Volume 8, Issue 2 (4-2020)
J. Pediatr. Rev 2020, 8(2): 139-144 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rahimzadeh G, Ekrami Noghabi M, Kadkhodaei Elyaderani F, Navaeifar M R, Enayati A A, Manafi Anari A, et al . COVID-19 Infection in Iranian Children: A Case Series of 9 Patients. J. Pediatr. Rev 2020; 8 (2) :139-144
URL: http://jpr.mazums.ac.ir/article-1-314-en.html
URL: http://jpr.mazums.ac.ir/article-1-314-en.html
Golnar Rahimzadeh1 

 , Mina Ekrami Noghabi2
, Mina Ekrami Noghabi2 
 , Fereshteh Kadkhodaei Elyaderani3
, Fereshteh Kadkhodaei Elyaderani3 
 , Mohammad Reza Navaeifar1
, Mohammad Reza Navaeifar1 
 , Ahmad Ali Enayati4
, Ahmad Ali Enayati4 
 , Ali Manafi Anari5
, Ali Manafi Anari5 
 , Maryam Hujati1
, Maryam Hujati1 
 , Shaghayegh Rezai6
, Shaghayegh Rezai6 
 , Mohammad Sadegh Rezai *
, Mohammad Sadegh Rezai * 

 7
7


 , Mina Ekrami Noghabi2
, Mina Ekrami Noghabi2 
 , Fereshteh Kadkhodaei Elyaderani3
, Fereshteh Kadkhodaei Elyaderani3 
 , Mohammad Reza Navaeifar1
, Mohammad Reza Navaeifar1 
 , Ahmad Ali Enayati4
, Ahmad Ali Enayati4 
 , Ali Manafi Anari5
, Ali Manafi Anari5 
 , Maryam Hujati1
, Maryam Hujati1 
 , Shaghayegh Rezai6
, Shaghayegh Rezai6 
 , Mohammad Sadegh Rezai *
, Mohammad Sadegh Rezai * 

 7
7
1- Pediatric Infectious Diseases Research Center, Mazandaran University of Medical Sciences, Sari, Iran.
2- Department of Pediatrics, Bohlool Hospital, Gonabad University of Medical Sciences, Gonabad, Iran.
3- Taleghani Hospital, Mazandaran University of Medical Sciences, Chalus, Mazandaran, Iran.
4- School of Public Health and Health Sciences Research Center, Mazandaran University of Medical Sciences, Sari, Iran.
5- Ali Asghar children’s Hospital, Iran University of Medical Sciences, Tehran, Iran.
6- Department of Microbiology and Virology, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
7- Pediatric Infectious Diseases Research Center, Mazandaran University of Medical Sciences, Sari, Iran. ,rezai@mazums.ac.ir
2- Department of Pediatrics, Bohlool Hospital, Gonabad University of Medical Sciences, Gonabad, Iran.
3- Taleghani Hospital, Mazandaran University of Medical Sciences, Chalus, Mazandaran, Iran.
4- School of Public Health and Health Sciences Research Center, Mazandaran University of Medical Sciences, Sari, Iran.
5- Ali Asghar children’s Hospital, Iran University of Medical Sciences, Tehran, Iran.
6- Department of Microbiology and Virology, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
7- Pediatric Infectious Diseases Research Center, Mazandaran University of Medical Sciences, Sari, Iran. ,
Full-Text [PDF 363 kb]
(6013 Downloads)
| Abstract (HTML) (12138 Views)
Full-Text: (6092 Views)
1. Introduction
The novel coronavirus, which was temporarily named “2019 novel coronavirus (2019-nCoV),” emerged in Wuhan, China. It is now commonly known as the COVID-19. The first infected patient was admitted to Wuhan Central Hospital on December 26, 2019, experiencing severe respiratory syndrome along with fever, dizziness, and cough. As of February 24, 2020, 79331 confirmed cases, and 2618 deaths due to COVID-19 have been reported worldwide (1). The occurrence rate is relatively low in people 18 years old and younger (2.4% of all reported cases) (2-3).
The incubation period of the COVID-19 is about 2 to 14 days and transmitted by respiratory droplets and close contact. Reported illnesses have ranged from mild to severe symptoms and, eventually, death (4). Significant symptoms include fever, cough, shortness of breath, pneumonia, and other respiratory tract involvement complications. The clinical manifestation of pediatric patients may be different from those of the adults, e.g., lack of diarrhea and runny nose in children.
According to the national guidelines, the diagnosis of COVID-19 is confirmed by reverse-transcription polymerase chain reaction (RT-PCR) test from pharyngeal swab samples and detection of lesions by chest CT-scan (5-9). However, according to the experience of fellow Chinese physicians, chest CT-scan had a sensitivity of 97% for diagnosing COVID-19—even superior to RT-PCR (10). Although COVID-19 has no specific treatment up until now, antibiotic and antiviral therapies in conjunction with respiratory and other supportive care are recommended to manage the cases.
As the literature on pediatric COVID-19 cases is limited, we believe that sharing the experiences of the management of pediatric COVID-19 cases from Iran may be of interest to those involved in providing care for these patients all over the world.
2. Case Presentations
Cases 1 and 2
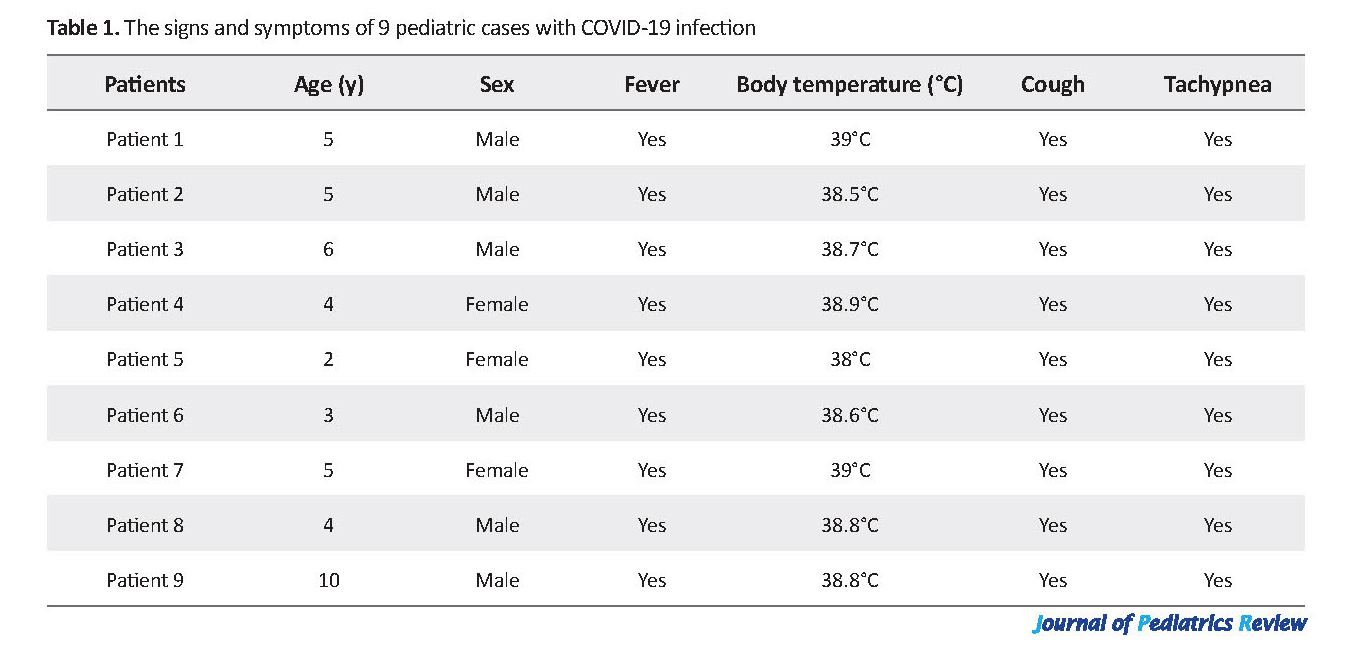
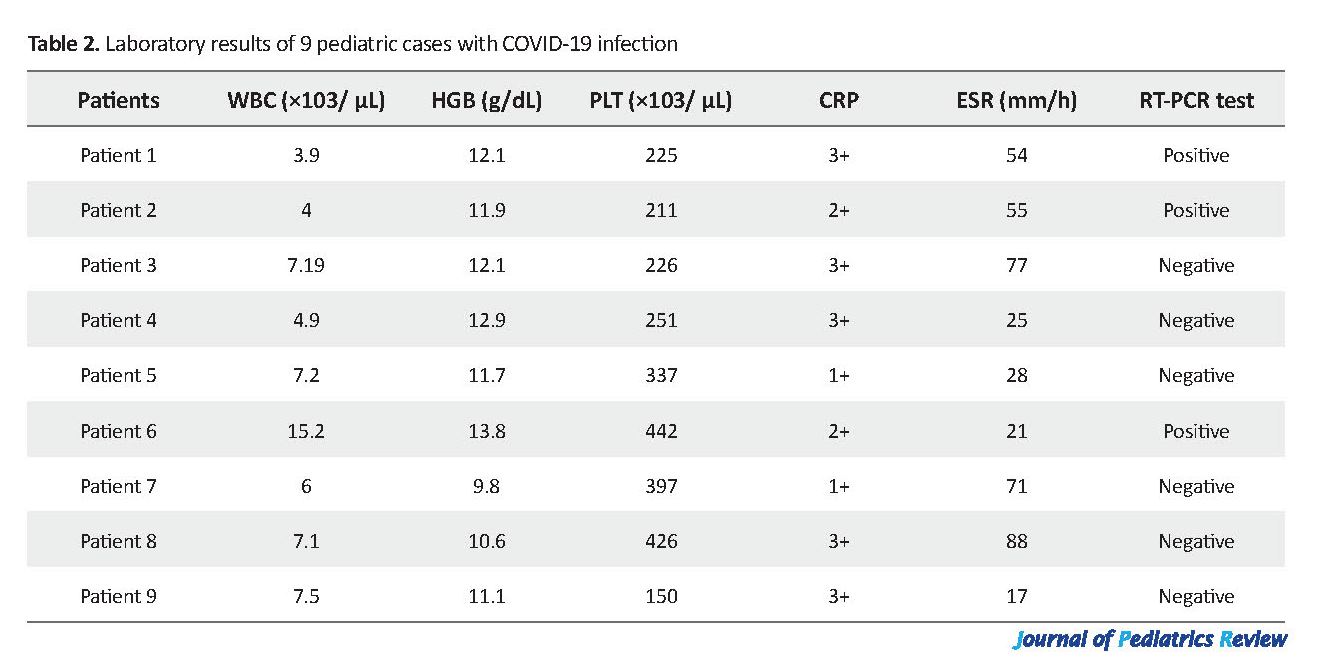
Two 5-year-old twin boys developed fever, chills, myalgia, weakness, cough, tachycardia, tachypnea, retraction, and crackle in both lungs after attending a wedding ceremony. They were admitted to the Taleghani Hospital in Chalus City, Iran (Table 1). They had no history of underlying diseases. Their aunt and grandmother were infected with COVID-19, too. The patients’ physical examination of cardiovascular, abdominal, and neurological characteristics was normal. Elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were detected in both cases, and RT-PCR was positive. Other laboratory data are presented in Table 2. At the time of referral, the blood oxygen was 67%, as measured by pulse oximetry.
The novel coronavirus, which was temporarily named “2019 novel coronavirus (2019-nCoV),” emerged in Wuhan, China. It is now commonly known as the COVID-19. The first infected patient was admitted to Wuhan Central Hospital on December 26, 2019, experiencing severe respiratory syndrome along with fever, dizziness, and cough. As of February 24, 2020, 79331 confirmed cases, and 2618 deaths due to COVID-19 have been reported worldwide (1). The occurrence rate is relatively low in people 18 years old and younger (2.4% of all reported cases) (2-3).
The incubation period of the COVID-19 is about 2 to 14 days and transmitted by respiratory droplets and close contact. Reported illnesses have ranged from mild to severe symptoms and, eventually, death (4). Significant symptoms include fever, cough, shortness of breath, pneumonia, and other respiratory tract involvement complications. The clinical manifestation of pediatric patients may be different from those of the adults, e.g., lack of diarrhea and runny nose in children.
According to the national guidelines, the diagnosis of COVID-19 is confirmed by reverse-transcription polymerase chain reaction (RT-PCR) test from pharyngeal swab samples and detection of lesions by chest CT-scan (5-9). However, according to the experience of fellow Chinese physicians, chest CT-scan had a sensitivity of 97% for diagnosing COVID-19—even superior to RT-PCR (10). Although COVID-19 has no specific treatment up until now, antibiotic and antiviral therapies in conjunction with respiratory and other supportive care are recommended to manage the cases.
As the literature on pediatric COVID-19 cases is limited, we believe that sharing the experiences of the management of pediatric COVID-19 cases from Iran may be of interest to those involved in providing care for these patients all over the world.
2. Case Presentations
Cases 1 and 2
Two 5-year-old twin boys developed fever, chills, myalgia, weakness, cough, tachycardia, tachypnea, retraction, and crackle in both lungs after attending a wedding ceremony. They were admitted to the Taleghani Hospital in Chalus City, Iran (Table 1). They had no history of underlying diseases. Their aunt and grandmother were infected with COVID-19, too. The patients’ physical examination of cardiovascular, abdominal, and neurological characteristics was normal. Elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were detected in both cases, and RT-PCR was positive. Other laboratory data are presented in Table 2. At the time of referral, the blood oxygen was 67%, as measured by pulse oximetry.
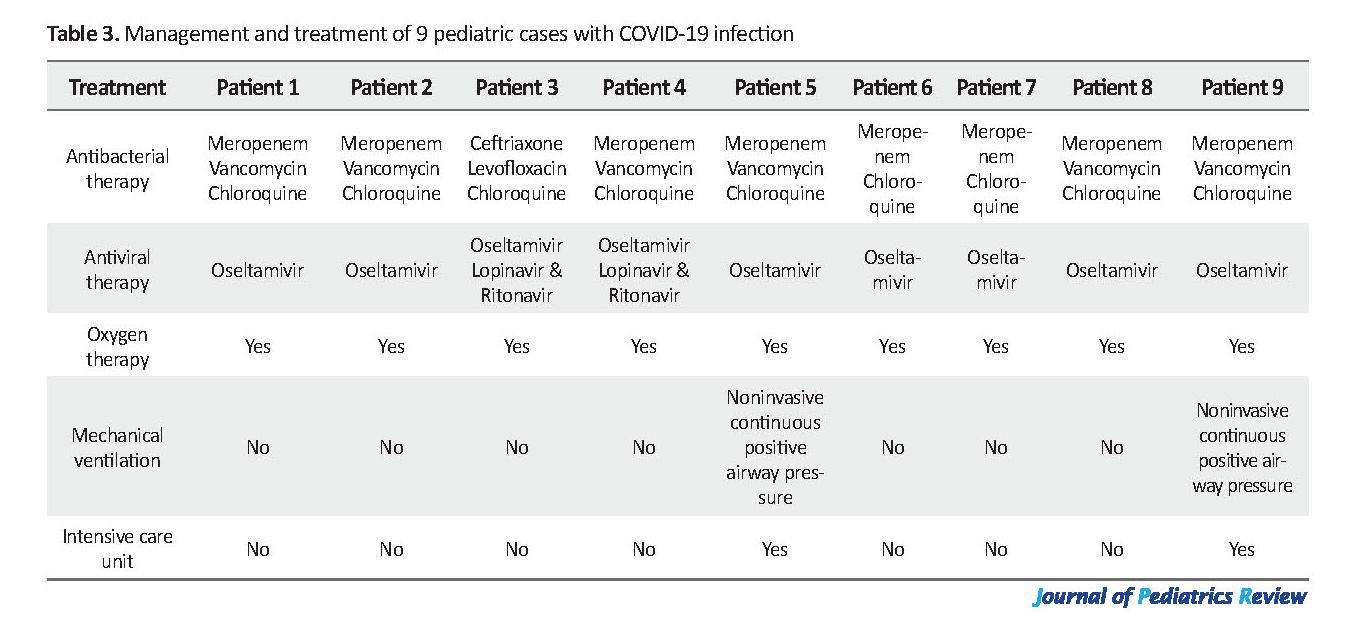
On the first day of admission, chest radiographs were abnormal with air-space shadowing. Chest high-resolution computed tomography (HRCT) findings were patchy consolidation with halo sign and ground glass appearance in both lungs (Figure 1). For their treatment, they received supportive care and antibiotic therapy (Table 3). After five days, their general condition improved, and their fever, tachypnea, and retraction subsided gradually. The video clip of the chest HRCT is uploaded on the website of the journal.
Cases 3, 4, and 5
A 6-year-old boy, a 2-year-old girl, and a 4-year-old girl with fever, chills, cough, tachypnea, retraction, and crackle in both lungs were hospitalized in Booali Sina Hospital, Sari City, Iran (Table 1). They had no history of underlying diseases. All cases had household contact with another COVID-19 case. Their physical examination of cardiovascular, abdominal, and neurological characteristics was normal. Their RT-PCR test results were negative. Only the 6-year-old boy complained of a headache. In all three cases, CRP and ESR values were high. Their laboratory data are presented in Table 2. The lactate dehydrogenase (LDH) test result of the 2-year-old girl was 671 U/L. The patients had mild hypoxemia with oxygen levels of 78%-90%, as determined by pulse oximetry.
A 6-year-old boy, a 2-year-old girl, and a 4-year-old girl with fever, chills, cough, tachypnea, retraction, and crackle in both lungs were hospitalized in Booali Sina Hospital, Sari City, Iran (Table 1). They had no history of underlying diseases. All cases had household contact with another COVID-19 case. Their physical examination of cardiovascular, abdominal, and neurological characteristics was normal. Their RT-PCR test results were negative. Only the 6-year-old boy complained of a headache. In all three cases, CRP and ESR values were high. Their laboratory data are presented in Table 2. The lactate dehydrogenase (LDH) test result of the 2-year-old girl was 671 U/L. The patients had mild hypoxemia with oxygen levels of 78%-90%, as determined by pulse oximetry.
On the first day of admission, chest radiographs were abnormal with air-space shadowing patchy consolidation with halo sign in both lungs. The 2-year-old girl needed a pediatric intensive care unit, and nasal continuous positive airway pressure (NCPAP) was used to improve her respiratory distress. All three patients received supportive care and antibiotic and antiviral therapy (Table 3). After 72 hours, the general condition of the patients improved, and their fever, tachypnea, and retraction subsided gradually. The video clips of their chest HRCT were uploaded on the website of the journal.
Cases 6, 7, and 8
A 5-year-old girl, a 3-year-old boy, and a 4-year-old boy were hospitalized in Bohlool Hospital, Gonabad City, Iran (Table 1) with fever, chills, myalgia, weakness, cough, tachypnea, retraction and crackle in both lungs. They had no history of underlying diseases. Their physical examination of cardiovascular, abdominal, and neurological characteristics was normal. Elevated CRP and ESR were detected in all of them. Table 2 presents their laboratory data. The patients had mild hypoxemia with oxygen levels of 90%-92%, as measured by pulse oximetry. COVID‐19 RNA was identified in the 3-year-old boy. This patient had normal chest CT-scan despite positive RT-PCR test. In other cases, the chest radiographs were abnormal with air-space shadowing and patchy consolidation with halo sign in chest HRCT (Figure 2). They received supportive care and antibiotic therapy (Table 3). Their general condition improved after three days, and they were discharged on outpatient orders, but the 5-year-old girl was discharged two days after admission with good general health. The 4-year-old boy was discharged seven days after admission.
Cases 6, 7, and 8
A 5-year-old girl, a 3-year-old boy, and a 4-year-old boy were hospitalized in Bohlool Hospital, Gonabad City, Iran (Table 1) with fever, chills, myalgia, weakness, cough, tachypnea, retraction and crackle in both lungs. They had no history of underlying diseases. Their physical examination of cardiovascular, abdominal, and neurological characteristics was normal. Elevated CRP and ESR were detected in all of them. Table 2 presents their laboratory data. The patients had mild hypoxemia with oxygen levels of 90%-92%, as measured by pulse oximetry. COVID‐19 RNA was identified in the 3-year-old boy. This patient had normal chest CT-scan despite positive RT-PCR test. In other cases, the chest radiographs were abnormal with air-space shadowing and patchy consolidation with halo sign in chest HRCT (Figure 2). They received supportive care and antibiotic therapy (Table 3). Their general condition improved after three days, and they were discharged on outpatient orders, but the 5-year-old girl was discharged two days after admission with good general health. The 4-year-old boy was discharged seven days after admission.
Case 9
A 10-year-old boy who was in close contact with a COVID-19 patient was hospitalized in Ali Asghar Hospital, Tehran city, Iran with fever, tachycardia, chills, myalgia, weakness, cough, tachypnea, retraction and crackle in is both lungs (Table 1). He had no history of an underlying disease. His physical examination of cardiovascular, abdominal, and neurological characteristics was normal. The patient had elevated CRP and ESR levels. Table 2 presents his other laboratory data. The patient had mild hypoxemia with oxygen levels of 68%, as measured by pulse oximetry. The level of LDH and creatine kinase (CPK) were high. On the first day of admission, his chest CT-scans were abnormal with air-space shadowing patchy consolidation and ground glass appearance in both lungs. The patient received supportive care and antibiotic therapy (Table 3). He was discharged after 13 days with a good general condition.
A 10-year-old boy who was in close contact with a COVID-19 patient was hospitalized in Ali Asghar Hospital, Tehran city, Iran with fever, tachycardia, chills, myalgia, weakness, cough, tachypnea, retraction and crackle in is both lungs (Table 1). He had no history of an underlying disease. His physical examination of cardiovascular, abdominal, and neurological characteristics was normal. The patient had elevated CRP and ESR levels. Table 2 presents his other laboratory data. The patient had mild hypoxemia with oxygen levels of 68%, as measured by pulse oximetry. The level of LDH and creatine kinase (CPK) were high. On the first day of admission, his chest CT-scans were abnormal with air-space shadowing patchy consolidation and ground glass appearance in both lungs. The patient received supportive care and antibiotic therapy (Table 3). He was discharged after 13 days with a good general condition.
3. Discussion
Herein, we reported nine 2-10 years old COVID-19 hospitalized patients from Iran. The incubation period in our cases ranged between 2 and 14 days. Our patients had no underlying diseases. Their common signs and symptoms were fever, chills, myalgia, weakness, cough, tachypnea, retraction, and crackle. All cases had household contact with COVID-19 cases. Although diarrhea and runny nose have been reported in Chinese cases, none of our patients experienced these symptoms, suggesting that the signs and symptoms in children may be different from adults (1, 5, 9).
The mean duration of fever before admission was four days, and almost all of them became afebrile after 48 to 72 hours. Furthermore, the general condition and respiratory status of the cases improved after 72 hours. Improvement of our patients may be due to the relatively benign course of viral infection, antiviral therapy, or management of probable bacterial superinfection.
Abnormal laboratory results include leukopenia, lymphopenia, and thrombocytopenia, elevated LDH, CPK, procalcitonin, ESR, and CRP (1, 9). In our cases, leukopenia and lymphopenia were observed in only 3 cases despite their poor condition. Elevated ESR and CRP were detected in all cases. We did not measure procalcitonin in our patients, but in the study of Wei et al. 2020, elevated procalcitonin was shown (80%) in pediatrics with COVID-19 infection, a condition not common in adults (9). RT-PCR test result of 3 patients was positive. Still, the rest of the cases had negative test results despite one family member being RT-PCR positive, which could be due to incorrect sampling or sensitivity of the test.
In the study of Liu et al. (2020), 366 children (≤16 years of age) were hospitalized at three branches of Tongji Hospital, Wuhan, China, for seven days. Previously six children had been completely healthy. The most frequently detected pathogens were influenza A virus in 23 patients (6.3%), influenza B virus in 20 (5.5%), and SARS-CoV-2 in 6 patients (1.6%). All six children had a high fever, cough, and lymphopenia. One child was admitted to the pediatric intensive care unit (ICU). All patients were discharged within 5-13 days with a good general condition (11).
Chest x-ray and HRCT findings in children with COVID-19 pneumonia may be similar to those of adults (10). All of our cases had abnormal findings in chest imaging, and most were mild to moderate. Based on our experience, diagnostic criteria, and condition of patients with COVID-19 pneumonia were relatively compatible with chest HRCT abnormality.
Most of our patients were treated with supportive management, including administrating oxygen, nebulizing with β2-agonist, using proper antibacterial therapy, hydroxychloroquine, and oseltamivir. In one study, 40% of the patients had a coinfection; so, empirical antibiotics were used (11).
Only LPN/r was added to the treatment protocol of two patients who did not tolerate it for more than two days. None of our patients were given ribavirin. Two cases needed pediatric intensive care unit, and NCPAP was used to improve their respiratory distress. Almost all of our patients were discharged within six days with a good general condition, no respiratory distress, and no need for oxygen. Obviously, no mortality occurred in our cases.
4. Conclusions
The prognosis for COVID-19 pneumonia is good in children with no underlying diseases. None of our patients presented with diarrhea, vomiting, or a runny nose. Appropriate supportive care, antibiotics, and antiviral therapy were the key to the patients’ recovery. Our patients recovered without the need for LPN/r, ribavirin, and mechanical ventilation.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed about the purpose of the research and its implementation stages; they were also assured about the confidentiality of their information. Moreover, they were allowed to leave the study whenever they wish, and if desired, the results of the research would be available to them.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
All authors contributed equally in preparing all parts of the research.
Conflicts of interest
The authors declared no conflict of interest.
References
Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020; 579:265-9. [DOI:10.1038/s41586-020-2008-3] [PMID]
Huang PC, Wang Y, Li PX, Ren PL, Zhao PG, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395(10223):497‐506. [DOI:10.1016/S0140-6736(20)30183-5]
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020; 382:727‐33. [DOI:10.1056/NEJMoa2001017] [PMID]
Hui DS, Azhar EI, Madani TA, Ntoumi F, Kock R, Dar O, et al. The continuing 2019‐nCoV epidemic threat of novel coronaviruses to global health - the latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020; 91:264‐6. [DOI:10.1016/j.ijid.2020.01.009] [PMID]
Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G, et al. Clinical analysis of 10 neonates born to mothers with 2019‐nCoV pneumonia. Transl Pediatr. 2020; 9(1):51‐60. [DOI:10.21037/tp.2020.02.06] [PMID] [PMCID]
Parry J. Wuhan: Britons to be evacuated as scientists estimate 44 000 cases of 2019‐nCOV in the city. BMJ. 2020; 368:m351. [DOI:10.1136/bmj.m351] [PMID]
Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, et al. Emerging 2019 novel coronavirus (2019-nCoV) Pneumonia. Radiology. 2020; 00(0):1-8. [DOI:10.1148/radiol.2020200274] [PMID]
Kanne JP. Chest CT findings in 2019 novel coronavirus (2019‐nCoV) infections from Wuhan, China: Key points for the radiologist. Radiology. 2020; xxx(x—xxxx):1-2. [DOI:10.1148/radiol.2020200241] [PMID]
Xia W, Shao J, Guo Y, Peng X, Li Z, Hu D. Clinical and CT features in pediatric patients with COVID‐19 infection: Different points from adults. Pediatr Pulmonol. 2020 March. [DOI:10.1002/ppul.24718]
Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology. 2020 February. [DOI:10.1148/radiol.2020200642] [PMID]
Liu W, Zhang Q, Chen J, Xiang R, Song H, Shu S, et al. Detection of Covid-19 in children in early January 2020 in Wuhan, China. N Engl J Med. 2020 March. [DOI:10.1056/NEJMc2003717]
Herein, we reported nine 2-10 years old COVID-19 hospitalized patients from Iran. The incubation period in our cases ranged between 2 and 14 days. Our patients had no underlying diseases. Their common signs and symptoms were fever, chills, myalgia, weakness, cough, tachypnea, retraction, and crackle. All cases had household contact with COVID-19 cases. Although diarrhea and runny nose have been reported in Chinese cases, none of our patients experienced these symptoms, suggesting that the signs and symptoms in children may be different from adults (1, 5, 9).
The mean duration of fever before admission was four days, and almost all of them became afebrile after 48 to 72 hours. Furthermore, the general condition and respiratory status of the cases improved after 72 hours. Improvement of our patients may be due to the relatively benign course of viral infection, antiviral therapy, or management of probable bacterial superinfection.
Abnormal laboratory results include leukopenia, lymphopenia, and thrombocytopenia, elevated LDH, CPK, procalcitonin, ESR, and CRP (1, 9). In our cases, leukopenia and lymphopenia were observed in only 3 cases despite their poor condition. Elevated ESR and CRP were detected in all cases. We did not measure procalcitonin in our patients, but in the study of Wei et al. 2020, elevated procalcitonin was shown (80%) in pediatrics with COVID-19 infection, a condition not common in adults (9). RT-PCR test result of 3 patients was positive. Still, the rest of the cases had negative test results despite one family member being RT-PCR positive, which could be due to incorrect sampling or sensitivity of the test.
In the study of Liu et al. (2020), 366 children (≤16 years of age) were hospitalized at three branches of Tongji Hospital, Wuhan, China, for seven days. Previously six children had been completely healthy. The most frequently detected pathogens were influenza A virus in 23 patients (6.3%), influenza B virus in 20 (5.5%), and SARS-CoV-2 in 6 patients (1.6%). All six children had a high fever, cough, and lymphopenia. One child was admitted to the pediatric intensive care unit (ICU). All patients were discharged within 5-13 days with a good general condition (11).
Chest x-ray and HRCT findings in children with COVID-19 pneumonia may be similar to those of adults (10). All of our cases had abnormal findings in chest imaging, and most were mild to moderate. Based on our experience, diagnostic criteria, and condition of patients with COVID-19 pneumonia were relatively compatible with chest HRCT abnormality.
Most of our patients were treated with supportive management, including administrating oxygen, nebulizing with β2-agonist, using proper antibacterial therapy, hydroxychloroquine, and oseltamivir. In one study, 40% of the patients had a coinfection; so, empirical antibiotics were used (11).
Only LPN/r was added to the treatment protocol of two patients who did not tolerate it for more than two days. None of our patients were given ribavirin. Two cases needed pediatric intensive care unit, and NCPAP was used to improve their respiratory distress. Almost all of our patients were discharged within six days with a good general condition, no respiratory distress, and no need for oxygen. Obviously, no mortality occurred in our cases.
4. Conclusions
The prognosis for COVID-19 pneumonia is good in children with no underlying diseases. None of our patients presented with diarrhea, vomiting, or a runny nose. Appropriate supportive care, antibiotics, and antiviral therapy were the key to the patients’ recovery. Our patients recovered without the need for LPN/r, ribavirin, and mechanical ventilation.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed about the purpose of the research and its implementation stages; they were also assured about the confidentiality of their information. Moreover, they were allowed to leave the study whenever they wish, and if desired, the results of the research would be available to them.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
All authors contributed equally in preparing all parts of the research.
Conflicts of interest
The authors declared no conflict of interest.
References
Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020; 579:265-9. [DOI:10.1038/s41586-020-2008-3] [PMID]
Huang PC, Wang Y, Li PX, Ren PL, Zhao PG, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395(10223):497‐506. [DOI:10.1016/S0140-6736(20)30183-5]
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020; 382:727‐33. [DOI:10.1056/NEJMoa2001017] [PMID]
Hui DS, Azhar EI, Madani TA, Ntoumi F, Kock R, Dar O, et al. The continuing 2019‐nCoV epidemic threat of novel coronaviruses to global health - the latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020; 91:264‐6. [DOI:10.1016/j.ijid.2020.01.009] [PMID]
Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G, et al. Clinical analysis of 10 neonates born to mothers with 2019‐nCoV pneumonia. Transl Pediatr. 2020; 9(1):51‐60. [DOI:10.21037/tp.2020.02.06] [PMID] [PMCID]
Parry J. Wuhan: Britons to be evacuated as scientists estimate 44 000 cases of 2019‐nCOV in the city. BMJ. 2020; 368:m351. [DOI:10.1136/bmj.m351] [PMID]
Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, et al. Emerging 2019 novel coronavirus (2019-nCoV) Pneumonia. Radiology. 2020; 00(0):1-8. [DOI:10.1148/radiol.2020200274] [PMID]
Kanne JP. Chest CT findings in 2019 novel coronavirus (2019‐nCoV) infections from Wuhan, China: Key points for the radiologist. Radiology. 2020; xxx(x—xxxx):1-2. [DOI:10.1148/radiol.2020200241] [PMID]
Xia W, Shao J, Guo Y, Peng X, Li Z, Hu D. Clinical and CT features in pediatric patients with COVID‐19 infection: Different points from adults. Pediatr Pulmonol. 2020 March. [DOI:10.1002/ppul.24718]
Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology. 2020 February. [DOI:10.1148/radiol.2020200642] [PMID]
Liu W, Zhang Q, Chen J, Xiang R, Song H, Shu S, et al. Detection of Covid-19 in children in early January 2020 in Wuhan, China. N Engl J Med. 2020 March. [DOI:10.1056/NEJMc2003717]
Type of Study: Case Report and Review of Literature |
Subject:
Pediatric Infectious Diseases
Received: 2020/03/13 | Accepted: 2020/03/13 | Published: 2020/04/1
Received: 2020/03/13 | Accepted: 2020/03/13 | Published: 2020/04/1
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |