-2015-010734] [PMID] [PMCID]
- Shaterian N, Pakzad R, Fekri SD, Abdi F, Shaterian N. Labor pain in different dilatations of the cervix and apgar scores affected by aromatherapy: A systematic review and meta-analysis. Reprod Sci. 2021:1-17. [DOI:10.1007/s43032-021-00666-4] [PMID]
- Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019; 366:l4898. [DOI:10.1136/bmj.l4898] [PMID]
- Fitriani H, Achmad A. The effect of hypnotherapy on primary dismenore in adolescents. J Mat Care Reprod Health. 2018; 1(2):285-91. [DOI:10.36780/jmcrh.v1i2.34]
- Arab R-K, Khani S, Khademloo M, Atarod Z, Nazari Z. [Effect of Hypnosis on pregnancy and delivery outcomes: A systematic review (Persian)]. J Mazandaran Unive Med Sci. 2021; 30(194):156-70. [Link]
- Gay M-C, Philippot P, Luminet O. Differential effectiveness of psychological interventions for reducing osteoarthritis pain: A comparison of Erickson hypnosis and Jacobson relaxation. Eur J Pain. 2002; 6(1):1-16. [DOI:10.1053/eujp.2001.0263] [PMID]
- Abrahamsen R, Baad-Hansen L, Zachariae R, Svensson P. Effect of hypnosis on pain and blink reflexes in patients with painful temporomandibular disorders. Clin J Pain. 2011; 27(4):344-51. [DOI:10.1097/AJP.0b013e3181ffbfcb] [PMID]
- Meissner K, Böhling B, Schweizer-Arau A. Long-term effects of traditional chinese medicine and hypnotherapy in patients with severe endometriosis-a retrospective evaluation. Complementary Medicine Research. 2010; 17(6):314-20. [DOI:10.1159/000322890] [PMID]
- Montgomery GH, David D, Winkel G, Silverstein JH, Bovbjerg DH. The effectiveness of adjunctive hypnosis with surgical patients: A meta-analysis. Anesth Analg. 2002; 94(6):1639-45. [DOI:10.1097/00000539-200206000-00052] [PMID]
- Adeyemi A, Adekanle D. Management of dysmenorrrhoea among medical students. Internet J Gynecol Obstet. 2006; 7:1. [Link]
- Unsal A, Ayranci U, Tozun M, Arslan G, Calik E. Prevalence of dysmenorrhea and its effect on quality of life among a group of female university students. Ups J Med Sci. 2010; 115(2):138-45. [DOI:10.3109/03009730903457218] [PMID] [PMCID]
- Shah M, Monga A, Patel S, Shah M, Bakshi H. The effect of hypnosis on dysmenorrhea. Int J Clin Exp Hypn. 2014; 62(2):164-78. [DOI:10.1080/00207144.2014.869128] [PMID]
- Baihaqi Ry. (Pengaruh hipnoterapi terhadap penurunan dismenorea primer pada siswi sma 1 Muhammadiyah Malang (Indonasian). [Bachelor thesis] Jawa Timur: University of Muhammadiyah Malang; 2017. [Link]
- Lestari P, Putri RA. Kombinasi self hypnosis dan senam yoga terhadap tingkat nyeri dan kecemasan saat menstruasi. Indones J Midwifery. 2018; 1(2). [DOI:10.35473/ijm.v1i2.105]
Type of Study: Systematic Review |
Subject:
Pediatric Nephrology
Received: 2022/07/14 | Accepted: 2022/11/7 | Published: 2023/01/1
Received: 2022/07/14 | Accepted: 2022/11/7 | Published: 2023/01/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |