Volume 12, Issue 1 (1-2024)
J. Pediatr. Rev 2024, 12(1): 27-40 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Varvani Farahani P, Öztürk C. Investigating the Effects of COVID-19 on the World Trend of Childhood Vaccination: A Systematic Review. J. Pediatr. Rev 2024; 12 (1) :27-40
URL: http://jpr.mazums.ac.ir/article-1-568-en.html
URL: http://jpr.mazums.ac.ir/article-1-568-en.html
1- Department of Nursing, Faculty of Health Science, Cyprus International University, Nicosia, Turkish Republic of Northern Cyprus (TRNC). , 20222948@std.neu.edu.tr
2- Faculty of Nursing, Near East University, Nicosia, Turkish Republic of Northern Cyprus (TRNC).
2- Faculty of Nursing, Near East University, Nicosia, Turkish Republic of Northern Cyprus (TRNC).
Full-Text [PDF 1645 kb]
(1049 Downloads)
| Abstract (HTML) (2826 Views)
Full-Text: (843 Views)
Introduction
Vaccination stands as a cornerstone in the edifice of public health, playing a pivotal role in mitigating the spread of infectious diseases and averting their potentially severe consequences [1]. The development and health of youngsters are positively impacted by vaccinations. According to data released by the World Health Organization (WHO), pediatric immunization prevents 2.5 million deaths globally each year in children under the age of five [2]. As we confront new public health challenges and infectious agents, the continued importance of vaccination in preserving the well-being of populations cannot be overstated [3]. The global coronavirus disease 2019 pandemic, which began as a localized outbreak in December 2019, has over 634 million confirmed cases and around 6.6 million fatalities as of November 2022 [4, 5]. Early in 2020, when SARS-CoV-2 spread quickly worldwide and governments worked to stop the spread, many health systems, including regular immunization, experienced major interruptions. These impacts were a result of several variables, including travel restrictions and laws intended to limit interaction and socializing, cancellation or postponement of patient appointments, as well as the deployment of medical staff for the COVID-19 reaction due to viral exposure worries [6-8]. The COVID-19 pandemic has significantly impacted public health, economic systems, socio-cultural patterns, and political institutions. Negative effects include halting routine vaccination programs due to resource demands and quarantine measures. Uptake is impacted for older children, while positive effects include influencing people’s perceptions of vaccination [9]. WHO recently performed a national pulse survey with 135 participating nations; accordingly, 94% of the respondent countries suffered an interruption of essential healthcare services from January to March 2021 [10]. The suspension of immunization programs in more than 68 countries has put at least 80 million infants under the age of one in danger, according to information compiled by the WHO, UNICEF, and the Sabin Vaccine Institute [1, 12]. In addition, the WHO estimates that the COVID-19 pandemic prevented 23 million youngsters from receiving their immunizations in 2020 [13]. Between January to December 2020, a total of 30.0 million children failed to receive the third dose of the diphtheria, tetanus, and pertussis vaccination, and 27.2 million youngsters failed to receive the first dose of the vaccine that contained measles [14]. In Pakistan and Afghanistan, there have been several reports of polio and diphtheria [15, 16], and instances of illnesses that may be prevented by vaccination, such as measles, diphtheria, and pertussis, have increased outbreaks that are making headlines. Measles cases are increasing globally [17, 18]. These outbreaks serve as a stark reminder that public health concerns are just as important, if not more, during pandemics. The significance of preserving vital health services, including vaccination, has been emphasized by drawing on analyses of historical and epidemiological data as well as information from current modeling efforts [19]. One of the most efficient and affordable public health programs that might lower the rates of morbidity and death for illnesses that can be prevented by vaccination is childhood immunization [20]. In this article, we discuss probable COVID-19 pandemic consequences on global immunization rates as well as possible causes. The findings of this study offer insight into how pandemics affect existing immunization efforts and help to design policies for effective future pandemics and other crisis preparations.
Methods
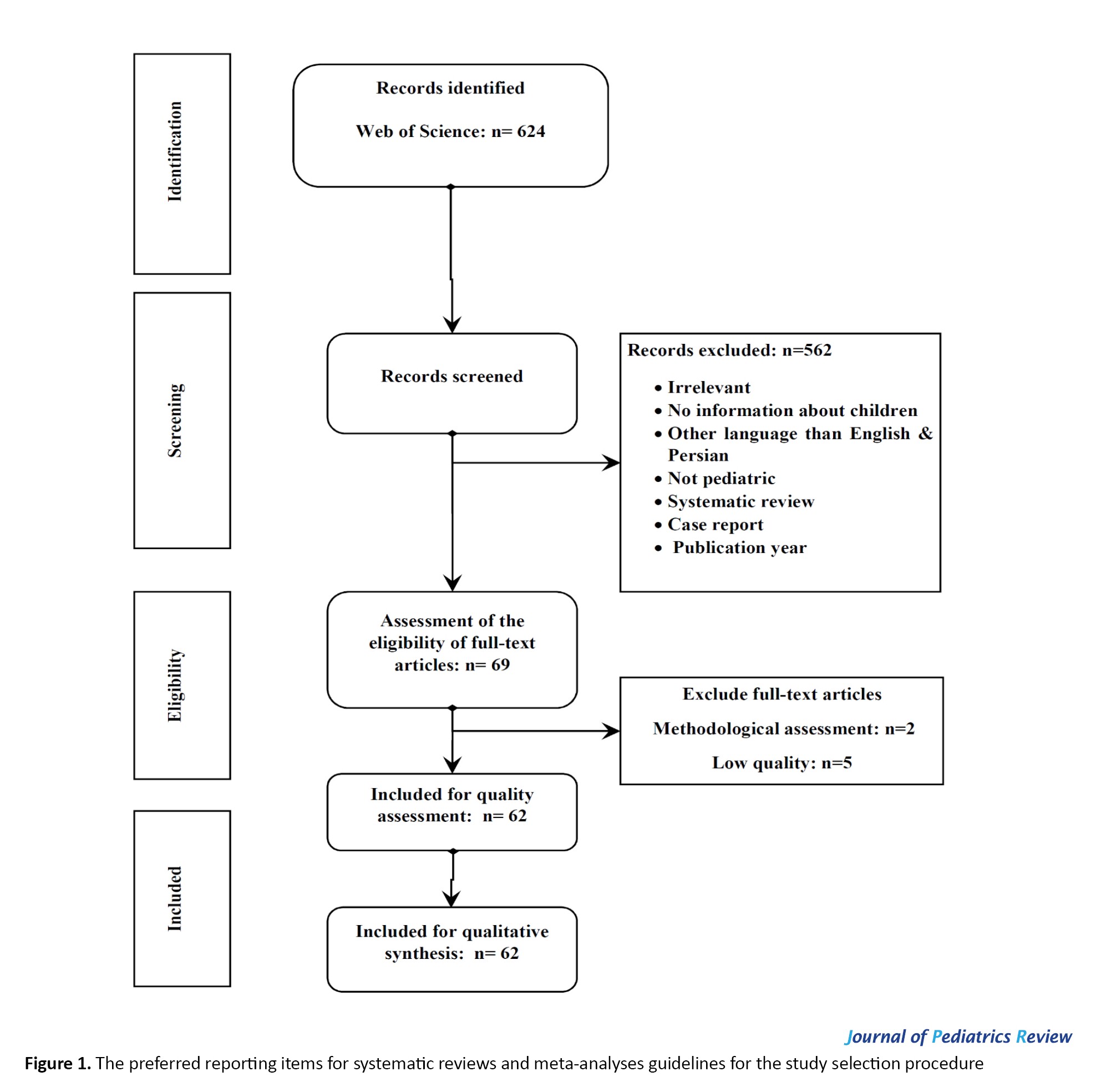
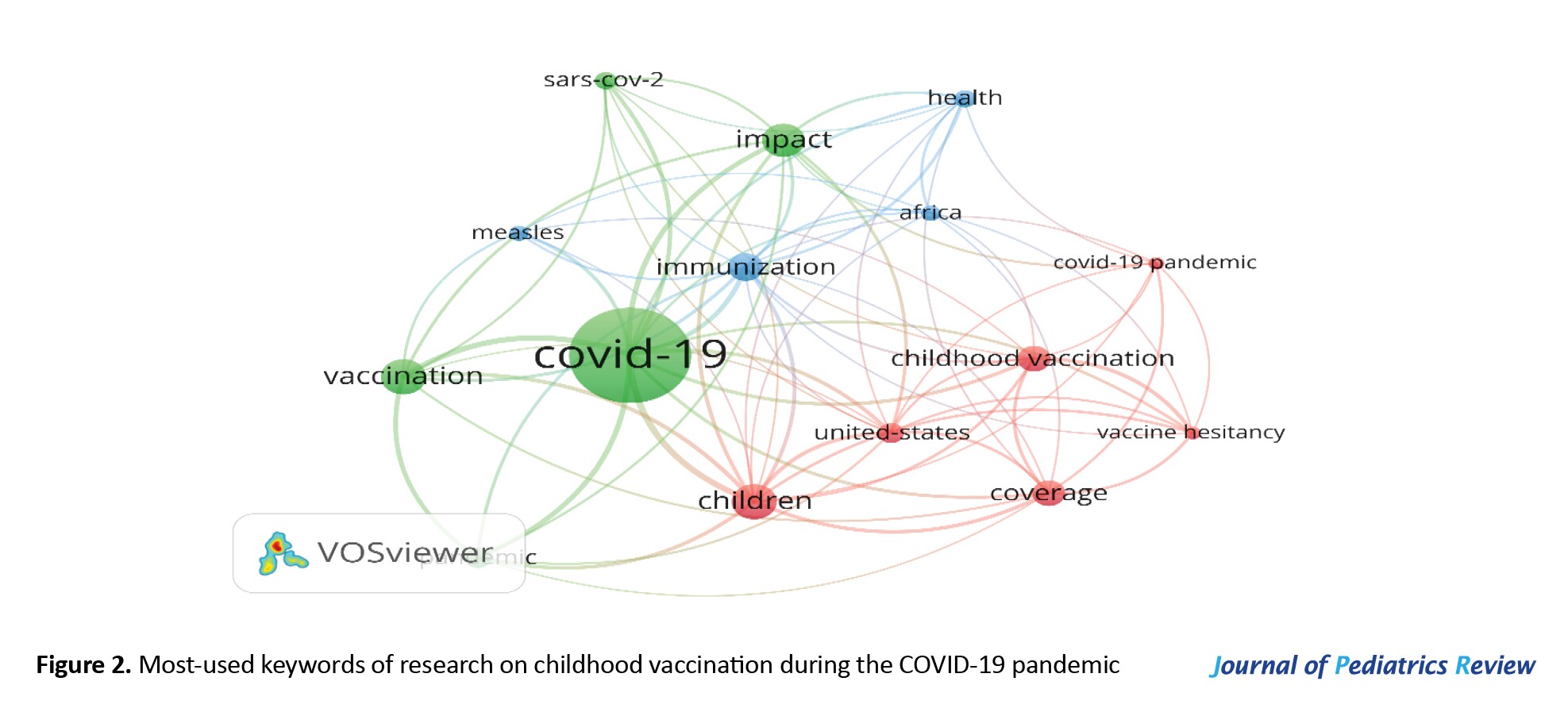
It is necessary to assess the field’s cumulative advancements and keep track of the current level of knowledge in this area because of the rising volume of literature on COVID-19 and childhood vaccination. We used the preferred reporting items for systematic reviews and meta-analyses checklist to ensure that the systematic review’s reporting was of high quality [21], which is available at “PRISMA” the checklist, which includes four sequential processes (identification, screening, eligibility, and inclusion) and 27 elements, is intended to help writers perform more effective systematic reviews (Figure 1). In addition, the scientific literature was visualized and analyzed using VOSviewer software, version 1.6.17 for bibliometric research.
Search technique
From January 1, 2020, to July 13, 2023, a comprehensive search of pertinent literature was conducted on the Web of Science. The keywords used in English were TS=([“SARS-CoV-2” OR “COVID-19” OR “coronavirus”] AND [“pediatric immunization” OR “childhood vaccination” OR “vaccine coverage”]). The initial search yielded 624 articles, out of which 569 were removed for not meeting the inclusion criteria, leaving 62 articles for analysis. Downloads were made of the full record and cited references for these publications. Next, we use them as input data for our VOSviewer-based bibliometric analysis and science mapping. The main applications of VOSviewer in this review research were the analysis of word co-occurrences, citations, and bibliographies.
Inclusion criteria
The inclusion criteria comprised the following items: 1) Clinical trials, observational, quasi-experimental, and qualitative studies; 2) Studies investigating the worldwide effects of COVID-19 on childhood immunization; 3) Studies reporting on vaccination coverage rates, vaccine hesitancy, missed or delayed vaccinations, catch-up immunization efforts, and disruptions to routine immunization programs; 4) Articles published from 2020 to 2023 in English; and 5) Studies that had a code of ethics.
Exclusion criteria
The exclusion criteria were as follows: 1) A lack of access to full texts; 2) Individual case reports, systematic reviews, and meta-analyses; and 3) Unrelated objectives. The preferred reporting items for systematic reviews and meta-analysis guidelines were followed to ensure a rigorous and transparent review process.
Quality assessment of the articles
A critical appraisal was performed according to the study design of the articles. The critical appraisal skills program was used for the analysis. To ensure consistency and reliability in the critical appraisal process, two independent reviewers conducted the assessments. Any discrepancies in their evaluations were resolved through consensus, guaranteeing a thorough and unbiased analysis.
Extraction of the data
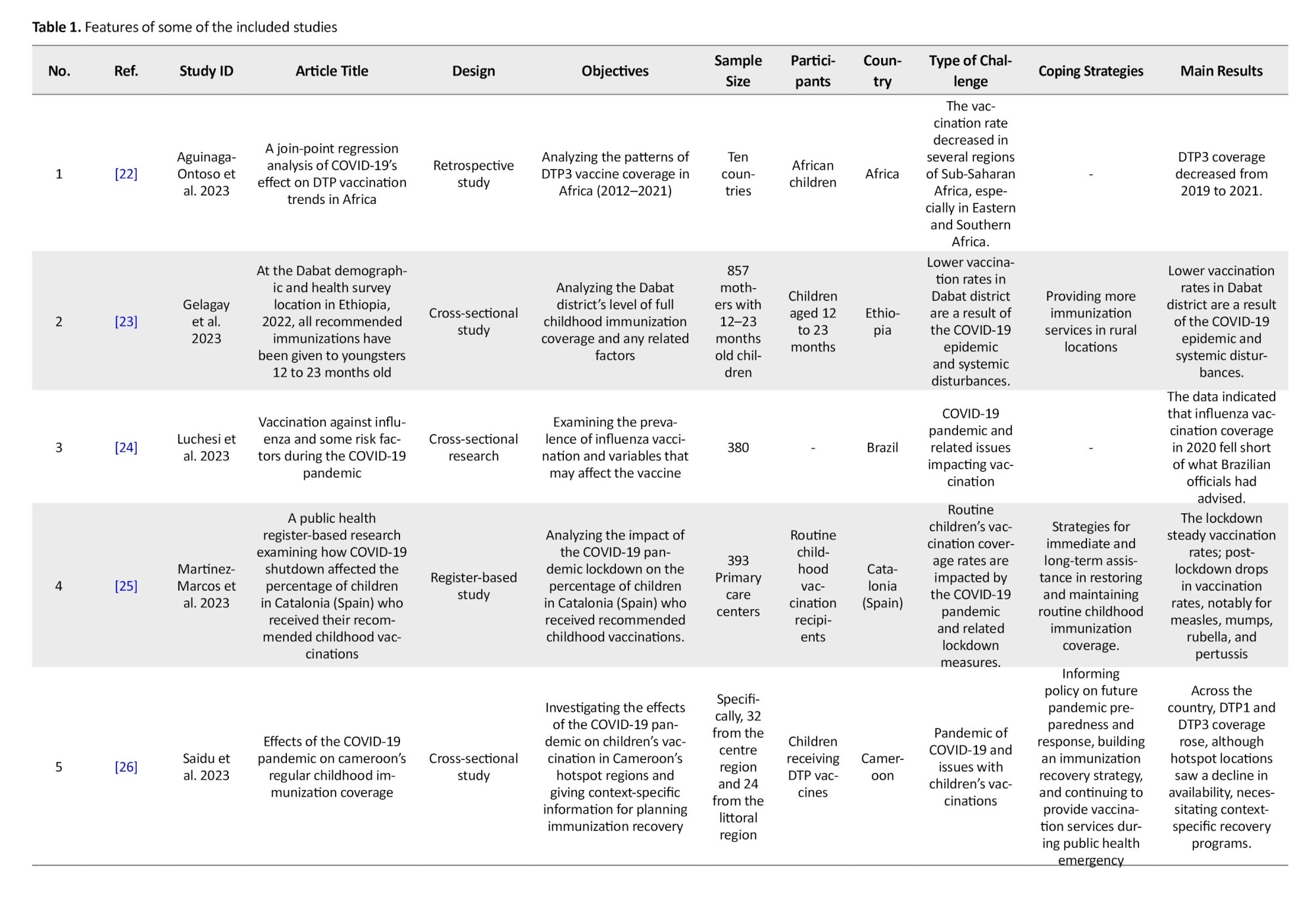
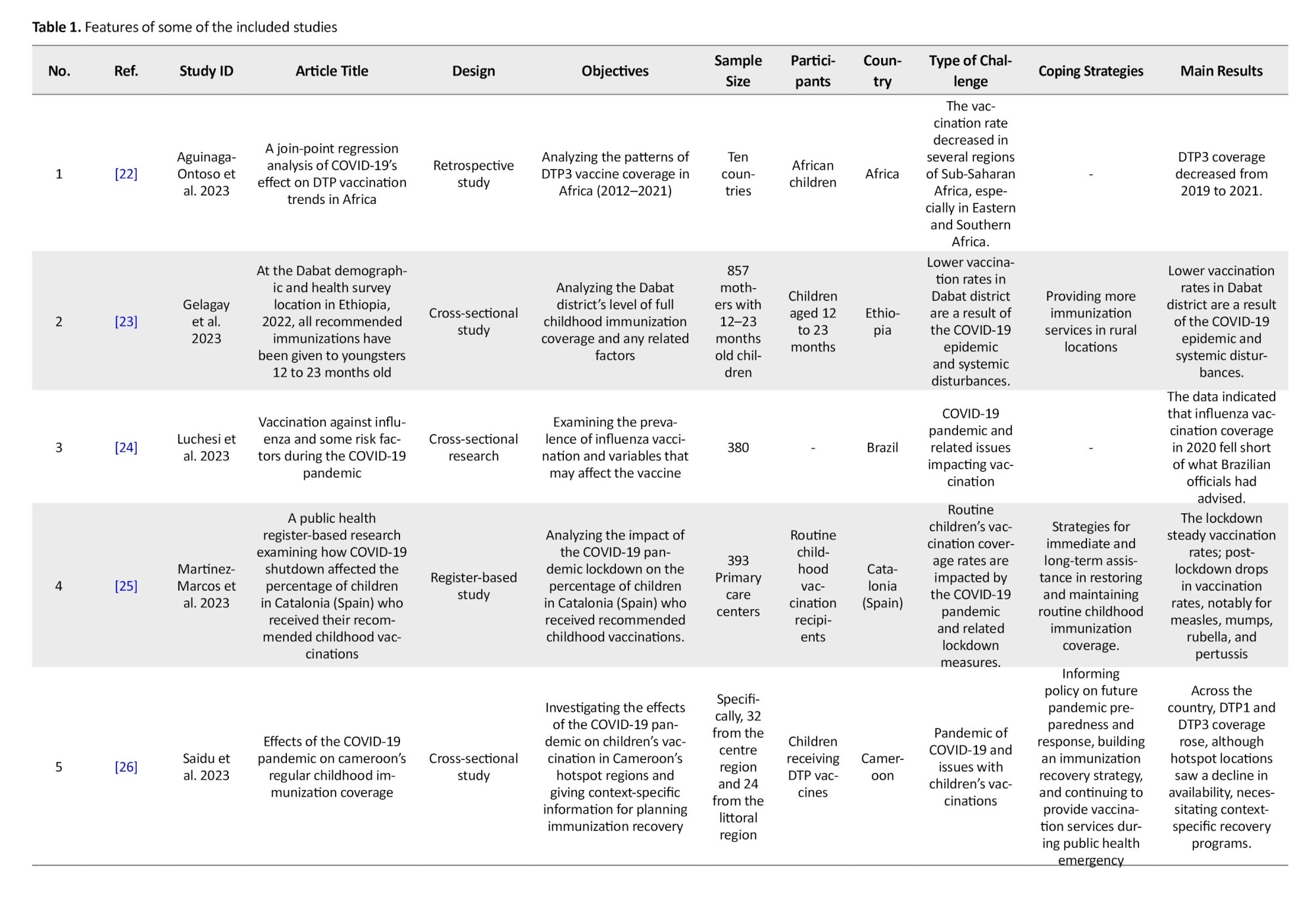
The preferred reporting items for systematic reviews and meta-analysis guidelines were followed to ensure a rigorous and transparent review process. To ensure comprehensive coverage of relevant articles, a thorough manual search of relevant publications was conducted. The screening process was carried out using EndNote software, version 7.7.1. Data was extracted from the final set of included full texts, encompassing information such as the first author, publication year, research design, geographic location, objectives, sample size, age range of children included, changes in vaccination coverage rates, coping strategies, and key results related to the effect of COVID-19 on the global trend of childhood immunization (Table 1).
Questions and research objectives
This study conducted a systematic review and bibliometric analysis to investigate the impact of COVID-19 on the global trend of child immunization in light of the rapidly expanding requirements during the pandemic. To address the difficulties in maintaining children’s vaccination rates throughout the pandemic, the goal was to develop insights into important research issues, tactics, and policies. The available literature from 2020 to 2023 was analyzed using statistical approaches. The following research questions were utilized in our bibliometric analysis to examine the effect of COVID-19 on childhood immunization:
How have worldwide child immunization rates been impacted by the COVID-19 pandemic?
In terms of publications published and citations, what was the yearly frequency of research on the worldwide trend of child immunization during the COVID-19 pandemic?
Which representative nations or regions participated in the research on children’s immunizations for COVID-19?
During the COVID-19 pandemic, what terms were most often used in studies on child immunization?
Results
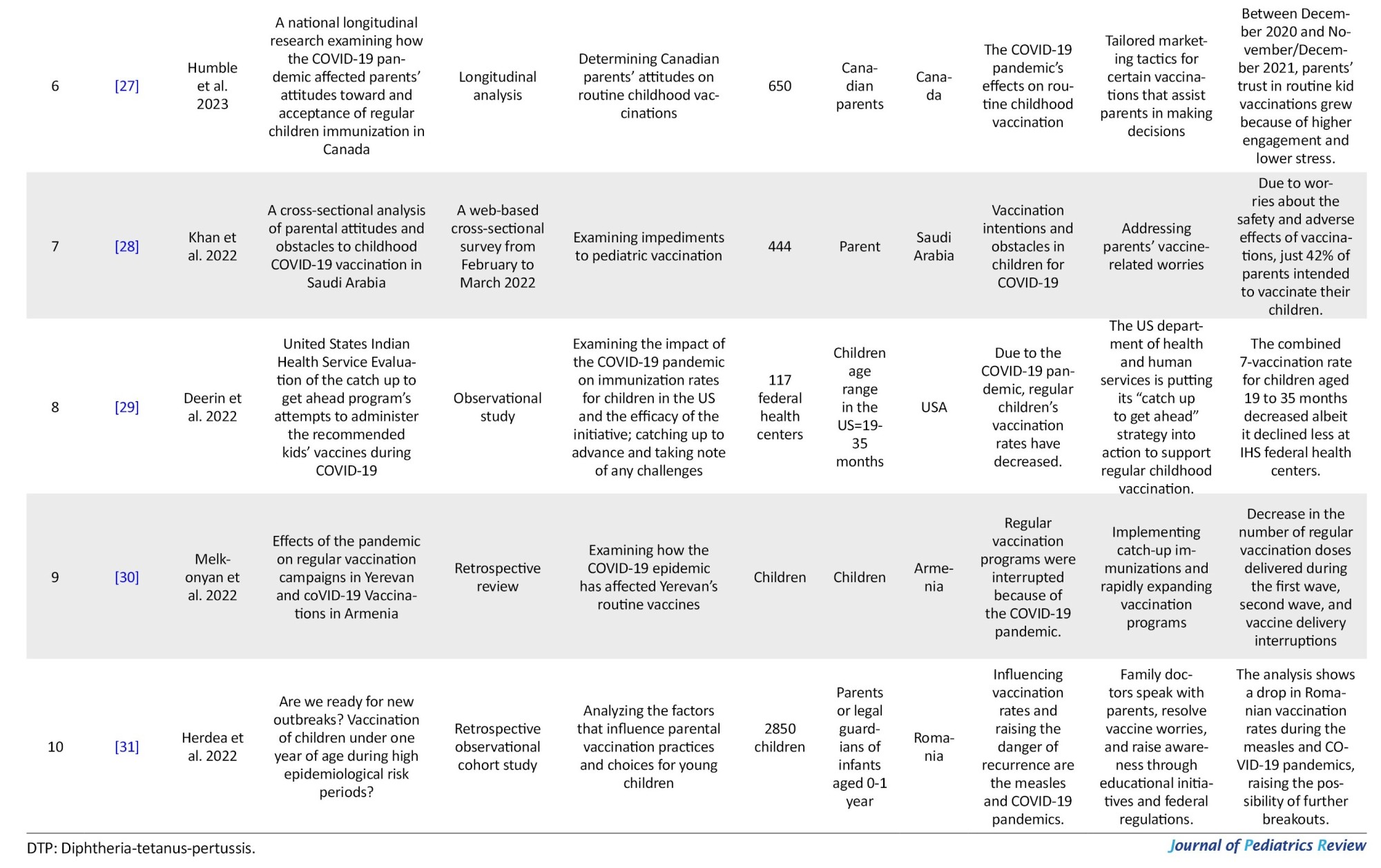
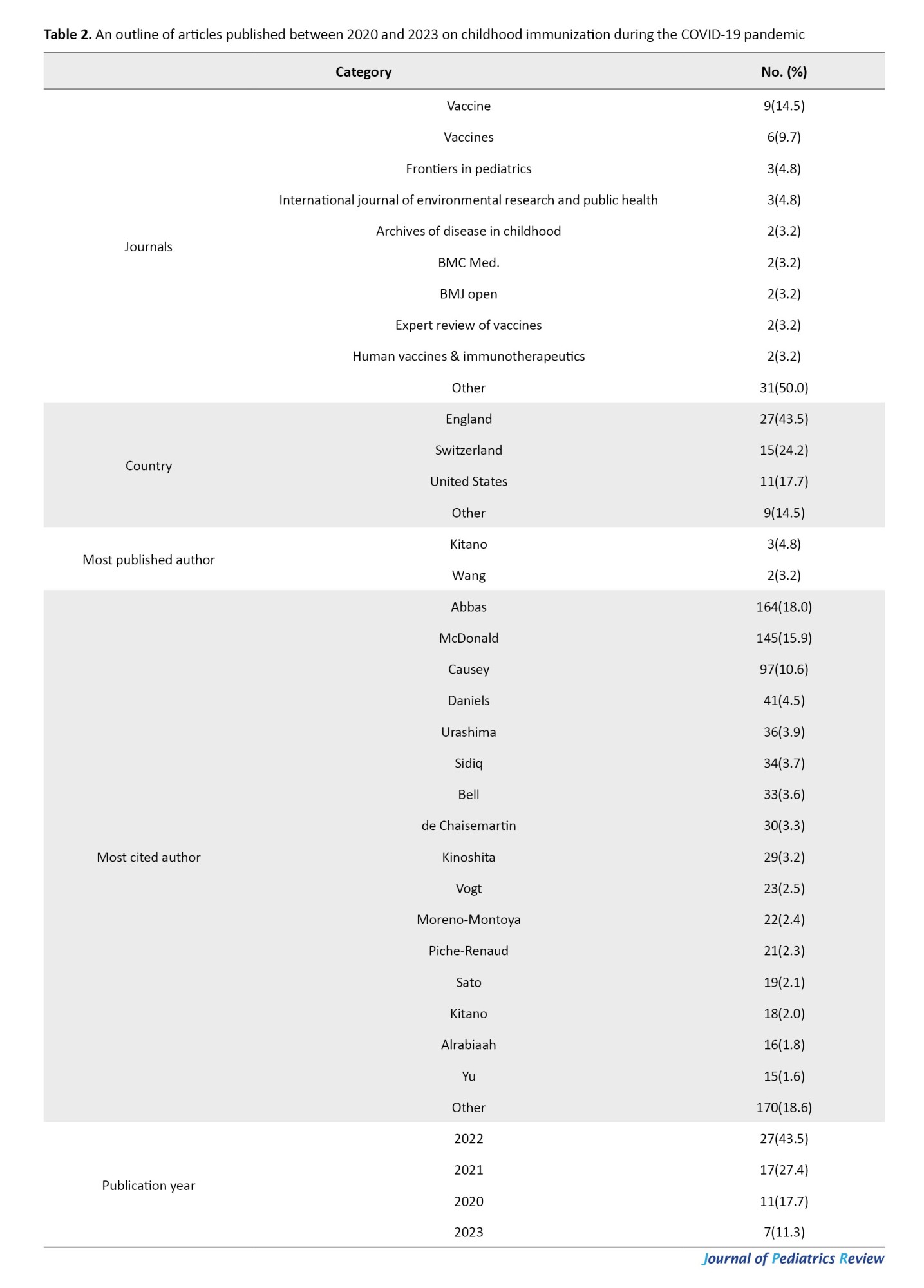
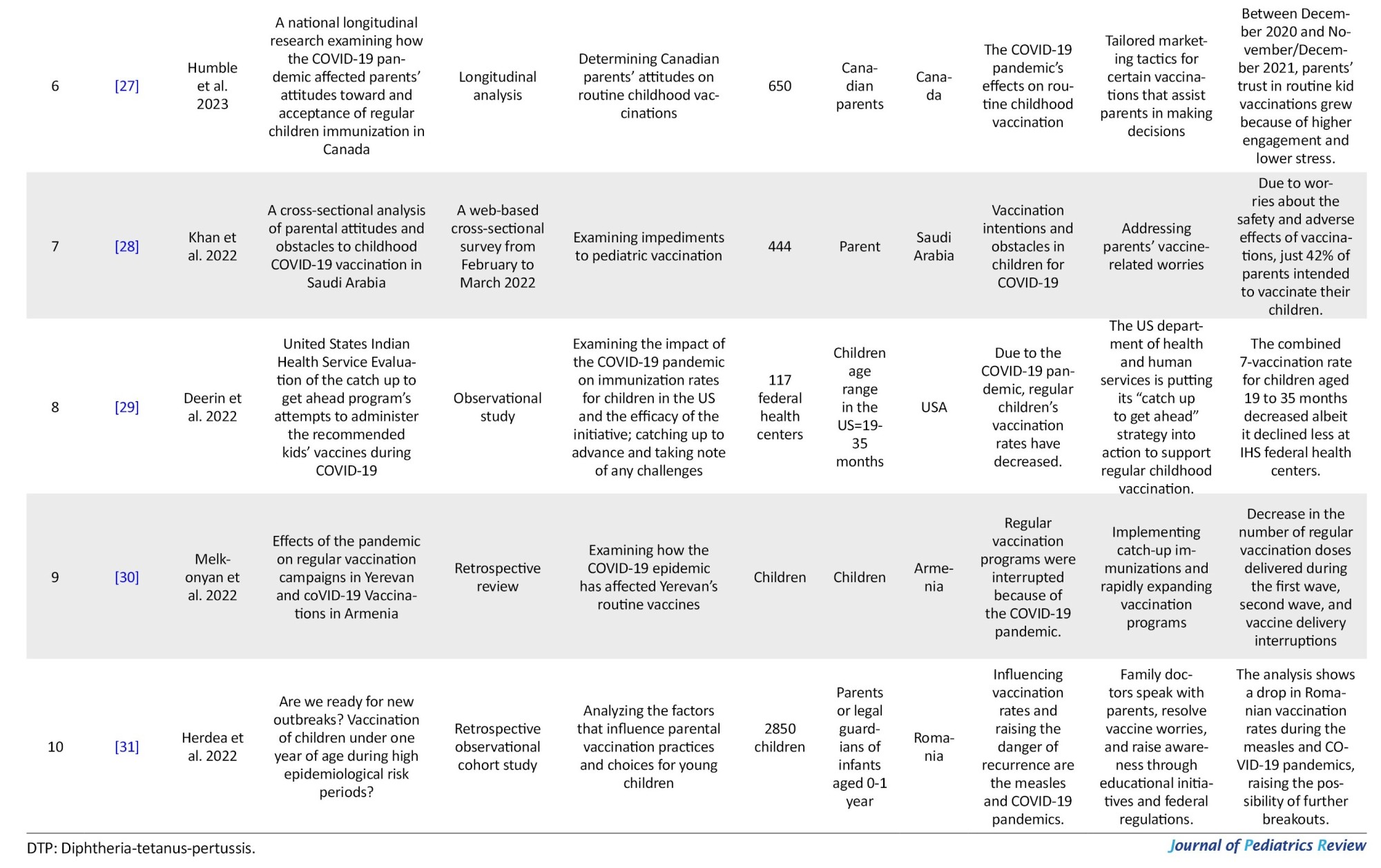
Figure 1 presents an overview of the search strategy’s outcomes. Initially, 624 articles were identified, and after screening, 562 references were excluded. A total of 69 articles met the initial inclusion criteria given their English titles, abstracts, and full texts. The inclusion and exclusion criteria were then carefully reviewed for the full texts of these 69 articles, resulting in the exclusion of 7 papers. Ultimately, 62 papers were included in this study, and their information was systematically extracted from each paper, as presented in Table 1, which includes data on the first author, publication year, research design, geographic location, objectives, sampling size, age range of children included, changes in vaccination coverage rates, coping strategies, and important results relating to the influence of COVID-19 on the global trend of child immunization. From the Web of Science database, a total of 62 items that qualified were discovered. For our bibliometric analysis and scientific mapping with VOSviewer, the full record and cited references of these works were downloaded. In this review research, VOSviewer was primarily used for citation analysis, bibliographic coupling, and word co-occurrence analysis (Table 2).
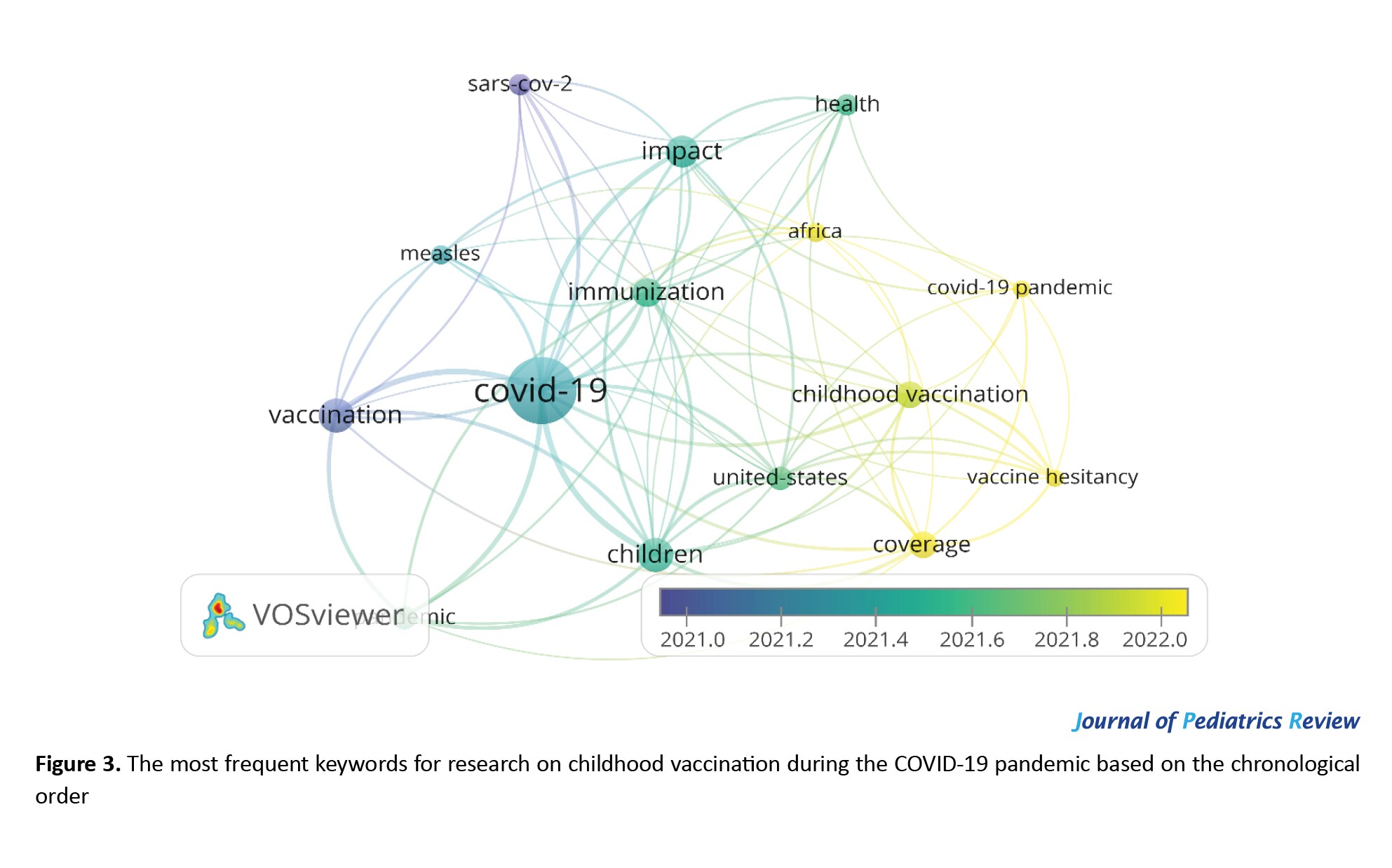
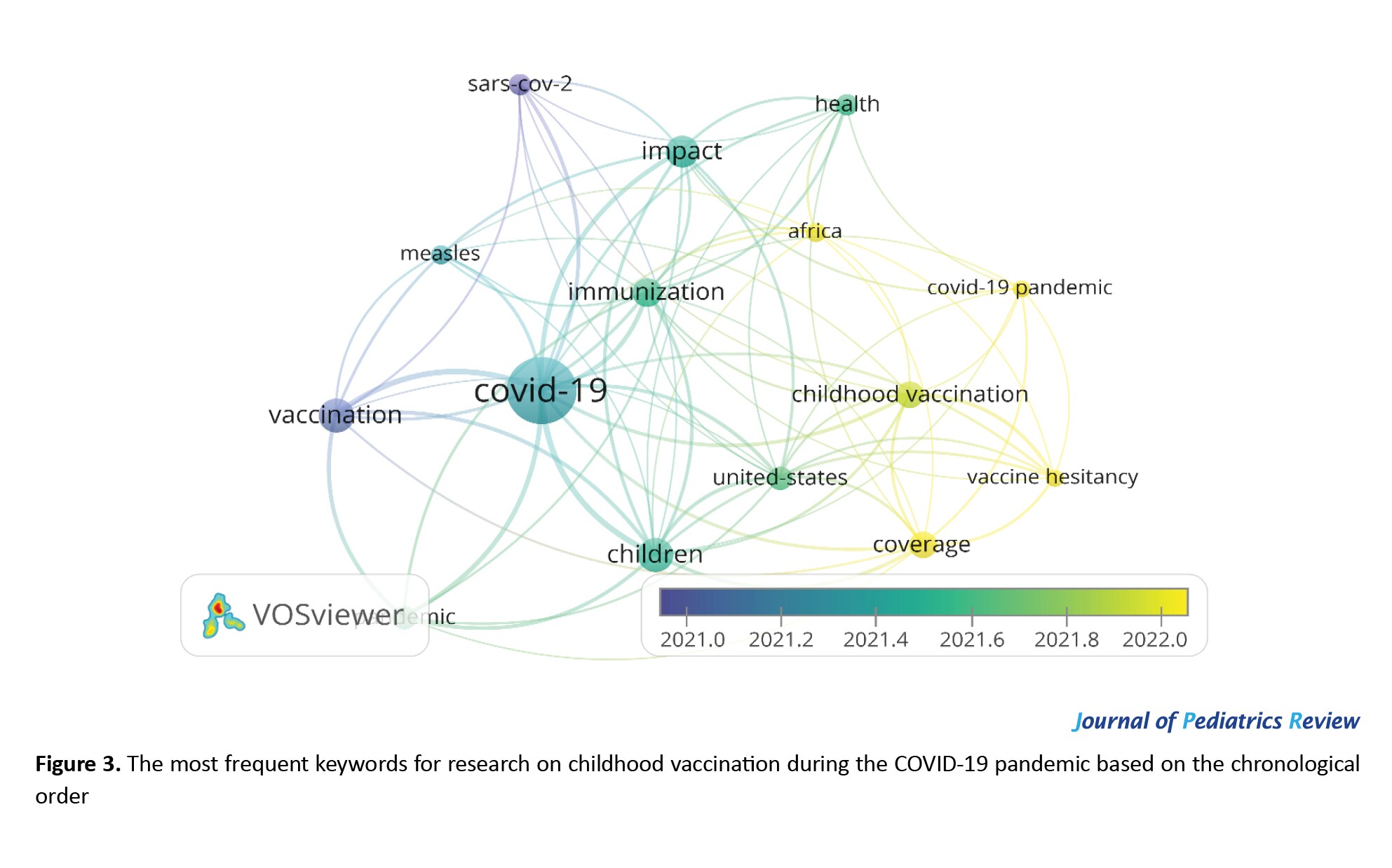
Co-occurrence author keywords
The keywords assisted in finding the most significant information associated with the study topics. The subjects that are most prevalent in publications in a certain field may be ascertained using the co-occurrence analysis of keywords [32]. We conducted a keyword co-occurrence analysis using the VOSviewer. Accordingly, 228 keywords in all were looked up in the Web of Science papers. In the Web of Science database, 15 terms on this subject were displayed more than five times, as shown in Figure 2. COVID-19 is the most used keyword, with 37 repetitions. In the COVID-19 pandemic research, the terms “children,” “vaccination,” “impact,” “coverage education,” and “childhood vaccination” were each used more than 10–14 times. Furthermore, measles was important while considering childhood vaccination during the COVID-19 epidemic, as shown by the observation that it was used as a keyword 6 times. “United States” (used as a keyword 8 times) and Africa (6 times) were also significant. Meanwhile, Figure 2 shows the chronological order of the appearance of words from 2021 to 2022. The following words appeared in the articles in order: Vaccine, COVID-19, children, immunization, United States, childhood vaccination, coverage, and vaccine hesitancy.
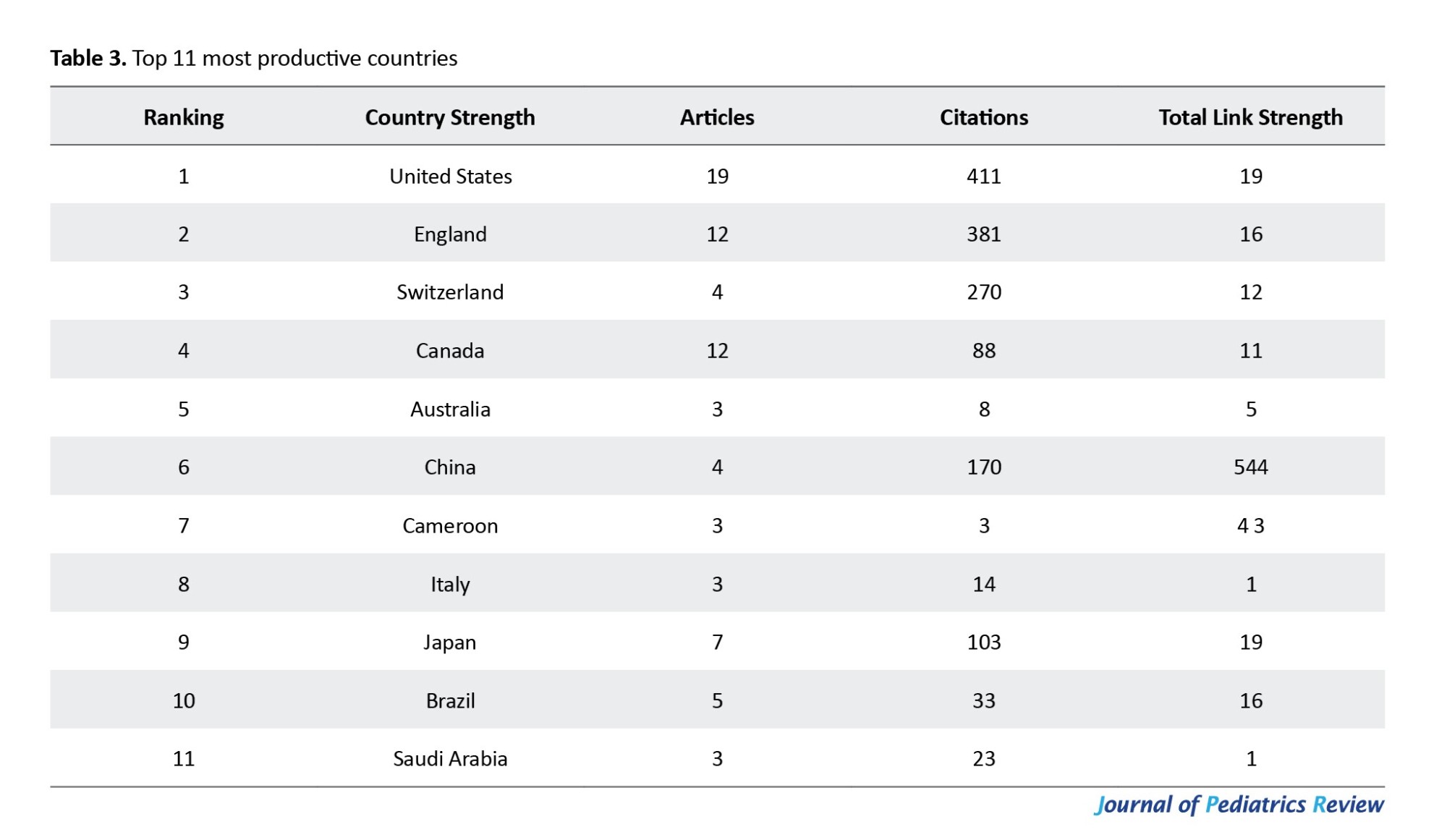
Keyword clustering
We could identify and categorize concepts that were closely connected in the chosen literature because of their arrangement and connections between the main words. Three major groups were identified by the study (Figure 3). The node size reflects the keyword frequency. The strength of connections between nodes is inversely correlated with the thickness of the interconnections between them. The research led to the formation of three groups. The words “COVID-19,” “immunization,” AND “children” had the highest number of links and overall link strength. All three clusters had a total of 74 linkages, with a total link strength of 210. The two terms that predominated cluster 1 (green) were COVID-19 and immunization. The topics in Cluster 2 (blue) were vaccination, measles, Africa, and health. Cluster 3 (red) focused on children, childhood vaccination, coverage, vaccination hesitancy, and the United States, which emerged as highly visible keywords.
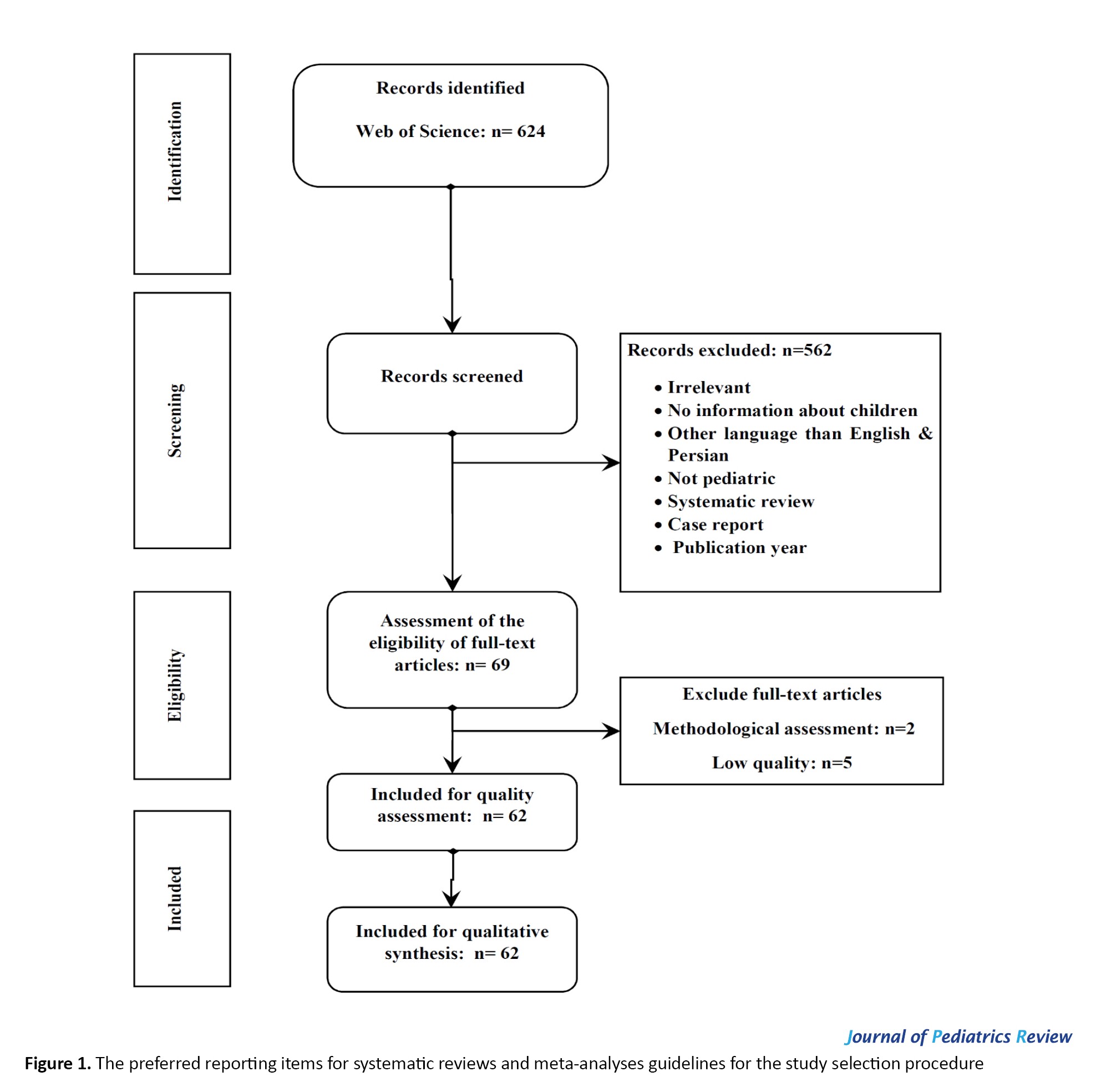
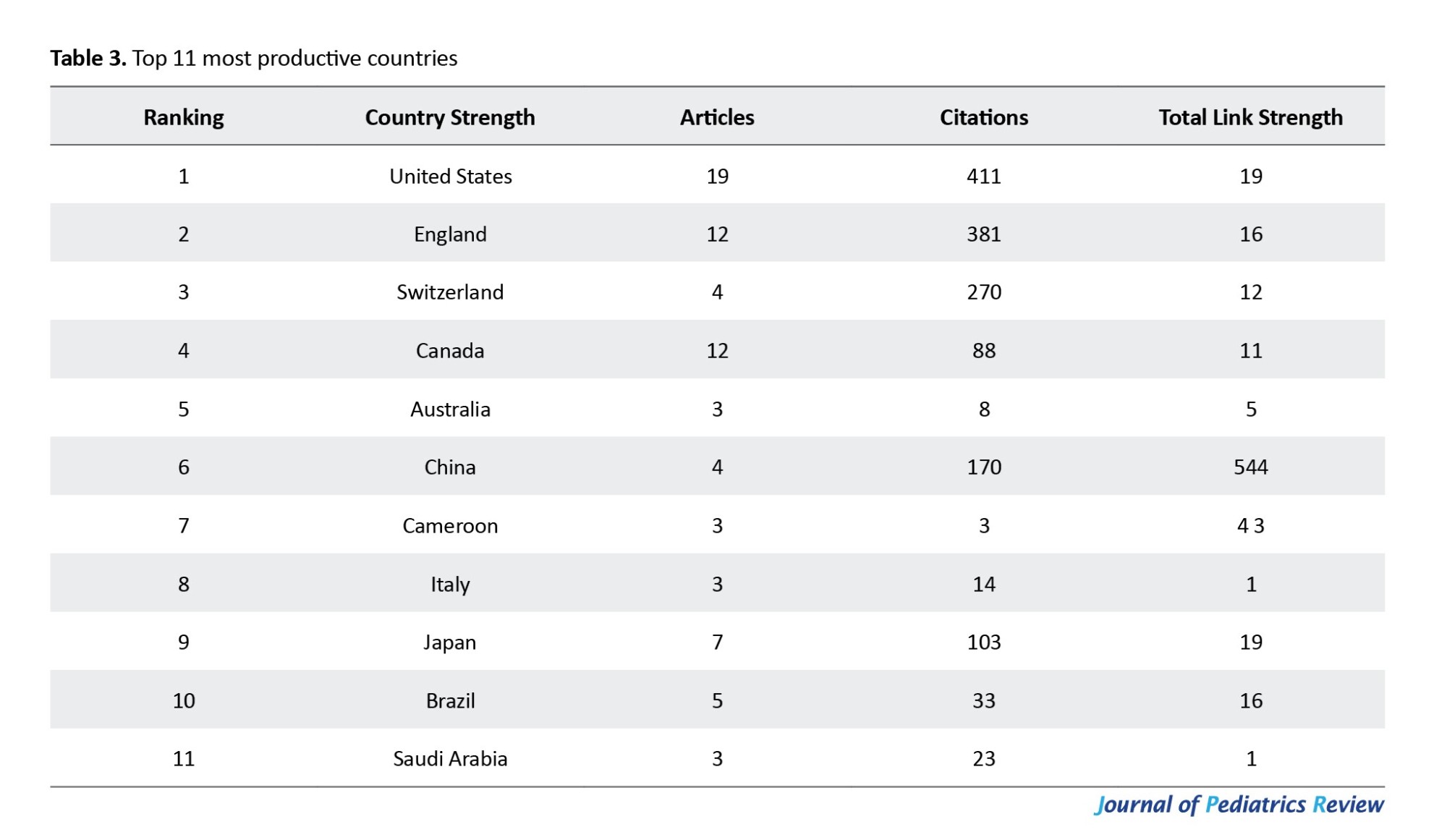
Co-authorship countries/regions
During the COVID-19 epidemic, 47 countries conducted studies on child immunization according to the Web of Science databases. Six countries, including the USA, England, Canada, Switzerland, China, Japan, and Brazil, published more than three publications on the Web of Science databases. The United States and England have made 19 and 12 publications, respectively. The United States and England were the two major countries that demonstrated international cooperation in the field of childhood immunization throughout the COVID-19 epidemic, according to the database (Table 3).
Discussion
This study used the Web of Science databases to analyze several recent publications to identify trends in childhood vaccination research that are connected to the COVID-19 pandemic. To analyze the included studies, descriptive and quantitative statistics were employed. The research papers were examined using the bibliometric approach in terms of article counts, prolific nations and regions, categories, and keyword distributions. According to this study, the COVID-19 pandemic considerably influenced child immunization internationally and caused large pauses in scheduled vaccination programs. The disruptions can be attributed to various factors in the following five categories.
Changes in vaccination coverage rates
Most research indicated that during the COVID-19 pandemic, rates of child immunization coverage significantly decreased [29, 33, 34]. These declines were observed across various vaccines, including routine vaccines such as measles, [25, 35, 36] polio, and diphtheria-tetanus-pertussis [22, 26]. Different nations and regions saw different levels of the reduction, with some locations seeing greater declines in vaccination coverage than others [37-39]. The results of one previous study are in line with this research. Studies indicated that the Southeast Asia and Western Pacific regions, where 18 of the 19(95%) countries included in the study reported disruptions to vaccination, especially infancy and school-entry-age vaccinations [40]. Similar findings were reported in the Spanish Association of Pediatrics (AEP), which also recorded a decline in vaccination coverage (range: 5.0%–60.0%) in March 2020 compared with the monthly average from January 2019 to February 2020 [41]. Similar findings were reported in Pakistan, where a 52.5% decrease was observed in the daily average total number of vaccinations administered from September 2019 to March 2020 [16].
Vaccine hesitancy and parental concerns
The pandemic has amplified vaccine hesitancy [42] and parental concerns [28, 43] regarding the safety and efficacy of vaccines. According to several studies, there was an increase in vaccination reluctance during the COVID-19 pandemic, which was brought on by false information, worry about getting COVID-19 in healthcare facilities, and worries about the quick development of COVID-19 vaccines. These factors have contributed to a reluctance among parents to seek routine immunization services for their children [44].
Missed or delayed vaccinations
The disruptions caused by the pandemic, including lockdown measures and restricted healthcare access, have resulted in missed [45] or delayed vaccinations for many children [45, 46]. Studies reported that children have not been able to receive vaccines according to the recommended schedule, leading to potential gaps in immunity and a greater possibility of illnesses with vaccination protection [47]. Similarly, in a study In England, during the coronavirus disease, the measles-mumps-rubella vaccination started falling in 2020 before the introduction of physical distancing measures implemented in response to the COVID-19 epidemic. In the first 3 weeks of physical distancing, measles-mumps-rubella vaccination counts were 19.8% lower than for the same period in 2019. There was a general decrease in hexavalent vaccinations delivered in 2020 compared with 2019 [48].
Catch-up immunization efforts
Some countries and healthcare systems implemented catch-up immunization strategies to address the gaps in vaccination coverage caused by the pandemic [49]. These strategies involved targeted campaigns, outreach programs, and extended clinic hours to ensure that missed vaccinations are administered and immunization schedules are brought up to date [31].
Disruptions to routine immunization programs
The COVID-19 pandemic has disrupted regular vaccination campaigns throughout the world. Health system challenges, including reallocation of resources [50], a reduced healthcare workforce, and disruptions in vaccine supply chains, have impacted the delivery of immunization services [30]. Additionally, reduced healthcare-seeking behavior and fear of visiting healthcare facilities have further contributed to the disruption of routine immunization programs [51, 52]. The findings highlight the magnitude of the problem, with estimates indicating that millions of infants are now at risk due to the suspension of vaccination services in multiple countries. The pandemic resulted in a substantial number of children missing out on essential vaccines such as the measles-containing vaccination and the diphtheria, tetanus, and pertussis vaccines. Disruptions like this have previously caused epidemics of illnesses like polio, diphtheria, pertussis, and measles that can be prevented by vaccination [31]. The results of some previous studies support our study. One study reported that diphtheria-tetanus-pertussis (DTP) vaccine coverage decreased by 42.0%, oral polio vaccine coverage decreased by 79.0%, and measles vaccine coverage decreased by 9.0% among the school-entry age group [40]. The largest decline was 40.6% for the BCG vaccine [16].
Conclusion
The current review summarizes and analyses the global impact of the COVID-19 pandemic on childhood vaccination. These disruptions included: Disruptions in vaccination coverage, increased hesitancy, missing or delayed vaccinations, compensatory efforts, and disruptions to routine programs. Based on the evidence presented in this review, this coverage compromises immunization and endangers the health of millions of babies worldwide. Urgent action is needed, emphasizing targeted interventions, resilient healthcare systems, and public health awareness. This may help protect children from vaccine-preventable diseases during or after the COVID-19 pandemic. Policymakers and public health officials need to restore disrupted immunization services, implement targeted catch-up vaccination programs, and address vaccine hesitancy through community engagement and tailored awareness campaigns. Strengthening global collaboration, investing in research, and incorporating immunization into crisis preparedness plans are essential steps to safeguard childhood immunization after the COVID-19 pandemic.
Study limitations
This review faced some restrictions. We only found a relatively small number of papers that looked at how the COVID-19 pandemic has affected vaccine coverage, especially those that described the obstacles or other variables that have affected the interruptions from the standpoint of users or providers. We probably missed a large number of non-English publications throughout our search. Furthermore, the existing body of evidence was further constrained by using the inclusion criteria first. The cost of vaccinations and the rules governing immunization have not been examined, nevertheless, as we strive to emphasize the effects of COVID-19 on immunization programs.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The author declared no conflict of interest.
References
Vaccination stands as a cornerstone in the edifice of public health, playing a pivotal role in mitigating the spread of infectious diseases and averting their potentially severe consequences [1]. The development and health of youngsters are positively impacted by vaccinations. According to data released by the World Health Organization (WHO), pediatric immunization prevents 2.5 million deaths globally each year in children under the age of five [2]. As we confront new public health challenges and infectious agents, the continued importance of vaccination in preserving the well-being of populations cannot be overstated [3]. The global coronavirus disease 2019 pandemic, which began as a localized outbreak in December 2019, has over 634 million confirmed cases and around 6.6 million fatalities as of November 2022 [4, 5]. Early in 2020, when SARS-CoV-2 spread quickly worldwide and governments worked to stop the spread, many health systems, including regular immunization, experienced major interruptions. These impacts were a result of several variables, including travel restrictions and laws intended to limit interaction and socializing, cancellation or postponement of patient appointments, as well as the deployment of medical staff for the COVID-19 reaction due to viral exposure worries [6-8]. The COVID-19 pandemic has significantly impacted public health, economic systems, socio-cultural patterns, and political institutions. Negative effects include halting routine vaccination programs due to resource demands and quarantine measures. Uptake is impacted for older children, while positive effects include influencing people’s perceptions of vaccination [9]. WHO recently performed a national pulse survey with 135 participating nations; accordingly, 94% of the respondent countries suffered an interruption of essential healthcare services from January to March 2021 [10]. The suspension of immunization programs in more than 68 countries has put at least 80 million infants under the age of one in danger, according to information compiled by the WHO, UNICEF, and the Sabin Vaccine Institute [1, 12]. In addition, the WHO estimates that the COVID-19 pandemic prevented 23 million youngsters from receiving their immunizations in 2020 [13]. Between January to December 2020, a total of 30.0 million children failed to receive the third dose of the diphtheria, tetanus, and pertussis vaccination, and 27.2 million youngsters failed to receive the first dose of the vaccine that contained measles [14]. In Pakistan and Afghanistan, there have been several reports of polio and diphtheria [15, 16], and instances of illnesses that may be prevented by vaccination, such as measles, diphtheria, and pertussis, have increased outbreaks that are making headlines. Measles cases are increasing globally [17, 18]. These outbreaks serve as a stark reminder that public health concerns are just as important, if not more, during pandemics. The significance of preserving vital health services, including vaccination, has been emphasized by drawing on analyses of historical and epidemiological data as well as information from current modeling efforts [19]. One of the most efficient and affordable public health programs that might lower the rates of morbidity and death for illnesses that can be prevented by vaccination is childhood immunization [20]. In this article, we discuss probable COVID-19 pandemic consequences on global immunization rates as well as possible causes. The findings of this study offer insight into how pandemics affect existing immunization efforts and help to design policies for effective future pandemics and other crisis preparations.
Methods
It is necessary to assess the field’s cumulative advancements and keep track of the current level of knowledge in this area because of the rising volume of literature on COVID-19 and childhood vaccination. We used the preferred reporting items for systematic reviews and meta-analyses checklist to ensure that the systematic review’s reporting was of high quality [21], which is available at “PRISMA” the checklist, which includes four sequential processes (identification, screening, eligibility, and inclusion) and 27 elements, is intended to help writers perform more effective systematic reviews (Figure 1). In addition, the scientific literature was visualized and analyzed using VOSviewer software, version 1.6.17 for bibliometric research.
Search technique
From January 1, 2020, to July 13, 2023, a comprehensive search of pertinent literature was conducted on the Web of Science. The keywords used in English were TS=([“SARS-CoV-2” OR “COVID-19” OR “coronavirus”] AND [“pediatric immunization” OR “childhood vaccination” OR “vaccine coverage”]). The initial search yielded 624 articles, out of which 569 were removed for not meeting the inclusion criteria, leaving 62 articles for analysis. Downloads were made of the full record and cited references for these publications. Next, we use them as input data for our VOSviewer-based bibliometric analysis and science mapping. The main applications of VOSviewer in this review research were the analysis of word co-occurrences, citations, and bibliographies.
Inclusion criteria
The inclusion criteria comprised the following items: 1) Clinical trials, observational, quasi-experimental, and qualitative studies; 2) Studies investigating the worldwide effects of COVID-19 on childhood immunization; 3) Studies reporting on vaccination coverage rates, vaccine hesitancy, missed or delayed vaccinations, catch-up immunization efforts, and disruptions to routine immunization programs; 4) Articles published from 2020 to 2023 in English; and 5) Studies that had a code of ethics.
Exclusion criteria
The exclusion criteria were as follows: 1) A lack of access to full texts; 2) Individual case reports, systematic reviews, and meta-analyses; and 3) Unrelated objectives. The preferred reporting items for systematic reviews and meta-analysis guidelines were followed to ensure a rigorous and transparent review process.
Quality assessment of the articles
A critical appraisal was performed according to the study design of the articles. The critical appraisal skills program was used for the analysis. To ensure consistency and reliability in the critical appraisal process, two independent reviewers conducted the assessments. Any discrepancies in their evaluations were resolved through consensus, guaranteeing a thorough and unbiased analysis.
Extraction of the data
The preferred reporting items for systematic reviews and meta-analysis guidelines were followed to ensure a rigorous and transparent review process. To ensure comprehensive coverage of relevant articles, a thorough manual search of relevant publications was conducted. The screening process was carried out using EndNote software, version 7.7.1. Data was extracted from the final set of included full texts, encompassing information such as the first author, publication year, research design, geographic location, objectives, sample size, age range of children included, changes in vaccination coverage rates, coping strategies, and key results related to the effect of COVID-19 on the global trend of childhood immunization (Table 1).
Questions and research objectives
This study conducted a systematic review and bibliometric analysis to investigate the impact of COVID-19 on the global trend of child immunization in light of the rapidly expanding requirements during the pandemic. To address the difficulties in maintaining children’s vaccination rates throughout the pandemic, the goal was to develop insights into important research issues, tactics, and policies. The available literature from 2020 to 2023 was analyzed using statistical approaches. The following research questions were utilized in our bibliometric analysis to examine the effect of COVID-19 on childhood immunization:
How have worldwide child immunization rates been impacted by the COVID-19 pandemic?
In terms of publications published and citations, what was the yearly frequency of research on the worldwide trend of child immunization during the COVID-19 pandemic?
Which representative nations or regions participated in the research on children’s immunizations for COVID-19?
During the COVID-19 pandemic, what terms were most often used in studies on child immunization?
Results
Figure 1 presents an overview of the search strategy’s outcomes. Initially, 624 articles were identified, and after screening, 562 references were excluded. A total of 69 articles met the initial inclusion criteria given their English titles, abstracts, and full texts. The inclusion and exclusion criteria were then carefully reviewed for the full texts of these 69 articles, resulting in the exclusion of 7 papers. Ultimately, 62 papers were included in this study, and their information was systematically extracted from each paper, as presented in Table 1, which includes data on the first author, publication year, research design, geographic location, objectives, sampling size, age range of children included, changes in vaccination coverage rates, coping strategies, and important results relating to the influence of COVID-19 on the global trend of child immunization. From the Web of Science database, a total of 62 items that qualified were discovered. For our bibliometric analysis and scientific mapping with VOSviewer, the full record and cited references of these works were downloaded. In this review research, VOSviewer was primarily used for citation analysis, bibliographic coupling, and word co-occurrence analysis (Table 2).
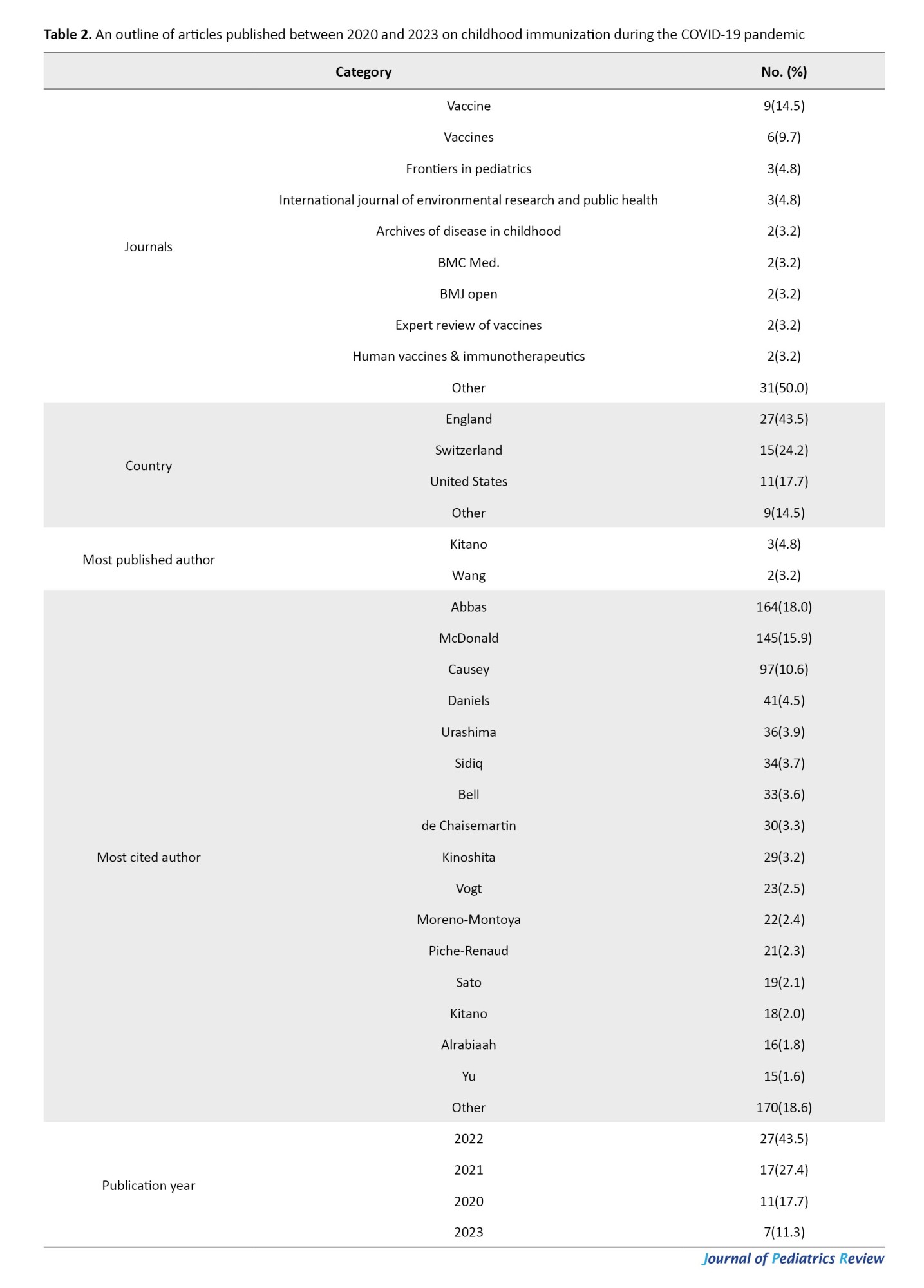
Co-occurrence author keywords
The keywords assisted in finding the most significant information associated with the study topics. The subjects that are most prevalent in publications in a certain field may be ascertained using the co-occurrence analysis of keywords [32]. We conducted a keyword co-occurrence analysis using the VOSviewer. Accordingly, 228 keywords in all were looked up in the Web of Science papers. In the Web of Science database, 15 terms on this subject were displayed more than five times, as shown in Figure 2. COVID-19 is the most used keyword, with 37 repetitions. In the COVID-19 pandemic research, the terms “children,” “vaccination,” “impact,” “coverage education,” and “childhood vaccination” were each used more than 10–14 times. Furthermore, measles was important while considering childhood vaccination during the COVID-19 epidemic, as shown by the observation that it was used as a keyword 6 times. “United States” (used as a keyword 8 times) and Africa (6 times) were also significant. Meanwhile, Figure 2 shows the chronological order of the appearance of words from 2021 to 2022. The following words appeared in the articles in order: Vaccine, COVID-19, children, immunization, United States, childhood vaccination, coverage, and vaccine hesitancy.
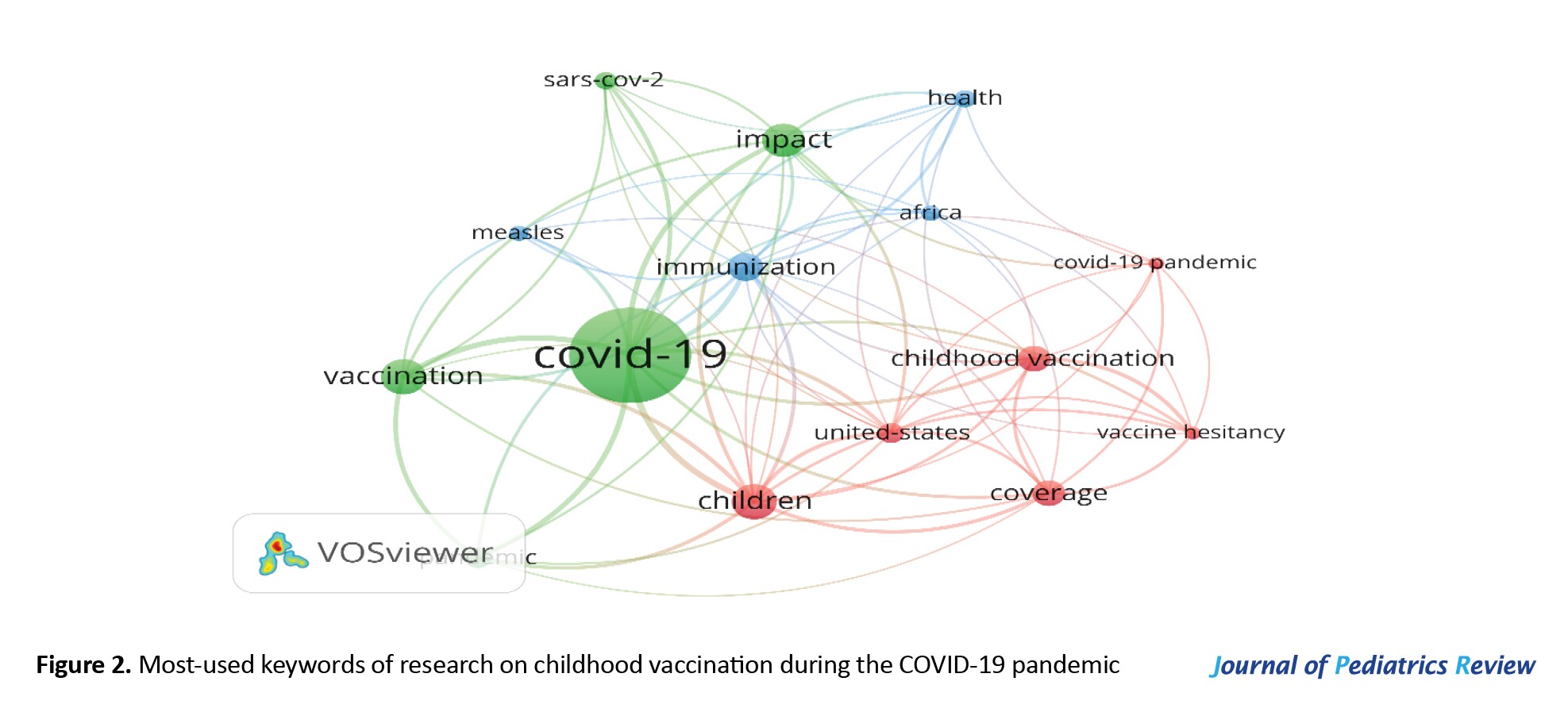
Keyword clustering
We could identify and categorize concepts that were closely connected in the chosen literature because of their arrangement and connections between the main words. Three major groups were identified by the study (Figure 3). The node size reflects the keyword frequency. The strength of connections between nodes is inversely correlated with the thickness of the interconnections between them. The research led to the formation of three groups. The words “COVID-19,” “immunization,” AND “children” had the highest number of links and overall link strength. All three clusters had a total of 74 linkages, with a total link strength of 210. The two terms that predominated cluster 1 (green) were COVID-19 and immunization. The topics in Cluster 2 (blue) were vaccination, measles, Africa, and health. Cluster 3 (red) focused on children, childhood vaccination, coverage, vaccination hesitancy, and the United States, which emerged as highly visible keywords.
Co-authorship countries/regions
During the COVID-19 epidemic, 47 countries conducted studies on child immunization according to the Web of Science databases. Six countries, including the USA, England, Canada, Switzerland, China, Japan, and Brazil, published more than three publications on the Web of Science databases. The United States and England have made 19 and 12 publications, respectively. The United States and England were the two major countries that demonstrated international cooperation in the field of childhood immunization throughout the COVID-19 epidemic, according to the database (Table 3).
Discussion
This study used the Web of Science databases to analyze several recent publications to identify trends in childhood vaccination research that are connected to the COVID-19 pandemic. To analyze the included studies, descriptive and quantitative statistics were employed. The research papers were examined using the bibliometric approach in terms of article counts, prolific nations and regions, categories, and keyword distributions. According to this study, the COVID-19 pandemic considerably influenced child immunization internationally and caused large pauses in scheduled vaccination programs. The disruptions can be attributed to various factors in the following five categories.
Changes in vaccination coverage rates
Most research indicated that during the COVID-19 pandemic, rates of child immunization coverage significantly decreased [29, 33, 34]. These declines were observed across various vaccines, including routine vaccines such as measles, [25, 35, 36] polio, and diphtheria-tetanus-pertussis [22, 26]. Different nations and regions saw different levels of the reduction, with some locations seeing greater declines in vaccination coverage than others [37-39]. The results of one previous study are in line with this research. Studies indicated that the Southeast Asia and Western Pacific regions, where 18 of the 19(95%) countries included in the study reported disruptions to vaccination, especially infancy and school-entry-age vaccinations [40]. Similar findings were reported in the Spanish Association of Pediatrics (AEP), which also recorded a decline in vaccination coverage (range: 5.0%–60.0%) in March 2020 compared with the monthly average from January 2019 to February 2020 [41]. Similar findings were reported in Pakistan, where a 52.5% decrease was observed in the daily average total number of vaccinations administered from September 2019 to March 2020 [16].
Vaccine hesitancy and parental concerns
The pandemic has amplified vaccine hesitancy [42] and parental concerns [28, 43] regarding the safety and efficacy of vaccines. According to several studies, there was an increase in vaccination reluctance during the COVID-19 pandemic, which was brought on by false information, worry about getting COVID-19 in healthcare facilities, and worries about the quick development of COVID-19 vaccines. These factors have contributed to a reluctance among parents to seek routine immunization services for their children [44].
Missed or delayed vaccinations
The disruptions caused by the pandemic, including lockdown measures and restricted healthcare access, have resulted in missed [45] or delayed vaccinations for many children [45, 46]. Studies reported that children have not been able to receive vaccines according to the recommended schedule, leading to potential gaps in immunity and a greater possibility of illnesses with vaccination protection [47]. Similarly, in a study In England, during the coronavirus disease, the measles-mumps-rubella vaccination started falling in 2020 before the introduction of physical distancing measures implemented in response to the COVID-19 epidemic. In the first 3 weeks of physical distancing, measles-mumps-rubella vaccination counts were 19.8% lower than for the same period in 2019. There was a general decrease in hexavalent vaccinations delivered in 2020 compared with 2019 [48].
Catch-up immunization efforts
Some countries and healthcare systems implemented catch-up immunization strategies to address the gaps in vaccination coverage caused by the pandemic [49]. These strategies involved targeted campaigns, outreach programs, and extended clinic hours to ensure that missed vaccinations are administered and immunization schedules are brought up to date [31].
Disruptions to routine immunization programs
The COVID-19 pandemic has disrupted regular vaccination campaigns throughout the world. Health system challenges, including reallocation of resources [50], a reduced healthcare workforce, and disruptions in vaccine supply chains, have impacted the delivery of immunization services [30]. Additionally, reduced healthcare-seeking behavior and fear of visiting healthcare facilities have further contributed to the disruption of routine immunization programs [51, 52]. The findings highlight the magnitude of the problem, with estimates indicating that millions of infants are now at risk due to the suspension of vaccination services in multiple countries. The pandemic resulted in a substantial number of children missing out on essential vaccines such as the measles-containing vaccination and the diphtheria, tetanus, and pertussis vaccines. Disruptions like this have previously caused epidemics of illnesses like polio, diphtheria, pertussis, and measles that can be prevented by vaccination [31]. The results of some previous studies support our study. One study reported that diphtheria-tetanus-pertussis (DTP) vaccine coverage decreased by 42.0%, oral polio vaccine coverage decreased by 79.0%, and measles vaccine coverage decreased by 9.0% among the school-entry age group [40]. The largest decline was 40.6% for the BCG vaccine [16].
Conclusion
The current review summarizes and analyses the global impact of the COVID-19 pandemic on childhood vaccination. These disruptions included: Disruptions in vaccination coverage, increased hesitancy, missing or delayed vaccinations, compensatory efforts, and disruptions to routine programs. Based on the evidence presented in this review, this coverage compromises immunization and endangers the health of millions of babies worldwide. Urgent action is needed, emphasizing targeted interventions, resilient healthcare systems, and public health awareness. This may help protect children from vaccine-preventable diseases during or after the COVID-19 pandemic. Policymakers and public health officials need to restore disrupted immunization services, implement targeted catch-up vaccination programs, and address vaccine hesitancy through community engagement and tailored awareness campaigns. Strengthening global collaboration, investing in research, and incorporating immunization into crisis preparedness plans are essential steps to safeguard childhood immunization after the COVID-19 pandemic.
Study limitations
This review faced some restrictions. We only found a relatively small number of papers that looked at how the COVID-19 pandemic has affected vaccine coverage, especially those that described the obstacles or other variables that have affected the interruptions from the standpoint of users or providers. We probably missed a large number of non-English publications throughout our search. Furthermore, the existing body of evidence was further constrained by using the inclusion criteria first. The cost of vaccinations and the rules governing immunization have not been examined, nevertheless, as we strive to emphasize the effects of COVID-19 on immunization programs.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The author declared no conflict of interest.
References
- Kuznetsova L, Cortassa G, Trilla A. Effectiveness of mandatory and incentive-based routine childhood immunization programs in europe: A systematic review of the literature. Vaccines (Basel). 2021; 9(10):1173. [DOI:10.3390/vaccines9101173] [PMID]
- Wang Z, Chen S, Fang Y. Parental willingness and associated factors of pediatric vaccination in the era of COVID-19 pandemic: A systematic review and meta-analysis. Vaccines (Basel). 2022; 10(9):1453. [DOI:10.3390/vaccines10091453] [PMID]
- Paul S, Mishra CM. Do we need to vaccinate every child against COVID-19: What evidence suggests -A systematic review of opinions. Front Public Heal. 2022; 10:1002992. [DOI:10.3389/fpubh.2022.1002992] [PMID]
- WHO. Weekly epidemiological update on COVID-19 23 November 2022: Edition 119. Geneva: WHO; 2022. [Link]
- Olorunsaiye CZ, Yusuf KK, Reinhart K, Salihu HM. COVID-19 and child vaccination: A systematic approach to closing the immunization gap. Int J Matern Child Heal AIDS. 2020; 9(3):381-5. [DOI:10.21106/ijma.401] [PMID]
- Causey K, Fullman N, Sorensen RJD, Galles NC, Zheng P, Aravkin A, et al. Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020: A modelling study. Lancet. 2021; 398(10299):522-34. [DOI:10.1016/S0140-6736(21)01337-4] [PMID]
- Castrejon MM, Leal I, de Jesus Pereira Pinto T, Guzmán-Holst A. The impact of COVID-19 and catch-up strategies on routine childhood vaccine coverage trends in Latin America: A systematic literature review and database analysis. Hum Vaccin Immunother. 2022; 18(6):2102353. [DOI:10.1080/21645515.2022.2102353] [PMID]
- Al-Amer R, Maneze D, Everett B, Montayre J, Villarosa AR, Dwekat E, et al. COVID-19 vaccination intention in the first year of the pandemic: A systematic review. J Clin Nurs. 2022; 31(1-2):62-86. [DOI:10.1111/jocn.15951] [PMID]
- Ali I. Impact of COVID-19 on vaccination programs: Adverse or positive? Hum Vaccin Immunother. 2020; 16(11):2594-2600. [DOI:10.1080/21645515.2020.1787065] [PMID]
- WHO. Second round of the national pulse survey on continuity of essential health services during the COVID-19 pandemic. Geneva: WHO; 2021. [Link]
- Nelson R. COVID-19 disrupts vaccine delivery. Lancet Infect Dis. 2020; 20(5):546. [DOI:10.1016/S1473-3099(20)30304-2] [PMID]
- Malcangi G, Inchingolo AD, Inchingolo AM, Piras F, Settanni V, Garofoli G, et al. COVID-19 infection in children and infants: Current status on therapies and vaccines. Children (Basel). 2022; 9(2):249. [DOI:10.3390/children9020249] [PMID]
- Chiappini E, Parigi S, Galli L, Licari A, Brambilla I, Angela Tosca M, et al. Impact that the COVID-19 pandemic on routine childhood vaccinations and challenges ahead: A narrative review. Acta Paediatr. 2021; 110(9):2529-35. [DOI:10.1111/apa.15949] [PMID]
- Spencer N, Markham W, Johnson S, Arpin E, Nathawad R, Gunnlaugsson G, et al. The Impact of COVID-19 pandemic on inequity in routine childhood vaccination coverage: A systematic review. Vaccines. 2022; 10(7):1013. [DOI:10.3390/vaccines10071013] [PMID]
- Alleman MM, Jorba J, Henderson E, Diop OM, Shaukat S, Traoré MA, et al. Update on vaccine-derived poliovirus outbreaks-worldwide, January 2020-June 2021. Morb Mortal Wkly Rep. 2021; 70(49):1691-9. [DOI:10.15585/mmwr.mm7049a1] [PMID]
- Chandir S, Siddiqi DA, Mehmood M, Setayesh H, Siddique M, Mirza A, et al. Impact of COVID-19 pandemic response on uptake of routine immunizations in Sindh, Pakistan: An analysis of provincial electronic immunization registry data. Vaccine. 2020; 38(45):7146-55. [DOI:10.1016/j.vaccine.2020.08.019] [PMID]
- Bagcchi S. COVID-19 and measles: Double trouble for Burundi. The Lancet Microbe. 2020; 1(2):e65. [DOI:10.1016/S2666-5247(20)30040-9] [PMID]
- Roberts L. Why measles deaths are surging - and coronavirus could make it worse. Nature. 2020; 580(7804):446-7. [DOI:10.1038/d41586-020-01011-6] [PMID]
- Verity R, Okell LC, Dorigatti I, Winskill P, Whittaker C, Imai N, et al. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect Dis. 2020; 20(6):669-77. [DOI:10.1016/S1473-3099(20)30243-7] [PMID]
- SeyedAlinaghi S, Karimi A, Mojdeganlou H, Alilou S, Mirghaderi SP, Noori T, et al. Impact of COVID-19 pandemic on routine vaccination coverage of children and adolescents: A systematic review. Health Sci Rep. 2022; 5(2):e00516. [DOI:10.1002/hsr2.516] [PMID]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021; 372:n71. [DOI:10.1136/bmj.n71] [PMID]
- Aguinaga-Ontoso I, Guillen-Aguinaga S, Guillen-Aguinaga L, Alas-Brun R, Onambele L, Aguinaga-Ontoso E, et al. COVID-19 Impact on DTP vaccination trends in Africa: A joinpoint regression analysis. Vaccines (Basel). 2023; 11(6):1103. [DOI:10.3390/vaccines11061103] [PMID]
- Gelagay AA, Worku AG, Bashah DT, Tebeje NB, Gebrie MH, Yeshita HY, et al. Complete childhood vaccination and associated factors among children aged 12-23 months in Dabat demographic and health survey site, Ethiopia, 2022. BMC Public Health. 2023; 23(1):802. [DOI:10.1186/s12889-023-15681-0] [PMID]
- Luchesi BM, de Oliveira Andrade N, Carrijo MF, Azambuja HCS, Martins TCR, Seixas RAM. Factors associated with Influenza vaccination during the COVID-19 pandemic in older adults residing in Brazil. J Gerontol Nurs. 2023; 49(5):31-8. [DOI:10.3928/00989134-20230414-03] [PMID]
- Martínez-Marcos M, Zabaleta-Del-Olmo E, Gómez-Durán EL, Reñé-Reñé A, Cabezas-Peña C. Impact of the COVID-19 lockdown on routine childhood vaccination coverage rates in Catalonia (Spain): A public health register-based study. Public Health. 2023; 218:68-74. [DOI:10.1016/j.puhe.2023.02.017] [PMID]
- Saidu Y, Di Mattei P, Nchinjoh SC, Edwige NN, Nsah B, Muteh NJ, et al. The Hidden Impact of the COVID-19 Pandemic on Routine Childhood Immunization Coverage in Cameroon. Vaccines (Basel). 2023; 11(3):645. [DOI:10.3390/vaccines11030645] [PMID]
- Humble RM, Scott SD, Dubé E, Olson J, MacDonald SE. The impact of the COVID-19 pandemic on parents' perceptions and acceptance of routine childhood vaccination in Canada: A national longitudinal study. Vaccine. 2023; 41(2):407-15. [DOI:10.1016/j.vaccine.2022.11.052] [PMID]
- Khan YH, Mallhi TH, Salman M, Tanveer N, Butt MH, Mustafa ZU, et al. Parental perceptions and barriers towards childhood COVID-19 vaccination in Saudi Arabia: A cross-sectional analysis. Vaccines (Basel). 2022; 10(12):2093. [DOI:10.3390/vaccines10122093] [PMID]
- Deerin JF, Gyekye-Kusi AA, Doss-Walker J, Bablak H, Kim D. Evaluation of "Catch Up to Get Ahead" efforts on administration of routine childhood vaccinations during COVID-19 pandemic, United States Indian Health Service, 2020. J Public Health Policy. 2022; 43(4):613-20. [DOI:10.1057/s41271-022-00373-7] [PMID]
- Melkonyan N, Badalyan A, Hovhannisyan H, Poghosyan K. Impact of the COVID-19 pandemic on routine immunization services in Yerevan and vaccinations against COVID-19 in Armenia. J Infect Dev Ctries. 2022; 16(11):1687-95. [DOI:10.3855/jidc.17028] [PMID]
- Herdea V, Ghionaru R, Lungu CN, Leibovitz E, Diaconescu S. Vaccine coverage in children younger than 1 year of age during periods of high epidemiological risk: Are we preparing for new outbreaks? Children (Basel). 2022; 9(9):1334. [DOI:10.3390/children9091334] [PMID]
- Kim H, So KKF. Two decades of customer experience research in hospitality and tourism: A bibliometric analysis and thematic content analysis. Int J Hosp Manag. 2022; 100:103082. [DOI:10.1016/j.ijhm.2021.103082]
- Moura C, Truche P, Sousa Salgado L, Meireles T, Santana V, Buda A, et al. The impact of COVID-19 on routine pediatric vaccination delivery in Brazil. Vaccine. 2022; 40(15):2292-8. [DOI:10.1016/j.vaccine.2022.02.076] [PMID]
- Connolly E, Boley EJ, Fejfar DL, Varney PF, Aron MB, Fulcher IR, et al. Childhood immunization during the COVID-19 pandemic: Experiences in Haiti, Lesotho, Liberia and Malawi. Bull World Health Organ. 2022; 100(2):115-26C. [DOI:10.2471/BLT.21.286774] [PMID]
- Hoang U, de Lusignan S, Joy M, Sherlock J, Williams J, Bankhead C, et al. National rates and disparities in childhood vaccination and vaccine-preventable disease during the COVID-19 pandemic: English sentinel network retrospective database study. Arch Dis Child. 2022; 107(8):733-9. [DOI:10.1136/archdischild-2021-323630] [PMID]
- MacDonald SE, Paudel YR, Kiely M, Rafferty E, Sadarangani M, Robinson JL, et al. Impact of the COVID-19 pandemic on vaccine coverage for early childhood vaccines in Alberta, Canada: A population-based retrospective cohort study. BMJ Open. 2022; 12(1):e055968. [DOI:10.1136/bmjopen-2021-055968] [PMID]
- Sabbatucci M, Odone A, Signorelli C, Siddu A, Silenzi A, Maraglino FP, et al. Childhood immunisation coverage during the COVID-19 epidemic in Italy. Vaccines (Basel). 2022; 10(1):120. [DOI:10.3390/vaccines10010120] [PMID]
- Kiely M, Mansour T, Brousseau N, Rafferty E, Paudel YR, Sadarangani M, et al. COVID-19 pandemic impact on childhood vaccination coverage in Quebec, Canada. Hum Vaccin Immunother. 2022; 18(1):2007707. [DOI:10.1080/21645515.2021.2007707] [PMID]
- Sell H, Assi A, Driedger SM, Dubé È, Gagneur A, Meyer SB, et al. Continuity of routine immunization programs in Canada during the COVID-19 pandemic. Vaccine. 2021; 39(39):5532-7. [DOI:10.1016/j.vaccine.2021.08.044] [PMID]
- Harris RC, Chen Y, Côte P, Ardillon A, Nievera MC, Ong-Lim A, et al. Impact of COVID-19 on routine immunisation in South-East Asia and Western Pacific: Disruptions and solutions. Lancet Reg Heal - West Pacific. 2021; 10:100140. [DOI:10.1016/j.lanwpc.2021.100140] [PMID]
- Moraga-Llop FA, Fernández-Prada M, Grande-Tejada AM, Martínez-Alcorta LI, Moreno-Pérez D, Pérez-Martín JJ. Recovering lost vaccine coverage due to COVID-19 pandemic. Vacunas (English Edition). 2020; 21(2):129-35. [DOI:10.1016/j.vacune.2020.10.004]
- Derdemezis C, Markozannes G, Rontogianni MO, Trigki M, Kanellopoulou A, Papamichail D, et al. Parental Hesitancy towards the established childhood vaccination programmes in the COVID-19 Era: Assessing the drivers of a challenging public health concern. Vaccines (Basel). 2022;10(5):814. [DOI:10.3390/vaccines10050814] [PMID]
- Alrabiaah AA, Alshaer AH, Estrella SMC, Inclan KAS, Aljammaz HA, Almoosa KM, et al. Effects of the Coronavirus disease 2019 pandemic on routine pediatric immunization coverage rates at the main University Hospital in Saudi Arabia. SAUDI Med J. 2020; 41(11):1197-203. [DOI:10.15537/smj.2020.11.25457] [PMID]
- Salazar TL, Pollard DL, Pina-Thomas DM, Benton MJ. Parental vaccine hesitancy and concerns regarding the COVID-19 virus. J Pediatr Nurs. 2022; 65:10-5. [DOI:10.1016/j.pedn.2022.03.010] [PMID]
- Shapiro GK, Gottfredson N, Leask J, Wiley K, Ganter-Restrepo FE, Jones SP, et al. COVID-19 and missed or delayed vaccination in 26 middle- and high-income countries: An observational survey. Vaccine. 2022; 40(6):945-52. [DOI:10.1016/j.vaccine.2021.12.041] [PMID]
- Abu-rish EY, Bustanji Y, Abusal K. Nationwide routine childhood vaccination coverage during the COVID-19 pandemic in Jordan: Current situation, reasons, and predictors of vaccination. Int J Clin Pract. 2022; 2022:7918604. [DOI:10.1155/2022/7918604] [PMID]
- Baghdadi LR, Younis A, Al Suwaidan HI, Hassounah MM, Al Khalifah R. Impact of the COVID-19 pandemic lockdown on routine childhood immunization: A Saudi nationwide cross-sectional study. Front Pediatr. 2021; 9:692877. [DOI:10.3389/fped.2021.692877] [PMID]
- McDonald HI, Tessier E, White JM, Woodruff M, Knowles C, Bates C, et al. Early impact of the coronavirus disease (COVID-19) pandemic and physical distancing measures on routine childhood vaccinations in England, January to April 2020. Euro Surveill. 2020; 25(19):2000848. [DOI:10.2807/1560-7917.ES.2020.25.19.2000848] [PMID]
- Mancarella M, Natarelli F, Bertolini C, Zagari A, Enrica Bettinelli M, Castaldi S. Catch-up vaccination campaign in children between 6 and 8 years old during COVID-19 pandemic: The experience in a COVID hub in Milan, Italy. Vaccine. 2022; 40(26):3664-9. [DOI:10.1016/j.vaccine.2022.05.005] [PMID]
- Soomar SM, Soomar SM, Khan M, Moin G, Azam I. COVID-19 vaccine acceptance and hesitancy among the general population of Pakistan: A population-based survey. BMJ Open. 2022; 12(9):e064096. [DOI:10.1136/bmjopen-2022-064096] [PMID]
- Bell S, Clarke R, Paterson P, Mounier-Jack S. Parents' and guardians' views and experiences of accessing routine childhood vaccinations during the Coronavirus (COVID-19) pandemic: A mixed methods study in England. PLoS One. 2020; 15(12):e0244049. [DOI:10.1371/journal.pone.0244049] [PMID]
- Aizawa Y, Katsuta T, Sakiyama H, Tanaka-Taya K, Moriuchi H, Saitoh A. Changes in childhood vaccination during the Coronavirus disease 2019 pandemic in Japan. Vaccine. 2021; 39(29):4006-12. [DOI:10.1016/j.vaccine.2021.05.050] [PMID]
Type of Study: Review Article |
Subject:
Pediatric Infectious Diseases
Received: 2023/09/17 | Accepted: 2023/12/12 | Published: 2024/01/1
Received: 2023/09/17 | Accepted: 2023/12/12 | Published: 2024/01/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









