Volume 12, Issue 1 (1-2024)
J. Pediatr. Rev 2024, 12(1): 65-72 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Aburayyan L, Ozturk C, Varvani Farahani P. Investigating the Application of Orem’s Self-care Nursing Theory for Spinal Muscular Atrophy: A Case Study Design. J. Pediatr. Rev 2024; 12 (1) :65-72
URL: http://jpr.mazums.ac.ir/article-1-571-en.html
URL: http://jpr.mazums.ac.ir/article-1-571-en.html
1- Department of Pediatric Nursing, Faculty of Nursing, Near East University, Nicosia, Cyprus. , 20215414@std.neu.edu.tr
2- Department of Pediatric Nursing, Faculty of Nursing, Near East University, Nicosia, Cyprus.
3- Department of Nursing, Faculty of Health Science, Cyprus International University, Nicosia, Turkish Republic of Northern Cyprus (TRNC).
2- Department of Pediatric Nursing, Faculty of Nursing, Near East University, Nicosia, Cyprus.
3- Department of Nursing, Faculty of Health Science, Cyprus International University, Nicosia, Turkish Republic of Northern Cyprus (TRNC).
Keywords: Nursing education, Spinal muscular atrophy (SMA), Nursing theories, Children, Neuromuscular disorders
Full-Text [PDF 384 kb]
(18557 Downloads)
| Abstract (HTML) (4920 Views)
Full-Text: (3164 Views)
Background
Spinal muscular atrophy (SMA) is one of the most prevalent neuromuscular diseases in children and has a high morbidity and mortality rate [1, 2]. Infant mortality due to genetics is the most common, accounting for 1 in 10 000 live births with a global prevalence of between 1-2 per 100000 people [3]. The complex condition known as SMA causes muscle weakness, atrophy, and functional impairment due to degeneration and spinal cord motor neuron loss. SMA can range greatly in severity. Type 1 SMA, which typically manifests in the first few months of life, is the most severe [4]. Untreated SMA type 1 has a classic clinical presentation of flaccid weakness, motor regression, muscle atrophy, dysphagia, respiratory failure, and untimely death in the first six months of life [5, 6]. On the other hand, the mildest form of SMA (type 4) manifests symptoms in adults [7]. The child’s ability to move around, breathe, and swallow are all significantly impacted by the SMA-related progressive muscle weakness and functional limitations [8]. SMA also puts a significant burden on parents, who are crucial to the upbringing and welfare of their children [9, 10]. To gain control over their well-being and general health through a variety of disease-related activities, children with disabilities who self-care engage in a dynamic, regular, and adaptable process in which responsibility and decision-making are shared by them and their parents [11, 12]. The self-care deficit nursing theory by Dorothea Orem emphasizes the role of nursing in helping people meet their self-care needs. The definition of self-care is actions taken regularly to uphold one’s health and well-being and nurses must assist patients in daily activities until they can do them independently [13-16]. Orem’s theory recognizes the importance of parents taking care of and supporting their children to ensure the child’s well-being. It recognizes the value of educating and assisting parents so they can actively take part in the care of the child and increase their confidence in handling the condition [10]. Informed decision-making and efficient management of the difficulties caused by SMA are skills that nurses can teach parents to use in their active involvement in their child’s care. This entails instruction on medication administration, observation of the child’s respiratory condition, identification of deterioration signs, and seeking the proper medical attention. Orem’s self-care deficit nursing theory offers nurses a useful framework for evaluating, organizing, and putting into practice interventions that support independent self-care and maximize the well-being of the child [5]. Additionally, by encouraging parents to actively participate in their child’s care, nurses can recognize and support the crucial role that parents play in improving outcomes and improving the healthcare experience for everyone [17]. The case study demonstrates how nursing theories can direct efficient patient and parent education, encourage favorable outcomes, and emphasize the theory’s practical use in SMA treatment.
Case Presentation
In this case report, according to Orem’s self-care deficiency theory, data on a 3 years and 9 months boy patient who was monitored in the pediatric intensive care unit and diagnosed with SMA type I (Werdnig Hoffmann disease), which is characterized by delayed motor milestones, progressive muscle weakness, failure to thrive and compromised respiratory function, poor feeding, difficult swallowing, poor reflex and risk for aspiration. The child’s parents are actively involved in their son’s care and are seeking guidance to improve their understanding of SMA management and enhance their self-care abilities.
According to Orem’s theory, people may practice self-care to preserve their health and wellness; however, when a person is unable to meet their needs, a self-care deficit arises, which results in health problems. In the case of a 3-year and 9-month-old boy diagnosed with SMA type I (Werdnig Hoffmann disease), Orem’s self-care deficit nursing theory was applied to guide nursing interventions that promoted self-care independence for the child and empowered the parents in their caregiving role. The first step is to know the client and parent’s needs to determine what kind of nursing care the person needs. The second stage is the design of the supporting educational system and planning for the implementation of care. The implementation of the self-care program and evaluation of that program’s implementation make up the third step.
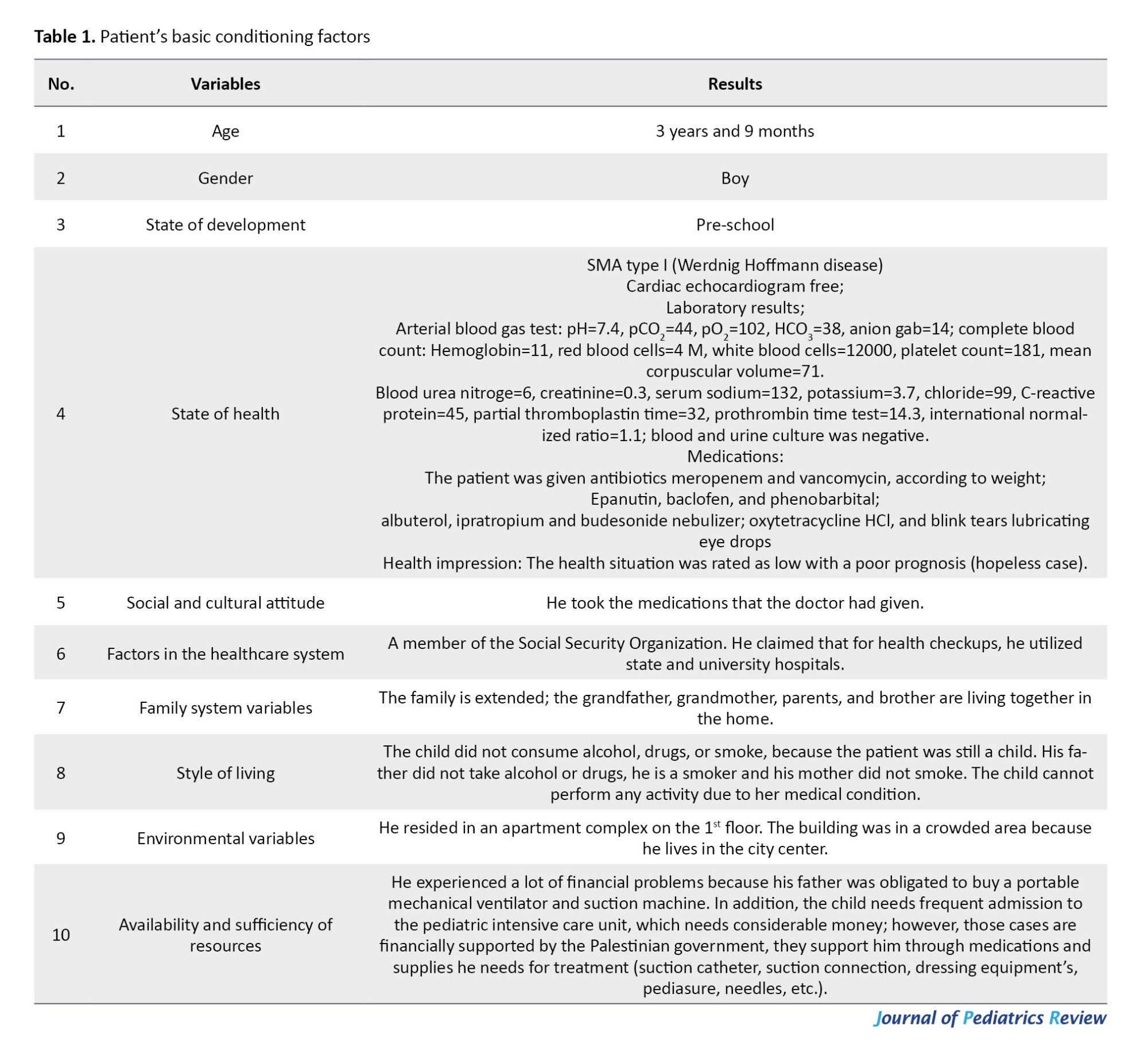
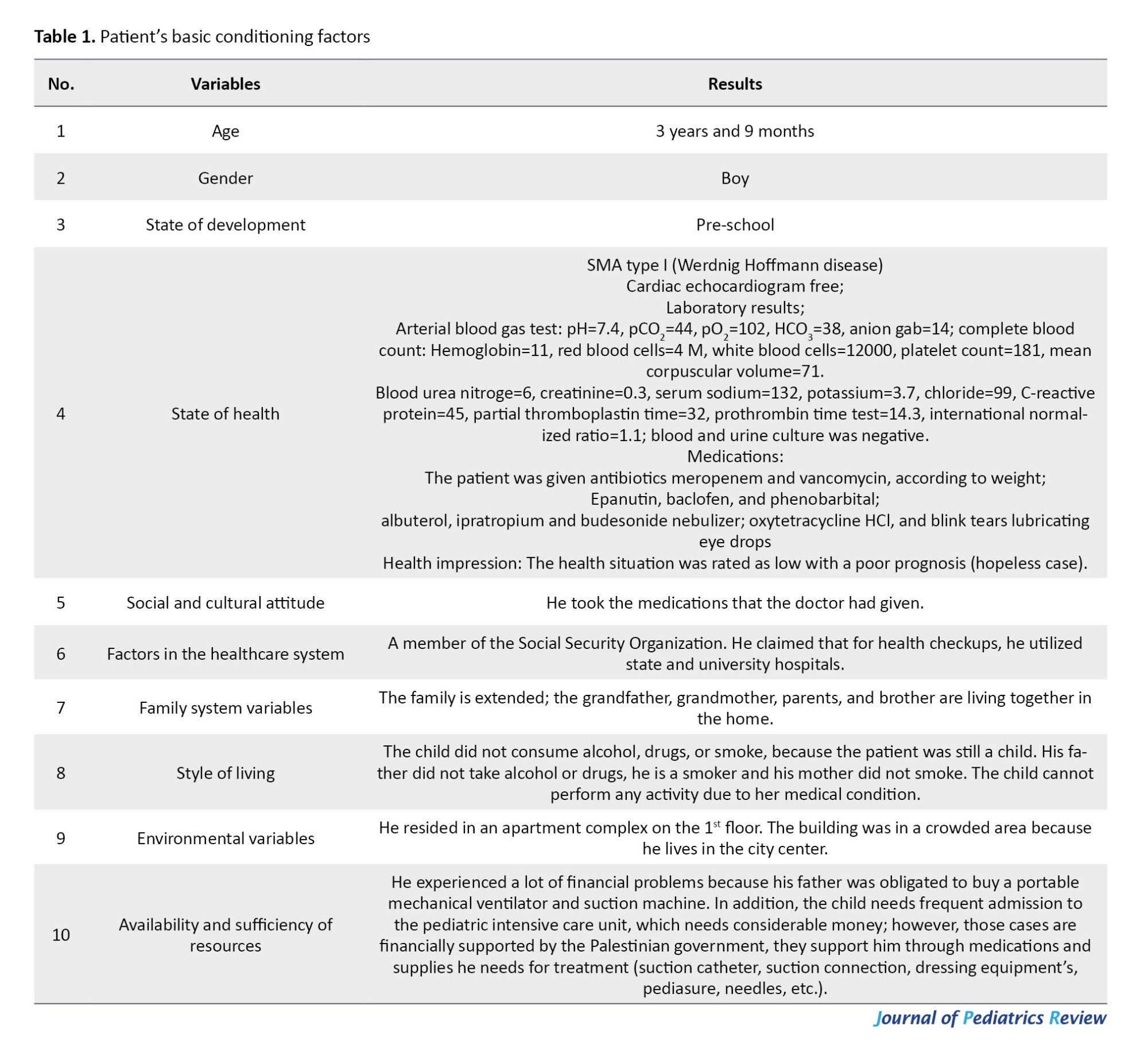
The first step was to assess the parents’ knowledge and understanding of SMA management and their current self-care practices, including her understanding of the disease process, and awareness of available treatment options, such as medication, physical therapy, respiratory support, and dietary modifications. Tools were used to collect the data, including: 1) A structured interview questionnaire sheet, and 2) Examine and recognize the conceptual structure of the Orem. This questionnaire was used to determine the nursing diagnoses for any self-care-related flaws or weaknesses. Based on the assessment data collected in line with Orem’s nursing theory of self-care insufficiency, the right strategy was developed to fulfill the needs of the patient. The researcher evaluated the limitations, deficiencies, disabilities, and abilities, as well as the study objectives, and discovered flaws based on the type of patient needs (Tables 1 and 2).

Diagnosis
Based on the assessment, nursing diagnoses were formulated, focusing on the child’s self-care deficits and the parents’ need for education and support. Some of the identified nursing diagnoses included impaired physical mobility related to muscle weakness, compromised nutrition and swallowing difficulties related to poor feeding and difficult swallowing, impaired respiratory function related to compromised respiratory function, and deficient knowledge related to SMA management.
Planning
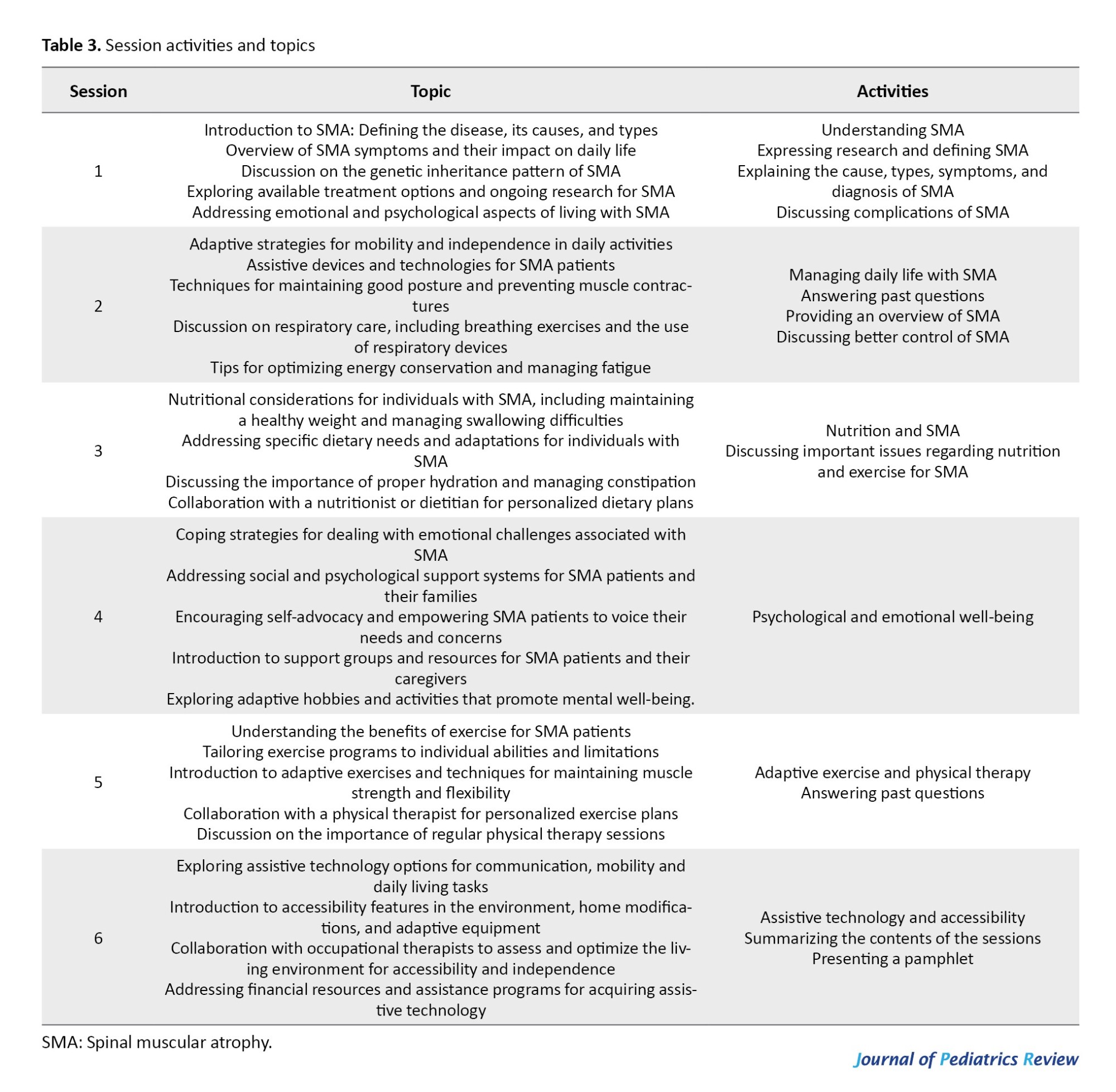
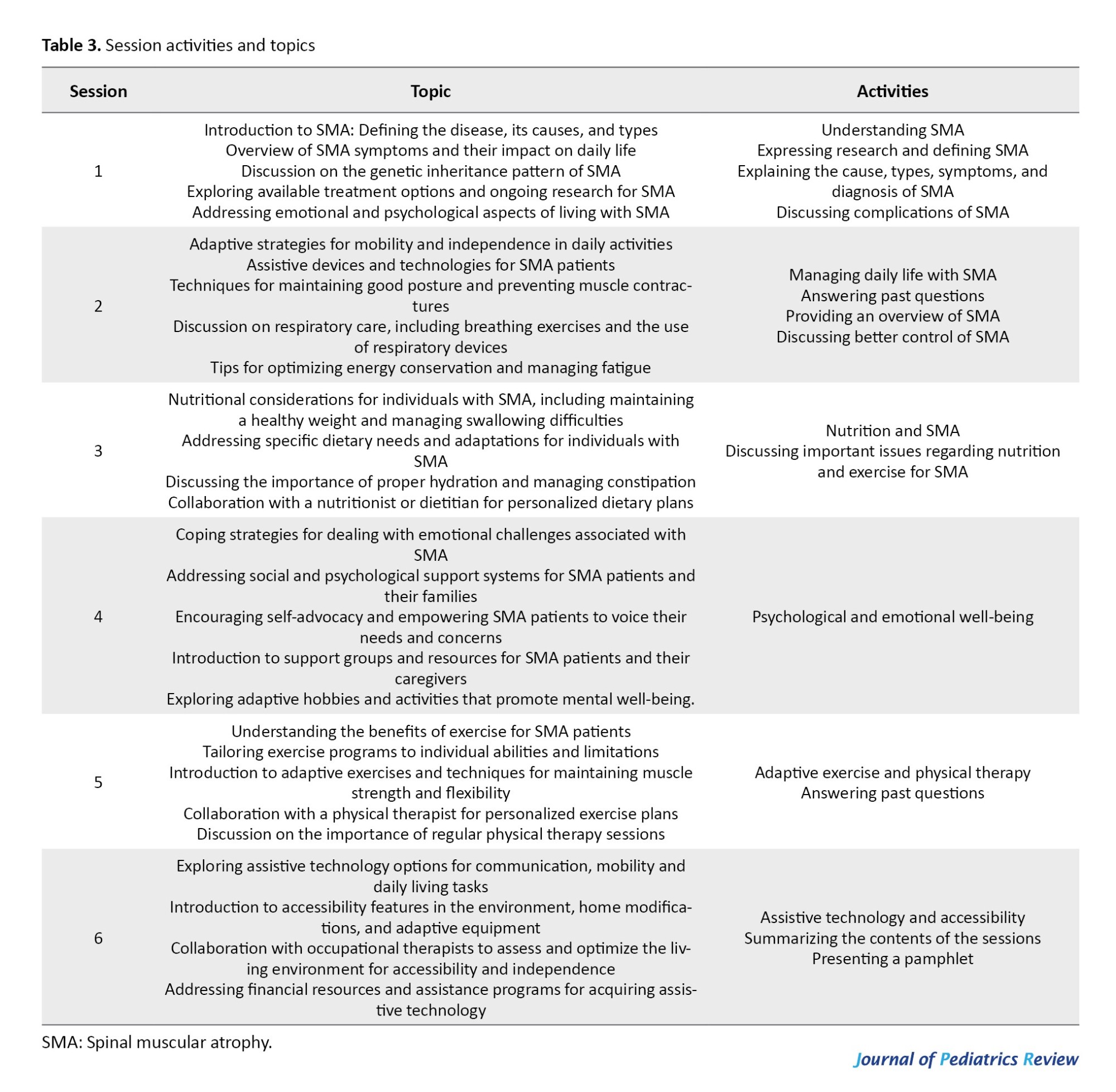
A care plan was developed based on the identified nursing diagnoses. The plan prioritized enhancing self-care abilities, improving the child’s overall well-being, and empowering the parents to effectively manage the child’s condition. Collaboration with a multidisciplinary team, including physicians, physical therapists, respiratory therapists, and nutritionists, was incorporated into the plan. An educational intervention was divided into four 60-min sessions in-person. The study’s instructional strategies included lectures, question-and-answer sessions, and movie screenings. An informative brochure was given out after the training session (Table 3).
Nursing interventions guided by Orem’s theory were implemented to address the identified nursing diagnoses. Reduced muscle mass, exercise intolerance, musculoskeletal impairment, and reduced physical mobility were demonstrated as seen by the child’s inability to walk, which are all symptoms of neuromuscular impairment. For impaired physical mobility, physical therapy interventions were introduced to promote motor development, muscle strength, and mobility. Adaptive devices such as braces, walkers, or wheelchairs were recommended to facilitate mobility. Swallowing and chewing abilities were tested in addition to the assessment of dietary consumption for adequate nutrition. A therapist evaluated the child’s swallowing abilities and advised on suitable feeding approaches, such as placement and texture changes, to address the child’s poor nutrition and swallowing issues. The parents got instruction on proper feeding techniques and aspiration warning signals, as well as help locating any necessary feeding devices. The patient’s respiratory pattern was not efficient. To manage the child’s impaired respiratory function, nurses educated the parents on respiratory support techniques, including chest physiotherapy and airway clearance methods. The parents were trained in recognizing signs of respiratory distress. To increase awareness and comprehension of the variables affecting one’s need for and capacity for self-care. Education and support were also provided to the parents regarding SMA management. This included understanding the disease process, medication administration, monitoring of respiratory function, recognizing signs of deterioration, and accessing appropriate medical interventions. The parents were involved in care planning and decision-making, allowing them to actively participate in their child’s care. In terms of support from family and caregivers, as the severity of their child’s SMA worsens, parents of SMA patients report feeling more and more stressed. The palliative care team’s involvement soon after diagnosis may be the best way to meet the parents and siblings of SMA patients’ needs for long-term support. Family-wide psychological support reduces healthcare use and improves quality of life. As a result, one of our main responsibilities is to mentally support and educate parents. Families frequently describe shock, anticipatory anguish, and a sense of helplessness when faced with a lethal form of SMA, especially after cardiac arrest. SMA is fatal, and her child’s case seems bleak. Therefore, my social worker and I have frequent contact with his parents and we support him in receiving end-of-life care.
Evaluation
Regular evaluation of the care plan and interventions was conducted to determine their effectiveness and make necessary adjustments. The child’s progress in achieving self-care independence, improvements in motor function, nutrition, and respiratory status, as well as the parents’ confidence in managing the child’s care, were assessed. Orem’s nursing theory may assist nurses in many disciplines in dynamically and meticulously evaluating patients’ capacity for self-care and implementing appropriate nursing interventions according to their needs, interests, and issues. By applying Orem’s self-care deficit nursing theory, nurses provided tailored care and support to the child with SMA and empowered the parents to actively participate in their child’s care. This approach promoted self-care independence, improved the child’s overall well-being, and enhanced the parents’ ability to effectively manage the challenges posed by SMA.
Discussion
This case study presented a comprehensive exploration of the effectiveness of applying Dorothea Orem’s self-care deficit nursing theory in managing a child diagnosed with SMA type I. By integrating Orem’s theoretical framework into nursing practice, this study aimed to promote self-care independence for the child while empowering the parents in their caregiving role. According to this study, the application of Orem’s theory facilitated a systematic approach to assessing the child’s and parent’s needs, formulating nursing diagnoses, and designing tailored interventions to address identified deficits. Through structured educational sessions and collaborative care planning, nurses equipped the parents with the knowledge and skills necessary to effectively manage the challenges associated with SMA.
The results of this study demonstrated the positive impact of nursing interventions guided by Orem’s theory on the child’s overall well-being and the parents’ confidence in managing their child’s care. By focusing on enhancing self-care abilities and promoting parental involvement, nurses contributed to improved outcomes for the child with SMA. Similarly, The findings of a study conducted by Awaliyah et al. in 2018 showed that the application of self-care theory is suitable for multiparous pregnant women with anemia as it helps them to be independent patients [18]. Moreover, the interdisciplinary collaboration involved in this study underscores the importance of a holistic approach to SMA management, involving healthcare professionals from various disciplines to address the multifaceted needs of the patient and family. Our findings are supported by research conducted by Hermalia et al. [19] and Si et al. [20] nursing care with the theory of an effective self-care model will shape the ability of patients and families to perform self-care and improve the quality of life of patients with chronic diseases.
The findings of this study highlight the practical relevance of nursing theories in pediatric care and the value of patient-centered approaches in managing complex conditions like SMA. By emphasizing the importance of patient education, empowerment, and collaboration, this study underscores the potential of nursing theories to inform evidence-based practice and enhance patient outcomes. Similarly, a study by Irshad Ali [14] showed that the usability of theory in practice resulted in drastic changes in practice and patient’s early recovery.
Conclusion
In conclusion, this study provides valuable insights into applying nursing theories in pediatric nursing practice, particularly in managing SMA. By leveraging theoretical frameworks like Orem’s self-care deficit nursing theory, nurses can play a pivotal role in promoting self-care independence and improving outcomes for children with SMA and their families.
Study limitations
This study’s limitation is that only one patient was used in it. The findings would be improved by more research in the form of a longitudinal study with more participants.
Ethical Considerations
Compliance with ethical guidelines
Written and verbal consent was obtained from the patient who participated in the study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the patient who agreed to participate in the case.
References
Spinal muscular atrophy (SMA) is one of the most prevalent neuromuscular diseases in children and has a high morbidity and mortality rate [1, 2]. Infant mortality due to genetics is the most common, accounting for 1 in 10 000 live births with a global prevalence of between 1-2 per 100000 people [3]. The complex condition known as SMA causes muscle weakness, atrophy, and functional impairment due to degeneration and spinal cord motor neuron loss. SMA can range greatly in severity. Type 1 SMA, which typically manifests in the first few months of life, is the most severe [4]. Untreated SMA type 1 has a classic clinical presentation of flaccid weakness, motor regression, muscle atrophy, dysphagia, respiratory failure, and untimely death in the first six months of life [5, 6]. On the other hand, the mildest form of SMA (type 4) manifests symptoms in adults [7]. The child’s ability to move around, breathe, and swallow are all significantly impacted by the SMA-related progressive muscle weakness and functional limitations [8]. SMA also puts a significant burden on parents, who are crucial to the upbringing and welfare of their children [9, 10]. To gain control over their well-being and general health through a variety of disease-related activities, children with disabilities who self-care engage in a dynamic, regular, and adaptable process in which responsibility and decision-making are shared by them and their parents [11, 12]. The self-care deficit nursing theory by Dorothea Orem emphasizes the role of nursing in helping people meet their self-care needs. The definition of self-care is actions taken regularly to uphold one’s health and well-being and nurses must assist patients in daily activities until they can do them independently [13-16]. Orem’s theory recognizes the importance of parents taking care of and supporting their children to ensure the child’s well-being. It recognizes the value of educating and assisting parents so they can actively take part in the care of the child and increase their confidence in handling the condition [10]. Informed decision-making and efficient management of the difficulties caused by SMA are skills that nurses can teach parents to use in their active involvement in their child’s care. This entails instruction on medication administration, observation of the child’s respiratory condition, identification of deterioration signs, and seeking the proper medical attention. Orem’s self-care deficit nursing theory offers nurses a useful framework for evaluating, organizing, and putting into practice interventions that support independent self-care and maximize the well-being of the child [5]. Additionally, by encouraging parents to actively participate in their child’s care, nurses can recognize and support the crucial role that parents play in improving outcomes and improving the healthcare experience for everyone [17]. The case study demonstrates how nursing theories can direct efficient patient and parent education, encourage favorable outcomes, and emphasize the theory’s practical use in SMA treatment.
Case Presentation
In this case report, according to Orem’s self-care deficiency theory, data on a 3 years and 9 months boy patient who was monitored in the pediatric intensive care unit and diagnosed with SMA type I (Werdnig Hoffmann disease), which is characterized by delayed motor milestones, progressive muscle weakness, failure to thrive and compromised respiratory function, poor feeding, difficult swallowing, poor reflex and risk for aspiration. The child’s parents are actively involved in their son’s care and are seeking guidance to improve their understanding of SMA management and enhance their self-care abilities.
According to Orem’s theory, people may practice self-care to preserve their health and wellness; however, when a person is unable to meet their needs, a self-care deficit arises, which results in health problems. In the case of a 3-year and 9-month-old boy diagnosed with SMA type I (Werdnig Hoffmann disease), Orem’s self-care deficit nursing theory was applied to guide nursing interventions that promoted self-care independence for the child and empowered the parents in their caregiving role. The first step is to know the client and parent’s needs to determine what kind of nursing care the person needs. The second stage is the design of the supporting educational system and planning for the implementation of care. The implementation of the self-care program and evaluation of that program’s implementation make up the third step.
The first step was to assess the parents’ knowledge and understanding of SMA management and their current self-care practices, including her understanding of the disease process, and awareness of available treatment options, such as medication, physical therapy, respiratory support, and dietary modifications. Tools were used to collect the data, including: 1) A structured interview questionnaire sheet, and 2) Examine and recognize the conceptual structure of the Orem. This questionnaire was used to determine the nursing diagnoses for any self-care-related flaws or weaknesses. Based on the assessment data collected in line with Orem’s nursing theory of self-care insufficiency, the right strategy was developed to fulfill the needs of the patient. The researcher evaluated the limitations, deficiencies, disabilities, and abilities, as well as the study objectives, and discovered flaws based on the type of patient needs (Tables 1 and 2).

Diagnosis
Based on the assessment, nursing diagnoses were formulated, focusing on the child’s self-care deficits and the parents’ need for education and support. Some of the identified nursing diagnoses included impaired physical mobility related to muscle weakness, compromised nutrition and swallowing difficulties related to poor feeding and difficult swallowing, impaired respiratory function related to compromised respiratory function, and deficient knowledge related to SMA management.
Planning
A care plan was developed based on the identified nursing diagnoses. The plan prioritized enhancing self-care abilities, improving the child’s overall well-being, and empowering the parents to effectively manage the child’s condition. Collaboration with a multidisciplinary team, including physicians, physical therapists, respiratory therapists, and nutritionists, was incorporated into the plan. An educational intervention was divided into four 60-min sessions in-person. The study’s instructional strategies included lectures, question-and-answer sessions, and movie screenings. An informative brochure was given out after the training session (Table 3).
Nursing interventions guided by Orem’s theory were implemented to address the identified nursing diagnoses. Reduced muscle mass, exercise intolerance, musculoskeletal impairment, and reduced physical mobility were demonstrated as seen by the child’s inability to walk, which are all symptoms of neuromuscular impairment. For impaired physical mobility, physical therapy interventions were introduced to promote motor development, muscle strength, and mobility. Adaptive devices such as braces, walkers, or wheelchairs were recommended to facilitate mobility. Swallowing and chewing abilities were tested in addition to the assessment of dietary consumption for adequate nutrition. A therapist evaluated the child’s swallowing abilities and advised on suitable feeding approaches, such as placement and texture changes, to address the child’s poor nutrition and swallowing issues. The parents got instruction on proper feeding techniques and aspiration warning signals, as well as help locating any necessary feeding devices. The patient’s respiratory pattern was not efficient. To manage the child’s impaired respiratory function, nurses educated the parents on respiratory support techniques, including chest physiotherapy and airway clearance methods. The parents were trained in recognizing signs of respiratory distress. To increase awareness and comprehension of the variables affecting one’s need for and capacity for self-care. Education and support were also provided to the parents regarding SMA management. This included understanding the disease process, medication administration, monitoring of respiratory function, recognizing signs of deterioration, and accessing appropriate medical interventions. The parents were involved in care planning and decision-making, allowing them to actively participate in their child’s care. In terms of support from family and caregivers, as the severity of their child’s SMA worsens, parents of SMA patients report feeling more and more stressed. The palliative care team’s involvement soon after diagnosis may be the best way to meet the parents and siblings of SMA patients’ needs for long-term support. Family-wide psychological support reduces healthcare use and improves quality of life. As a result, one of our main responsibilities is to mentally support and educate parents. Families frequently describe shock, anticipatory anguish, and a sense of helplessness when faced with a lethal form of SMA, especially after cardiac arrest. SMA is fatal, and her child’s case seems bleak. Therefore, my social worker and I have frequent contact with his parents and we support him in receiving end-of-life care.
Evaluation
Regular evaluation of the care plan and interventions was conducted to determine their effectiveness and make necessary adjustments. The child’s progress in achieving self-care independence, improvements in motor function, nutrition, and respiratory status, as well as the parents’ confidence in managing the child’s care, were assessed. Orem’s nursing theory may assist nurses in many disciplines in dynamically and meticulously evaluating patients’ capacity for self-care and implementing appropriate nursing interventions according to their needs, interests, and issues. By applying Orem’s self-care deficit nursing theory, nurses provided tailored care and support to the child with SMA and empowered the parents to actively participate in their child’s care. This approach promoted self-care independence, improved the child’s overall well-being, and enhanced the parents’ ability to effectively manage the challenges posed by SMA.
Discussion
This case study presented a comprehensive exploration of the effectiveness of applying Dorothea Orem’s self-care deficit nursing theory in managing a child diagnosed with SMA type I. By integrating Orem’s theoretical framework into nursing practice, this study aimed to promote self-care independence for the child while empowering the parents in their caregiving role. According to this study, the application of Orem’s theory facilitated a systematic approach to assessing the child’s and parent’s needs, formulating nursing diagnoses, and designing tailored interventions to address identified deficits. Through structured educational sessions and collaborative care planning, nurses equipped the parents with the knowledge and skills necessary to effectively manage the challenges associated with SMA.
The results of this study demonstrated the positive impact of nursing interventions guided by Orem’s theory on the child’s overall well-being and the parents’ confidence in managing their child’s care. By focusing on enhancing self-care abilities and promoting parental involvement, nurses contributed to improved outcomes for the child with SMA. Similarly, The findings of a study conducted by Awaliyah et al. in 2018 showed that the application of self-care theory is suitable for multiparous pregnant women with anemia as it helps them to be independent patients [18]. Moreover, the interdisciplinary collaboration involved in this study underscores the importance of a holistic approach to SMA management, involving healthcare professionals from various disciplines to address the multifaceted needs of the patient and family. Our findings are supported by research conducted by Hermalia et al. [19] and Si et al. [20] nursing care with the theory of an effective self-care model will shape the ability of patients and families to perform self-care and improve the quality of life of patients with chronic diseases.
The findings of this study highlight the practical relevance of nursing theories in pediatric care and the value of patient-centered approaches in managing complex conditions like SMA. By emphasizing the importance of patient education, empowerment, and collaboration, this study underscores the potential of nursing theories to inform evidence-based practice and enhance patient outcomes. Similarly, a study by Irshad Ali [14] showed that the usability of theory in practice resulted in drastic changes in practice and patient’s early recovery.
Conclusion
In conclusion, this study provides valuable insights into applying nursing theories in pediatric nursing practice, particularly in managing SMA. By leveraging theoretical frameworks like Orem’s self-care deficit nursing theory, nurses can play a pivotal role in promoting self-care independence and improving outcomes for children with SMA and their families.
Study limitations
This study’s limitation is that only one patient was used in it. The findings would be improved by more research in the form of a longitudinal study with more participants.
Ethical Considerations
Compliance with ethical guidelines
Written and verbal consent was obtained from the patient who participated in the study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the patient who agreed to participate in the case.
References
- Prior TW, Leach ME, Finanger E. Spinal muscular atrophy. In: Adam MP, Feldman J, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Amemiya A, editors. GeneReviews. Seattle: University of Washington; 2020. [PMID]
- Guo W, Meng L, Cao L. Risk factors for recurrent respiratory tract infections and acute respiratory failure in children with spinal muscular atrophy. Pediatr Pulmonol. 2023; 58(2):507-15. [DOI:10.1002/ppul.26218] [PMID]
- Ross LF, Kwon JM. Spinal muscular atrophy: Past, present, and future. Neoreviews. 2019; 20(8):e437-51. [DOI:10.1542/neo.20-8-e437] [PMID]
- Nicolau S, Waldrop MA, Connolly AM, Mendell JR. Spinal muscular atrophy. Seminars in pediatric neurology. 2021; 37:100878. [DOI:10.1016/j.spen.2021.100878] [PMID]
- Garces E, Puyuelo G, Sánchez-Iglesias I, Francisco Del Rey JC, Cumplido C, Destarac M, et al. Using a robotic exoskeleton at home: An activity tolerance case study of a child with spinal muscular atrophy. J Pediatr Nurs. 2022; 67:e71-8. [DOI:10.1016/j.pedn.2022.09.014] [PMID]
- Rosero S, Weinstein J, Seabury J, Zizzi C, Wagner E, Varma A, et al. Disease burden in children with spinal muscular atrophy: Results from a large cross-sectional study. J Child Neurol. 2023; 38(1-2):52-63. [DOI:10.1177/08830738221135918] [PMID]
- Baranello G, Darras BT, Day JW, Deconinck N, Klein A, Masson R, et al. Risdiplam in type 1 spinal muscular atrophy. N Engl J Med. 2021; 384(10):915-23. [DOI:10.1056/NEJMoa2009965] [PMID]
- Zang J, Johannsen J, Denecke J, Weiss D, Koseki JC, Nießen A, et al. Flexible endoscopic evaluation of swallowing in children with type 1 spinal muscular atrophy. Eur Arch Oto-Rhino-Laryngology. 2023; 280(3):1329-38. [DOI:10.1007/s00405-022-07685-0] [PMID]
- Chen JY, Yen MH, Lin YH, Liu MC, Chen HS, Hu SH, et al. Testing the family health promotion model for family having children with Duchenne muscular dystrophy/spinal muscular atrophy. Adv Neurodev Disord. 2018; 2:391-401. [DOI:10.1007/s41252-018-0067-3]
- Ruta F, Ferrara P, Dal Mas F. “No SMA can hold”: Nursing care for children with spinal muscular atrophy. Descriptive analysis of two case studies. Rev Científica la Soc Española Enfermería Neurológica. 2023. [DOI:10.1016/j.sedene.2022.11.002]
- Murrell DV, Crawford CA, Jackson CT, Lotze TE, Wiemann CM. Identifying opportunities to provide family-centered care for families with children with type 1 spinal muscular atrophy. J Pediatr Nurs. 2018; 43:111-9. [DOI:10.1016/j.pedn.2018.09.007] [PMID]
- Inhestern L, Brandt M, Driemeyer J, Denecke J, Johannsen J, Bergelt C. Experiences of health care and psychosocial needs in parents of children with spinal muscular atrophy. Int J Environ Res Public Health. 2023; 20(7):5360. [DOI:10.3390/ijerph20075360] [PMID]
- Yang BH, Chung CY, Weng WC, Lo KW, Li YS. Self-care experiences of adolescents with spinal muscular atrophy. Asian Nurs Res (Korean Soc Nurs Sci). 2021; 15(4):231-8. [DOI:10.1016/j.anr.2021.07.002] [PMID]
- Irshad Ali BH. Application of Orem self care deficit theory on psychiatric patient. Ann Nurs Pr. 2018; 5(1):1093. [DOI: 10.47739/2379-9501/1093]
- Amir MD, Msf SQ ‘Aini, Sansuwito T bin. Relationship of knowledge and self-care according to dorothea E. Orem theory in hypertension elderly in the working Area of Takokak Public Health Center, Cianjur Regency, 2022. HIV Nurs. 2022; 22(2):3944-50. [Link]
- Hemmati Maslakpak M, Shahbaz A, Parizad N, Ghafourifard M. Preventing and managing diabetic foot ulcers: Application of Orem’s self-care model. Int J Diabetes Dev Ctries. 2018; 38:165-72. [DOI:10.1007/s13410-017-0570-5]
- Tan K, Karakas SA. The health literacy and self-efficacy levels of parents of patients with spinal muscular atrophy. Int J Caring Sci. 2022; 15(2):763. [Link]
- Awaliyah SN, SS, Budiati T. The application of nursing theory “self care orem” in nursing care of multiparous pregnancy with anaemia: A case report. J Matern Care Reprod Heal. 2018;1(2). [DOI:10.36780/jmcrh.v1i2.31]
- Hermalia I, Yetti K, Masfuri, Riyanto W. [Application of Orem self-care nursing model theory in diabetic nephropathy patients: A case study (Turkish)]. J Ris Kesehat. 2020; 12(2): 378-387. [DOI: 10.34011/juriskesbdg.v12i2.1790]
- Si Y, Yuan H, Ji P, Chen X. The combinative effects of orem self-care theory and PDCA nursing on cognitive function, neurological function and daily living ability in acute stroke. Am J Transl Res. 2021; 13(9):10493-500. [PMID]
Type of Study: Case & Review |
Subject:
Pediatric Rehabilitation
Received: 2023/06/1 | Accepted: 2023/11/11 | Published: 2024/01/1
Received: 2023/06/1 | Accepted: 2023/11/11 | Published: 2024/01/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









