Volume 12, Issue 1 (1-2024)
J. Pediatr. Rev 2024, 12(1): 5-14 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Jalaly E, Ghazanfarpour M, Afiat M, Abdi F, Soleimany S, Saadat S. The Effects of Pleasant Odors on Transition From Gavage to Oral Feeding in Preterm Infants: A Systematic Review and Meta-analysis. J. Pediatr. Rev 2024; 12 (1) :5-14
URL: http://jpr.mazums.ac.ir/article-1-550-en.html
URL: http://jpr.mazums.ac.ir/article-1-550-en.html
Eghlima Jalaly1 

 , Masumeh Ghazanfarpour2
, Masumeh Ghazanfarpour2 

 , Malihe Afiat3
, Malihe Afiat3 

 , Fatemeh Abdi4
, Fatemeh Abdi4 

 , Saeed Soleimany5
, Saeed Soleimany5 

 , Sara Saadat *6
, Sara Saadat *6 




 , Masumeh Ghazanfarpour2
, Masumeh Ghazanfarpour2 

 , Malihe Afiat3
, Malihe Afiat3 

 , Fatemeh Abdi4
, Fatemeh Abdi4 

 , Saeed Soleimany5
, Saeed Soleimany5 

 , Sara Saadat *6
, Sara Saadat *6 


1- Unit of Clinical Research Development, Velayat Hospital, Semnan University of Medical Sciences, Semnan, Iran.
2- Family and Population Research Center, Kerman University of Medical Sciences, Kerman, Iran.
3- Milad Infertility Clinic Center, Mashhad University of Medical Sciences, Mashhad, Iran.
4- Nursing and Midwifery Care Research Center, Health Management Research Institute, Iran University of Medical Sciences, Tehran, Iran.
5- Regional Educational Blood Transfusion Center, Kerman, Iran.
6- Division of Nephrology, Department of Pediatric, Dr Sheikh Hospital, Mashhad University of Medical Sciences, Mashhad, Iran. ,dr.sarasaadat90@gmail.com
2- Family and Population Research Center, Kerman University of Medical Sciences, Kerman, Iran.
3- Milad Infertility Clinic Center, Mashhad University of Medical Sciences, Mashhad, Iran.
4- Nursing and Midwifery Care Research Center, Health Management Research Institute, Iran University of Medical Sciences, Tehran, Iran.
5- Regional Educational Blood Transfusion Center, Kerman, Iran.
6- Division of Nephrology, Department of Pediatric, Dr Sheikh Hospital, Mashhad University of Medical Sciences, Mashhad, Iran. ,
Full-Text [PDF 568 kb]
(1120 Downloads)
| Abstract (HTML) (3001 Views)
Full-Text: (879 Views)
Introduction
Premature birth refers to pregnancy under 37 weeks and it can increase the risk of mortality and disability due to ineffective oral feeding function [1]. Although current advances in technology have led to improvements in the survival rate of premature infants, such infants are physically immature and prone to long-term health disorders [2]. These infants are immature in terms of oral feeding functions, such as sucking reflex, swallowing, and their harmony with respiration. This emphasizes the need for prolonged enteral feeding gavage [3].
Gavage feeding is a nutritional support before a premature baby can successfully feed from the nipple. It occurs via breast or formula milk with the help of a flexible tube that enters the baby’s stomach through the nostril. Occupational therapists focus on facilitating the transition from gavage feeding to lactation or bottle feeding [4]. Gavage feeding can be followed by multiple side effects, such as breathing problems among low birth weight babies, feeding conditions and irritations in and around the mouth, bradycardia, gag reflex, hyperactivity, and parental rejection and frustration [5]. One of the basic measures for better care and faster discharge of infants from the hospital is to improve their oral feeding capacity. Many beneficial approaches have been studied and reported in this area, such as the smell of milk applied to the nipple, sensory-motor-oral stimulation, and non-nutritive sucking [6]. The non-nutritive sucking can have a positive impact on subsequent feeding performance and tube-to-bottle feeding transition [7]. According to the evidence, premature infants stimulated by the smell of maternal breast milk have shown an increase in the frequency of non-nutritive sucking [4, 8].
Accordingly, it is essential to undertake a comprehensive review of the compression of effects of breast milk and other pleasant odors with the control group on the transition from gavage to oral feeding in preterm infants.
Methods
The current systematic review was based on the cochrane handbook for systematic reviews of interventions [9] and uses the preferred reporting items for systematic reviews and meta-analyses statement [10] and the patient, intervention, comparison, and outcome strategy of the population was determined as follows: Patient=premature birth defined as birth under 37 weeks [11] investigated in these papers; interventions=breast milk and other pleasant odors; comparison=any treatment could be included in the study as a control group; outcomes=the measured primary outcome was transition time from tube feeding (gavage) to oral feeding.
The following electronic databases were searched for relevant articles: PubMed, Cochrane Library, Web of Science, and Scopus. To retrieve the original clinical trials, all the selected databases were searched in English without time limitation up to March 2022. The initial search provided 106 relevant articles.
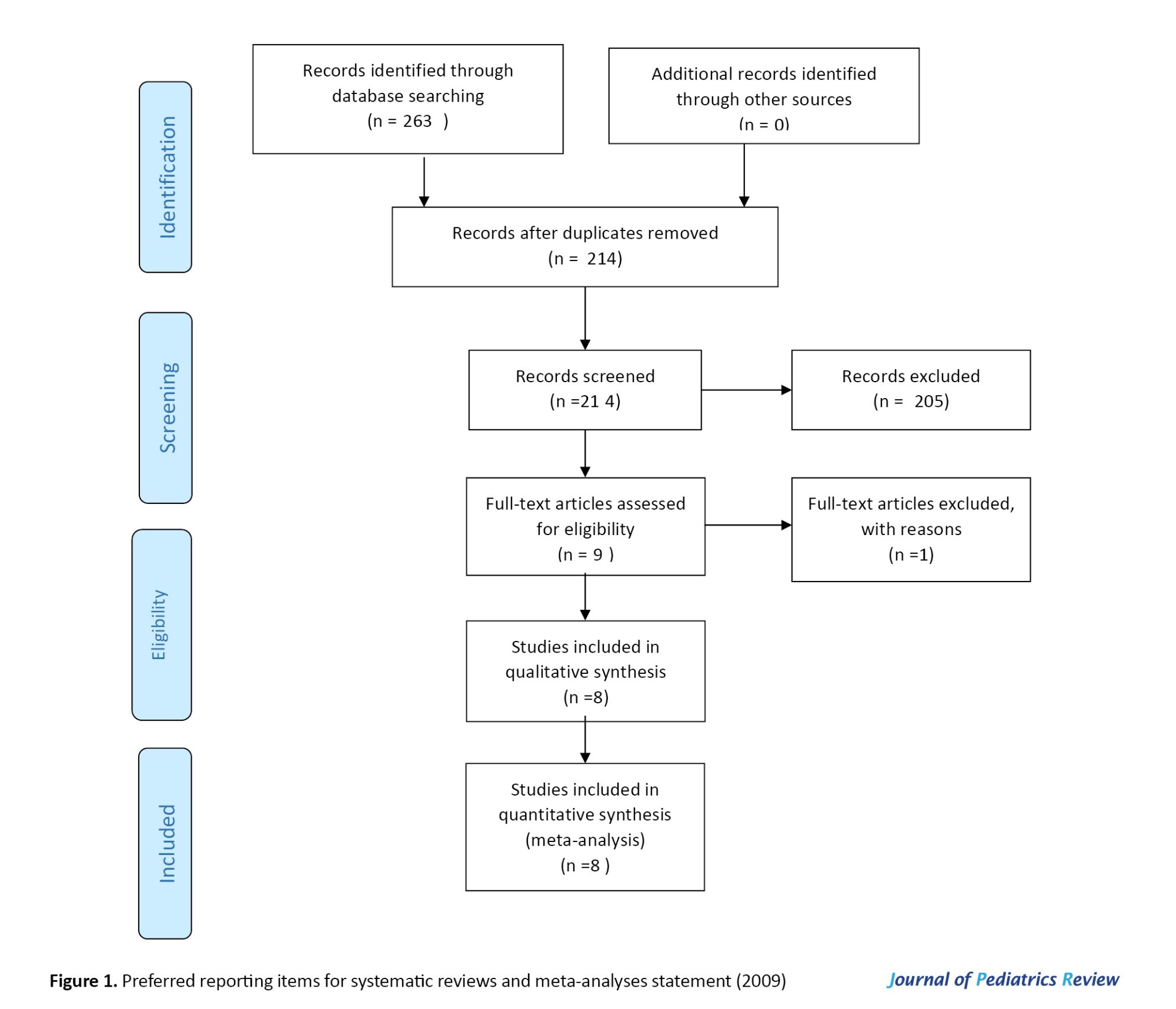
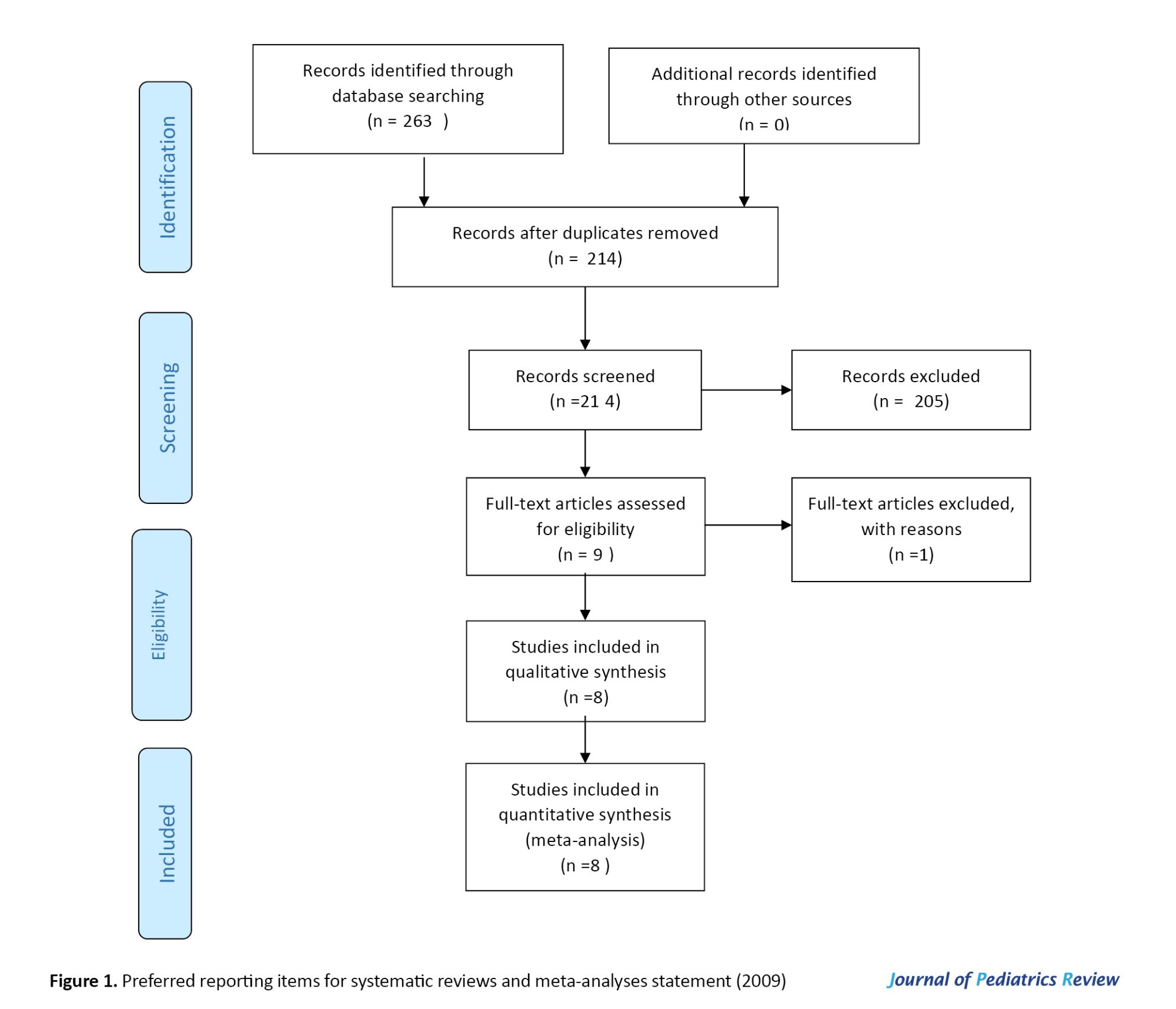
The combination of terms used in the search was based on MeSH as well as the keywords mentioned in the related articles, including preterm infant, premature infant, aromatherapy, aroma, smell, odor, gavage, and breastfeeding using logical operators (OR, NOT, AND). An example of a search strategy was aromatherapy OR aroma OR smell OR odor AND gavage feeding OR non-nutritive sucking OR breastfeeding OR preterm infant OR premature infant. In addition, other references from original articles and related reviews were searched and reviewed in these databases. Duplicate papers were deleted based on the screening of titles and abstracts. The full text of all remaining articles was assessed for eligibility criteria. The search was performed manually in electronic databases for seminars, conferences, congresses, and references. In case of finding a study abstract related to the subject of the present study, the full text of the article was requested from the corresponding author through correspondence. Figure 1 shows the process of data selection.
Data extraction and integration
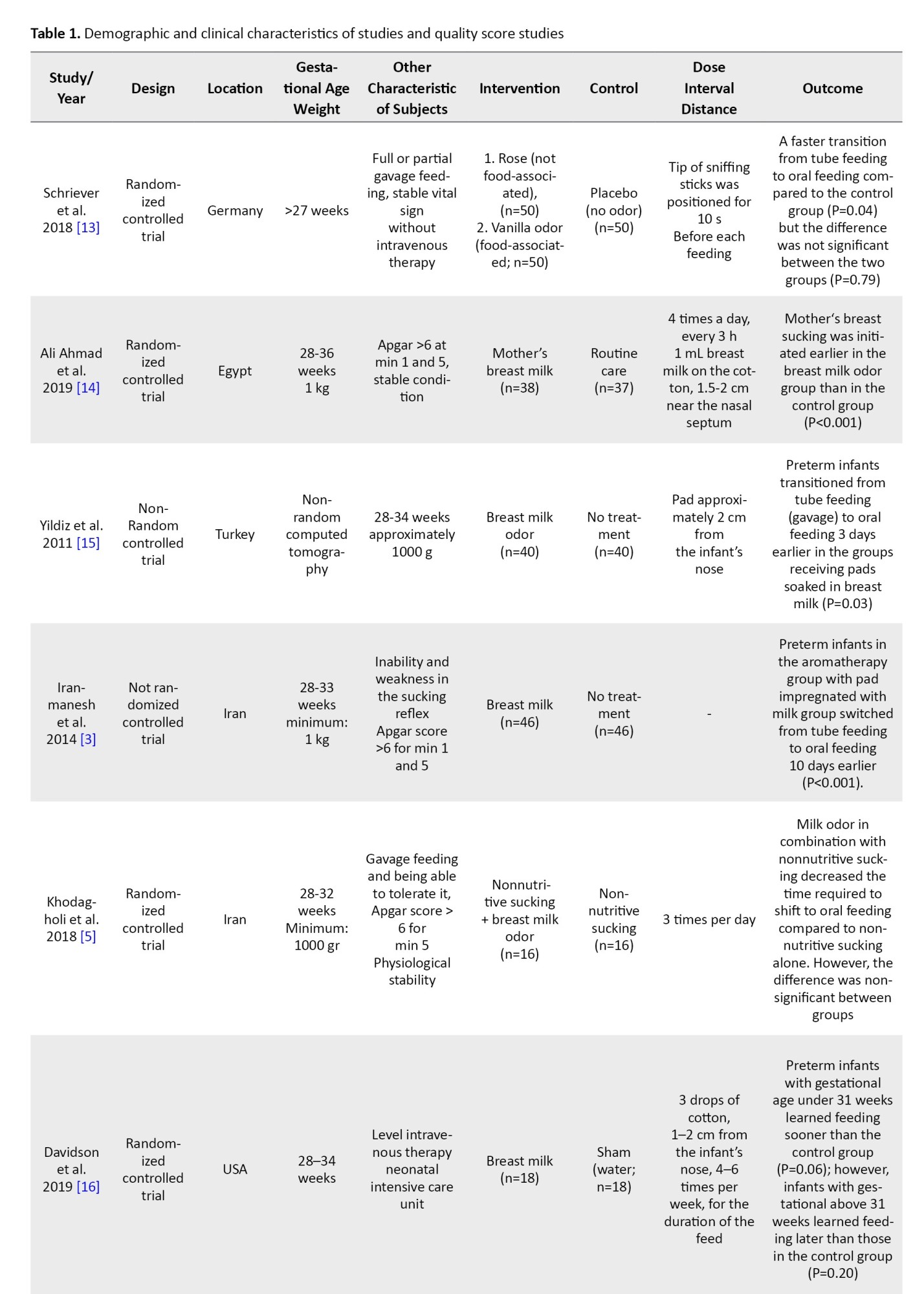
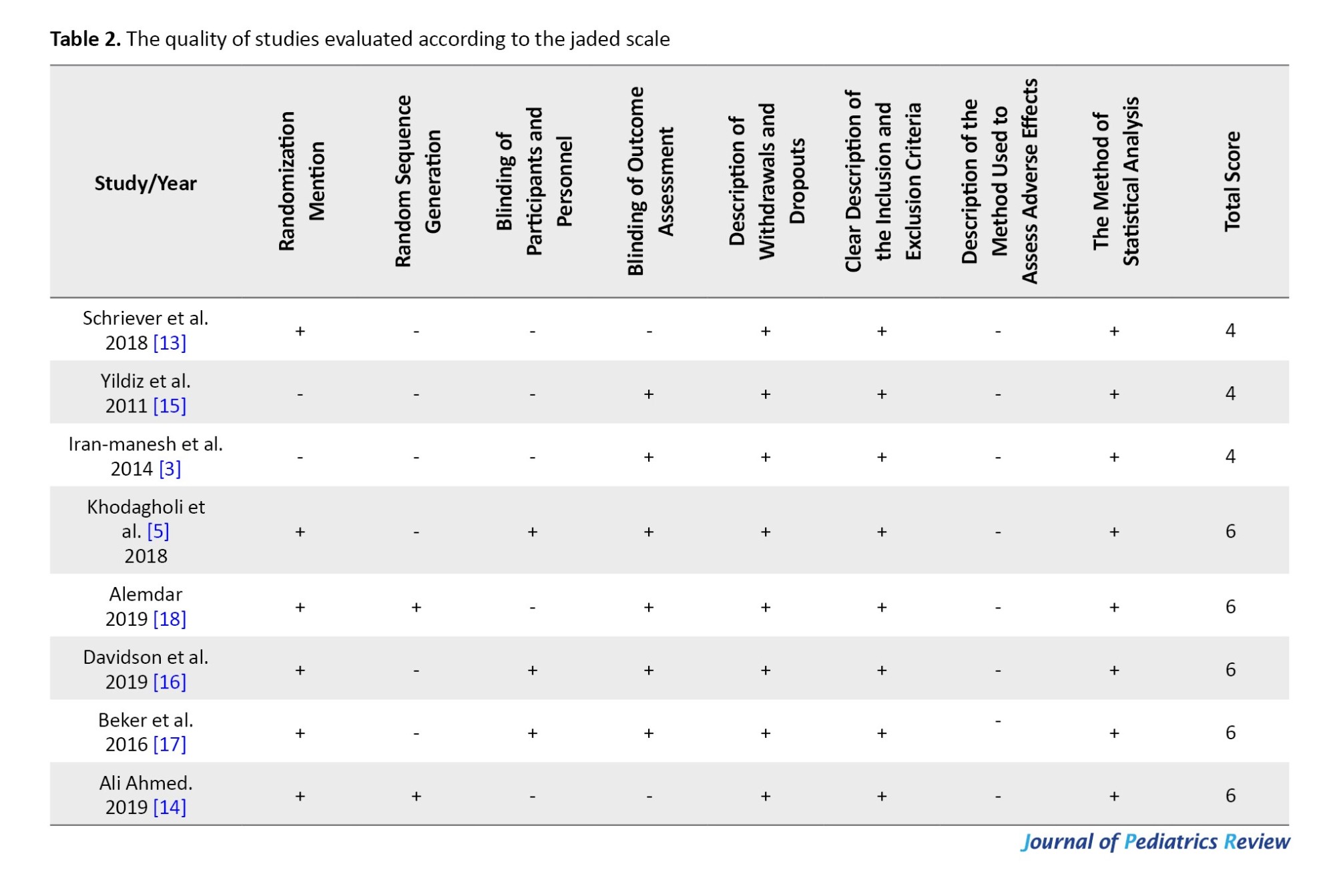
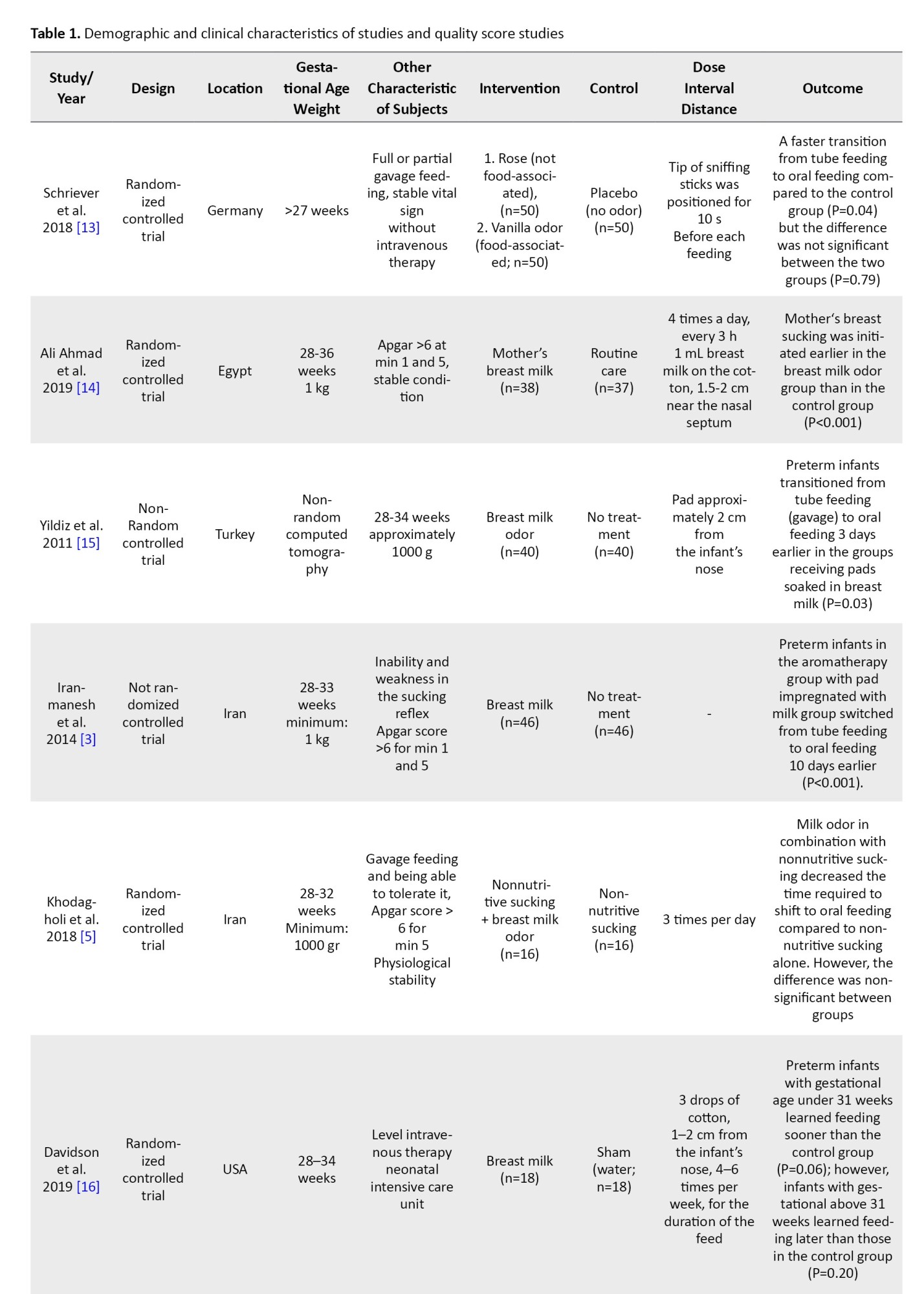
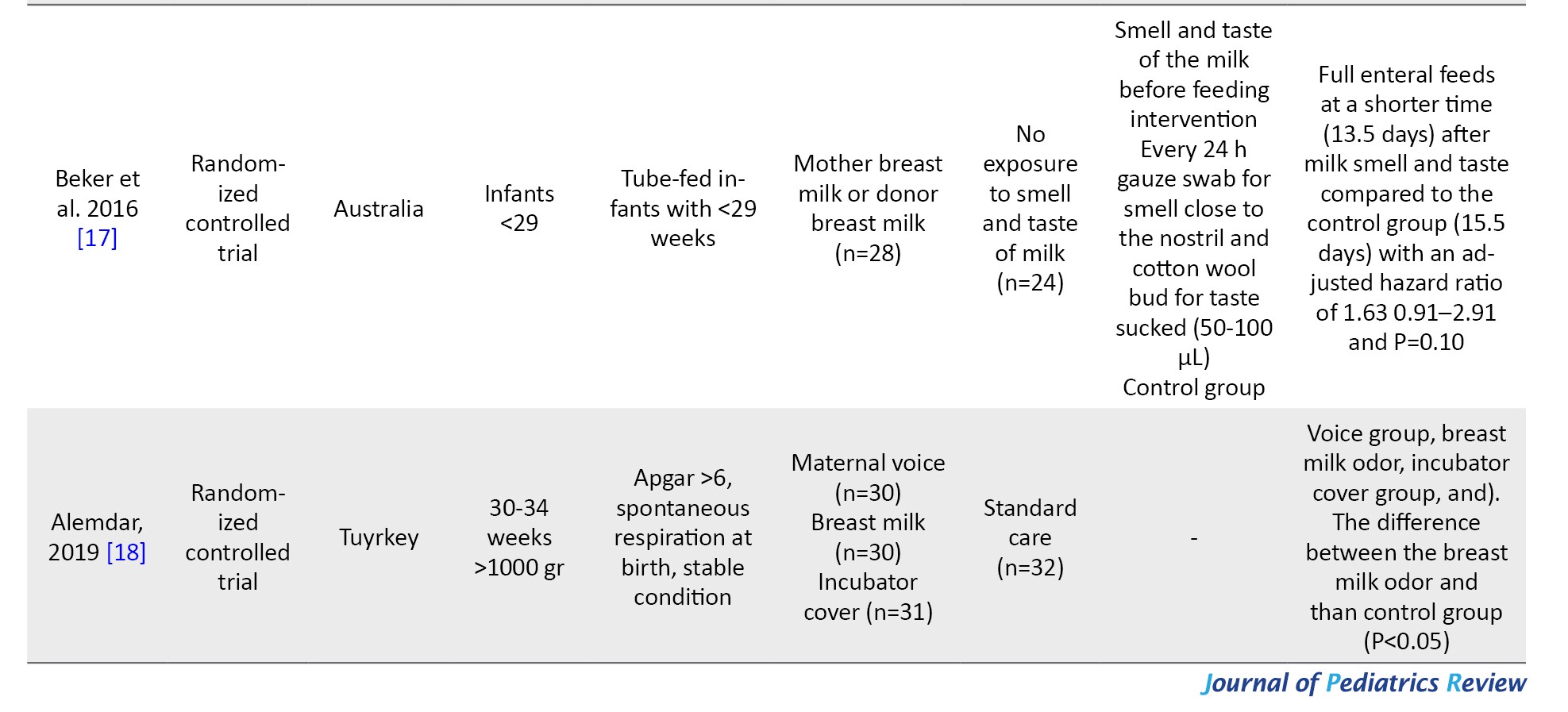
The Cochrane data extraction form was used for systematic review. Two authors of this research separately extracted information from the included studies and reached a consensus after discussion. The required information was the name of the first author, year of publication, place of research, study design, intervention measures, educational content, sessions and duration, and the main findings of the study. The findings were reported in several sections as follows: General characteristics of the reviewed articles and their quality, type of interventions presented and their assessed outcomes, and primary and secondary outcomes (Table 1).
Inclusion and exclusion criteria
The inclusion criteria comprised all clinical trials evaluating the effect of aromatherapy on variables of apnea, oral food intake, pain, oxygen saturation, heart rate, growth, and length of hospital stay in preterm infants. The preterm infants were defined as newborns with less than 37 weeks of gestation. We only enrolled interventions using olfactory senses. The exclusion criteria were non-English articles, letters to the editor, reviews, non-human studies, and multi-sensorial intervention studies.
Quality assessment
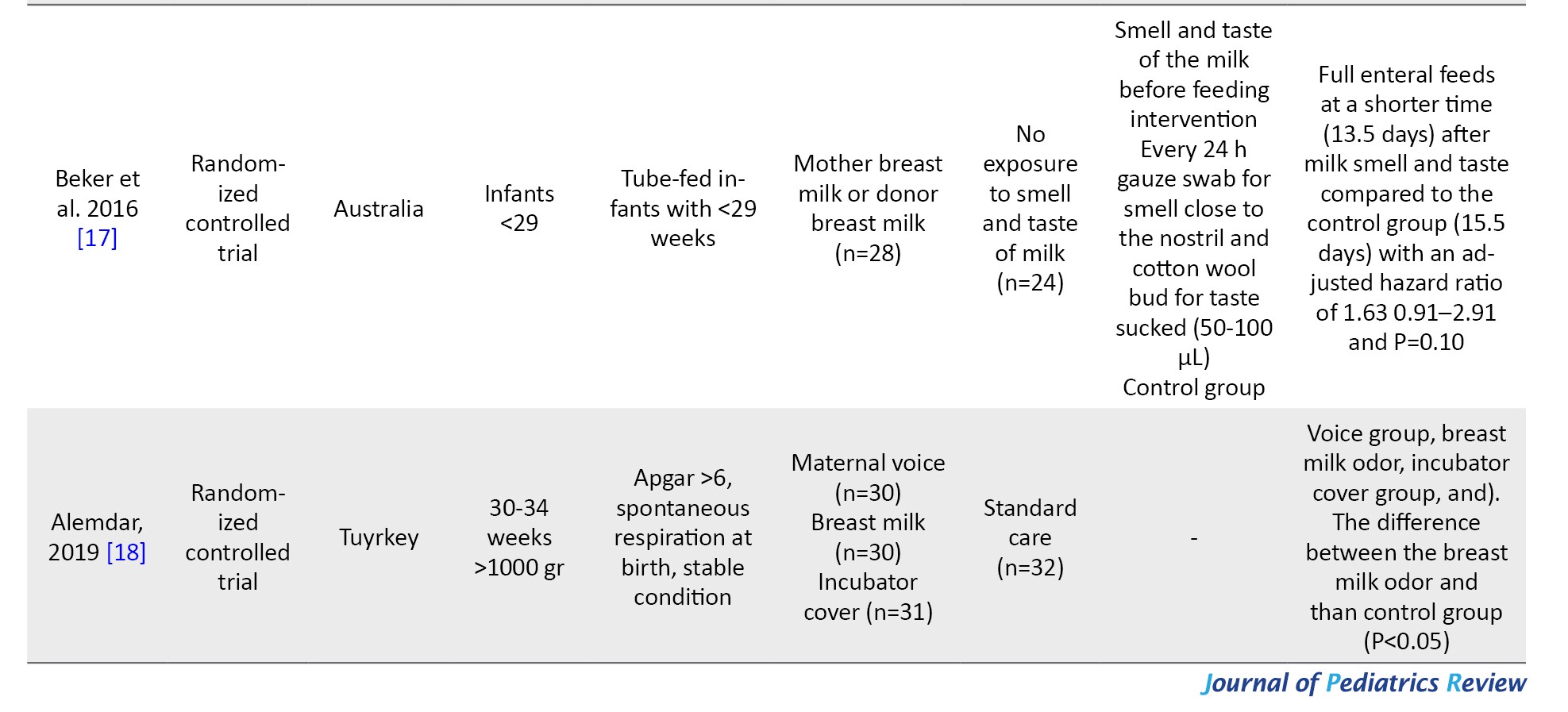
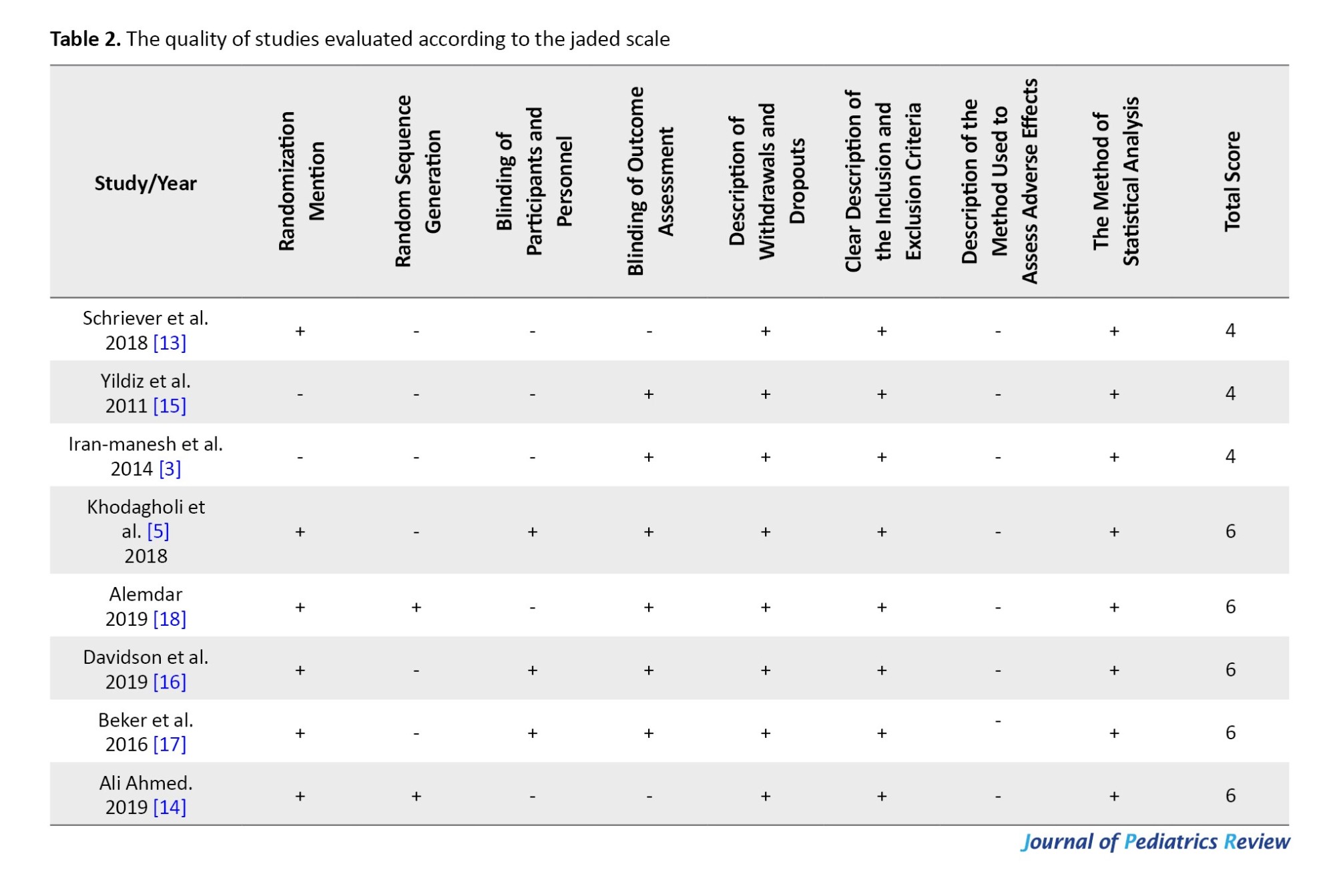
The quality of studies was evaluated according to the Jaded scale that consisted of randomization (reference to randomization, random sequence generation method), blinding (blinding of staff or outcome assessor), a description of withdrawals and dropouts, a clear description of inclusion or exclusion criteria, a description of the method of assessing adverse effects, a description of the statistical analysis method and the total score. The quality of the studies was examined independently by the two authors. Disagreements between the assessors were resolved by a third party (Table 2).
Statistical analysis
The analysis was conducted using the given evidence [12]. Standardized mean difference (SMD) with 95% confidence interval (CI). Heterogeneity was measured using the Tau2 test and I2 statistics. SM <0.40 was considered a small effect size, while SMD between 0.40-0.70 indicated a moderate effect size and >0.70 showed a larger effect size.
Results
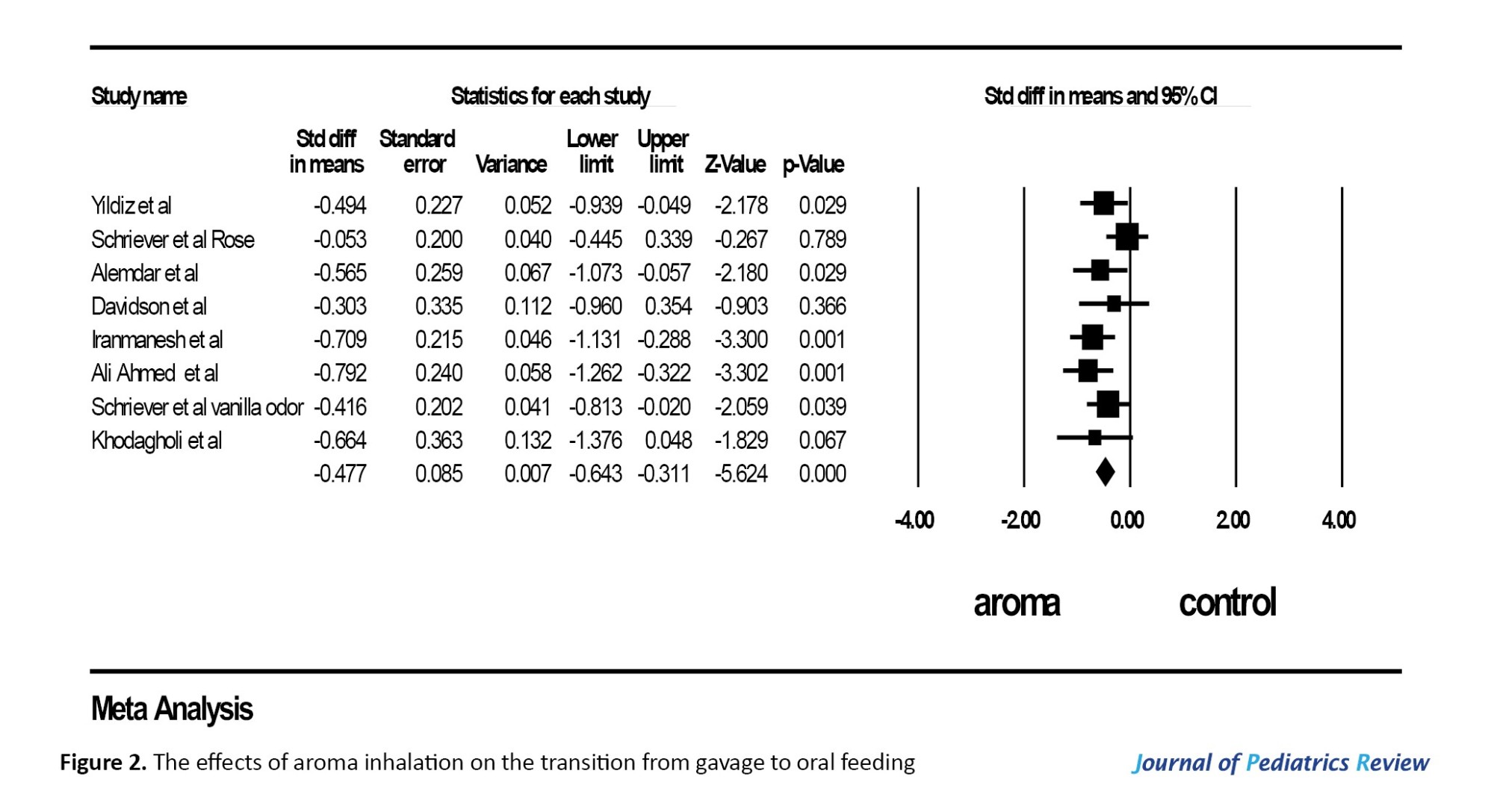
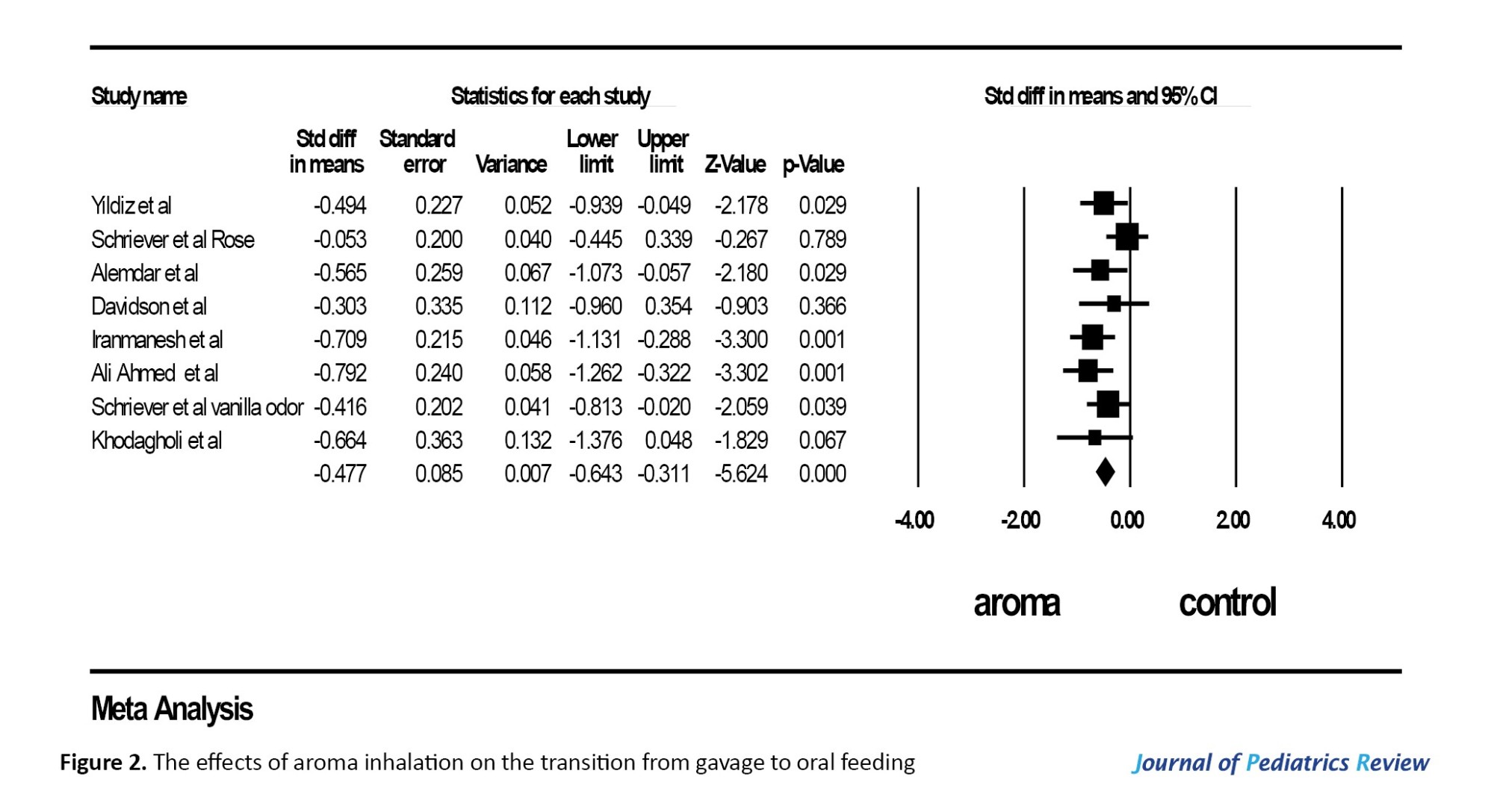
According to the results, one study was in Germany, two studies in Turkey, two studies in Iran, one study in the USA, one study in Australia, and one study in Egypt. Seven studies were conducted on the odor of breast milk and one study compared the odor of rose and the odor of vanilla odor. Also, eight studies assessed the effects of the transition from gavage to oral feeding. Mild heterogeneity was observed in the meta-analysis between studies. Meta-analysis of these studies shows that preterm infants transitioned from tube feeding (gavage) to oral feeding earlier in the groups stimulated by odor in the comparison control group (SMD=₋0.47, 95% CI, ₋0.64%, ₋0.31%, P=0.32, I2=13%, fixed effect model) Figure 2).
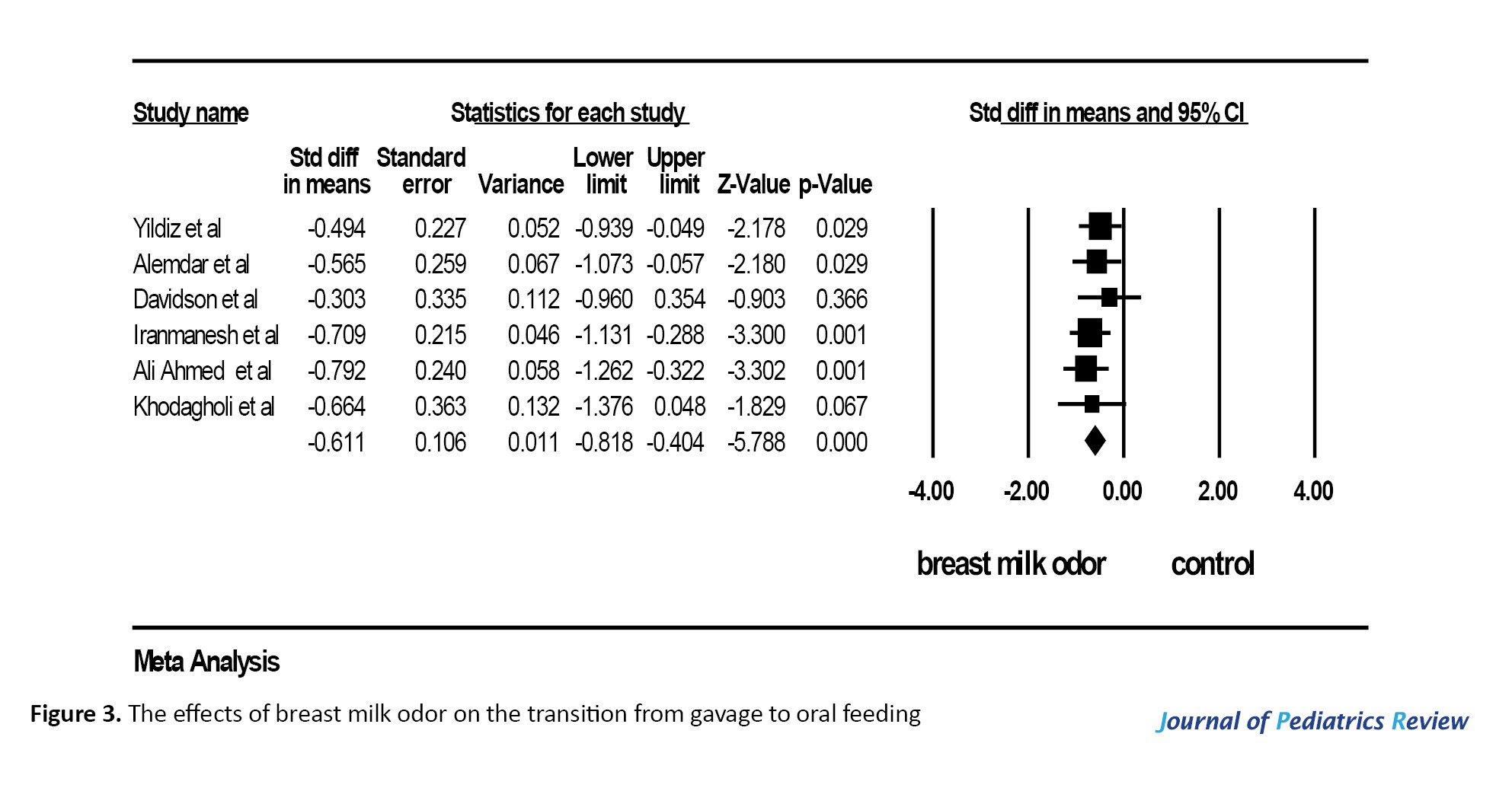
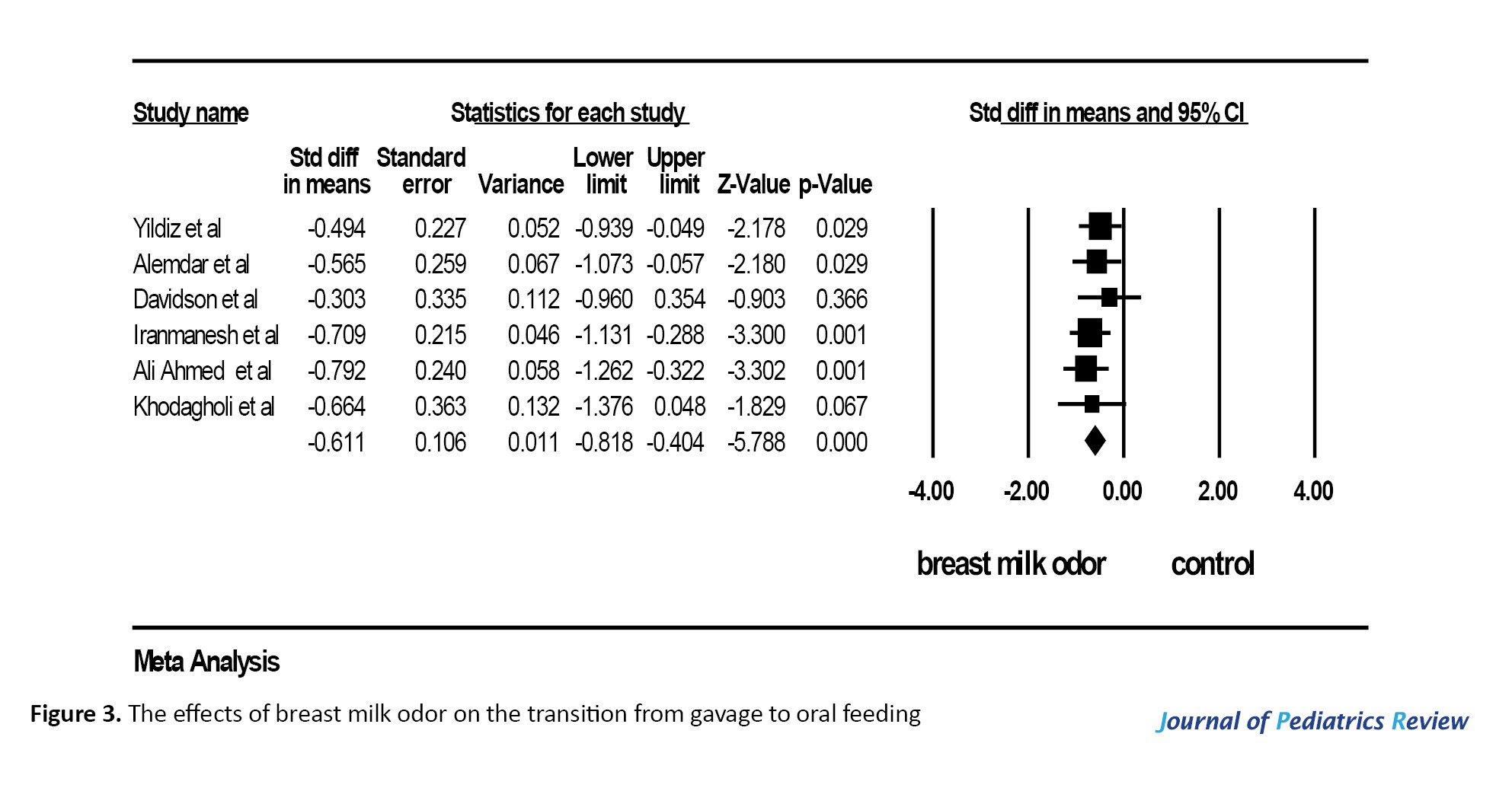
To detect resources of heterogeneity, analysis was done based on the type of aroma inhalation and breast milk odor. Meanwhile, six studies assessed the effects of the transition from gavage to oral feeding meta-analysis of these studies shows that preterm infants transitioned from tube feeding (gavage) to oral feeding earlier in the groups stimulated by odor compared with the control group (SMD=₋0.61, 95% CI, ₋0.64%, ₋0.31%, heterogeneity, P=0.85, I2=0%, fixed effect model) (Figure 3).
Discussion
This is the first meta-analysis to assess the effects of breast milk and other pleasant odors on the transition from gavage to oral feeding in preterm infants. Our meta-analysis showed that preterm infants transitioned from tube feeding (gavage) to oral feeding earlier in the groups stimulated by the combination of various odors (vanilla, roes, and milk breast) and milk breast odors in the comparison control group. A meta-analysis that combined 2 studies reported preterm infants exposed to the smell and taste of milk reached full enteral feeds in a shorter time. In contrast, the results of a systematic review revealed that exposure to the smell and taste of milk with gastric ormnasogastric tube feedings did not show any significant effect on the transition time from gavage to oral feeding. However, they concluded exposure to the smell and taste of milk with orogastric or nasogastric tubes may decrease the length of hospitalization in preterm infants [19]. These results are in contrast with our meta-analysis results, which showed a significant effect of milk breast odor on the time to reach full oral feeding. These differences in results between our meta-analysis and Muelbert et al. can be explained by the number of studies included and the difference in statistical methods in which we reported the effect size of our data with the SMD while Muelbert et al. [19] used the mean difference to report their data.
In the preterm infants exposed to vanilla odor, a faster transition from tube feeding to oral feeding compared to the control group was observed (P=0.04); however, the difference was not significant between the rose and control groups (P=0.79) [13]. Nonetheless, it is still clear what the mechanisms underlying of vanilla effect caused a faster transition from tube feeding to oral feeding. This will be the focus of future research.
Infants whose mothers had consumed anise during pregnancy had stable preference for anise odor immediately after birth and on a day than infants whose mothers had not the consumption of anise [20]. These findings suggest that infants’ preferences and olfactory responses are affected by their diet as human mothers. No study included in this systematic review collected information about the infant’s mother’s diet during pregnancy. Therefore, infants’ preferences and olfactory responses could have possibly influenced the results in the systematic review.
Five studies showed a positive effect of aroma inhalation on the transition from gavage to oral feeding. Alemdar discovered a significant difference in terms of the average time of transition to oral feeding among four groups (voice group, breast milk odor, incubator cover group, and control group). According to the post hoc analysis, the difference is attributed to the breast milk odor (group feeding) (P<0.05) [18]. In the study of Iranmanesh et al. in comparison to infants in the control group, preterm infants in the aromatherapy group with pad impregnated with milk group switched from tube feeding to oral feeding 10 days earlier (P<0.001) [3].
As reported by Yildiz et al. preterm infants transitioned from tube feeding (gavage) to oral feeding 3 days earlier in the groups receiving pads soaked in breast milk (P=0.03) [15]. In Beker et al.’s study, infants reached full enteral feeds at a shorter time (13.5 days) after milk smell and taste compared to the control group (15.5 days) with an adjusted hazard ratio of 1.63 0.91–2.91 and P=0.10 [17]. In the study of Ali Ahmed, the mother’s breast sucking was initiated earlier in the breast milk odor group than in the control group (P<0.001) [14]. Two studies have reported borderline significant results. According to Davidson et al., infants in the sham intervention group and mother’s own milk infants were not different in terms of improved oral feeding skills. However, preterm infants responded differently to mothers’ own milk based on gestational age (3131). Preterm infants with gestational age under 31 weeks learned feeding sooner than the control group (P=0.06); however, infants with gestational above 31 weeks learned feeding later than those in the control group (P=0.20) [16]. In a study by Khodagholi et al., milk odor in combination with nonnutritive sucking decreased the time required to shift to oral feeding compared to nonnutritive sucking alone. However, the difference was non-significant between groups (P=0.07) [5].
Our meta-analysis shows that preterm infants transitioned from tube feeding (gavage) to oral feeding earlier in the groups stimulated milk breast odors.
Breastfeeding behavior may be the reason our meta-analysis shows that preterm infants transitioned from tube feeding (gavage) to oral feeding earlier in the groups stimulated by milk breastfeeding odors. The odor of mother’s milk was found to affect on breastfeeding behavior of premature neonates. In Raimbault’s study, infants in the milk-odor group showed longer sucking bouts and more bursts consisting of >7 sucking movements in comparison to control infants [21]. In the study of Porter et al., the odor of fresh breast milk at week 36 significantly increased sucking movements compared to both water (P<0.005) and pooled donor milk (P<0.005) as opposed to infants in the control group. The frequency of sucking in response to fresh breast milk was also higher than that of frozen breast milk, but the difference was not statistically significant (P=0.09). Both frozen breast milk and pooled donor milk showed a higher rate of sucking compared to water trials (P<0.05). However, the conditions of frozen breast milk and pooled donor milk were not different in the sucking behavior [22]. In the study of Meza et al., the frequency of high-amplitude non-nutritive sucking was greater in the maternal breast odor group than in the control group (no odor) [4].
The reported literature showed controversial findings regarding sex differences in response to environmental stimuli [23, 24]. In a study by Davidson et al. [16], no sex differences were found in response to aroma inhalation with breastfeeding on the transition from gavage to oral feeding. In addition, premature newborns with <31 weeks gestation learned to feed sooner when stimulated with the mother’s own milk than the control group [16]. However, the authors concluded that their findings should be interpreted with caution small sample size.
Conclusion
Our meta-analysis supports the use of breast milk odor as a safe, noninvasive, and shorter time reach to oral feeds in preterm infants. It costs only commented to health providers to develop such family-friendly interventions that incorporate parents, have an active and important role in providing care to their premature infants
Ethical Considerations
Compliance with ethical guidelines
All ethical principles are considered in this article.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization, project administration, and funding acquisition: Masumeh Ghazanfarpour, Malihe Afiat, Sara Saadat, Eghlima Jalaly and Saeed Soleimany; Methodology: Masumeh Ghazanfarpour, Fatemeh Abdi, Sara Saadat, Eghlima Jalaly and Saeed Soleimany; Software: Eghlima Jalaly, Malihe Afiat and Masumeh Ghazanfarpour; Validation and supervision: Masumeh Ghazanfarpour and Sara Saadat; Formal analysis: Masumeh Ghazanfarpour, Fatemeh Abdi, Malihe Afiat and Saeed Soleimany; Investigation: Eghlima Jalaly, Malihe Afiat and Sara Saadat; Resources: Masumeh Ghazanfarpour, Fatemeh Abdi and Eghlima Jalaly; Data curation, Masumeh Ghazanfarpour, Malihe Afiat and Fatemeh Abdi; Writing the original draft: Eghlima Jalaly, Masumeh Ghazanfarpour and Sara Saadat; Review and editing: All authors.
Conflicts of interest
The authors declared no conflict of interest.
References
Premature birth refers to pregnancy under 37 weeks and it can increase the risk of mortality and disability due to ineffective oral feeding function [1]. Although current advances in technology have led to improvements in the survival rate of premature infants, such infants are physically immature and prone to long-term health disorders [2]. These infants are immature in terms of oral feeding functions, such as sucking reflex, swallowing, and their harmony with respiration. This emphasizes the need for prolonged enteral feeding gavage [3].
Gavage feeding is a nutritional support before a premature baby can successfully feed from the nipple. It occurs via breast or formula milk with the help of a flexible tube that enters the baby’s stomach through the nostril. Occupational therapists focus on facilitating the transition from gavage feeding to lactation or bottle feeding [4]. Gavage feeding can be followed by multiple side effects, such as breathing problems among low birth weight babies, feeding conditions and irritations in and around the mouth, bradycardia, gag reflex, hyperactivity, and parental rejection and frustration [5]. One of the basic measures for better care and faster discharge of infants from the hospital is to improve their oral feeding capacity. Many beneficial approaches have been studied and reported in this area, such as the smell of milk applied to the nipple, sensory-motor-oral stimulation, and non-nutritive sucking [6]. The non-nutritive sucking can have a positive impact on subsequent feeding performance and tube-to-bottle feeding transition [7]. According to the evidence, premature infants stimulated by the smell of maternal breast milk have shown an increase in the frequency of non-nutritive sucking [4, 8].
Accordingly, it is essential to undertake a comprehensive review of the compression of effects of breast milk and other pleasant odors with the control group on the transition from gavage to oral feeding in preterm infants.
Methods
The current systematic review was based on the cochrane handbook for systematic reviews of interventions [9] and uses the preferred reporting items for systematic reviews and meta-analyses statement [10] and the patient, intervention, comparison, and outcome strategy of the population was determined as follows: Patient=premature birth defined as birth under 37 weeks [11] investigated in these papers; interventions=breast milk and other pleasant odors; comparison=any treatment could be included in the study as a control group; outcomes=the measured primary outcome was transition time from tube feeding (gavage) to oral feeding.
The following electronic databases were searched for relevant articles: PubMed, Cochrane Library, Web of Science, and Scopus. To retrieve the original clinical trials, all the selected databases were searched in English without time limitation up to March 2022. The initial search provided 106 relevant articles.
The combination of terms used in the search was based on MeSH as well as the keywords mentioned in the related articles, including preterm infant, premature infant, aromatherapy, aroma, smell, odor, gavage, and breastfeeding using logical operators (OR, NOT, AND). An example of a search strategy was aromatherapy OR aroma OR smell OR odor AND gavage feeding OR non-nutritive sucking OR breastfeeding OR preterm infant OR premature infant. In addition, other references from original articles and related reviews were searched and reviewed in these databases. Duplicate papers were deleted based on the screening of titles and abstracts. The full text of all remaining articles was assessed for eligibility criteria. The search was performed manually in electronic databases for seminars, conferences, congresses, and references. In case of finding a study abstract related to the subject of the present study, the full text of the article was requested from the corresponding author through correspondence. Figure 1 shows the process of data selection.
Data extraction and integration
The Cochrane data extraction form was used for systematic review. Two authors of this research separately extracted information from the included studies and reached a consensus after discussion. The required information was the name of the first author, year of publication, place of research, study design, intervention measures, educational content, sessions and duration, and the main findings of the study. The findings were reported in several sections as follows: General characteristics of the reviewed articles and their quality, type of interventions presented and their assessed outcomes, and primary and secondary outcomes (Table 1).
Inclusion and exclusion criteria
The inclusion criteria comprised all clinical trials evaluating the effect of aromatherapy on variables of apnea, oral food intake, pain, oxygen saturation, heart rate, growth, and length of hospital stay in preterm infants. The preterm infants were defined as newborns with less than 37 weeks of gestation. We only enrolled interventions using olfactory senses. The exclusion criteria were non-English articles, letters to the editor, reviews, non-human studies, and multi-sensorial intervention studies.
Quality assessment
The quality of studies was evaluated according to the Jaded scale that consisted of randomization (reference to randomization, random sequence generation method), blinding (blinding of staff or outcome assessor), a description of withdrawals and dropouts, a clear description of inclusion or exclusion criteria, a description of the method of assessing adverse effects, a description of the statistical analysis method and the total score. The quality of the studies was examined independently by the two authors. Disagreements between the assessors were resolved by a third party (Table 2).
Statistical analysis
The analysis was conducted using the given evidence [12]. Standardized mean difference (SMD) with 95% confidence interval (CI). Heterogeneity was measured using the Tau2 test and I2 statistics. SM <0.40 was considered a small effect size, while SMD between 0.40-0.70 indicated a moderate effect size and >0.70 showed a larger effect size.
Results
According to the results, one study was in Germany, two studies in Turkey, two studies in Iran, one study in the USA, one study in Australia, and one study in Egypt. Seven studies were conducted on the odor of breast milk and one study compared the odor of rose and the odor of vanilla odor. Also, eight studies assessed the effects of the transition from gavage to oral feeding. Mild heterogeneity was observed in the meta-analysis between studies. Meta-analysis of these studies shows that preterm infants transitioned from tube feeding (gavage) to oral feeding earlier in the groups stimulated by odor in the comparison control group (SMD=₋0.47, 95% CI, ₋0.64%, ₋0.31%, P=0.32, I2=13%, fixed effect model) Figure 2).
To detect resources of heterogeneity, analysis was done based on the type of aroma inhalation and breast milk odor. Meanwhile, six studies assessed the effects of the transition from gavage to oral feeding meta-analysis of these studies shows that preterm infants transitioned from tube feeding (gavage) to oral feeding earlier in the groups stimulated by odor compared with the control group (SMD=₋0.61, 95% CI, ₋0.64%, ₋0.31%, heterogeneity, P=0.85, I2=0%, fixed effect model) (Figure 3).
Discussion
This is the first meta-analysis to assess the effects of breast milk and other pleasant odors on the transition from gavage to oral feeding in preterm infants. Our meta-analysis showed that preterm infants transitioned from tube feeding (gavage) to oral feeding earlier in the groups stimulated by the combination of various odors (vanilla, roes, and milk breast) and milk breast odors in the comparison control group. A meta-analysis that combined 2 studies reported preterm infants exposed to the smell and taste of milk reached full enteral feeds in a shorter time. In contrast, the results of a systematic review revealed that exposure to the smell and taste of milk with gastric ormnasogastric tube feedings did not show any significant effect on the transition time from gavage to oral feeding. However, they concluded exposure to the smell and taste of milk with orogastric or nasogastric tubes may decrease the length of hospitalization in preterm infants [19]. These results are in contrast with our meta-analysis results, which showed a significant effect of milk breast odor on the time to reach full oral feeding. These differences in results between our meta-analysis and Muelbert et al. can be explained by the number of studies included and the difference in statistical methods in which we reported the effect size of our data with the SMD while Muelbert et al. [19] used the mean difference to report their data.
In the preterm infants exposed to vanilla odor, a faster transition from tube feeding to oral feeding compared to the control group was observed (P=0.04); however, the difference was not significant between the rose and control groups (P=0.79) [13]. Nonetheless, it is still clear what the mechanisms underlying of vanilla effect caused a faster transition from tube feeding to oral feeding. This will be the focus of future research.
Infants whose mothers had consumed anise during pregnancy had stable preference for anise odor immediately after birth and on a day than infants whose mothers had not the consumption of anise [20]. These findings suggest that infants’ preferences and olfactory responses are affected by their diet as human mothers. No study included in this systematic review collected information about the infant’s mother’s diet during pregnancy. Therefore, infants’ preferences and olfactory responses could have possibly influenced the results in the systematic review.
Five studies showed a positive effect of aroma inhalation on the transition from gavage to oral feeding. Alemdar discovered a significant difference in terms of the average time of transition to oral feeding among four groups (voice group, breast milk odor, incubator cover group, and control group). According to the post hoc analysis, the difference is attributed to the breast milk odor (group feeding) (P<0.05) [18]. In the study of Iranmanesh et al. in comparison to infants in the control group, preterm infants in the aromatherapy group with pad impregnated with milk group switched from tube feeding to oral feeding 10 days earlier (P<0.001) [3].
As reported by Yildiz et al. preterm infants transitioned from tube feeding (gavage) to oral feeding 3 days earlier in the groups receiving pads soaked in breast milk (P=0.03) [15]. In Beker et al.’s study, infants reached full enteral feeds at a shorter time (13.5 days) after milk smell and taste compared to the control group (15.5 days) with an adjusted hazard ratio of 1.63 0.91–2.91 and P=0.10 [17]. In the study of Ali Ahmed, the mother’s breast sucking was initiated earlier in the breast milk odor group than in the control group (P<0.001) [14]. Two studies have reported borderline significant results. According to Davidson et al., infants in the sham intervention group and mother’s own milk infants were not different in terms of improved oral feeding skills. However, preterm infants responded differently to mothers’ own milk based on gestational age (31
Our meta-analysis shows that preterm infants transitioned from tube feeding (gavage) to oral feeding earlier in the groups stimulated milk breast odors.
Breastfeeding behavior may be the reason our meta-analysis shows that preterm infants transitioned from tube feeding (gavage) to oral feeding earlier in the groups stimulated by milk breastfeeding odors. The odor of mother’s milk was found to affect on breastfeeding behavior of premature neonates. In Raimbault’s study, infants in the milk-odor group showed longer sucking bouts and more bursts consisting of >7 sucking movements in comparison to control infants [21]. In the study of Porter et al., the odor of fresh breast milk at week 36 significantly increased sucking movements compared to both water (P<0.005) and pooled donor milk (P<0.005) as opposed to infants in the control group. The frequency of sucking in response to fresh breast milk was also higher than that of frozen breast milk, but the difference was not statistically significant (P=0.09). Both frozen breast milk and pooled donor milk showed a higher rate of sucking compared to water trials (P<0.05). However, the conditions of frozen breast milk and pooled donor milk were not different in the sucking behavior [22]. In the study of Meza et al., the frequency of high-amplitude non-nutritive sucking was greater in the maternal breast odor group than in the control group (no odor) [4].
The reported literature showed controversial findings regarding sex differences in response to environmental stimuli [23, 24]. In a study by Davidson et al. [16], no sex differences were found in response to aroma inhalation with breastfeeding on the transition from gavage to oral feeding. In addition, premature newborns with <31 weeks gestation learned to feed sooner when stimulated with the mother’s own milk than the control group [16]. However, the authors concluded that their findings should be interpreted with caution small sample size.
Conclusion
Our meta-analysis supports the use of breast milk odor as a safe, noninvasive, and shorter time reach to oral feeds in preterm infants. It costs only commented to health providers to develop such family-friendly interventions that incorporate parents, have an active and important role in providing care to their premature infants
Ethical Considerations
Compliance with ethical guidelines
All ethical principles are considered in this article.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization, project administration, and funding acquisition: Masumeh Ghazanfarpour, Malihe Afiat, Sara Saadat, Eghlima Jalaly and Saeed Soleimany; Methodology: Masumeh Ghazanfarpour, Fatemeh Abdi, Sara Saadat, Eghlima Jalaly and Saeed Soleimany; Software: Eghlima Jalaly, Malihe Afiat and Masumeh Ghazanfarpour; Validation and supervision: Masumeh Ghazanfarpour and Sara Saadat; Formal analysis: Masumeh Ghazanfarpour, Fatemeh Abdi, Malihe Afiat and Saeed Soleimany; Investigation: Eghlima Jalaly, Malihe Afiat and Sara Saadat; Resources: Masumeh Ghazanfarpour, Fatemeh Abdi and Eghlima Jalaly; Data curation, Masumeh Ghazanfarpour, Malihe Afiat and Fatemeh Abdi; Writing the original draft: Eghlima Jalaly, Masumeh Ghazanfarpour and Sara Saadat; Review and editing: All authors.
Conflicts of interest
The authors declared no conflict of interest.
References
- Neshat H, Jebreili M, Seyyedrasouli A, Ghojazade M, Hosseini MB, Hamishehkar H. Effects of breast milk and vanilla odors on premature neonate's heart rate and blood oxygen saturation during and after venipuncture. Pediatr Neonatol. 2016; 57(3):225-31. [DOI:10.1016/j.pedneo.2015.09.004] [PMID]
- Selina Ho, Saroj Saigal. Current survival and early outcomes of infants of borderline viability. Neoreviews. 2005; 6(3):e123–32. [DOI:10.1542/neo.6-3-e123]
- Iranmanesh S, Shamsi A, pour Aboli B, Movahedi Z. The effect of breast milk odor on transition time from gavage to oral feeding and hospital stay in premature infants. ICAN: Infant, Child, & Adolescent Nutrition. 2015; 7(1):5-11. [DOI:10.1177/1941406414563390]
- Meza CV, Powell NJ, Covington C. The influence of olfactory intervention on non-nutritive sucking skills in a premature infant. The Occupational Therapy Journal of Research. 1998; 18(3):71-83. [DOI:10.1177/153944929801800301]
- Khodagholi Z, Zarifian T, Soleimani F, Khoshnood Shariati M, Bakhshi E. The effect of non-nutritive sucking and maternal milk odor on the independent oral feeding in preterm infants. Iran J Child Neurol. 2018; 12(4):55-64. [PMID]
- Cao Van H, Guinand N, Damis E, Mansbach AL, Poncet A, Hummel T, et al. Olfactory stimulation may promote oral feeding in immature newborn: A randomized controlled trial. Eur Arch Otorhinolaryngol. 2018; 275(1):125-9. [DOI:10.1007/s00405-017-4796-0] [PMID]
- Pinelli J, Symington AJ. Non-nutritive sucking for promoting physiologic stability and nutrition in preterm infants. Cochrane Database Sys Rev. 2005; 4(4):CD001071. [DOI:10.1002/14651858.CD001071.pub2]
- Bingham PM, Abassi S, Sivieri E. A pilot study of milk odor effect on nonnutritive sucking by premature newborns. Arch Pediatr Adolesc Med. 2003; 157(1):72-5. [PMID]
- Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. Chicheste: John Wiley & Sons; 2008. [Link]
- Lempesi E, Koletsi D, Fleming PS, Pandis N. The reporting quality of randomized controlled trials in orthodontics. J Evid Based Dent Pract. 2014; 14(2):46-52. [DOI:10.1016/j.jebdp.2013.12.001] [PMID]
- Marino LV, Venkatesh P, Ho A, Beattie RM, Bharucha T. Hypophosphataemia in infants with CHD treated with amino acid infant formula. Cardiol Young. 2018; 28(11):1370-4. [DOI:10.1017/S1047951118001324] [PMID]
- Mirzaei M, Amirajam S, Moghimi ES, Behzadi S, Rohani A, Zerangian N, et al. The effects of hydroxychloroquine on pregnancy outcomes in infertile women: A systematic review and meta-analysis. J Med Life. 2023; 16(2):189-94. [DOI:10.25122/jml-2022-0095] [PMID]
- Schriever VA, Gellrich J, Rochor N, Croy I, Cao-Van H, Rüdiger M, et al. Sniffin' away the feeding tube: The influence of olfactory stimulation on oral food intake in newborns and premature infants. Chem Senses. 2018; 43(7):469-74. [DOI:10.1093/chemse/bjy034] [PMID]
- Ali Ahmed F. Breast milk odor effect on weight gain, first breastfeeding time and length of hospital stay in premature infants. J Nurs Health Sci. 2019; 8(3):42-9. [DOI: 10.9790/1959-0803034249]
- Yildiz A, Arikan D, Gözüm S, Taştekın A, Budancamanak I. The effect of the odor of breast milk on the time needed for transition from gavage to total oral feeding in preterm infants. J Nurs Scholarsh. 2011; 43(3):265-73. [DOI:10.1111/j.1547-5069.2011.01410.x] [PMID]
- Davidson J, Ruthazer R, Maron JL. Optimal Davidson J, Ruthazer R, Maron JL. Optimal timing to utilize olfactory stimulation with maternal breast milk to improve oral feeding skills in the premature newborn. Breastfeed Med. 2019; 14(4):230-5. [DOI:10.1089/bfm.2018.0180] [PMID]
- Beker F, Opie G, Noble E, Jiang Y, Bloomfield FH. Smell and taste to improve nutrition in very preterm infants: A randomized controlled pilot trial. Neonatology. 2017; 111(3):260-6. [DOI:10.1159/000450883] [PMID]
- Alemdar DK. Effect of recorded maternal voice, breast milk odor, and incubator cover on pain and comfort during peripheral cannulation in preterm infants. Appl Nurs Res. 2018; 40:1-6. [DOI:10.1016/j.apnr.2017.12.001] [PMID]
- Muelbert M, Lin L, Bloomfield FH, Harding JE. Exposure to the smell and taste of milk to accelerate feeding in preterm infants. Cochrane Database Syst Rev. 2019; 7(7):CD013038. [DOI:10.1002/14651858.CD013038.pub2] [PMID]
- Schaal B, Marlier L, Soussignan R. Human foetuses learn odours from their pregnant mother's diet. Chem Senses. 2000; 25(6):729-37. [DOI:10.1093/chemse/25.6.729] [PMID]
- Raimbault C, Saliba E, Porter RH. The effect of the odour of mother's milk on breastfeeding behaviour of premature neonates. Acta Paediatr. 2007; 96(3):368-71. [DOI:10.1111/j.1651-2227.2007.00114.x] [PMID]
- Porter RH, Raimbault C, Henrot A, Saliba E. Responses of pre-term infants to the odour of mother’s milk. In: Hurst JL, Beynon RJ, Roberts SC, Wyatt TD, editors. Chemical signals in vertebrates 11. New York: Springer; 2008. [DOI:10.1007/978-0-387-73945-8_32]
- Cheng TS, Loy SL, Cheung YB, Chan JK, Pang WW, Godfrey KM, et al. Sexually dimorphic response to feeding mode in the growth of infants. Am J Clin Nutr. 2016; 103(2):398-405. [DOI:10.3945/ajcn.115.115493] [PMID]
- Cheng TS, Kwok MK, Leung GM, Schooling CM. The associations of breast feeding with infant growth and body mass index to 16 years: 'Children of 1997'. Paediatr Perinat Epidemiol. 2018; 32(2):200-9. [DOI:10.1111/ppe.12434] [PMID]
Type of Study: Review Article |
Subject:
Pediatrics
Received: 2023/07/29 | Accepted: 2023/12/1 | Published: 2024/01/1
Received: 2023/07/29 | Accepted: 2023/12/1 | Published: 2024/01/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






