Volume 12, Issue 1 (1-2024)
J. Pediatr. Rev 2024, 12(1): 1-4 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Naderisorki M, Rezapour M, Naderi Soorki M. Investigating the Application of Artificial Intelligence in the Pediatric Oncology. J. Pediatr. Rev 2024; 12 (1) :1-4
URL: http://jpr.mazums.ac.ir/article-1-546-en.html
URL: http://jpr.mazums.ac.ir/article-1-546-en.html
1- Thalassemia Research Center, Hemoglobinopathy Institute, Mazandaran University of Medical Sciences, Sari, Iran. , dr.naderisorki@gmail.com
2- Psychiatry and Behavioral Sciences Research Center, Addiction Institute, Mazandaran University of Medical Sciences, Sari, Iran.
3- Research Laboratory of Intelligent Wireless Networks, Faculty of Engineering, Shahid Chamran University of Ahvaz, Ahvaz, Iran.
2- Psychiatry and Behavioral Sciences Research Center, Addiction Institute, Mazandaran University of Medical Sciences, Sari, Iran.
3- Research Laboratory of Intelligent Wireless Networks, Faculty of Engineering, Shahid Chamran University of Ahvaz, Ahvaz, Iran.
Full-Text [PDF 566 kb]
(1035 Downloads)
| Abstract (HTML) (2925 Views)
Full-Text: (720 Views)
Dear Editor
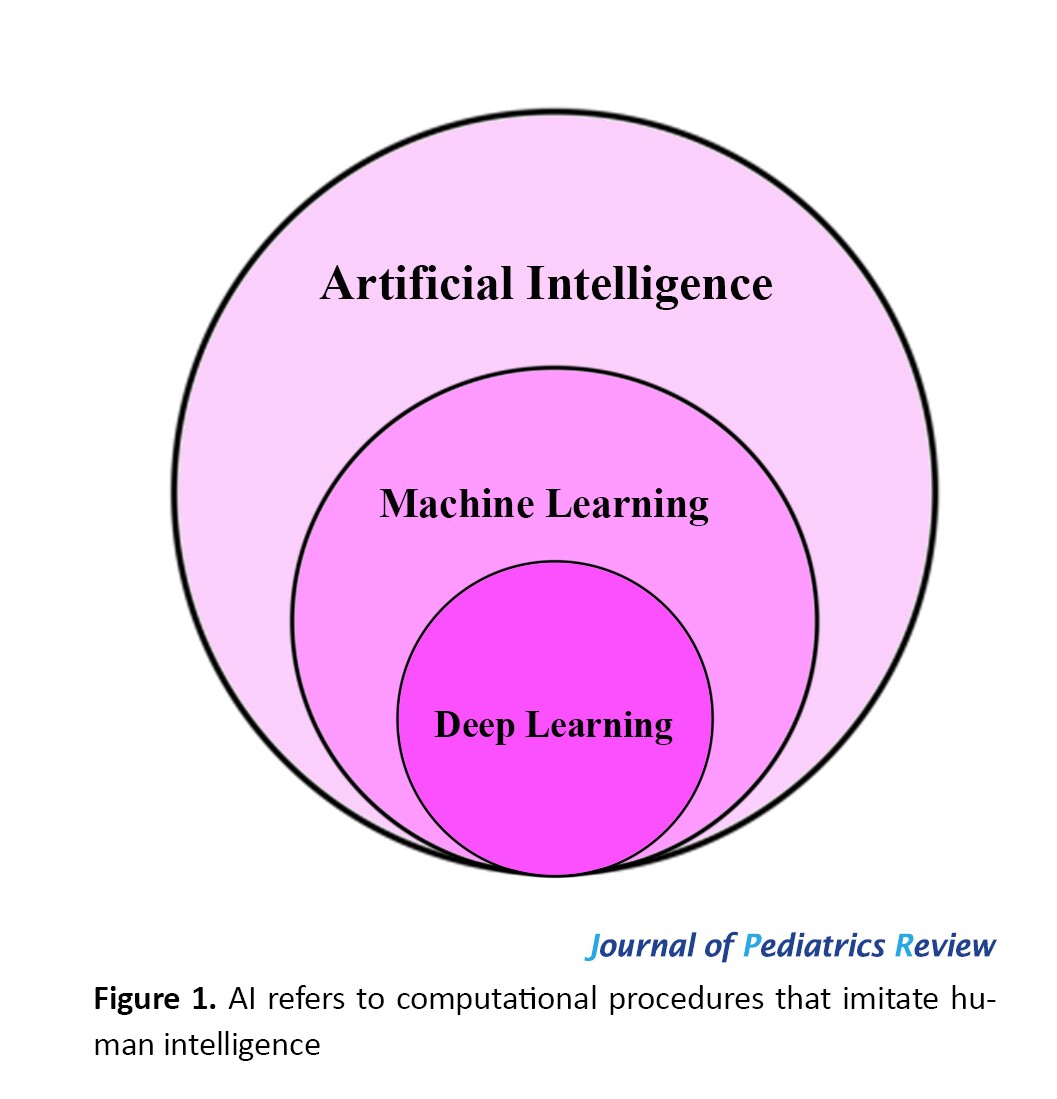
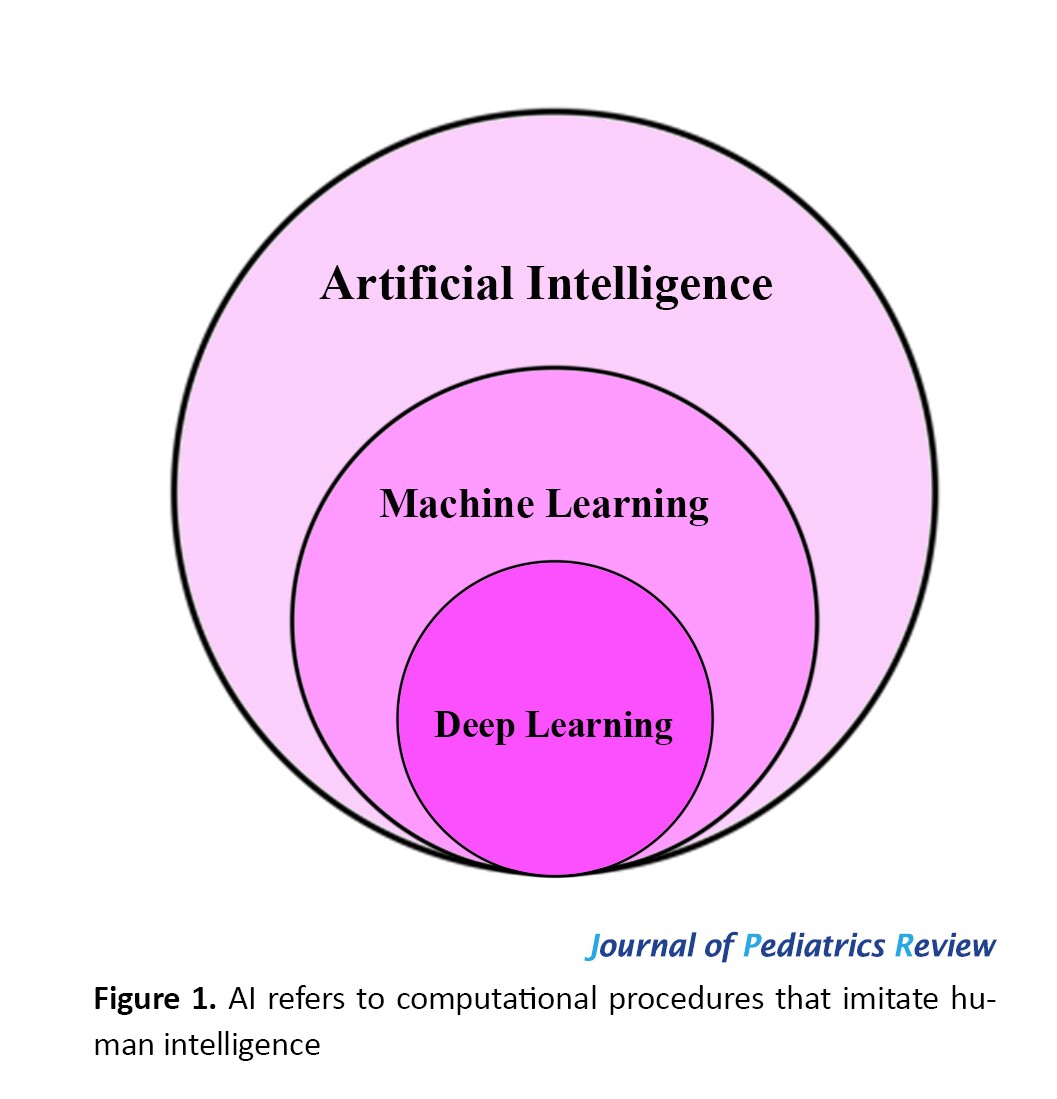
Artificial intelligence (AI) is defined as the ability of a machine to learn and recognize patterns in a sample of a dataset and apply the findings to make decisions about new data [1, 2]. In 1950, Alan Turing introduced the concept of using computers to simulate intelligent behavior and critical thinking. Since then, John McCarthy has used the term AI to refer to the knowledge and engineering of intelligent machines [3]. In the past decade, the popularity of AI has been accelerating in various fields, including medicine, due to our ability to gather enough sample data in different applications. AI subfields in medicine include machine learning (ML), deep learning (DL), and computer vision, depending on the type of application [2-4]. In ML, specific characteristics are used to identify patterns and analyze a specific situation. The machine can then learn from that information and apply it to similar but unknown future scenarios. In DL, which is a more advanced form of ML, algorithms are used to create an artificial neural network that can learn and make decisions independently, similar to the human brain (Figure 1). Computer vision is a process in which a computer obtains and understands information from a set of images or videos and then uses specific patterns to recognize similar cases [3, 5-8].
The application of AI in medicine can be divided into the following three categories based on its purpose:
Assisted interpretation, such as computer-aided detection or computer-aided diagnosis to assist in detection or diagnosis; Additional insight, where AI provides information beyond the understanding of physicians, such as gene prediction and image-based forecasting; Augmented image, including tasks like generating new and high-quality images [8].
In oncology, similar to other branches of medicine, AI has been employed to assist in various areas, such as risk prediction, screening, diagnosis, prognosis, initial treatment, response assessment, subsequent treatment, and follow-up. For example, a recently developed tool called molecular prognostic score can determine the prognosis of breast cancer patients [9, 10]. The use of AI to analyze a large amount of cancer genomic data or omics data (exome, transcriptome, and epigenome) and data related to the sensitivity of acute myeloid leukemia patients to anti-cancer drugs has led to the identification of specific drug-sensitive genes [10].
Currently, more than 20 AI-based applications have been approved by the FDA for clinical oncology and are used in specific areas of cancer treatment [11].
The CONSORT 2010 statement provides minimum guidelines for reporting randomized trials and has been widely used to ensure transparency in evaluating new interventions. With the expansion of AI-based clinical research in medicine, CONSORT-AI has been defined as a standard guideline for AI-based clinical trials in medicine [12].
As a branch of oncology, pediatric oncology has similarities and specific differences compared to adult oncology. Considering the increasing use of AI in pediatric oncology and cancer treatment, there is a need for studies and research projects specifically focused on pediatric oncology [13].
In AI, having accurate and abundant data is the key to success, and establishing proper databases and data classification can be a crucial step in optimizing the use of AI in medicine, especially in pediatric oncology.
In conclusion, it is highly recommended that healthcare providers in pediatric oncology familiarize themselves with AI. This stems from the fact that AI’s practical applications in medicine and more specifically in pediatric oncology will be a new emerging technology improving the quality of healthcare service soon.
References
Artificial intelligence (AI) is defined as the ability of a machine to learn and recognize patterns in a sample of a dataset and apply the findings to make decisions about new data [1, 2]. In 1950, Alan Turing introduced the concept of using computers to simulate intelligent behavior and critical thinking. Since then, John McCarthy has used the term AI to refer to the knowledge and engineering of intelligent machines [3]. In the past decade, the popularity of AI has been accelerating in various fields, including medicine, due to our ability to gather enough sample data in different applications. AI subfields in medicine include machine learning (ML), deep learning (DL), and computer vision, depending on the type of application [2-4]. In ML, specific characteristics are used to identify patterns and analyze a specific situation. The machine can then learn from that information and apply it to similar but unknown future scenarios. In DL, which is a more advanced form of ML, algorithms are used to create an artificial neural network that can learn and make decisions independently, similar to the human brain (Figure 1). Computer vision is a process in which a computer obtains and understands information from a set of images or videos and then uses specific patterns to recognize similar cases [3, 5-8].
The application of AI in medicine can be divided into the following three categories based on its purpose:
Assisted interpretation, such as computer-aided detection or computer-aided diagnosis to assist in detection or diagnosis; Additional insight, where AI provides information beyond the understanding of physicians, such as gene prediction and image-based forecasting; Augmented image, including tasks like generating new and high-quality images [8].
In oncology, similar to other branches of medicine, AI has been employed to assist in various areas, such as risk prediction, screening, diagnosis, prognosis, initial treatment, response assessment, subsequent treatment, and follow-up. For example, a recently developed tool called molecular prognostic score can determine the prognosis of breast cancer patients [9, 10]. The use of AI to analyze a large amount of cancer genomic data or omics data (exome, transcriptome, and epigenome) and data related to the sensitivity of acute myeloid leukemia patients to anti-cancer drugs has led to the identification of specific drug-sensitive genes [10].
Currently, more than 20 AI-based applications have been approved by the FDA for clinical oncology and are used in specific areas of cancer treatment [11].
The CONSORT 2010 statement provides minimum guidelines for reporting randomized trials and has been widely used to ensure transparency in evaluating new interventions. With the expansion of AI-based clinical research in medicine, CONSORT-AI has been defined as a standard guideline for AI-based clinical trials in medicine [12].
As a branch of oncology, pediatric oncology has similarities and specific differences compared to adult oncology. Considering the increasing use of AI in pediatric oncology and cancer treatment, there is a need for studies and research projects specifically focused on pediatric oncology [13].
In AI, having accurate and abundant data is the key to success, and establishing proper databases and data classification can be a crucial step in optimizing the use of AI in medicine, especially in pediatric oncology.
In conclusion, it is highly recommended that healthcare providers in pediatric oncology familiarize themselves with AI. This stems from the fact that AI’s practical applications in medicine and more specifically in pediatric oncology will be a new emerging technology improving the quality of healthcare service soon.
References
- Iqbal JD, Vinay R. Are we ready for artificial intelligence in medicine? Swiss Med Wkly. 2022; 152:w30179. [DOI:10.4414/SMW.2022.w30179] [PMID]
- Yasnitsky LN. Artificial intelligence and medicine: History, current state, and forecasts for the future. Curr Hypertens Rev. 2020; 16(3):211-5. [DOI: 0.2174/1573402116666200714150953]
- Kaul V, Enslin S, Gross SA. History of artificial intelligence in medicine. Gastrointest Endosc. 2020; 92(4):807-12. [DOI:10.1016/j.gie.2020.06.040] [PMID]
- Deshmukh R, Rathi P. Artificial intelligence in medicine. The Journal of the Association of Physicians of India. 2022; 70(3):11-2. [PMID]
- Haug CJ, Drazen JM. Artificial intelligence and machine learning in clinical medicine, 2023. N Engl J Med. 2023; 388(13):1201-8. [DOI:10.1056/NEJMra2302038] [PMID]
- Herman DS, Rhoads DD, Schulz WL, Durant TJS. Artificial intelligence and mapping a new direction in laboratory medicine: A review. Clin Chem. 2021; 67(11):1466-82. [DOI:10.1093/clinchem/hvab165] [PMID]
- Huynh E, Hosny A, Guthier C, Bitterman DS, Petit SF, Haas-Kogan DA, et al. Artificial intelligence in radiation oncology. Nat Rev Clin Oncol. 2020; 17(12):771-81. [DOI:10.1038/s41571-020-0417-8] [PMID]
- Hirata K, Sugimori H, Fujima N, Toyonaga T, Kudo K. Artificial intelligence for nuclear medicine in oncology. Ann Nucl Med. 2022; 36(2):123-32. [DOI:10.1007/s12149-021-01693-6] [PMID]
- Shimizu H, Nakayama KI. A 23 gene-based molecular prognostic score precisely predicts overall survival of breast cancer patients. EBioMedicine. 2019; 46:150-9. [DOI:10.1016/j.ebiom.2019.07.046] [PMID]
- Lee JS, Das A, Jerby-Arnon L, Arafeh R, Auslander N, Davidson M, et al. Harnessing synthetic lethality to predict the response to cancer treatment. Nat Commun. 2018; 9(1):2546. [DOI:10.1038/s41467-018-04647-1] [PMID]
- Kann BH, Hosny A, Aerts H. Artificial intelligence for clinical oncology. Cancer Cell. 2021; 39(7):916- 27. [DOI:10.1016/j.ccell.2021.04.002] [PMID]
- Shimizu H, Nakayama KI. Artificial intelligence in oncology. Cancer Sci. 2020; 111(5):1452-60. [DOI:10.1111/cas.14377] [PMID]
- Kattner P, Strobel H, Khoshnevis N, Grunert M, Bartholomae S, Pruss M, et al. Compare and contrast: Pediatric cancer versus adult malignancies. Cancer Metastasis Rev. 2019; 38:673-82. [DOI:10.1007/s10555-019-09836-y] [PMID]
Type of Study: Letter to the Editor |
Subject:
Pediatric Hematology and Oncology
Received: 2023/06/21 | Accepted: 2023/11/11 | Published: 2024/01/1
Received: 2023/06/21 | Accepted: 2023/11/11 | Published: 2024/01/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









