Volume 12, Issue 3 (7-2024)
J. Pediatr. Rev 2024, 12(3): 233-242 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shokri E, Ghazi S. Instrumental Assessment for Pediatric Feeding Disorders in Infants Under Six Months: A Literature Review. J. Pediatr. Rev 2024; 12 (3) :233-242
URL: http://jpr.mazums.ac.ir/article-1-616-en.html
URL: http://jpr.mazums.ac.ir/article-1-616-en.html
1- Department of Speech Therapy, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Speech Therapy, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,shamimghazi1997@gmail.com
2- Department of Speech Therapy, School of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
Keywords: Instrumental feeding assessment, Swallowing analysis, Aspiration, Penetration, Infant, Neonate, Newborn
Full-Text [PDF 503 kb]
(973 Downloads)
| Abstract (HTML) (2033 Views)
Full-Text: (1099 Views)
Introduction
Neurodevelopmental disabilities in infants can cause feeding and swallowing disorders. During the fetal period, swallowing functions begin to develop. The coordination between sucking and swallowing is usually established between 32 and 34 weeks of gestation, and becomes fully rational by 37 weeks of gestation. Several life-threatening neonatal diseases cause dysphagia, including premature birth, cardiopulmonary conditions, and neurological disorders. Additionally, negative experiences related to feeding, such as intubation, tube feeding and airway suctioning, may further impair sucking and swallowing [1]. Serious consequences associated with abnormal feeding and swallowing can include stunted growth and respiratory complications, such as aspiration pneumonia [1]. Early identification of feeding and swallowing impairments will enable the appropriate healthcare professionals to provide careful monitoring and/or assessment to mitigate potential serious complications. Nevertheless, an infant’s natural physiologic and anatomic changes make assessing and treating abnormal swallowing particularly challenging [2].
Speech-language pathologists (SLPs) have played crucial parts in the assessment and management of feeding disorders in infants for more than five periods [3, 4]. The prevalence of feeding disorders in infants has increased as a result of medical and surgical advancements [5, 6]. Newborns, infants and young children with these problems or indicative disorders related to feeding disorders may need information provided by particular studies that measure specific aspects of anatomy, physiology, and basic pathophysiology of swallowing function, which are not detectable through instrumental and non-instrumental assessments [7]. These specific studies use investigative modalities that go beyond the data obtained from comprehensive instrumental and non-instrumental assessments [8].
In non-instrumental assessments, we use chart reviews, parent reports, oral mechanism assessments, cranial nerve tests, and food/liquid trials to evaluate an infant’s swallowing and feeding skills [9, 10]. However, this information is occasionally insufficient, as we need more data to determine why the infant is experiencing difficulty with feeding and swallowing, especially if the infant shows signs and symptoms of aspiration [3, 11]. Non-instrumental examinations fail to reveal structural and functional aspects of swallowing [4, 12]. They can address detailed inquiries regarding the occurrence and extent of feeding disorders, safety during feeding, and the effectiveness of therapeutic strategies [9, 12-14]. The majority of healthcare professionals recognize the importance of instrumental swallowing assessments in hospitals. In the context of infants, the videofluoroscopic swallowing study (VFSS) and the fiberoptic endoscopic swallowing evaluation (FEES) are the most commonly used instrumental assessments [4, 9, 12, 14]. Although bedside feeding evaluations may detect clinical signs or behaviors of dysphagia, instrumental examinations are the only way to confirm laryngeal penetration or aspiration. A fluoroscopic and/or endoscopic examination may be performed as part of an instrumental examination [15]. SLPs use both methods in the neonatal intensive care unit (NICU) to assess oropharyngeal anatomy and physiology, control swallowing safety, evaluate intervention strategies, and develop a functional and safe feeding plan [4, 9].
SLPs collaborate with the medical team to determine which examination is more suitable based on the patient’s individual needs and the evidence we aim to obtain. Therefore, we focused on studies that investigated instrumental assessments for pediatric feeding disorders in infants under six months.
Instrumental assessment in infants
Infants experiencing feeding and swallowing difficulties require a comprehensive, long-term approach involving a multidisciplinary team. Clinicians must determine whether an instrumental swallowing assessment is needed and, if so, which type is appropriate. Timely and accurate identification, along with intervention, can significantly decrease the risk of the infant developing additional conditions related to dysphagia [16].
In clinical evaluations, we employ various methods, such ::as char::t reviews, feedback from parents, oral mechanism assessments, cranial nerve evaluations and trials with food and liquids to evaluate the infant’s swallowing safety and feeding abilities [17]. However, these methods may sometimes be insufficient. To better understand the underlying reasons for an infant’s feeding and swallowing challenges—particularly in cases where there are indications of aspiration—instrumental assessments can be crucial for diagnosis [18].
Instrumental assessments evaluate both the functional and structural components of swallowing that cannot be observed through physical examination. These assessments provide critical insights regarding the presence and severity of swallowing dysfunction, feeding safety, and the efficacy of various therapeutic approaches [19]. Most healthcare professionals in hospitals recognize the importance of conducting instrumental swallowing assessments [18]. For physicians who are hesitant about additional testing, I emphasize the valuable information these assessments provide, such as uncovering the underlying causes of feeding and swallowing issues and identifying safe feeding strategies [16].
The two most frequently utilized instrumental assessments for infants are the VFSS and the FEES. In the NICU, we employ both methods to evaluate oropharyngeal anatomy and physiology, ascertain swallowing safety, assess intervention techniques, and create a functional and safe feeding plan [20]. We collaborate with the medical team to select the most suitable exam based on the specific needs of the patient and the information we aim to obtain.
VFSS
The VFSS is a radiographic procedure that offers a dynamic view of the swallowing process [20]. During this assessment, we can adjust various factors such as the delivery method, and liquid viscosity, or apply therapeutic swallowing techniques—like external pacing or chin tuck—to enhance the safety and efficiency of swallowing [18]. It is essential that the infant’s positioning and the utensils used during the study reflect real-life feeding scenarios. If there are clinical concerns regarding how the infant’s oral motor skills impact the pharyngeal phase of swallowing, the VFSS can provide valuable insights [19].
To minimize radiation exposure, we adhere to as low as reasonably achievable (ALARA) principles and using a standardized commercial barium product helps reduce variability across studies. Video swallow studies can be conducted with infants of any age, including those who have reached term age and older. The medical team should carefully consider how often this examination is repeated in the pediatric population [21].
The VFSS serves as the primary instrumental evaluation for dynamic imaging of the upper oral, pharyngeal, and esophageal stages of swallowing [22]. It is important to note that this examination captures only a brief moment and does not replicate a full meal. Its main objective is to assess the pharyngeal phase of swallowing rather than solely to identify aspiration [23]. When aspiration is observed, clinicians must document whether it occurred before, during, or after the evaluation and identify the specific textures or consistencies involved [24]. The findings should be interpreted in conjunction with the infant’s medical history, other diagnostic tests, and multidimensional data that contribute to understanding the current situation of the infant and family [25].
Fiberoptic endoscopic evaluation of swallowing
By viewing the upper aerodigestive tract through a transnasal endoscope during swallowing, FEES provides specific information about the pharyngeal phase of swallowing [16]. This procedure is usually performed by a multidisciplinary team of an SLP, an otolaryngologist, and a nurse [25]. For many years, FEES has been used successfully in infants and is considered safe and reliable for all newborns, including NICU infants at term and older [26]. It is imperative that the infant is cooperative to gain meaningful swallowing information; therefore, it is important to take into account the infant’s age, developmental stage, and diagnosis when predicting compliance [16]. In cases of suspected airway abnormalities affecting swallowing function or when assessing swallowing in a breastfeeding infant, FEES exams are recommended.
The laboratory developed FEES as a supplement to VFSS and for testing swallowing function in adults, children and infants [27]. FEES may be used in conjunction with VFSS in some cases. Over the past few years, technology has improved to the point where it is possible to integrate FEES with VFSS in a single patient [28].
Methods
Identification of instrumental assessments
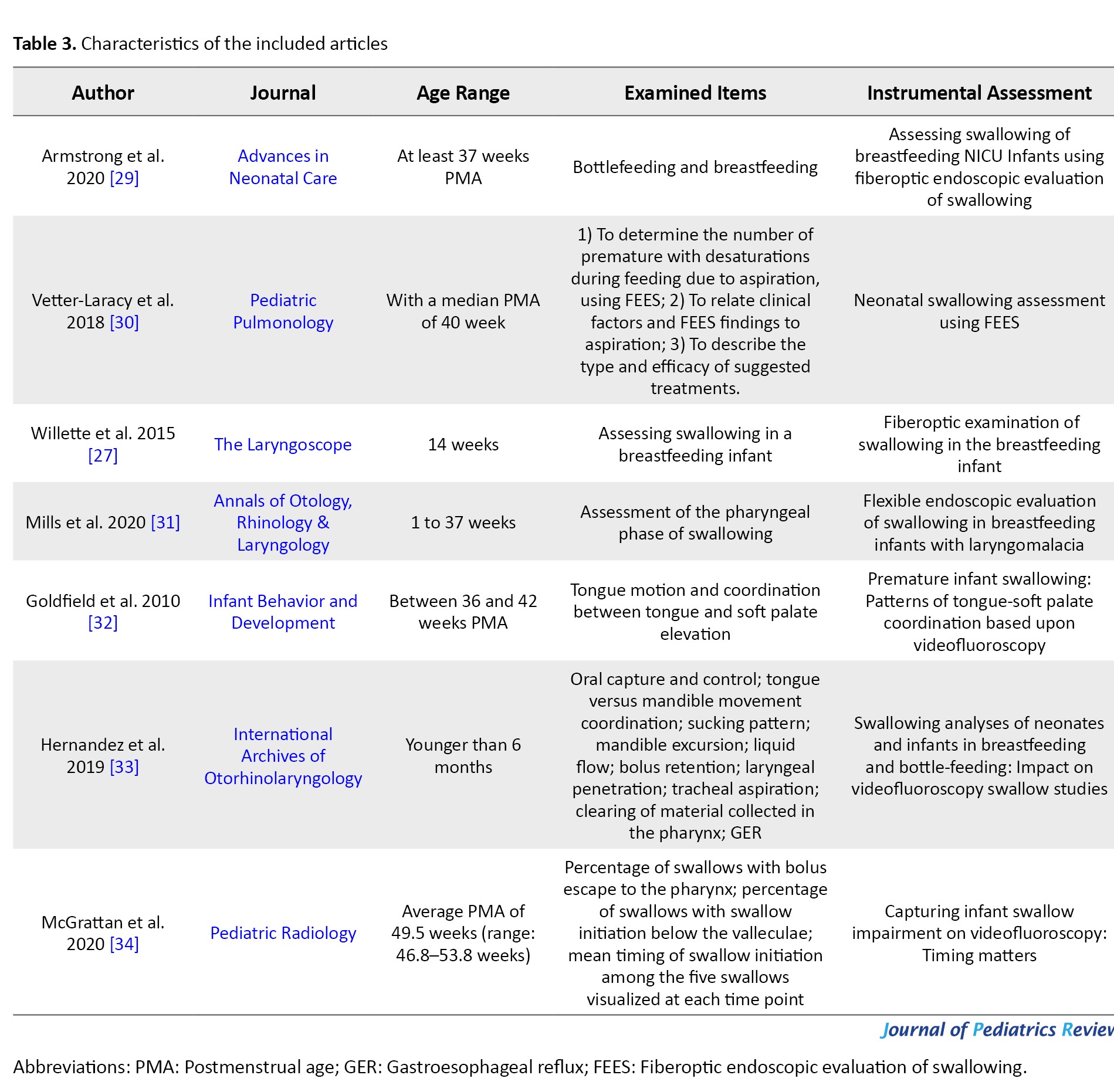
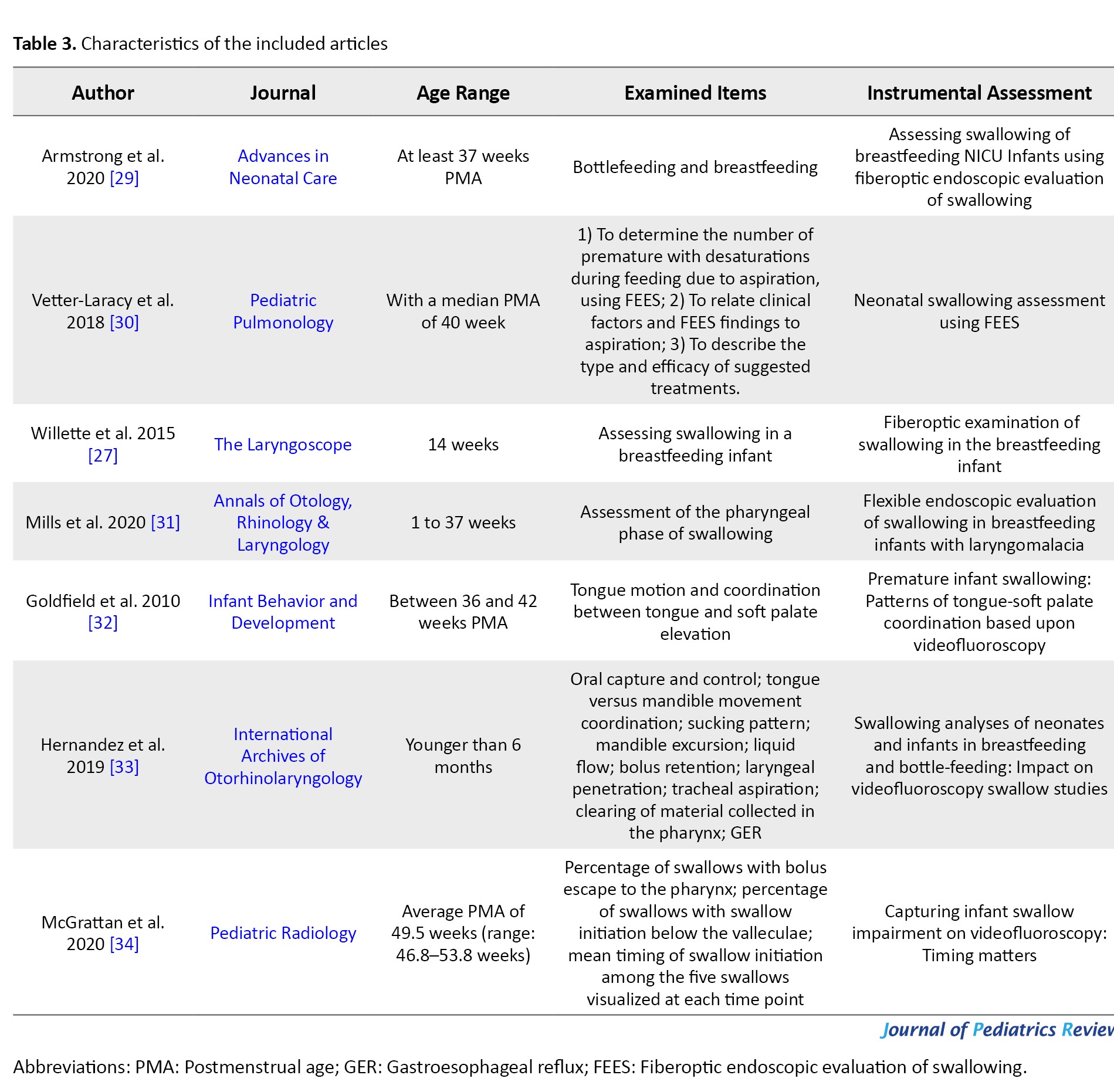
A systematic overview of seven published instrumental assessments was performed to evaluate infants’ feeding skills (Tables 1 and 2).


The criteria for inclusion of assessment tools were as follows: a) They evaluated feeding skills, b) They included evaluations for which articles were obtainable and available and c) They could be acquired or provided by the authors of this article. A list of usability evaluations was created based on the following sources:
Source 1) This paper has compiled a database of instrumental assessments for infants over the past 20 years. The purpose was to keep a record of instrumental assessments by reviewing journal articles, attending lectures, visiting speech therapy clinics and contacting colleagues.
Source 2) There were no limitations on the year of publication or the requirements for full-text articles. Each title and abstract was reviewed, resulting in the identification of seven papers. To enhance understanding and evaluation, the tools mentioned are explained further below (Table 3).
Obtaining instrumental assessments
A comprehensive search was conducted in databases including EMBASE, Scopus, Medline (via PubMed), Google Scholar, ProQuest and Cochrane from December 2000 to May 2023. The keywords and search strategies used in different databases were Instrumental (feeding assessment) OR (swallowing) OR (analysis) AND (aspiration) OR (penetration) AND (infant) OR (neonate) OR (newborn). As part of the complete database search, the reference lists of the searched articles were evaluated, and specialists in this field were consulted to submit related studies.
Appraisal criteria
The following inclusion criteria were applied to the included studies:
1) Selected keywords were confined to the title or abstract; 2) Published between December 2000 and May 2023.
Based on the inclusion criteria, a total of 1287 articles were included. Two authors individually revised the abstracts of all included studies. A total of 1280 articles were excluded based on the following exclusion criteria:
1) Both authors agreed that the article was not relevant to the research objectives (480 articles); 2) Articles that included children, adolescents, or adult participants (800 articles).
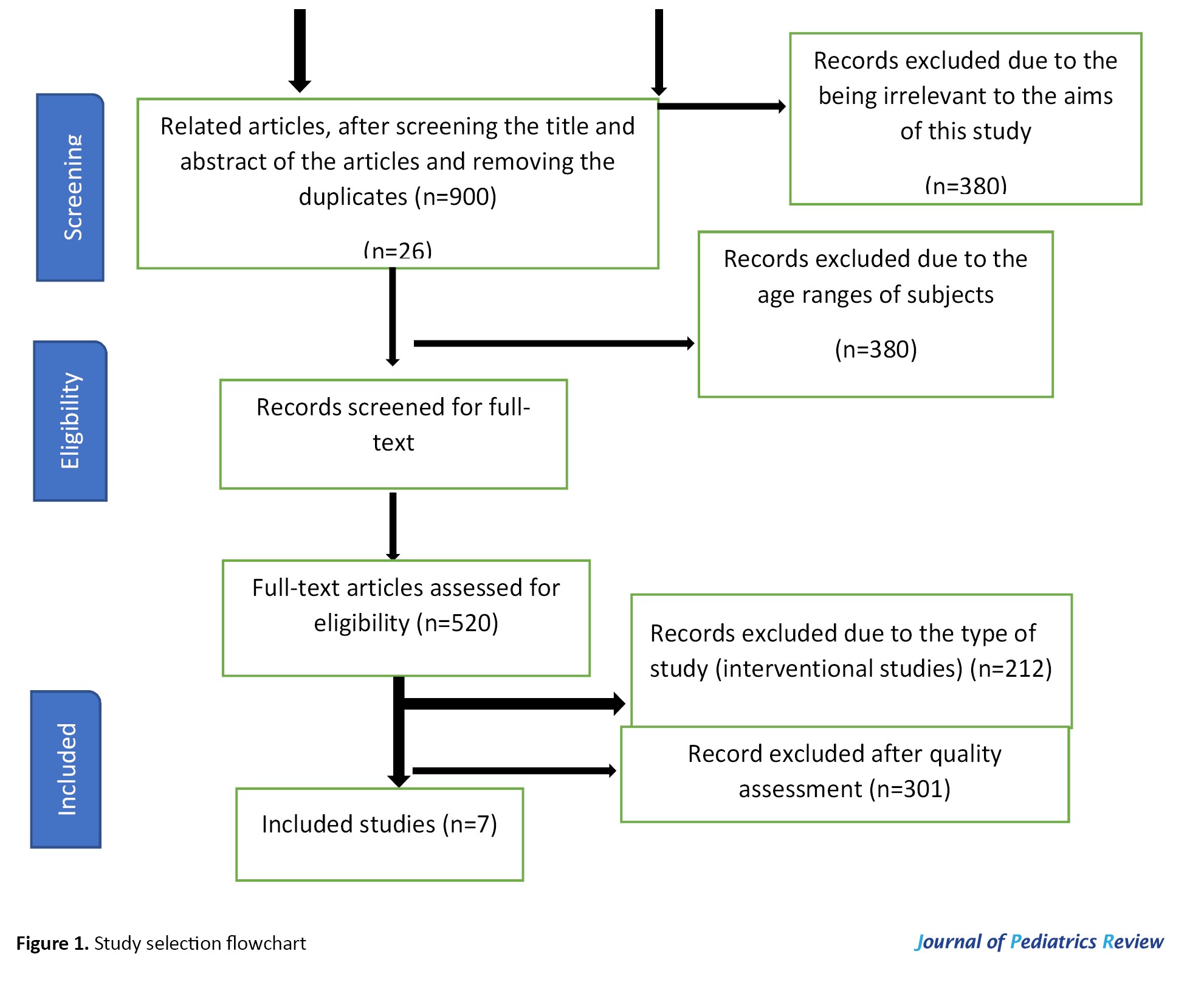
As a result, seven articles remained that were completely downloaded and appraised for quality (Figure 1).
Reviewers
The authors of this article (hereafter referred to as the reviewers) had experience in working with instrumental assessments and a good knowledge of English.
Quality
To evaluate the remaining seven cross-sectional assessments, we utilized the Newcastle Ottawa scale (NOS) checklist. This tool rates articles based on three factors: sample selection (four questions), subject comparability (one question), and statistical methods and outcomes (two questions). According to the scoring guidelines, studies scoring above seven are considered good quality, those scoring below four are deemed poor quality, and those with scores of 5-6 are considered satisfactory.
Two independent raters completed the quality assessment scale for each article to confirm their quality. After evaluating the scores, we included and thoroughly reviewed seven studies that received scores of 5 to 10 from both raters. Figure 1 provides a detailed overview of the inclusion and exclusion processes.
Results
The conceptual and operational assessments
FEES studies
There were many similarities in the conceptual and operational between the assessments. They evaluate different swallowing components, which include feeding difficulties, noisy breathing, direct aspiration, penetration, signs of dynamic airway obstruction, and compromised airway protection during swallowing [27, 29-31]. According to the research conducted within the framework of this study, it should be mentioned that no adverse occasions, including mortality, epistaxis, or laryngospasm were reported during procedures and all four studies provided detailed accounts of the processes. Only two studies included statistical analysis at the end of the methods section [29, 30], while the other studies presented this information in the table of results section [27, 31]. Additionally, all of the studies reported that the FEES exam is one of the safe and effective assessments for feeding infants.
VFS studies
The studies analyzed various aspects of swallowing and liquids, including the coordination between individual tongue points and soft palate movements, as well as the similarities and differences in infant swallowing function (oral capture and control, coordination of tongue versus mandible movement, sucking patterns, mandible excursion, liquid flow, bolus retention, laryngeal penetration, tracheal aspiration, clearing of material in the pharynx and gastroesophageal reflux [GER]), components of swallow physiology (oral bolus hold, initiation of pharyngeal swallow, timing of swallow initiation) and airway protection mechanisms (penetration and aspiration) [32-35]. All of the studies reported the variables in charts or tables. In the investigation conducted for this study, it is significant to highlight the absence of any adverse incidents throughout the procedures, which have been meticulously documented to ensure thorough comprehension.
Furthermore, it is worth mentioning that across all studies examined, there were no indications of inefficiencies associated with the VFSS method for assessing infant feeding.
Sample selection and size
This study aimed to review accessible feeding assessments that are safe for infants under six months. The sample size for the FEES studies does not differ significantly among the included studies, ranging from 24 to 26 participants, with only one study reviewing 62 infants [30 ]. Also, all of the studies reported demographic information, such as gestational age, age at testing, birth weight, weight at testing, time of wearing a nasogastric/orogastric and gender. The sample sizes for the VFSS studies varied, ranging from 25 to 30 participants, while one study reported on 12 infants [32]. All the studies reported demographic characteristics, and one study detailed primary diagnosis and indications for VFSS [34]. The infants reported were aged 0 to 6 months (Table 3).
Discussion
The two accessible methods for instrumental assessment of swallowing are the VFSS and the FEES. Both measures have benefits and limitations that were defined in this article. Although both methods are very practical and valid, researchers have different opinions regarding their advantages and disadvantages. Some researchers advocate for the VFSS method, while others consider FEES to be more beneficial for infants.
Currently, the most common evaluation method is an observational clinical feeding and swallowing examination followed by a VFSS if deemed necessary [26]. Although VFSS is frequently used, its reliability in detecting laryngeal penetration (material entering the laryngeal vestibule) or tracheal aspiration (material entering the trachea below the vocal folds) in infants has not been well-documented [15, 36, 37]. The reliability of VFSS in identifying penetration and aspiration in adults and children ranges from moderate to excellent [26]. However, VFSS has significant limitations for NICU infants, such as transportation to radiology, radiation exposure, use of barium, limited assessment time, and nonphysiological feeding positions [15, 26, 38].
On the other hand, FEES has been reported to be safe and reliable (comparable to VFSS) [15, 26, 38]. FEES has been used in the pediatric population for over two decades, with several studies demonstrating its safety and reliability in identifying penetration and aspiration in infants [39].
A comprehensive review of the instrumental assessments (FEES and VFSS) reported that VFSS has several limitations, including radiation exposure, transportation to the radiology suite, and, notably, the inability to assess the mother-infant dyad during breastfeeding. FEES, on the other hand, avoids these limitations and is now considered a secure and substantial alternative in a comprehensive feeding and swallowing assessment [31]. FEES also allows for the assessment of secretion management prior to breastfeeding, as well as the visualization of laryngeal penetration and tracheal aspiration [31, 39].
Thus, FEES could be an important clinical instrument that has advanced our understanding of swallowing when evaluating infants with laryngomalacia who are encountering trouble feeding. Moreover, FEES has provided endoscopic evidence for the potential use of infant positioning as a modifiable variable, by elucidating the effect of infant position on dynamic airway compromise and liquid flow during the pharyngeal stage of swallowing. Also, we have recognized several particular anatomical and physiological factors related to an increased risk of penetration and/or aspiration through FEES.
VFSS is a radiographic procedure that uses fluoroscopy to visualize the oral, pharyngeal, and esophageal phases of swallowing. This method allows for a comprehensive assessment of the swallowing mechanism, including the identification of aspiration, penetration, and residue. However, VFSS exposes the infant to ionizing radiation, which is a concern for this vulnerable population. Additionally, the administration of barium-coated substances may alter the taste and texture of the food, potentially affecting the infant’s feeding behavior. Furthermore, the supine position required for VFSS may not be representative of the infant’s typical feeding position, potentially limiting the ecological validity of the assessment. In contrast, FEES is an endoscopic procedure that involves the insertion of a flexible laryngoscope through the infant’s nasal passage to visualize the pharyngeal and laryngeal structures during swallowing. This method allows for the assessment of the pharyngeal phase of swallowing, with a particular focus on the function of the vocal folds and laryngeal closure [40, 41]. FEES does not expose the infant to radiation and does not require the use of barium-coated substances, making it a safer and more naturalistic assessment. Additionally, FEES can be performed in the infant’s typical feeding position, providing a more ecologically valid assessment of swallowing function. However, FEES is limited in its ability to assess the esophageal phase of swallowing and may not be suitable for infants with severe respiratory compromise or anatomic abnormalities that preclude nasal insertion of the endoscope [42].
One of the primary advantages of VFSS is its ability to provide a comprehensive evaluation of the entire swallowing process, including the oral, pharyngeal, and esophageal phases. This allows for a more complete understanding of the underlying causes of dysphagia and can help guide treatment decisions. In contrast, FEES is limited to the evaluation of the pharyngeal and laryngeal structures. VFSS is also highly sensitive for detecting silent aspiration, which is when food or liquid enters the airway without the individual showing outward signs of distress. This is a critical benefit for individuals who are at risk for aspiration pneumonia, as early detection and management of silent aspiration can help prevent this potentially life-threatening complication. Another advantage of VFSS is its ability to provide quantitative measures of swallowing function, such as the timing and duration of swallowing events [43]. These measures can be used to track progress over time and assess the effectiveness of interventions. In contrast, FEES provides qualitative information about swallowing function but does not provide quantitative data. Finally, VFSS is generally well-tolerated by patients and does not require the insertion of an endoscope, which can be uncomfortable for some individuals. This can be an important consideration when selecting an assessment tool, particularly for individuals who may have difficulty cooperating with the procedure. While FEES has its advantages, such as the ability to directly visualize the pharyngeal and laryngeal structures and the absence of radiation exposure, VFSS is a valuable tool for assessing dysphagia and provides important information that can guide treatment decisions and improve outcomes for individuals with swallowing impairments. The choice of assessment tool should be based on the specific needs and circumstances of the individual and should be made in consultation with a speech-language pathologist or other qualified healthcare professional [44].
Clinicians should carefully consider the strengths and limitations of each assessment, as well as the specific needs and circumstances of the infant when selecting the most appropriate method for evaluating dysphagia in this population. Ultimately, a comprehensive and individualized approach to the assessment and management of dysphagia in infants is essential for optimizing swallowing function and promoting positive feeding outcomes.
Conclusion
Even though both the FEES and VFSS approaches are essential for evaluating infant feeding, the approximate validity and reliability of established conventions for instrumental assessment within the neonatal and pediatric populations are limited. Therefore, further investigations should focus on advancing studies aimed at developing standardized and approved conventions for instrumental appraisals in these populations.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank physicians, nurses and the parents of infants in hospitals in Tehran.
Neurodevelopmental disabilities in infants can cause feeding and swallowing disorders. During the fetal period, swallowing functions begin to develop. The coordination between sucking and swallowing is usually established between 32 and 34 weeks of gestation, and becomes fully rational by 37 weeks of gestation. Several life-threatening neonatal diseases cause dysphagia, including premature birth, cardiopulmonary conditions, and neurological disorders. Additionally, negative experiences related to feeding, such as intubation, tube feeding and airway suctioning, may further impair sucking and swallowing [1]. Serious consequences associated with abnormal feeding and swallowing can include stunted growth and respiratory complications, such as aspiration pneumonia [1]. Early identification of feeding and swallowing impairments will enable the appropriate healthcare professionals to provide careful monitoring and/or assessment to mitigate potential serious complications. Nevertheless, an infant’s natural physiologic and anatomic changes make assessing and treating abnormal swallowing particularly challenging [2].
Speech-language pathologists (SLPs) have played crucial parts in the assessment and management of feeding disorders in infants for more than five periods [3, 4]. The prevalence of feeding disorders in infants has increased as a result of medical and surgical advancements [5, 6]. Newborns, infants and young children with these problems or indicative disorders related to feeding disorders may need information provided by particular studies that measure specific aspects of anatomy, physiology, and basic pathophysiology of swallowing function, which are not detectable through instrumental and non-instrumental assessments [7]. These specific studies use investigative modalities that go beyond the data obtained from comprehensive instrumental and non-instrumental assessments [8].
In non-instrumental assessments, we use chart reviews, parent reports, oral mechanism assessments, cranial nerve tests, and food/liquid trials to evaluate an infant’s swallowing and feeding skills [9, 10]. However, this information is occasionally insufficient, as we need more data to determine why the infant is experiencing difficulty with feeding and swallowing, especially if the infant shows signs and symptoms of aspiration [3, 11]. Non-instrumental examinations fail to reveal structural and functional aspects of swallowing [4, 12]. They can address detailed inquiries regarding the occurrence and extent of feeding disorders, safety during feeding, and the effectiveness of therapeutic strategies [9, 12-14]. The majority of healthcare professionals recognize the importance of instrumental swallowing assessments in hospitals. In the context of infants, the videofluoroscopic swallowing study (VFSS) and the fiberoptic endoscopic swallowing evaluation (FEES) are the most commonly used instrumental assessments [4, 9, 12, 14]. Although bedside feeding evaluations may detect clinical signs or behaviors of dysphagia, instrumental examinations are the only way to confirm laryngeal penetration or aspiration. A fluoroscopic and/or endoscopic examination may be performed as part of an instrumental examination [15]. SLPs use both methods in the neonatal intensive care unit (NICU) to assess oropharyngeal anatomy and physiology, control swallowing safety, evaluate intervention strategies, and develop a functional and safe feeding plan [4, 9].
SLPs collaborate with the medical team to determine which examination is more suitable based on the patient’s individual needs and the evidence we aim to obtain. Therefore, we focused on studies that investigated instrumental assessments for pediatric feeding disorders in infants under six months.
Instrumental assessment in infants
Infants experiencing feeding and swallowing difficulties require a comprehensive, long-term approach involving a multidisciplinary team. Clinicians must determine whether an instrumental swallowing assessment is needed and, if so, which type is appropriate. Timely and accurate identification, along with intervention, can significantly decrease the risk of the infant developing additional conditions related to dysphagia [16].
In clinical evaluations, we employ various methods, such ::as char::t reviews, feedback from parents, oral mechanism assessments, cranial nerve evaluations and trials with food and liquids to evaluate the infant’s swallowing safety and feeding abilities [17]. However, these methods may sometimes be insufficient. To better understand the underlying reasons for an infant’s feeding and swallowing challenges—particularly in cases where there are indications of aspiration—instrumental assessments can be crucial for diagnosis [18].
Instrumental assessments evaluate both the functional and structural components of swallowing that cannot be observed through physical examination. These assessments provide critical insights regarding the presence and severity of swallowing dysfunction, feeding safety, and the efficacy of various therapeutic approaches [19]. Most healthcare professionals in hospitals recognize the importance of conducting instrumental swallowing assessments [18]. For physicians who are hesitant about additional testing, I emphasize the valuable information these assessments provide, such as uncovering the underlying causes of feeding and swallowing issues and identifying safe feeding strategies [16].
The two most frequently utilized instrumental assessments for infants are the VFSS and the FEES. In the NICU, we employ both methods to evaluate oropharyngeal anatomy and physiology, ascertain swallowing safety, assess intervention techniques, and create a functional and safe feeding plan [20]. We collaborate with the medical team to select the most suitable exam based on the specific needs of the patient and the information we aim to obtain.
VFSS
The VFSS is a radiographic procedure that offers a dynamic view of the swallowing process [20]. During this assessment, we can adjust various factors such as the delivery method, and liquid viscosity, or apply therapeutic swallowing techniques—like external pacing or chin tuck—to enhance the safety and efficiency of swallowing [18]. It is essential that the infant’s positioning and the utensils used during the study reflect real-life feeding scenarios. If there are clinical concerns regarding how the infant’s oral motor skills impact the pharyngeal phase of swallowing, the VFSS can provide valuable insights [19].
To minimize radiation exposure, we adhere to as low as reasonably achievable (ALARA) principles and using a standardized commercial barium product helps reduce variability across studies. Video swallow studies can be conducted with infants of any age, including those who have reached term age and older. The medical team should carefully consider how often this examination is repeated in the pediatric population [21].
The VFSS serves as the primary instrumental evaluation for dynamic imaging of the upper oral, pharyngeal, and esophageal stages of swallowing [22]. It is important to note that this examination captures only a brief moment and does not replicate a full meal. Its main objective is to assess the pharyngeal phase of swallowing rather than solely to identify aspiration [23]. When aspiration is observed, clinicians must document whether it occurred before, during, or after the evaluation and identify the specific textures or consistencies involved [24]. The findings should be interpreted in conjunction with the infant’s medical history, other diagnostic tests, and multidimensional data that contribute to understanding the current situation of the infant and family [25].
Fiberoptic endoscopic evaluation of swallowing
By viewing the upper aerodigestive tract through a transnasal endoscope during swallowing, FEES provides specific information about the pharyngeal phase of swallowing [16]. This procedure is usually performed by a multidisciplinary team of an SLP, an otolaryngologist, and a nurse [25]. For many years, FEES has been used successfully in infants and is considered safe and reliable for all newborns, including NICU infants at term and older [26]. It is imperative that the infant is cooperative to gain meaningful swallowing information; therefore, it is important to take into account the infant’s age, developmental stage, and diagnosis when predicting compliance [16]. In cases of suspected airway abnormalities affecting swallowing function or when assessing swallowing in a breastfeeding infant, FEES exams are recommended.
The laboratory developed FEES as a supplement to VFSS and for testing swallowing function in adults, children and infants [27]. FEES may be used in conjunction with VFSS in some cases. Over the past few years, technology has improved to the point where it is possible to integrate FEES with VFSS in a single patient [28].
Methods
Identification of instrumental assessments
A systematic overview of seven published instrumental assessments was performed to evaluate infants’ feeding skills (Tables 1 and 2).


The criteria for inclusion of assessment tools were as follows: a) They evaluated feeding skills, b) They included evaluations for which articles were obtainable and available and c) They could be acquired or provided by the authors of this article. A list of usability evaluations was created based on the following sources:
Source 1) This paper has compiled a database of instrumental assessments for infants over the past 20 years. The purpose was to keep a record of instrumental assessments by reviewing journal articles, attending lectures, visiting speech therapy clinics and contacting colleagues.
Source 2) There were no limitations on the year of publication or the requirements for full-text articles. Each title and abstract was reviewed, resulting in the identification of seven papers. To enhance understanding and evaluation, the tools mentioned are explained further below (Table 3).
Obtaining instrumental assessments
A comprehensive search was conducted in databases including EMBASE, Scopus, Medline (via PubMed), Google Scholar, ProQuest and Cochrane from December 2000 to May 2023. The keywords and search strategies used in different databases were Instrumental (feeding assessment) OR (swallowing) OR (analysis) AND (aspiration) OR (penetration) AND (infant) OR (neonate) OR (newborn). As part of the complete database search, the reference lists of the searched articles were evaluated, and specialists in this field were consulted to submit related studies.
Appraisal criteria
The following inclusion criteria were applied to the included studies:
1) Selected keywords were confined to the title or abstract; 2) Published between December 2000 and May 2023.
Based on the inclusion criteria, a total of 1287 articles were included. Two authors individually revised the abstracts of all included studies. A total of 1280 articles were excluded based on the following exclusion criteria:
1) Both authors agreed that the article was not relevant to the research objectives (480 articles); 2) Articles that included children, adolescents, or adult participants (800 articles).
As a result, seven articles remained that were completely downloaded and appraised for quality (Figure 1).
Reviewers
The authors of this article (hereafter referred to as the reviewers) had experience in working with instrumental assessments and a good knowledge of English.
Quality
To evaluate the remaining seven cross-sectional assessments, we utilized the Newcastle Ottawa scale (NOS) checklist. This tool rates articles based on three factors: sample selection (four questions), subject comparability (one question), and statistical methods and outcomes (two questions). According to the scoring guidelines, studies scoring above seven are considered good quality, those scoring below four are deemed poor quality, and those with scores of 5-6 are considered satisfactory.
Two independent raters completed the quality assessment scale for each article to confirm their quality. After evaluating the scores, we included and thoroughly reviewed seven studies that received scores of 5 to 10 from both raters. Figure 1 provides a detailed overview of the inclusion and exclusion processes.
Results
The conceptual and operational assessments
FEES studies
There were many similarities in the conceptual and operational between the assessments. They evaluate different swallowing components, which include feeding difficulties, noisy breathing, direct aspiration, penetration, signs of dynamic airway obstruction, and compromised airway protection during swallowing [27, 29-31]. According to the research conducted within the framework of this study, it should be mentioned that no adverse occasions, including mortality, epistaxis, or laryngospasm were reported during procedures and all four studies provided detailed accounts of the processes. Only two studies included statistical analysis at the end of the methods section [29, 30], while the other studies presented this information in the table of results section [27, 31]. Additionally, all of the studies reported that the FEES exam is one of the safe and effective assessments for feeding infants.
VFS studies
The studies analyzed various aspects of swallowing and liquids, including the coordination between individual tongue points and soft palate movements, as well as the similarities and differences in infant swallowing function (oral capture and control, coordination of tongue versus mandible movement, sucking patterns, mandible excursion, liquid flow, bolus retention, laryngeal penetration, tracheal aspiration, clearing of material in the pharynx and gastroesophageal reflux [GER]), components of swallow physiology (oral bolus hold, initiation of pharyngeal swallow, timing of swallow initiation) and airway protection mechanisms (penetration and aspiration) [32-35]. All of the studies reported the variables in charts or tables. In the investigation conducted for this study, it is significant to highlight the absence of any adverse incidents throughout the procedures, which have been meticulously documented to ensure thorough comprehension.
Furthermore, it is worth mentioning that across all studies examined, there were no indications of inefficiencies associated with the VFSS method for assessing infant feeding.
Sample selection and size
This study aimed to review accessible feeding assessments that are safe for infants under six months. The sample size for the FEES studies does not differ significantly among the included studies, ranging from 24 to 26 participants, with only one study reviewing 62 infants [30 ]. Also, all of the studies reported demographic information, such as gestational age, age at testing, birth weight, weight at testing, time of wearing a nasogastric/orogastric and gender. The sample sizes for the VFSS studies varied, ranging from 25 to 30 participants, while one study reported on 12 infants [32]. All the studies reported demographic characteristics, and one study detailed primary diagnosis and indications for VFSS [34]. The infants reported were aged 0 to 6 months (Table 3).
Discussion
The two accessible methods for instrumental assessment of swallowing are the VFSS and the FEES. Both measures have benefits and limitations that were defined in this article. Although both methods are very practical and valid, researchers have different opinions regarding their advantages and disadvantages. Some researchers advocate for the VFSS method, while others consider FEES to be more beneficial for infants.
Currently, the most common evaluation method is an observational clinical feeding and swallowing examination followed by a VFSS if deemed necessary [26]. Although VFSS is frequently used, its reliability in detecting laryngeal penetration (material entering the laryngeal vestibule) or tracheal aspiration (material entering the trachea below the vocal folds) in infants has not been well-documented [15, 36, 37]. The reliability of VFSS in identifying penetration and aspiration in adults and children ranges from moderate to excellent [26]. However, VFSS has significant limitations for NICU infants, such as transportation to radiology, radiation exposure, use of barium, limited assessment time, and nonphysiological feeding positions [15, 26, 38].
On the other hand, FEES has been reported to be safe and reliable (comparable to VFSS) [15, 26, 38]. FEES has been used in the pediatric population for over two decades, with several studies demonstrating its safety and reliability in identifying penetration and aspiration in infants [39].
A comprehensive review of the instrumental assessments (FEES and VFSS) reported that VFSS has several limitations, including radiation exposure, transportation to the radiology suite, and, notably, the inability to assess the mother-infant dyad during breastfeeding. FEES, on the other hand, avoids these limitations and is now considered a secure and substantial alternative in a comprehensive feeding and swallowing assessment [31]. FEES also allows for the assessment of secretion management prior to breastfeeding, as well as the visualization of laryngeal penetration and tracheal aspiration [31, 39].
Thus, FEES could be an important clinical instrument that has advanced our understanding of swallowing when evaluating infants with laryngomalacia who are encountering trouble feeding. Moreover, FEES has provided endoscopic evidence for the potential use of infant positioning as a modifiable variable, by elucidating the effect of infant position on dynamic airway compromise and liquid flow during the pharyngeal stage of swallowing. Also, we have recognized several particular anatomical and physiological factors related to an increased risk of penetration and/or aspiration through FEES.
VFSS is a radiographic procedure that uses fluoroscopy to visualize the oral, pharyngeal, and esophageal phases of swallowing. This method allows for a comprehensive assessment of the swallowing mechanism, including the identification of aspiration, penetration, and residue. However, VFSS exposes the infant to ionizing radiation, which is a concern for this vulnerable population. Additionally, the administration of barium-coated substances may alter the taste and texture of the food, potentially affecting the infant’s feeding behavior. Furthermore, the supine position required for VFSS may not be representative of the infant’s typical feeding position, potentially limiting the ecological validity of the assessment. In contrast, FEES is an endoscopic procedure that involves the insertion of a flexible laryngoscope through the infant’s nasal passage to visualize the pharyngeal and laryngeal structures during swallowing. This method allows for the assessment of the pharyngeal phase of swallowing, with a particular focus on the function of the vocal folds and laryngeal closure [40, 41]. FEES does not expose the infant to radiation and does not require the use of barium-coated substances, making it a safer and more naturalistic assessment. Additionally, FEES can be performed in the infant’s typical feeding position, providing a more ecologically valid assessment of swallowing function. However, FEES is limited in its ability to assess the esophageal phase of swallowing and may not be suitable for infants with severe respiratory compromise or anatomic abnormalities that preclude nasal insertion of the endoscope [42].
One of the primary advantages of VFSS is its ability to provide a comprehensive evaluation of the entire swallowing process, including the oral, pharyngeal, and esophageal phases. This allows for a more complete understanding of the underlying causes of dysphagia and can help guide treatment decisions. In contrast, FEES is limited to the evaluation of the pharyngeal and laryngeal structures. VFSS is also highly sensitive for detecting silent aspiration, which is when food or liquid enters the airway without the individual showing outward signs of distress. This is a critical benefit for individuals who are at risk for aspiration pneumonia, as early detection and management of silent aspiration can help prevent this potentially life-threatening complication. Another advantage of VFSS is its ability to provide quantitative measures of swallowing function, such as the timing and duration of swallowing events [43]. These measures can be used to track progress over time and assess the effectiveness of interventions. In contrast, FEES provides qualitative information about swallowing function but does not provide quantitative data. Finally, VFSS is generally well-tolerated by patients and does not require the insertion of an endoscope, which can be uncomfortable for some individuals. This can be an important consideration when selecting an assessment tool, particularly for individuals who may have difficulty cooperating with the procedure. While FEES has its advantages, such as the ability to directly visualize the pharyngeal and laryngeal structures and the absence of radiation exposure, VFSS is a valuable tool for assessing dysphagia and provides important information that can guide treatment decisions and improve outcomes for individuals with swallowing impairments. The choice of assessment tool should be based on the specific needs and circumstances of the individual and should be made in consultation with a speech-language pathologist or other qualified healthcare professional [44].
Clinicians should carefully consider the strengths and limitations of each assessment, as well as the specific needs and circumstances of the infant when selecting the most appropriate method for evaluating dysphagia in this population. Ultimately, a comprehensive and individualized approach to the assessment and management of dysphagia in infants is essential for optimizing swallowing function and promoting positive feeding outcomes.
Conclusion
Even though both the FEES and VFSS approaches are essential for evaluating infant feeding, the approximate validity and reliability of established conventions for instrumental assessment within the neonatal and pediatric populations are limited. Therefore, further investigations should focus on advancing studies aimed at developing standardized and approved conventions for instrumental appraisals in these populations.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
All authors equally contributed to preparing this article.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank physicians, nurses and the parents of infants in hospitals in Tehran.
References
- Uhm KE, Yi SH, Chang HJ, Cheon HJ, Kwon JY. Videofluoroscopic swallowing study findings in full-term and preterm infants with dysphagia. Ann Rehabil Med. 2013; 37(2):175-82. [DOI:10.5535/arm.2013.37.2.175]
- Coon ER, Srivastava R, Stoddard GJ, Reilly S, Maloney CG, Bratton SL. Infant videofluoroscopic swallow study testing, swallowing interventions, and future acute respiratory illness. Hosp Pediatr. 2016; 6(12):707-13. [DOI:10.1542/hpeds.2016-0049]
- Nevo N, Rubin L, Tamir A, Levine A, Shaoul R. Infant feeding patterns in the first 6 months: An assessment in full-term infants. J Pediatr Gastroenterol Nutr. 2007; 45(2):234-9. [DOI:10.1097/MPG.0b013e31803e1706]
- Arvedson JC, Lefton-Greif MA. Instrumental assessment of pediatric dysphagia. Semin Speech Lang. 2017; 38(2):135-46. [DOI:10.1055/s-0037-1599111]
- Lefton-Greif MA, Loughlin GM. Specialized studies in pediatric dysphagia. Semin Speech Lang. 1996; 17(4):311-29. [DOI:10.1055/s-2008-1064106]
- Lefton-Greif MA, Arvedson JC. Pediatric feeding/swallowing: yesterday, today, and tomorrow. Semin Speech Lang. 2016; 37(4):298-309.
- Frakking TT, Chang AB, O’Grady K-AF, David M, Walker-Smith K, Weir KA. The use of cervical auscultation to predict oropharyngeal aspiration in children: A randomized controlled trial. Dysphagia. 2016; 31(6):738-48. [DOI:10.1007/s00455-016-9727-5]
- McClellan HL, Sakalidis VS, Hepworth AR, Hartmann PE, Geddes DT. Validation of nipple diameter and tongue movement measurements with B-mode ultrasound during breastfeeding. Ultrasound Med Biol. 2010; 36(11):1797-807. [DOI:10.1016/j.ultrasmedbio.2010.08.005]
- Heckathorn D-E, Speyer R, Taylor J, Cordier R. Systematic review: Non-instrumental swallowing and feeding assessments in pediatrics. Dysphagia. 2016; 31(1):1-23. [DOI:10.1007/s00455-015-9667-5]
- Arvedson JC. Assessment of pediatric dysphagia and feeding disorders: Clinical and instrumental approaches. Dev Disabil Res Rev. 2008; 14(2):118-27. [DOI:10.1002/ddrr.17]
- Speyer R, Cordier R, Parsons L, Denman D, Kim JH. Psychometric characteristics of non-instrumental swallowing and feeding assessments in pediatrics: A systematic review using COSMIN. Dysphagia. 2018; 33(1):1-14. [DOI:10.1007/s00455-017-9835-x]
- Fujinaga CI, Zamberlan NE, Rodarte MDdO, Scochi CGS. Reliability of an instrument to assess the readiness of preterm infants for oral feeding. Pró-Fono Revista de Atualização Científica. 2007; 19(2):143-50. [DOI:10.1590/S0104-56872007000200002]
- Carrasco S, Panea B, Ripoll G, Sanz A, Joy M. Influence of feeding systems on cortisol levels, fat color and instrumental meat quality in light lambs. Meat Sci. 2009; 83(1):50-6. [DOI:10.1016/j.meatsci.2009.03.014]
- Anez E, Remington A, Wardle J, Cooke L. The impact of instrumental feeding on children’s responses to taste exposure. J Hum Nutr Diet. 2013; 26(5):415-20. [DOI:10.1111/jhn.12028]
- Reynolds J, Carroll S, Sturdivant C, Ikuta L, Zukowsky K. Fiberoptic endoscopic evaluation of swallowing. Adv Neonatal Care. 2016; 16(1):37-43. [DOI:10.1097/ANC.0000000000000245]
- Hartnick CJ, Hartley BE, Miller C, Willging JP. Pediatric fiberoptic endoscopic evaluation of swallowing. Ann Otology Rhinol Laryngol. 2000; 109(11):996-9. [DOI:10.1177/000348940010901102]
- Langmore SE. History of fiberoptic endoscopic evaluation of swallowing for evaluation and management of pharyngeal dysphagia: Changes over the years. Dysphagia. 2017; 32(1):27-38. [DOI:10.1007/s00455-016-9775-x]
- Lefton-Greif MA, McGrattan KE, Carson KA, Pinto JM, Wright JM, Martin-Harris B. First steps towards development of an instrument for the reproducible quantification of oropharyngeal swallow physiology in bottle-fed children. Dysphagia. 2018; 33(1):76-82. [DOI:10.1007/s00455-017-9834-y]
- Tian X, Yi LJ, Zhang L, Zhou JG, Ma L, Ou YX, et al. Oral motor intervention improved the oral feeding in preterm infants: Evidence based on a meta-analysis with trial sequential analysis. Medicine. 2015; 94(31):e1310. [DOI:10.1097/MD.0000000000001310]
- Martin-Harris B, Carson KA, Pinto JM, Lefton-Greif MA. BaByVFSSImP© a novel measurement tool for videofluoroscopic assessment of swallowing impairment in bottle-fed babies: establishing a standard. Dysphagia. 2020; 35(1):90-8. [DOI:10.1007/s00455-019-10008-x]
- Jaffal H, Isaac A, Johannsen W, Campbell S, El-Hakim HG. The prevalence of swallowing dysfunction in children with laryngomalacia: A systematic review. Int J Pediatr Otorhinolaryngol. 2020; 139:110464. [DOI:10.1016/j.ijporl.2020.110464]
- Hong JY, Hwang NK, Lee G, Park JS, Jung YJ. Radiation safety in videofluoroscopic swallowing study: Systematic review. Dysphagia. 2021; 36(1):73-82. [DOI:10.1007/s00455-020-10209-9]
- Narawane A, Rappazzo C, Hawney J, Eng J, Ongkasuwan J. Videofluoroscopic swallow study findings and correlations in infancy of children with cerebral palsy. Ann Otol Rhinol Laryngol. 2022; 131(5):478-84. [DOI:10.1177/00034894211026741]
- Kamity R, Kapavarapu PK, Chandel A. Feeding problems and long-term outcomes in preterm infants-A systematic approach to evaluation and management. Children. 2021; 8(12):1158. [DOI:10.3390/children8121158]
- O’Donoghue S, Bagnall A. Videofluoroscopic evaluation in the assessment of swallowing disorders in paediatric and adult populations. Folia Phoniatr Logop. 1999; 51(4-5):158-71. [DOI:10.1159/000021494]
- Suterwala MS, Reynolds J, Carroll S, Sturdivant C, Armstrong ES. Using fiberoptic endoscopic evaluation of swallowing to detect laryngeal penetration and aspiration in infants in the neonatal intensive care unit. J Perinatol. 2017; 37(4):404-8. [DOI:10.1038/jp.2016.239]
- Willette S, Molinaro LH, Thompson DM, Schroeder JW, Jr. Fiberoptic examination of swallowing in the breastfeeding infant. Laryngoscope. 2016; 126(7):1681-6. [DOI:10.1002/lary.25641]
- Willging JP. Endoscopic evaluation of swallowing in children. Int J Pediatr Otorhinolaryngol. 1995; 32:S107-8. [DOI:10.1016/0165-5876(94)01174-V]
- Armstrong ES, Reynolds J, Sturdivant C, Carroll S, Suterwala MS. Assessing swallowing of the breastfeeding nicu infant using fiberoptic endoscopic evaluation of swallowing: A feasibility study. Adv Neonatal Care. 2020; 20(3):244-50. [DOI:10.1097/ANC.0000000000000696]
- Vetter-Laracy S, Osona B, Roca A, Peña-Zarza JA, Gil JA, Figuerola J. Neonatal swallowing assessment using fiberoptic endoscopic evaluation of swallowing (FEES). Pediatr Pulmonol. 2018; 53(4):437-42. [DOI:10.1002/ppul.23946]
- Mills N, Keesing M, Geddes D, Mirjalili SA. Flexible endoscopic evaluation of swallowing in breastfeeding infants with laryngomalacia: Observed clinical and endoscopic changes with alteration of infant positioning at the breast. Ann Otol Rhinol Laryngol. 2021; 130(7):653-65. [DOI:10.1177/0003489420965636]
- Goldfield EC, Buonomo C, Fletcher K, Perez J, Margetts S, Hansen A, et al. Premature infant swallowing: patterns of tongue-soft palate coordination based upon videofluoroscopy. Infant Behav Dev. 2010; 33(2):209-18. [DOI:10.1016/j.infbeh.2009.10.001]
- Hernandez AM, Bianchini EMG. Swallowing analyses of neonates and infants in breastfeeding and bottle-feeding: Impact on videofluoroscopy swallow studies. Int Arch Otorhinolaryngol. 2019; 23(03):e343-53. [DOI:10.1055/s-0039-1677753]
- McGrattan KE, McGhee HC, McKelvey KL, Clemmens CS, Hill EG, DeToma A, et al. Capturing infant swallow impairment on videofluoroscopy: timing matters. Pediatr Radiol. 2020; 50(2):199-206. [DOI:10.1007/s00247-019-04527-w]
- Hernandez AM, Berto MI, Mandelbaum Gonçalves Bianchini E. Liquids offered in pediatric videofluoroscopy swallowing study: A preliminary rheological analysis. J Food Process Preserv. 2020; 44(12):e14910. [DOI:10.1111/jfpp.14910]
- Ekberg O, Nylander G, Fork FT, Sjöberg S, Birch-Iensen M, Hillarp B. Interobserver variability in cineradiographic assessment of pharyngeal function during swallow. Dysphagia. 1988; 3:46-8. [DOI:10.1007/BF02406279]
- Kim DH, Choi KH, Kim HM, Koo JH, Kim BR, Kim TW, et al. Inter-rater reliability of videofluoroscopic dysphagia scale. Ann Rehabil Med. 2012; 36(6):791-6. [DOI:10.5535/arm.2012.36.6.791]
- Kamran F, Sagheb S, Aghajanzade M, Ebadi A, Faryadras Y, Khatoonabadi AR. The interrater and intrarater reliability of the preterm infant oral feeding readiness assessment scale. J Modern Rehabil. 2019; 13(1):31-8. [DOI:10.32598/JMR.13.1.31]
- Prikladnicki A, Santana MG, Cardoso MC. Protocols and assessment procedures in fiberoptic endoscopic evaluation of swallowing: An updated systematic review. Brazilian J Otorhinolaryngology. 2022; 88(3):445-70. [DOI:10.1016/j.bjorl.2021.03.002]
- Langmore SE, Schatz K, Olsen N. Fiberoptic endoscopic examination of swallowing safety: A new procedure. Dysphagia. 1988; 2(4):216-9. [DOI:10.1007/BF02414429]
- Logemann JA, Pauloski BR, Rademaker AW, Colangelo LA. Speech and swallowing rehabilitation for head and neck cancer patients. Oncology. 1997; 11(5):651-9. [PMID]
- Langmore SE. Evaluation of oropharyngeal dysphagia: Which diagnostic tool is superior? Curr Opin Otolaryngol Head Neck Surg. 2003; 11(6):485-9. [DOI:10.1097/00020840-200312000-00014] [PMID]
- Silva APD, Neto JFL, Santoro PP. Comparison between videofluoroscopy and endoscopic evaluation of swallowing for the diagnosis of dysphagia in children. Otolaryngol Head Neck Surg. 2010; 143(2):204-9. [DOI:10.1016/j.otohns.2010.03.027]
- Snyderman CH, Gardner PA. Current opinion in otolaryngology and head and neck surgery: clival chordoma and its management. Curr Opin Otolaryngol Head Neck Surg. 2020; 28(2):118-21. [DOI:10.1097/MOO.0000000000000614]
Type of Study: Narrative Review |
Subject:
Pediatric Rehabilitation
Received: 2024/03/17 | Accepted: 2024/09/1 | Published: 2024/07/1
Received: 2024/03/17 | Accepted: 2024/09/1 | Published: 2024/07/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |